Abstract
Background
Despite available treatments, major depression is a highly heterogeneous disorder, which leads to problems in classification and treatment specificity. Previous studies have reported that personality traits predict and influence the course and treatment response of depression. The Temperament and Personality Questionnaire (T&P) assesses eight major constructs of personality traits observed in those who develop depression. The aim of this study was to investigate the influence of T&P’s eight constructs on the treatment outcome of depressed patients.
Patients and methods
A preliminary 6-month prospective study was conducted with a sample of 51 adult patients with a diagnosis of major depressive disorder (MDD) without remarkable psychomotor disturbance using the Diagnostic and Statistical Manual of Mental Disorders, fourth edition. All patients received comprehensive assessment including the T&P at baseline. We compared each T&P construct score between patients who achieved remission and those who did not achieve remission after 6 months of treatment for depression using both subjective and objective measures. All 51 (100%) patients received the 6-month follow-up assessment.
Results
This study demonstrated that higher scores on T&P personal reserve predicted poorer treatment outcome in patients with MDD. Higher levels of personal reserve, rejection sensitivity, and self-criticism correlated with higher levels of depression. Higher levels of rejection sensitivity and self-criticism were associated with non-remitters; however, when we controlled for baseline depression severity, this relationship did not show significance.
Conclusion
Although the results are preliminary, this study suggests that high scores on T&P personal reserve predict poorer treatment outcome and T&P rejection sensitivity and self-criticism correlate with the severity of depression. Longer follow-up studies with large sample sizes are required to improve the understanding of these relationships.
Keywords: Temperament and Personality Questionnaire, classification, treatment outcome, personal reserve, self-criticism, rejection sensitivity
Introduction
Depression is a common mental disorder. Approximately 350 million people suffer from depression globally.1 Major depressive disorder (MDD) can cause significant distress and impairment in individuals, and it also places a substantial burden on society.2 Despite available treatments, MDD is a remarkably heterogeneous disorder, causing problems in classification and treatment specificity.3 Studies have consistently reported that personality traits predict4 and influence the treatment outcome of depression in both pharmacotherapy5 and psychotherapy.6 Existing literature indicates that depressed patients show high scores on neuroticism and low scores for extraversion and conscientiousness.7 Moreover, depression severity correlates positively with neuroticism8 and inversely with extraversion.9 Furthermore, higher scores on neuroticism,10 as well as on measures of harm avoidance11 and obsessional interference,12 were associated with poorer outcomes in depression treatment.
Parker and Roy13 suggested that non-melancholic depression is associated with predisposing personality styles and performed several studies to clarify such personality traits. The researchers performed careful clinical observations and a comprehensive literature review of personality traits overrepresented in those who have depressive disorders to develop the Temperament and Personality Questionnaire (T&P).14 T&P comprises 109 self-report items and dimensionally assesses eight major constructs of temperament and personality observed in those who have non-melancholic depression.
Therefore, this study investigated the influence of T&P’s eight constructs on the treatment outcome of depressed patients. We compared each T&P construct score between patients who achieved remission and those who did not achieve remission after 6 months of treatment in a naturalistic, noncontrolled, treatment setting.
Patients and methods
Participants
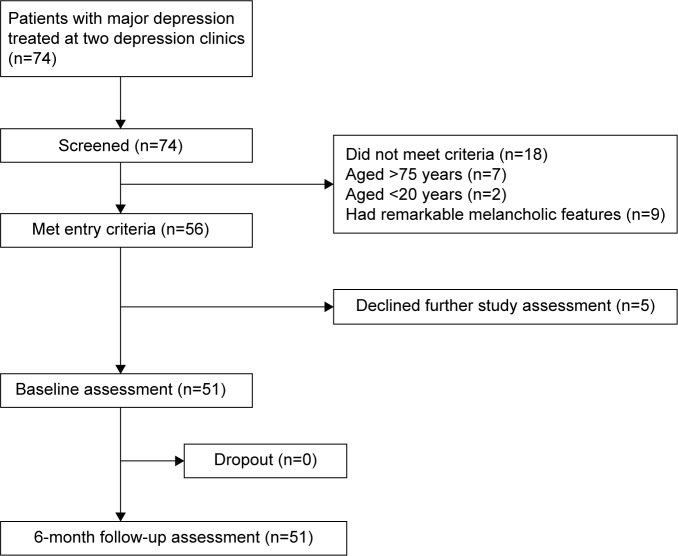
We recruited depressed patients from April 2014 to June 2016. Patients were eligible to be included in the study if they met the following criteria: 1) they were outpatients who had a diagnosis of MDD as defined by the Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) criteria for single or recurrent depression; 2) their age was between 20 and 75 years; and 3) they were competent and able to provide informed consent. Patients were excluded from the study if they presented remarkable psychomotor disturbances (a core feature of melancholia)15 at baseline based on clinical assessment by the study’s psychiatrists. We initially contacted 74 patients and 56 met the criteria. Among the 56 patients, five declined to participate in the study; therefore, 51 received the baseline assessment. All 51 (100%) patients received the 6-month follow-up assessment (Figure 1). For the total sample, the mean age of the patients was 40.9 years (SD =11.5), and 68.6% (n=35) were women. The mean years of education was 14.5 years (SD =2.3). A total of 33 patients (64.7%) were employed; 24 patients (47.1%) were married; and 39 patients (76.5%) were cohabiting. The average total number of depressive episodes was 1.6 (SD =1.2), and the median duration of current depressive episode was 9 months (interquartile range =4–27). The mean baseline 21-item GRID-Hamilton Depression Rating Scale (GRID-HAMD21) score was 13.9 (SD =8.2), indicating that the participants were experiencing a mild- to moderate-level depression. The study was conducted at a depression clinic at two hospitals, where the patients received clinical consultation and management; one was a university hospital located in central Tokyo, and the other was a psychiatric hospital located in the northern part of the Greater Tokyo Area. Written informed consent was obtained from all patients prior to participating in the study. The study was approved by the ethics committees of Keio University School of Medicine and Gunma Hospital.
