Abstract
Objective
Excess weight is a known risk factor for functional limitation and common in adults with knee osteoarthritis (OA). We asked to what extent high waist circumference was linked with developing difficulty with walking speed and distance over 4 years in adults with or at risk of knee OA.
Method
Using data from the Osteoarthritis Initiative, we employed WHO categories for Body Mass Index (BMI) and waist circumference (small/medium and large). Difficulty with speed was defined by slow gait: < 1.2 m/s during a 20-meter walk, and difficulty with distance was defined by an inability to walk 400 meters. We calculated risk ratios (RR) to examine the likelihood of developing difficulty with distance and speed using obesity and waist circumference as predictors with RRs adjusted for potential confounders (i.e., age, sex, race, education, physical activity, and OA status).
Results
Participants with obesity and large waists were 2.2 times more likely to have difficulty with speed at 4 years compared to healthy weight and small/medium waisted participants (Adjusted RR 2.2 [95% Confidence interval (CI) 1.6, 3.1], P < .0001). Participants with obesity and a large waist circumference had 2.4 times the risk of developing the inability to walk 400 meters compared with those with a healthy BMI and small/medium waist circumference (Adjusted RR 0.9 [95% CI 1.6, 3.7], P < .0001).
Conclusions
Waist circumference may be a main risk factor for developing difficulty with speed in adults with or at risk of knee OA.
Keywords: gait, obesity, walking, body mass index, osteoarthritis, waist circumference
Introduction
Knee osteoarthritis (OA) is the most common cause of functional limitation1–4 such as difficulty walking5. Obesity is a well-known risk factor for both knee OA1 and functional limitation4. The presence of obesity in adults with or at risk of knee OA engenders a vicious cycle wherein the development of walking difficulty restricts participation in activities of daily living, such as grocery shopping, leading to reduced physical activity, increased weight gain, and potentially incident or worsening of existing knee OA. Specifically, obesity has an effect on walking biomechanics and bioenergetics that affects the knee joint and gait patterns. Adults with obese BMI exhibit reduced range of motion at the ankle, knee, and hip during walking6. They also demonstrate greater absolute ground reaction forces7 and increased load at the knee8 when walking faster than their preferred speed compared to normal weight adults. Obesity also increases the energy cost of walking when walking at different, imposed stride frequencies9. These gait differences, particularly slower preferred walking speeds, can be attributed to an attempt to increase stability10, to minimize mechanical external work11, to decrease load at the knee12, and to curb energy cost and relative effort7.
Little is known about whether the distribution of weight is a relevant risk factor for difficulty walking in adults with or at risk of knee OA. From a biomechanical perspective, excess waist circumference limits postural stability in adults due to an anterior shift in the center of mass13 and is associated with slowing gait speed in adults14. Therefore, the distribution of body mass (as captured by waist circumference due to central adiposity in the abdominal area) may be associated with difficulty walking above and beyond the effects imposed by the overall mass, i.e., obesity, and additionally impact difficulty walking in adults with or at risk of knee OA. At present, the extent to which waist circumference is associated with the development of walking difficulty independent of obesity is not known. This is an important gap to fill in order to better tailor treatments targeted to individuals with or at risk of knee OA who have various BMI and waist circumference measures.
We are particularly interested in studying walking speed and distance because these functional abilities may be the first to change noticeably if patients develop difficulty with motor function. Both walking speed and endurance are important elements contributing to the ability to walk in the community. Existing evidence demonstrates that limited walking speed and endurance can hinder an individual’s ability to navigate in the community15,16. For instance, a speed of ≥ 1.2 meters/second (m/s), is the minimum speed necessary to cross a timed cross walk17. Moreover, the ability to walk at least 400 meters is associated with independence with walking in the community18,19. Other motor difficulties such as rising from a chair may appear later. Therefore, it may be beneficial for clinicians to monitor changes in speed and distance prior to patients with or at risk of knee OA developing further motor difficulties.
We investigated to what extent high waist circumference was associated with the development of difficulty in walking speed (1.2 m/s) and distance (400 meters) over four years in a well- established cohort of adults with or at risk of knee OA. Given the strong existing associations between overall body mass and the development of knee osteoarthritis20, we hypothesized that overall body mass rather than the distribution of body mass would be the driving factor in predicting functional limitations for adults.