Figure 1.
Flowchart of patient selection process for the study.
Procedure
At baseline, all participants received a comprehensive semi-structured clinical interview by the study psychiatrists and completed an assessment battery that included the T&P. The diagnostic interview was conducted using the Structured Clinical Interview for DSM-IV (SCID).16 Demographic data and clinical characteristics including age, sex, total education in years, employment status, marital status, habitation setting, total number of depressive episodes, and duration of current depressive episodes were collected. Depression severity was assessed using the observer-rated GRID-HAMD21,17,18 the self-report Beck Depression Inventory-Second Edition (BDI-II),19,20 and the 16-item Quick Inventory Depressive Symptomatology (Self-Report) (QIDS-SR16).21,22 The Sheehan Disability Scale (SDS)23,24 was used to measure the degree of disability and functional impairment due to depression. Depression severity and functional impairment were reassessed at 6-month follow-up. Patients with a GRID-HAMD21 score ≤7 were considered as achieving remission.25
Measures
T&P
The T&P comprises 109 self-report items that dimensionally assess eight personality trait constructs observed in those who develop non-melancholic depression.14 Each item on the questionnaire was rated on a 4-point Likert scale. Higher scores indicate a greater tendency of the personality trait. The eight constructs of T&P are 1) anxious worrying (a tendency to become stressed, worried, and anxious); 2) personal reserve (a tendency to keep one’s inner feelings to oneself); 3) perfectionism (a tendency to be very responsible, to have high standards for oneself, and to be highly committed to tasks and duties); 4) irritability (a tendency to be quick tempered and to “externalize” stress by becoming “snappy” and irritated by little things); 5) social avoidance (a tendency to be introverted and to keep to oneself, while those low on this dimension tend to be very sociable); 6) rejection sensitivity (a tendency to worry about rejection or abandonment); 7) self-criticism (a tendency to be very tough on oneself); and 8) self-focused (a tendency to prioritize one’s needs over others).26 The eight constructs of the T&P crossmatch with the constructs of the five-factor model (FFM), neuroticism, extraversion, openness, agreeableness, and conscientiousness, which is the most widely accepted model of the personality traits.27,28 The FFM construct of neuroticism corresponds to the T&P constructs of anxious worrying, irritability, self-criticism, and rejection sensitivity; FFM introversion (the other end of the extroversion dimension) corresponds to T&P personal reserve and social avoidance; FFM conscientiousness corresponds to T&P perfectionism; and FFM agreeableness inversely corresponds to the T&P self-focused construct.27 The Japanese version of T&P had high test–retest reliability (intra-class correlations of 0.77–0.89), internal consistency (Cronbach’s α of 0.67–0.91), and an adequate level of convergent validity (ρ=0.2–0.4).29
GRID-HAMD21
The GRID-HAMD21 has been the gold standard assessment for observer-rated depressive symptomatology. The GRID-HAMD was developed to set standards for scoring and administering the original HAMD.30 The GRID-HAMD is scored between 0 and 4, with larger numbers indicate greater severity, based upon the assessment of symptom intensity and symptom frequency over the past 7 days. Support for the validity and reliability of the GRID-HAMD has been shown.17,18
BDI-II
The BDI-II is a widely used self-report instrument to assess the severity of depressive symptoms and was developed by Beck et al,19 with its first version published in 1961. The BDI-II is a 21-item questionnaire, and each item is answered by circling a number between 0 and 3, with larger numbers indicating greater severity. Symptom severity for BDI-II is assessed for the previous 2 weeks to better coincide with DSM criteria. Good reliability and validity have been reported for the Japanese version.20
QIDS-SR16
The QIDS-SR16 is an abbreviated self-report version of the clinician-rated 30-item Inventory of Depressive Symptomatology (IDS), designed to assess the severity of depressive symptoms, which was developed by Rush et al.21 The QIDS-SR16 is a 16-item questionnaire and assesses all the DSM criterion symptoms for diagnosing a major depressive episode. Symptom severity is assessed for the previous 7 days before assessment. The total scores range from 0 to 27, with larger numbers indicating greater severity. The internal consistency is excellent, and the validity is very good,21 which was consistent with the Japanese version.22
SDS
The SDS is a self-report measure that assesses impairment from panic, anxiety, phobic, or depressive symptoms in three domains: 1) work, 2) social life or leisure activities, and 3) home life or family responsibilities. Each item was rated on a 10-point visual analog scale. The three items can be summed into a single dimensional measure of global functional impairment ranging from 0 (unimpaired) to 30 (highly impaired).23 Support has been found for the validity and reliability of the Japanese version of the SDS.24
Statistical analysis
T&P construct scores were compared between remitters (patients who achieved remission) and non-remitters with Student’s t-tests or Mann–Whitney U tests. Pearson correlations were used to assess relationships between the eight T&P construct scores and depression severity scores at 6-month follow-up. A paired-samples t-test was used to evaluate treatment improvement from baseline to 6 months later. To address the potential confounds between T&P constructs and depression severity, we performed logistic regression analyses with remitters/non-remitters as the dependent variable. Independent variables were T&P constructs that differed significantly in the univariate tests and baseline GRID-HAMD21 scores. The significance level was set at 0.05 (two-tailed) for all analyses. All statistical analyses were performed using SPSS Version 22.0 (IBM Corporation, Armonk, NY, USA).
Results
Demographic and clinical characteristics
The comparison of sociodemographics and clinical characteristics between remitters (n=23, 45.1%) and non-remitters (n=28, 54.9%) is shown in Table 1. The depression severity and functional impairment scores of non-remitters were higher than those of remitters. During the 6-month period, 45 patients (88.2%) received antidepressant therapy only, five (9.8%) received a combination of antidepressant therapy and cognitive behavioral therapy, and one (2.0%) received cognitive behavioral therapy only (Table 1).
Table 1.
Comparison of demographics and clinical characteristics between remitters and non-remitters
| Demographics and clinical characteristics | Remitter (n=23) | Non-remitter (n=28) | Total (n=51) |
|---|---|---|---|
| Age (years) | 40.3 (12.6) | 41.5 (10.8) | 40.9 (11.5) |
| Women | 17 (73.9%) | 18 (64.3%) | 35 (68.6%) |
| Education (years) | 14.9 (2.4) | 14.1 (2.2) | 14.5 (2.3) |
| Employed | 13 (56.5%) | 20 (71.4%) | 33 (64.7%) |
| Unemployed | 3 (13.0%) | 5 (17.8%) | 8 (15.7%) |
| Housewife and student | 7 (30.4%) | 3 (10.7%) | 10 (19.6%) |
| Marital status | |||
| Married | 13 (56.5%) | 11 (39.3%) | 24 (47.1%) |
| Separated, divorced, widowed | 1 (4.3%) | 4 (14.3%) | 5 (9.8%) |
| Single | 9 (39.1%) | 13 (46.4%) | 22 (43.1%) |
| Cohabiting | 20 (87.0%) | 19 (67.9%) | 39 (76.5%) |
| Family history of psychiatric disorders | 8 (34.7%) | 13 (46.4%) | 21 (41.2%) |