Method
Study Sample
We used data from the Osteoarthritis Initiative (OAI), which includes adults aged 45 to 79 years old who have been followed annually for the development or progression of OA since the initial enrollment period in 2004. OAI has four clinical recruitment sites: Baltimore, Maryland; Columbus, Ohio; Pittsburgh, Pennsylvania and Pawtucket, Rhode Island. Specific information about the OAI objectives and protocols are located online (http://www.oai.ucsf.edu/datarelease/About.asp). OAI recruited two primary subcohorts: one with symptomatic knee OA at baseline that was followed for worsening of disease (the Progression subcohort), and another without symptomatic knee OA, but selected on the basis of having specific characteristics which give them an increased risk of developing incident symptomatic knee OA during the study (the Incidence subcohort). For the current study, we used data from the baseline OAI visit and the Year 4 study visit from subjects in both the incidence and progression cohorts. All OAI sites received Institutional Review Board approval.
Study Outcomes
We examined two different aspects of walking: speed from a 20-meter walk and distance from a 400-meter walk test. For both tests, participants were instructed to walk at a usual pace from a starting point to an orange cone 20 meters away. For the 20-meter walk, participants walked the course once and for the 400-meter walk, participants performed 20 lengths of the course. Timing for the 20-meter walk started with the first step after the starting line and ended after the first step over the finishing line using a stopwatch.
We employed two definitions of difficulty walking: speed and distance. We defined limited walking speed as a gait speed < 1.2 meters/second (m/s) during the 20-meter walk test at the four year follow-up among study participants walking ≥ 1.2 m/s at baseline21. A speed ≥ 1.2 meters/second (m/s) is necessary to cross a timed cross walk17.
We defined difficulty with walking distance as not completing the 400-meter walk at the four year follow-up among study participants completing the 400-meter walk at baseline. Participants were not eligible to attempt the 400-meter walk if they did not complete the 20-meter walk, had a heart rate < 40 or > 110 beats per minute, had a systolic or diastolic blood pressure exceeding 180 mmHg or 100 mmHg, respectively, required a walker or quad cane to ambulate, called a doctor within the past 3 months for worsening chest pain or shortness of breath, were hospitalized in the past 3 months, or did not feel safe to perform the test. Study participants were allowed to take as many breaks as needed, but received a maximum of 15 minutes in which to complete the task.
Study Exposures
Body Mass Index (BMI) was computed from standardized weight and height assessments. Abdominal circumference was measured at the level of the umbilicus between the lower rib and the iliac crest. BMI and waist circumference were classified based on World Health Organization (WHO) health risk categories22. BMI was classified as: normal weight=BMI < 25 kg/m2, overweight=BMI ≥ 25 kg/m2 and < 30 kg/m2, and obesity=BMI ≥ 30 kg/m2. Waist circumference categories are: small circumference (men: ≤ 93.9 cm; women: ≤ 79.9 cm), medium circumference (men: ≥ 94 cm and < 101.9 cm; women: ≥ 80 cm and < 87.9 cm), and large circumference (men: ≥ 102 cm; women: ≥ 88 cm).
Potential Confounders
The following baseline factors were considered as potential confounders based on existing literature linking them to function: age23, sex (men/women)24, race (White, other)25, education (some college/< high School)26, and self-reported physical activity (Physical Activity Scale of the Elderly)27. We also employed disease status as a potential confounder defined as no radiographic knee osteoarthritis (ROA), presence of ROA, or the presence of symptomatic knee OA, i.e., the presence of ROA and knee pain (Table 1). This definition has been previously employed in the literature28,29. ROA was assessed from weight-bearing posteroanterior and lateral fixed flexion radiographic evaluations of both knees30. Radiographs were independently graded twice among three expert readers (two rheumatologists and a musculoskeletal radiologist) for joint space narrowing and osteophytes in the tibiofemoral joint according to Kellgren and Lawrence K/L criteria (grades 0–4)31. Any disagreements were adjudicated among all three expert readers to reach consensus. There was high agreement between readers with kappa statistics ranging from 0.70 to 0.80 for K/L grades. We defined the presence of ROA as a K/L grade ≥ 2. Knee joint radiography for the OAI focused on an assessment of the tibiofemoral joint, and patients with patellofemoral joint involvement were not included in the progression cohort. Knee pain (absent/present) was evaluated by asking participants if they had pain, aching, or stiffness in or around each knee on most days for at least one month within the past year. Since cardiovascular disease32 and diabetes33 are likely mediators in the causal pathway between excess weight and function limitations, we did not adjust for these factors34–36.
Table 1.