| Total number of lifetime depressive episodes | 1.4 (0.8) | 1.7 (1.4) | 1.6 (1.2) |
| Median duration of current depressive episode (months) | 7 | 13.5 | 9 |
| Depression severity at baseline | |||
| GRID-HAMD21 | 10.0 (7.9) | 17.1 (7.0) | 13.9 (8.2) |
| BDI-II | 17.8 (12.1) | 27.8 (11.0) | 23.6 (12.6) |
| QIDS-SR16 | 8.8 (6.9) | 14.0 (5.1) | 11.6 (6.5) |
| Degree of functional impairment at baseline | |||
| SDS total | 11.8 (7.8) | 16.2 (7.3) | 14.2 (7.8) |
| SDS work domain | 4.5 (3.2) | 6.1 (2.9) | 5.3 (3.1) |
| SDS social life domain | 4.5 (2.8) | 5.9 (2.8) | 5.3 (2.8) |
| SDS family life domain | 2.9 (2.7) | 4.2 (2.7) | 3.6 (2.7) |
| Number of antidepressant treatment courses for current episode | |||
| 0 | 0 (0.0%) | 1 (3.6%) | 1 (2.0%) |
| 1–2 | 20 (87.0%) | 14 (50.0%) | 34 (66.7%) |
| 3–4 | 2 (8.7%) | 11 (39.2%) | 13 (25.4%) |
| 5 or more | 1 (4.3%) | 2 (7.1%) | 3 (5.9%) |
| Duration of antidepressant treatment for current episode | |||
| <6 months | 16 (69.6%) | 12 (42.9%) | 28 (54.9%) |
| 6 months to 1 year | 4 (17.3%) | 3 (10.7%) | 7 (13.7%) |
| 1–2 years | 1 (4.3%) | 6 (21.4%) | 7 (13.7%) |
| >2 years | 2 (8.7%) | 7 (25.0%) | 9 (17.6%) |
| Used antidepressant at baseline | |||
| SSRI | |||
| Sertraline | 15 (65.2%) | 13 (46.4%) | 28 (54.9%) |
| Paroxetine | 0 (0.0%) | 2 (7.1%) | 2 (3.9%) |
| Fluvoxamine | 1 (4.3%) | 0 (0.0%) | 1 (2.0%) |
| Escitalopram | 2 (8.7%) | 0 (0.0%) | 2 (3.9%) |
| SNRI | |||
| Duloxetine | 2 (8.7%) | 3 (10.7%) | 5 (9.8%) |
| Milnacipran | 1 (4.3%) | 1 (3.6%) | 2 (3.9%) |
| TCA | |||
| Amoxapine | 0 (0.0%) | 1 (3.6%) | 1 (2.0%) |
| Nortriptyline | 0 (0.0%) | 1 (3.6%) | 1 (2.0%) |
| Amitriptyline | 1 (4.3%) | 1 (3.6%) | 2 (3.9%) |
| Other | |||
| Mirtazapine | 1 (4.3%) | 3 (10.7%) | 4 (7.8%) |
| Trazodone | 0 (0.0%) | 1 (3.6%) | 1 (2.0%) |
| Mianserin | 0 (0.0%) | 1 (3.6%) | 1 (2.0%) |
| Treatment modality at 6 months post baseline | |||
| Antidepressant therapy only | 20 (87.0%) | 25 (89.3%) | 45 (88.2%) |
| Combination of antidepressant therapy and CBT | 3 (13.0%) | 2 (7.1%) | 5 (9.8%) |
| CBT only | 0 (0.0%) | 1 (3.6%) | 1 (2.0%) |
Notes: Data are shown as mean (SD) or n (%). Remitters means patients who achieved remission by the 6-month assessment (GRID-HAMD21 ≤7).
Abbreviations: BDI-II, Beck Depression Inventory, Second Edition; CBT, cognitive behavioral therapy; GRID-HAMD21, 21-item GRID-Hamilton Depression Rating Scale; QIDS-SR16, 16-Item Quick Inventory Depressive Symptomatology (Self-Report); SDS, Sheehan Disability Scale; SNRI, serotonin–norepinephrine reuptake inhibitor; SSRI, selective serotonin reuptake inhibitor; TCA, tricyclic antidepressants.
Treatment outcomes
Treatment outcomes are summarized in Table 2. At the 6-month assessment, depressive symptoms improved based on both observer-rated GRID-HAMD21 scores and self-reported BDI-II and QIDS-SR16 scores. All three domains of SDS scores also showed significant improvement.
Table 2.
Scores on treatment outcome measures
| Baseline (n=51) |
6 months (n=51) |
P-valuea | |
|---|---|---|---|
| Depression severity | |||
| GRID-HAMD21 | 13.9 (8.2) | 9.9 (7.5) | 0.001 |
| BDI-II | 23.6 (12.6) | 16.9 (13.8) | 0.001 |
| QIDS-SR16 | 11.6 (6.5) | 8.2 (5.5) | <0.001 |
| Functional impairment | |||
| SDS total | 14.2 (7.8) | 10.1 (7.9) | <0.001 |
| SDS work domain | 5.3 (3.1) | 4.0 (3.3) | 0.001 |
| SDS social life domain | 5.3 (2.8) | 3.7 (2.9) | <0.001 |
| SDS family life domain | 3.6 (2.7) | 2.4 (2.4) | 0.001 |
Notes: Data are shown as mean (SD).
Paired-samples t-test.
Abbreviations: BDI-II, Beck Depression Inventory, Second Edition; GRID-HAMD21, 21-item GRID-Hamilton Depression Rating Scale; QIDS-SR16, 16-Item Quick Inventory Depressive Symptomatology (Self-Report); SDS, Sheehan Disability Scale.
Comparison of the eight T&P construct scores between remitters and non-remitters
The comparison of the eight T&P construct scores between remitters and non-remitters is shown in Table 3. Non-remitters at the 6-month assessment showed higher scores than remitters on personal reserve, rejection sensitivity, and self-criticism. On the other hand, anxious worrying, perfectionism, irritability, social avoidance, and self-focused did not show a significant difference between remitters and non-remitters.
Table 3.
Comparison of T&P construct scores between remitters and non-remitters (n=51)
| Characteristics | Remitter (n=23) |
Non-remitter (n=28) |
t | P-valuea |
|---|---|---|---|---|
| Anxious worrying | 14.2 (5.1) | 15.3 (4.5) | −0.82 | 0.42 |
| Personal reserve | 8.4 (6.0) | 12.3 (5.3) | −2.41 | 0.02 |
| Perfectionism | 12.2 (5.8) | 12.7 (5.0) | −0.36 | 0.72 |
| Irritability | 10.2 (6.0) | 10.7 (5.6) | −0.28 | 0.78 |
| Social avoidance | 13.8 (4.0) | 15.0 (4.5) | −1.03 | 0.31 |
| Rejection sensitivity | 5.8 (4.6) | 8.6 (4.8) | −2.14 | 0.04 |
| Self-criticism | 12.8 (4.2) | 15.4 (3.5) | −2.46 | 0.02 |
| Self-focused | 4.0 (2.9) | 4.4 (3.3) | −0.44 | 0.66 |
Notes: Data are shown as mean (SD).
Student’s t-test.
Abbreviation: T&P, Temperament and Personality Questionnaire.
We then reran the analyses substituting the subjective measure of BDI-II ≤10 for the objective measure of GRID-HAMD21 ≤7 as the remission criteria. Again, personal reserve (P=0.009), rejection sensitivity (P=0.049), and self-criticism (P=0.02) showed higher scores among non-remitters (n=21, 41.2%).
Next, we examined the association between T&P constructs and remitters/non-remitters in a subgroup of 18 patients with moderate–severe depression (baseline GRID-HAMD21 score ≥17),31 and found that personal reserve approached significance (P=0.05), but rejection sensitivity (P=0.17) and self-criticism (P=0.86) did not.
Multivariate analysis
Table 4 provides a summary of the multivariate analyses. In a logistic regression with remitters/non-remitters as the dependent variable, and personal reserve and baseline GRID-HAMD21 scores as the independent variables, both personal reserve and baseline GRID-HAMD21 scores were independently associated with remitters/non-remitters. Using the same model, substituting rejection sensitivity and self-criticism for personal reserve, baseline GRID-HAMD21 scores were independently associated with remitters/non-remitters but not with rejection sensitivity or self-criticism.
Table 4.
Logistic regression analysis of remitters and non-remitters for major depression (n=51)
| Variables | Odds ratio | 95% CI | χ2 (df=1)a | P-value |
|---|---|---|---|---|
| Personal reserve | 1.15 | 1.02–1.31 | 7.84 | 0.03 |
| GRID-HAMD21 score at baseline | 1.17 | 1.05–1.30 | 4.97 | 0.01 |
|
| ||||
| Rejection sensitivity | 1.08 | 0.93–1.25 | 5.91 | 0.30 |
| GRID-HAMD21 score at baseline | 1.14 | 1.03–1.27 | 1.09 | 0.02 |
|
| ||||
| Self-criticism | 1.10 | 0.93–1.30 | 5.13 | 0.28 |
| GRID-HAMD21 score at baseline | 1.14 | 1.02–1.27 | 1.16 | 0.02 |
Note:
Likelihood ratio test.
Abbreviations: CI, confidence interval; GRID-HAMD21, 21-item GRID-Hamilton Depression Rating Scale.
Association between T&P constructs and the severity of depression
Among the three T&P constructs that showed associations with non-remitters in univariate analyses, moderate correlations were found between T&P construct scores and GRID-HAMD21 scores at 6 months: personal reserve (r=0.32), rejection sensitivity (r=0.30), and self-criticism (r=0.41). Similar correlations were found when we substituted the GRID-HAMD21 with the BDI-II: personal reserve (r=0.33), rejection sensitivity (r=0.34), and self-criticism (r=0.41).
Discussion
This study demonstrated that higher scores on T&P personal reserve predict poorer treatment outcome in patients with MDD. Higher levels of personal reserve, rejection sensitivity, and self-criticism were correlated with higher levels of depression. Higher levels of rejection sensitivity and self-criticism were associated with non-remitters; however, when we controlled for baseline depression severity, this relationship did not show significance. To our knowledge, this is the first prospective study that investigated the influence of the eight constructs of T&P on depression treatment outcome.