Sample characteristics by those included and not included in analyses. Standard deviations are in parentheses and minimum and maximum values are in brackets.
| Community speed as outcome |
Community distance as outcome | |||
|---|---|---|---|---|
| Included (n= 2,646) |
No gait speed 4 years later (n=680) |
Included (n=3460) |
No 400m walk 4 years later (n=1041) |
|
| Age (years) [mean (sd) Min, max] |
60.2 (8.8) [45, 79] |
61.0 (9.1) [45, 79] |
61.1 (9.0) [45, 79] |
61.6 (9.5) [45, 79] |
| BMI (kg/m2) [mean (sd) Min, max] |
28.2 (4.5) [17.6, 45.4] |
28.6 (4.5) [16.9, 47.7] |
28.7 (4.7) [17.6, 48.7] |
28.5 (5.0) [16.9, 47.7] |
| Sex (% Men) | 46.2 | 41.2 | 43.2 | 37.5 |
| Race (% White) | 86.9 | 77.2 | 82.3 | 72.3 |
| Education (% College) | 68.1 | 55.3 | 63.5 | 50.2 |
| Physical Activity Scale of the Elderly [mean (sd) Min, max] |
173.5 (82.1) [0, 526.0] |
160.6 (80.8) [0, 454.0] |
165.1 (81.3) [0, 504.0] |
151.3 (82.6) [0, 516.0] |
| Radiographic OA (%) | 26.0 | 23.1 | 25.9 | 21.8 |
| Symptomatic OA (%) | 26.1 | 32.1 | 29.5 | 34.6 |
Statistical Analyses
Our primary aim was to examine the association of obesity and waist circumference with the risk of developing difficulty with walking four years later. Our study outcomes were the ability to complete the 400-meter walk and the ability to walk at least 1.2 m/s as dichotomous outcomes. We calculated risk to determine the probability of developing difficulty with walking in comparison to a reference group: individuals with normal BMI and small or medium waist circumference. The reference group serves as a control group in risk computations. To examine the association of BMI and waist circumference with study outcomes, we calculated unadjusted risk ratios (RR) and RR adjusted for potential confounders using Poisson regression models with robust error variance29. Specifically, we used PROC genmod with a Poisson distribution and a log-link function in SAS 9.3 (Cary, NC) to calculate RR and 95% Confidence Intervals37.
When interpreting RRs, if no differences exist between groups in terms of the risk of developing difficulty with walking, then RR=1. An RR < 1 would mean that developing difficulty with walking would be less likely in the comparison group than in the reference group. An RR > 1 would mean that developing difficulty with walking would be more likely in the comparison group than in the reference group. We report RRs along with confidence intervals. Confidence intervals that do not include a value of 1 are considered to represent statistically significant comparisons, and confidence intervals that include a value of 1 represent comparisons that are not significant.
We evaluated the association of BMI and waist circumference at baseline with our dependent variables. BMI and waist circumference were classified as follows: normal BMI and small or medium waist circumference, normal BMI and large waist circumference, overweight BMI and small or medium waist circumference, overweight BMI and large waist circumference, obese BMI and small or medium risk waist circumference, and obese BMI and large waist circumference.