Our findings are in line with previous studies reporting that higher levels of introversion32 predicted poorer treatment outcomes and depression severity correlates positively with neuroticism.8 The neuroticism trait crossmatches with T&P self-criticism and rejection sensitivity traits, and introversion crossmatches with the T&P personal reserve trait.27 Neuroimaging studies have demonstrated that degree of introversion is associated with activations in regions of the anterior cingulate cortex, dorsolateral prefrontal cortex, middle temporal gyrus, and the amygdala.33–36 Yet, the process underlying the predictive association between personality traits and treatment outcome is not entirely clear; further understanding of lower-order dimensions and their neurobiological background may contribute to making further progress in elucidating the predictors of treatment outcome.
In our sample, T&P personal reserve scores were higher in the non-remitter group than they were in the remitter group and they correlated with measures of depression severity. Furthermore, T&P personal reserve was associated with non-remitters even after controlling for baseline depression severity. T&P personal reserve is a personality style characterized by a tendency to dislike other people getting too close at an emotional or personal level.27 Verbalizing one’s conflicts to others via interpersonal engagement is a key psychological process for addressing one’s mood; however, people who have a personal reserve personality style have been reported to have difficulty engaging with others at a deeper, emotional level.27 Interestingly, studies have shown that extraversion, an inverse personality dimension of introversion including lower-order dimensions such as T&P personal reserve, has a significant effect on the reduction of depression severity via the therapeutic alliance.37 Perhaps poorer treatment outcomes found in patients with high personal reserve may in part be explained by the effect it has on the therapeutic alliance.
T&P rejection sensitivity and self-criticism scores did not show significant associations with treatment outcome in our logistic regression analyses. However, the two T&P constructs showed association with depression severity in the univariate analysis and correlated with both objective and subjective depression severity measures (GRID-HAMD21 and BDI-II). Thus, rejection sensitivity and self-criticism may be manifestations of more severe depressive symptomatology rather than independent traits. In fact, rejection sensitivity and self-criticism showed moderate correlations with depression severity in our previous T&P validation study (r=0.35 and r=0.49, respectively).29 In addition, rejection sensitivity is one of the core symptoms of atypical depression in the DSM-IV, which is positively associated with depression severity.38,39
When we examined the association between T&P constructs and remitters/non-remitters in a subgroup of patients with moderate–severe depression, T&P personal reserve approached significance (P=0.05). Although we could not detect significant associations due to limited power, the trend association of T&P personal reserve with non-remitters found in our study suggests that this relation may also be observed in patients with moderate–severe depression.
Several limitations of this study deserve mentioning. First, this study was conducted at only two sites with a relatively small sample size, which limits the power of our analyses. However, study sites included a typical university hospital and a psychiatric hospital in an urban/suburban city in Japan. In addition, our sample had some similarities with regard to sex ratio, age, partner status, and employment status with other samples drawn from larger cohort studies such as the Netherlands Study of Depression and Anxiety.40 Second, treatment outcome was analyzed only for a 6-month period. Third, participants’ characteristics such as duration of current depressive episodes and depression severity at baseline varied.
Conclusion
Although our results are still preliminary, this study revealed that higher scores of T&P personal reserve predicted poorer treatment outcome in patients with MDD. Consequently, longer observations in naturalistic treatment settings with larger sample sizes including a wide range of demographic characteristics are required to advance our understanding of the personality factors affecting treatment outcomes.