We conducted sensitivity analyses and repeated all analyses restricting our sample to those with ROA at baseline to investigate if our study findings apply specifically to people with ROA37. Our sample size was 2,646 and 3,460 for gait speed and walking endurance as study outcomes, respectively. Restricting our sample for the sensitivity analysis reduced our sample size to 1,909 and 2,579, respectively, for these outcomes.
Results
Sample Characteristics
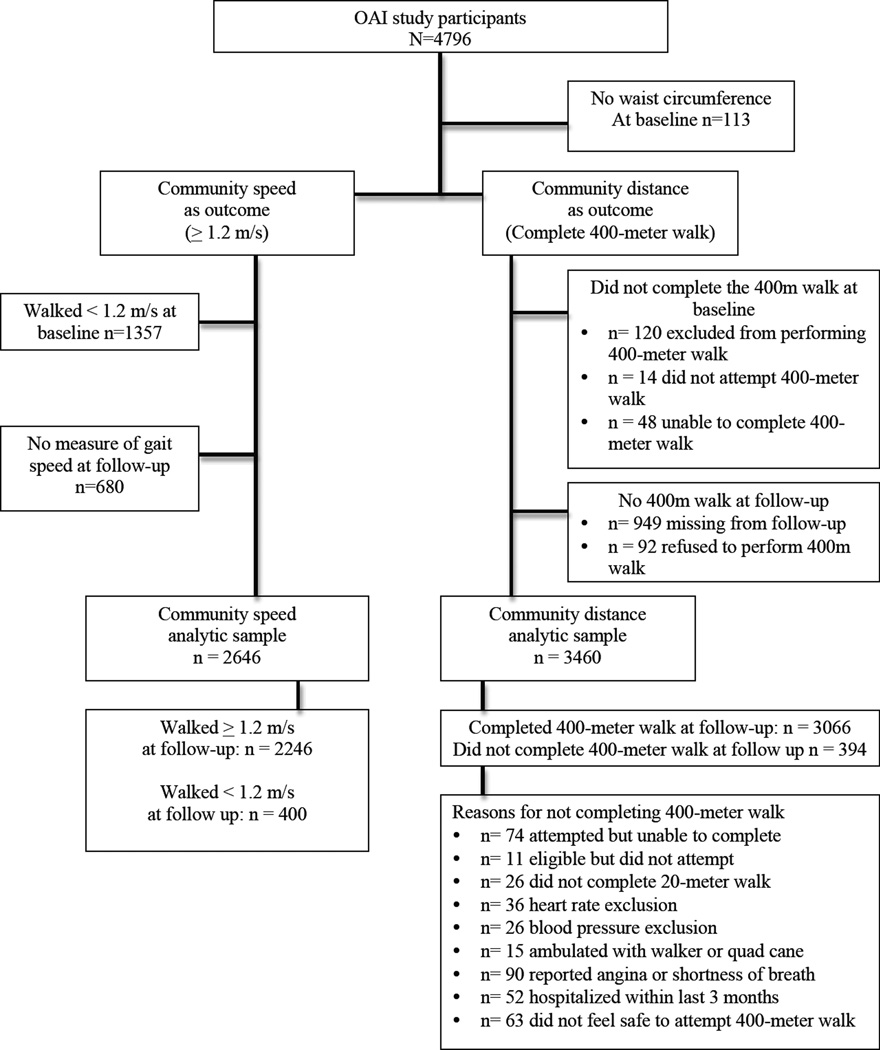
Of the 4,796 study participants in OAI, 113 did not have waist circumference recorded at baseline. For speed as a study outcome, at follow up, 20% did not have measures of gait speed (680/3,326) resulting in an analytic sample of 2,646 (Figure 1). The average age (SD) of our gait speed sample was 60.2 years old (8.8), 46.2% were men, and 68.1% had at least some college education (Table 1). For distance as outcome, at follow up, 23% did not have measures of distance (1,041/4,501) resulting in an analytic sample of 3,460 (Figure 1). The average age was 61.1 (9.0), 43.2% were men, and 63.5% had at least some college education for distance as outcome. Those included in our analytic datasets were more likely to have more education and physical activity, were more likely to be White, and not have ROA or symptomatic OA compared with those not included (Table 1).
Figure 1. Flow diagram analytic samples selection for study outcomes from the OAI.
Description of the number of participants who contributed distance (400 meters) and speed (1.2 m/s) data accounting for inclusion/exclusion criteria and missing data.
Ability to walk 1.2 m/s
Among the 2,646 participants walking 1.2 m/s at baseline, 15.1% were unable to walk 1.2 m/s by the four-year follow-up. Greater BMI and waist circumference at baseline were associated with increased risk of developing the inability to walk 1.2 m/s in separate models (Supplemental table 1). Compared to the reference group, overweight and obese adults with small/medium waist circumference had the same likelihood as the reference group in developing difficulty walking 1.2 m/s. In contrast, overweight and obese adults with large waist circumference had a 1.5 and 2.2 chance of developing an inability to walk 1.2 m/s respectively (Table 2).
Table 2.
Association of BMI categories with inability to walk at 1.2 m/s. Risk Ratios are shown with 95% confidence intervals (CI) in brackets, and p-values beneath.
| BMI Category | BMI (kg/m2) Mean (sd) |
% (n/N) incident inability to walk 1.2 m/s |
Unadjusted Risk Ratio [95% CI] |
Adjusted* Risk Ratio [95% CI] |
|---|---|---|---|---|
| BMI ≥ 19 and < 25 kg/m2 and Waist WHO** category 1 or 2 |
22.6 (1.7) | 8.4 (35/415) | 1.0*** | 1.0*** |
| BMI < 25 kg/m2 and Waist WHO** category 3 |
23.2 (1.3) | 14.0 (39/279) | 1.7 [1.1, 2.5] P = .02 |
1.2 [0.8, 1.8] P = .62 |
| BMI ≥25 and < 30 kg/m2 and Waist WHO** category 1 or 2 |
26.8 (1.3) | 8.5 (36/426) | 1.0 [0.6, 1.6] P = .99 |
1.0[0.6, 1.6] 2.0 P = .93 |
| BMI ≥25 and < 30 kg/m2 and Waist WHO** category 3 |
27.7 (1.5) | 17.1 (118/689) | 2.0 [1.4, 2.9] P < .0001 |
1.5 [1.1, 2.1] P = .03 |
| BMI ≥ 30 kg/m2 and Waist WHO** category 1 or 2 |
31.2 (1.3) | 6.5 (2/31) | 0.8 [0.2, 3.0] P = .70 |
0.9 [0.2, 3.7] P = .93 |
| BMI ≥ 30 kg/m2 and Waist WHO** category 3 |
33.4 (2.9) | 21.1 (170/806) | 2.5 [1.8, 3.5] P < .0001 |
2.2 [1.6, 3.1] P < .0001 |
Adjusted for age, sex, education, race, physical activity, and symptomatic knee osteoarthritis.