Acknowledgments
This study was supported by JSPS KAKENHI (grant number, JP26780396). The funding source had no role in the study design; in data collection, analysis, and interpretation; in the writing of the report; or in the decision to submit the paper for publication.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.World Health Organization [webpage on the Internet] Depression. 2016. [Accessed September 7, 2016]. Available from: http://www.who.int/mediacentre/factsheets/fs369/en/
- 2.Hasin DS, Goodwin RD, Stinson FS, Grant BF. Epidemiology of major depressive disorder: results from the national epidemiologic survey on alcoholism and related conditions. Arch Gen Psychiatry. 2005;62(10):1097–1106. doi: 10.1001/archpsyc.62.10.1097. [DOI] [PubMed] [Google Scholar]
- 3.Paris J. The mistreatment of major depressive disorder. Can J Psychiatry. 2014;59(3):148–151. doi: 10.1177/070674371405900306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Klein DN, Kotov R, Bufferd SJ. Personality and depression: explanatory models and review of the evidence. Annu Rev Clin Psychol. 2011;7:269–295. doi: 10.1146/annurev-clinpsy-032210-104540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mulder RT. The influence of personality on the treatment outcome of psychopathology. World Psychiatry. 2011;10(2):115–116. [PMC free article] [PubMed] [Google Scholar]
- 6.Spek V, Nyklícek I, Cuijpers P, Pop V. Predictors of outcome of group and internet-based cognitive behavior therapy. J Affect Disord. 2008;105(1–3):137–145. doi: 10.1016/j.jad.2007.05.001. [DOI] [PubMed] [Google Scholar]
- 7.Peterson T, Bottonari K, Alpert JE, Fava M, Nierenberg AA. Use of the five-factory in characterizing patients with major depressive disorder. Compr Psychiatry. 2001;42(6):488–493. doi: 10.1053/comp.2001.27897. [DOI] [PubMed] [Google Scholar]
- 8.Farmer A, Redman K, Harris T, et al. Neuroticism, extraversion, life events and depression. The Cardiff Depression Study. Br J Psychiatry. 2002;181:118–122. doi: 10.1017/s0007125000161823. [DOI] [PubMed] [Google Scholar]
- 9.Koorevaar AM, Comijs HC, Dhondt AD, et al. Big Five personality and depression diagnosis, severity and age of onset in older adults. J Affect Disord. 2013;151(1):178–185. doi: 10.1016/j.jad.2013.05.075. [DOI] [PubMed] [Google Scholar]
- 10.Steffens DC, McQuid DR, Smoski MJ, Potter GG. Clinical outcomes of older depressed patients with and without comorbid neuroticism. Int Psychogeriatr. 2013;25(12):1985–1990. doi: 10.1017/S1041610213001324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mulder RT, Frampton CM, Luty SE, Joyce PR. Eighteen months of drug treatment for depression: predicting relapse and recovery. J Affect Disord. 2009;114(1–3):263–270. doi: 10.1016/j.jad.2008.08.002. [DOI] [PubMed] [Google Scholar]
- 12.Duggan CF, Lee AS, Murray RM. Does personality predict long-term outcome in depression? Br J Psychiatry. 1990;157:19–24. doi: 10.1192/bjp.157.1.19. [DOI] [PubMed] [Google Scholar]
- 13.Parker G, Roy K. Examining the utility of temperament model for modelling non-melancholic depression. Acta Psychiatr Scand. 2002;106(1):54–61. doi: 10.1034/j.1600-0447.2002.02357.x. [DOI] [PubMed] [Google Scholar]
- 14.Parker G, Manicavasagar V, Crawford J, Tully L, Gladstone G. Assessing personality traits associated with depression: the utility of tiered model. Psychol Med. 2006;36(8):1131–1139. doi: 10.1017/S0033291706007562. [DOI] [PubMed] [Google Scholar]
- 15.Spanemberg L, Caldieraro MA, Vares EA, et al. Biological differences between melancholic and nonmelancholic depression subtyped by the CORE measure. Neuropsychiatr Dis Treat. 2014;10:1523–1531. doi: 10.2147/NDT.S66504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.First MB, Spitzer RT, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV=TR Axis I Disorders-Patient Edition (SCID-I/P1/2007 revision) New York, NY: Biometrics Research Department; 2007. [Google Scholar]
- 17.Williams JB, Kobak KA, Bech P, et al. The GRID-HAMD: standardization of the Hamilton Depression Rating Scale. Int Clin Psychopharmacol. 2008;23(3):120–129. doi: 10.1097/YIC.0b013e3282f948f5. [DOI] [PubMed] [Google Scholar]
- 18.Tabuse H, Kalali A, Azuma H, et al. The new GRID Hamilton Rating Scale for depression demonstrates excellent inter-rater reliability for inexperienced and experienced raters before and after training. Psychiatry Res. 2007;153(1):61–67. doi: 10.1016/j.psychres.2006.07.004. [DOI] [PubMed] [Google Scholar]
- 19.Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961;4:561–571. doi: 10.1001/archpsyc.1961.01710120031004. [DOI] [PubMed] [Google Scholar]
- 20.Hiroe T, Kojima M, Yamamoto I, et al. Gradations of clinical severity and sensitivity to change assessed with the Beck Depression Inventory-II in Japanese patients with depression. Psychiatry Res. 2005;135(3):229–235. doi: 10.1016/j.psychres.2004.03.014. [DOI] [PubMed] [Google Scholar]
- 21.Rush AJ, Trivedi MH, Ibrahim HM, et al. The 16-item quick inventory of depressive symptomatology (QIDS), clinician rating (QIDS-C), and self-report (QIDS-SR): a psychometric evaluation in patients with chronic major depression. Biol Psychiatry. 2003;54(5):573–583. doi: 10.1016/s0006-3223(02)01866-8. [DOI] [PubMed] [Google Scholar]
- 22.Fujisawa D, Nakagawa A, Tajima M, et al. Cross-cultural adaptation of the quick inventory of depressive symptomatology-self report (QIDS-SR-J) Jpn J Stress Sci. 2010;25(1):43–52. [Google Scholar]
- 23.Sheehan DV. Sheehan Disability Scale. In: Rush AJ, First MB, Blacker D, editors. Handbook of Psychiatric Measures. 2nd ed. Washington, DC: American Psychiatric Publishing; 2008. pp. 100–102. [Google Scholar]
- 24.Yoshida T, Otubo T, Tsuchida H, Wada Y, Kamijima K, Hukui K. Reliability and validity of the Sheehan Disability Scale-Japanese version. Rinsho Seishin Yakuri. 2004;7(10):1645–1653. [Google Scholar]
- 25.Riedel M, Möller HJ, Obermeier M, et al. Response and remission criteria in major depression – a validation of current practice. J Psychiatr Res. 2010;44(15):1063–1068. doi: 10.1016/j.jpsychires.2010.03.006. [DOI] [PubMed] [Google Scholar]
- 26.The Black Dog Institute [webpage on the Internet] Temperament and Personality (T&P) Questionnaire. [Accessed February 4, 2013]. Available from: http://www.blackdoginstitute.org.au/public/research/researchtools.cfm.