Waist World Health Organization category 1=small (men: ≤ 93.9 cm; women: ≤ 79.9 cm), 2=medium (men: ≥ 94 cm and < 101.9 cm; women: ≥ 80 cm and < 87.9 cm), and 3=large circumference (men: ≥ 102 cm; women: ≥ 88 cm).
The first BMI category is the reference group. Therefore, these risk ratios =1.
Ability to walk 400 meters
Of the 3,460 study participants able to complete the 400-meter walk at baseline, 394 were unable to complete the test at the four-year follow-up. Reasons for not completing the 400-meter walk are detailed in Figure 1. Greater BMI and waist circumference at baseline were associated with increased risk of developing the inability to walk 400 meters in separate models (Supplemental table 2). In the combined model, increasing waist circumference and BMI were both associated with greater risk of incident inability to walk 400 meters (Table 3). For instance, among study participants who were obese, those with a large waist circumference had 2.4 times the risk of developing the inability to walk 400 meters compared with those with a healthy BMI and small/medium waist circumference.
Table 3.
Association of BMI categories with incident inability to walk 400 meters. Risk Ratios are shown with 95% confidence intervals (CI) in brackets, and p-values beneath.
| BMI Category | BMI (kg/m2) Mean (sd) |
% (n/N) incident inability to walk 400 meters |
Unadjusted Risk Ratio [95% CI] |
Adjusted* Risk Ratio [95% CI] |
|---|---|---|---|---|
| BMI < 25 kg/m2 and Waist WHO** category 1 or 2 |
22.6 (1.7) | 5.5 (26/476) | 1.0*** | 1.0*** |
|
BMI < 25 kg/m2 and Waist WHO** category 3 |
23.1 (1.3) | 9.7 (33/339) | 1.8 [1.1, 2.9] P = .02 |
1.3 [0.8, 2.2] P = .35 |
| BMI ≥25 and < 30 kg/m2 and Waist WHO** category 1 or 2 |
26.9 (1.3) | 8.3 (41/494) | 1.5 [0.9, 2.4] P = .08 |
1.5 [0.9, 2.4] P =.14 |
| BMI ≥25 and < 30 kg/m2 and Waist WHO** category 3 |
27.7 (1.5) | 11.9 (108/905) | 2.2 [1.4, 3.3] P =.0002 |
1.6 [1.1, 2.5] P =.02 |
| BMI ≥ 30 kg/m2 and Waist WHO** category 1 or 2 |
31.0 (1.1) | 10.0 (4/40) | 1.8 [0.7, 5] P =.25 |
1.9 [0.7, 5.1] P = .21 |
| BMI ≥ 30 kg/m2 and Waist WHO** category 3 |
33.7 (3.0) | 15.1 (182/1206) | 2.8 [1.9, 4.1] P < .0001 |
2.4 [1.6, 3.7] P < .0001 |
Adjusted for age, sex, education, race, physical activity, and symptomatic knee osteoarthritis.
Waist World Health Organization category 1=small (men: ≤ 93.9 cm; women: ≤ 79.9 cm), 2=medium (men: ≥ 94 cm and < 101.9 cm; women: ≥ 80 cm and < 87.9 cm), and 3=large circumference (men: ≥ 102 cm; women: ≥ 88 cm).
The first BMI category is the reference group. Therefore, these risk ratios =1.
Restricting our sample to those with radiographic knee OA at baseline did not change our effect estimates materially (Supplemental table 3).
Discussion
We found that waist circumference in addition to obesity was associated with the development of difficulty with walking speed and distance four years later. The distribution of mass more so than overall mass may be a risk factor for the development of difficulty walking at a speed and distance necessary for the community among adults with or at risk of knee OA.
These findings align with known medical concerns about excessive abdominal mass38. Excess body mass distribution in the abdominal area is associated with illnesses such as cardiovascular disease39 and type 2 diabetes mellitus (T2DM)40. With the health risks associated with body fat distribution, our finding of decreased functional limitations with increased waist circumference is notable. The addition of our finding to the other deleterious effects of excess abdominal mass builds a profile of risks associated with body fat distribution. Increased knowledge about the collective, harmful effects of excess abdominal mass can help in identifying and treating patients with increased health risks.
The distribution of body mass measured by waist circumference has not been a main focus on research examining functional limitation or gait. Most biomechanical research on gait and obesity finds that obesity is associated with impaired gait and subsequent limitation in function2–4,7,41,42. Specifically, compared to normal weight adults without knee OA, adults with obese BMI walk more slowly with decreased walking velocities, expend more energy and relative effort when walking7, and use more mechanical external work12. An overall higher BMI increases loading on the knee43–45, which exacerbates pain and gait deficits in those with knee OA46,47. Consequently, the lifetime risk of knee OA doubles with high body mass (i.e., an obese BMI)48. However, previous studies show that waist circumference is also associated with atypical walking patterns (i.e., decreased walking endurance and slow walking speed) in adults with knee OA49. Higher waist circumference predicts a decline in walking speed in adults aged 55 to 74 years old14. Some research has also implicated excess abdominal mass with reduced postural stability13. Continued loading on the knee and the anterior shift in the center of mass can contribute to the rate of disease progression (i.e., increase the rate) and have large effects on patients’ functional performance. Therefore, our finding that waist circumference may be associated with difficulty walking speed and distance is highly relevant for adults with knee OA. Our results suggest that future research on gait and obesity from a biomechanical perspective would benefit from considering body mass distribution as a main factor. Including waist circumference as a possible variable would augment our knowledge of how body mass distribution influences function.
We acknowledge that there are some limitations to our study. First, additional measures of functional performance were not available in the current dataset. It would be beneficial to gather prospective, longitudinal data that includes other measures of motor function in adults with obesity (e.g., timed stair climbing). Although only the 20- and 400-meter walks were available to capture changes in speed and distance, the fact that we did find declines in function using these basic measures is notable. Our findings imply that even basic measures of speed and distance applied commonly in clinical practice can be used to examine the effects of obesity and body mass distribution on function over time. Second, our data were not explicitly linked to patients that developed OA. Future studies are needed to examine how functional limitation relates to whether patients develop OA. If they do develop knee OA, more information would also be needed on how the location in the knee joint in which OA was developed and the severity of the disease impact functional limitation. Third, there were strict eligibility criteria to attempt the 400-meter walk and it is possible that some study participants may have been able to complete the test if allowed. We reran the analyses not including study participants who were classified as not completing the 400-meter walk due to restrictions related to heart rate, blood pressure, walker use, angina, and hospitalization. The effect estimates were similar to the primary analysis. Fourth, there is a possibility of residual confounding from BMI within each BMI/waist circumference exposure category. We reran the analyses also adjusting for baseline BMI, and found attenuated effect estimates. However, the trends of the data remained; those with large waist circumference had higher risk than those with small/medium waist circumference within each BMI WHO category.
Conclusion
In conclusion, we found that waist circumference was associated with the development of difficulty with walking a speed of at least 1.2 m/s and distance of at least 400 meters over four years among adults with or at risk of knee OA. These findings may suggest that measuring waist circumference in research and in clinical practice may be important to better stratify the risk of developing difficulty with walking among adults with or at risk of knee OA.
Supplementary Material
Acknowledgments
The OAI is a public–private partnership composed of five contracts (N01-AR-2-2258; N01-AR-2-2259; N01-AR-2-2260; N01-AR-2-2261; N01-AR-2-2262) funded by the National Institutes of Health (NIH), a branch of the Department of Health and Human Services, and conducted by the OAI Study Investigators. Private funding partners include Merck Research Laboratories, Novartis Pharmaceuticals Corporation, GlaxoSmithKline, and Pfizer, Inc. Private sector funding for the OAI is managed by the Foundation for the NIH. This manuscript was prepared using an OAI public use dataset and does not necessarily reflect the opinions or views of the OAI investigators, the NIH, or the private funding partners.
Funding
This research was supported in part by an NIH grants K12HD055931 and R03AR066344-01A1 to Simone V. Gill and NIH U54 GM104941 and K12HD055931 to Daniel K. White.
The funders of this manuscript did not have any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
We sincerely thank the Motor Development Laboratory and Dr. Thomas G. Travison for reading an earlier draft of this manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Author Contributions
SG and DW had full access to all of the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. SG and DW: study concept and design. SG, DW, YZ, JN, GH, and CA: analysis and interpretation of data. SG and DW: drafting of the manuscript. SG, DW, YZ, JN, GH, and CA: critical revision of the manuscript for important intellectual content. DW, YZ, and JN: statistical analysis. SG: obtained funding. SG, DW, YZ, JN, GH, and CA: administrative, technical, or material support. SG, DW, YZ, JN, GH, and CA: final approval for the version to be published.