- 27.Parker G, Manicavasagar V. Modelling and Managing the Depressive Disorders: A Clinical Guide. Cambridge: Cambridge University Press; 2005. [Google Scholar]
- 28.McCrae RR, Costa PT., Jr Validation of the five-factor model of personality across instruments and observers. J Pers Soc Psychol. 1987;52(1):81–90. doi: 10.1037//0022-3514.52.1.81. [DOI] [PubMed] [Google Scholar]
- 29.Kudo Y, Nakagawa A, Tamura N, et al. The reliability and validity of the Japanese version of the Temperament and Personality Questionnaire for patients with non-melancholic depression. J Affect Disord. 2016;198:237–241. doi: 10.1016/j.jad.2016.03.046. [DOI] [PubMed] [Google Scholar]
- 30.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zimmerman M, Martinez JH, Young D, Chelminski I, Dalrymple K. Severity classification on the Hamilton Depression Rating Scale. J Affect Disord. 2013;150(2):384–388. doi: 10.1016/j.jad.2013.04.028. [DOI] [PubMed] [Google Scholar]
- 32.Quilty LC, De Fruyt F, Rolland JP, Kennedy SH, Rouillon PF, Bagby RM. Dimensional personality traits and treatment outcome in patients with major depressive disorder. J Affect Disord. 2008;108(3):241–250. doi: 10.1016/j.jad.2007.10.022. [DOI] [PubMed] [Google Scholar]
- 33.Lei X, Yang T, Wu T. Functional neuroimaging of extraversion-introversion. Neurosci Bull. 2015;31(6):663–675. doi: 10.1007/s12264-015-1565-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Eisenberger NI, Lieberman MD, Satpute AB. Personality from a controlled processing perspective: an fMRI study of neuroticism, extraversion, and self-consciousness. Cogn Affect Behav Neurosci. 2005;5(2):169–181. doi: 10.3758/cabn.5.2.169. [DOI] [PubMed] [Google Scholar]
- 35.Kumari V, Ffytche DH, Williams SC, Gray JA. Personality predicts brain responses to cognitive demands. J Neurosci. 2004;24(47):10636–10641. doi: 10.1523/JNEUROSCI.3206-04.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Suslow T, Kugel H, Reber H, et al. Automatic brain response to facial emotion as a function of implicitly and explicitly measured extraversion. Neuroscience. 2010;167(1):111–123. doi: 10.1016/j.neuroscience.2010.01.038. [DOI] [PubMed] [Google Scholar]
- 37.Kushner SC, Quilty LC, Uliaszek AA, McBride C, Bagby RM. Therapeutic alliance mediates the association between personality and treatment outcome in patients with major depressive disorder. J Affect Disord. 2016;201:137–144. doi: 10.1016/j.jad.2016.05.016. [DOI] [PubMed] [Google Scholar]
- 38.Singh T, Williams K. Atypical depression. Psychiatry (Edgmont) 2006;3(4):33–39. [PMC free article] [PubMed] [Google Scholar]
- 39.Postermak MA, Zimmerman M. Symptoms of atypical depression. Psychiatry Res. 2001;104(2):175–181. doi: 10.1016/s0165-1781(01)00301-8. [DOI] [PubMed] [Google Scholar]
- 40.Schuch JJ, Roest AM, Nolen WA, Penninx BW, de Jonge P. Gender differences in major depressive disorder: results from the Netherlands study of depression and anxiety. J Affect Disord. 2014;156:156–163. doi: 10.1016/j.jad.2013.12.011. [DOI] [PubMed] [Google Scholar]