Ethical Approval
The study was conducted according to the declaration of Helsinki and All OAI sites received Institutional Review Board approval. All the patients gave informed written consent.
Conflict of Interest Disclosures
All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author).
All authors declare no conflicts of interest.
References
- 1.Himes CL. Obesity, disease, and functional limitation in later life. Demography. 2000;37(1):73–82. [PubMed] [Google Scholar]
- 2.Hung YC, Gill SV, Meredith GS. Influence of dual task constraints on whole body organization during walking in overweight and obese children. American Journal of Physical Medicine and Rehabilitation. 2013;92:461–467. doi: 10.1097/PHM.0b013e31828cd59d. [DOI] [PubMed] [Google Scholar]
- 3.Gill SV. Optimising motor adaptation in childhood obesity. Australian occupational therapy journal. 2011;58(5):386–389. doi: 10.1111/j.1440-1630.2011.00957.x. [DOI] [PubMed] [Google Scholar]
- 4.Forhan M, Gill SV. Obesity, functional mobility, and quality of life. Best Practice and Research: Clinical Endocrinology & Metabolism. 2013;27:129–137. doi: 10.1016/j.beem.2013.01.003. [DOI] [PubMed] [Google Scholar]
- 5.White DK, Niu J, Zhang Y. Is symptomatic knee osteoarthritis a risk factor for a trajectory of fast decline in gait speed? Results from a longitudinal cohort study. Arthritis care & research. 2013;65(2):187–194. doi: 10.1002/acr.21816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hills AP, Hennig EM, Byrne NM, Steele JR. The biomechanics of adiposity--structural and functional limitations of obesity and implications for movement. Obesity reviews : an official journal of the International Association for the Study of Obesity. 2002;3(1):35–43. doi: 10.1046/j.1467-789x.2002.00054.x. [DOI] [PubMed] [Google Scholar]
- 7.Browning RC, Kram R. Effects of obesity on the biomechanics of walking at different speeds. Medicine and science in sports and exercise. 2007;39(9):1632–1641. doi: 10.1249/mss.0b013e318076b54b. [DOI] [PubMed] [Google Scholar]
- 8.Peyrot N. Biomechanical constraints associated with walking in obese individuals. Physical Therapy Reviews. 2012;17(5):352–353. [Google Scholar]
- 9.Delextrat A, Matthew D, Cohen DD, Brisswalter J. Effect of stride frequency on the energy cost of walking in obese teenagers. Human movement science. 2011;30(1):115–124. doi: 10.1016/j.humov.2010.10.004. [DOI] [PubMed] [Google Scholar]
- 10.Singh D, Park W, Levy MS, Jung ES. The effects of obesity and standing time on postural sway during prolonged quiet standing. Ergonomics. 2009;52(8):977–986. doi: 10.1080/00140130902777636. [DOI] [PubMed] [Google Scholar]
- 11.Malatesta D, Vismara L, Menegoni F, Galli M, Romei M, Capodaglio P. Mechanical external work and recovery at preferred walking speed in obese subjects. Medicine and science in sports and exercise. 2009;41(2):426–434. doi: 10.1249/MSS.0b013e31818606e7. [DOI] [PubMed] [Google Scholar]
- 12.Peyrot N, Morin JB, Thivel D, et al. Mechanical work and metabolic cost of walking after weight loss in obese adolescents. Medicine and science in sports and exercise. 2010;42(10):1914–1922. doi: 10.1249/MSS.0b013e3181da8d1e. [DOI] [PubMed] [Google Scholar]
- 13.Corbeil P, Simoneau M, Rancourt D, Tremblay A, Teasdale N. Increased risk for falling associated with obesity: mathematical modeling of postural control. IEEE transactions on neural systems and rehabilitation engineering : a publication of the IEEE Engineering in Medicine and Biology Society. 2001;9(2):126–136. doi: 10.1109/7333.928572. [DOI] [PubMed] [Google Scholar]
- 14.Angleman SB, Harris TB, Melzer D. The role of waist circumference in predicting disability in periretirement age adults. Int J Obes (Lond) 2006;30(2):364–373. doi: 10.1038/sj.ijo.0803130. [DOI] [PubMed] [Google Scholar]
- 15.Gill SV, Narain A. Quantifying the Effects of Body Mass Index on Safety: Reliability of a Video Coding Procedure and Utility of a Rhythmic Walking Task. Archives of physical medicine and rehabilitation. 2012;93:728–730. doi: 10.1016/j.apmr.2011.09.012. [DOI] [PubMed] [Google Scholar]
- 16.Gill SV, Hung YC. Influence of weight classification on children stepping over obstacles. American Journal of Physical Medicine and Rehabilitation. 2012;91:625–630. doi: 10.1097/PHM.0b013e31824fa81e. [DOI] [PubMed] [Google Scholar]
- 17.Langlois JA, Keyl PM, Guralnik JM, Foley DJ, Marottoli RA, Wallace RB. Characteristics of older pedestrians who have difficulty crossing the street. American journal of public health. 1997;87(3):393–397. doi: 10.2105/ajph.87.3.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pahor M, Guralnik JM, Ambrosius WT, et al. Effect of structured physical activity on prevention of major mobility disability in older adults: the LIFE study randomized clinical trial. JAMA : the journal of the American Medical Association. 2014;311(23):2387–2396. doi: 10.1001/jama.2014.5616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Newman AB, Simonsick EM, Naydeck BL, et al. Association of long-distance corridor walk performance with mortality, cardiovascular disease, mobility limitation, and disability. JAMA : the journal of the American Medical Association. 2006;295(17):2018–2026. doi: 10.1001/jama.295.17.2018. [DOI] [PubMed] [Google Scholar]
- 20.Lohmander LS, Gerhardsson de Verdier M, Rollof J, Nilsson PM, Engstrom G. Incidence of severe knee and hip osteoarthritis in relation to different measures of body mass: a population-based prospective cohort study. Annals of the rheumatic diseases. 2009;68(4):490–496. doi: 10.1136/ard.2008.089748. [DOI] [PubMed] [Google Scholar]
- 21.Jerome GJ, Ko SU, Kauffman D, Studenski SA, Ferrucci L, Simonsick EM. Gait characteristics associated with walking speed decline in older adults: Results from the Baltimore Longitudinal Study of Aging. Archives of gerontology and geriatrics. 2015;60(2):239–243. doi: 10.1016/j.archger.2015.01.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shields M, Tremblay MS, Connor Gorber S, Janssen I. Measures of abdominal obesity within body mass index categories, 1981 and 2007–2009. Health reports. 2012;23(2):33–38. [PubMed] [Google Scholar]
- 23.Batsis JA, Germain CM, Vasquez E, Zbehlik AJ, Bartels SJ. Physical Activity Predicts Higher Physical Function in Older Adults: The Osteoarthritis Initiative. Journal of physical activity & health. 2015 doi: 10.1123/jpah.2014-0531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Callahan DM, Tourville TW, Miller MS, et al. Chronic Disuse and Skeletal Muscle Structure in Older Adults: Sex-Specific Differences and Relationships to Contractile Function. American journal of physiology. Cell physiology. 2015 doi: 10.1152/ajpcell.00014.2015. ajpcell 00014 02015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Smith SG, O'Conor R, Curtis LM, et al. Low health literacy predicts decline in physical function among older adults: findings from the LitCog cohort study. Journal of epidemiology and community health. 2015 doi: 10.1136/jech-2014-204915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Samuel LJ, Glass TA, Thorpe RJ, Jr, Szanton SL, Roth DL. Household and neighborhood conditions partially account for associations between education and physical capacity in the National Health and Aging Trends Study. Soc Sci Med. 2015;128:67–75. doi: 10.1016/j.socscimed.2015.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Washburn RA, Ficker JL. Physical Activity Scale for the Elderly (PASE): the relationship with activity measured by a portable accelerometer. J Sports Med Phys Fitness. 1999;39(4):336–340. [PubMed] [Google Scholar]
- 28.Sattler M, Dannhauer T, Hudelmaier M, et al. Side differences of thigh muscle cross-sectional areas and maximal isometric muscle force in bilateral knees with the same radiographic disease stage, but unilateral frequent pain - data from the osteoarthritis initiative. Osteoarthritis and cartilage / OARS, Osteoarthritis Research Society. 2012;20(6):532–540. doi: 10.1016/j.joca.2012.02.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Eckstein F, Maschek S, Wirth W, et al. One year change of knee cartilage morphology in the first release of participants from the Osteoarthritis Initiative progression subcohort: association with sex, body mass index, symptoms and radiographic osteoarthritis status. Annals of the rheumatic diseases. 2009;68(5):674–679. doi: 10.1136/ard.2008.089904. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Peterfy C, Li J, Zaim S, et al. Comparison of fixed-flexion positioning with fluoroscopic semi-flexed positioning for quantifying radiographic joint-space width in the knee: test-retest reproducibility. Skeletal Radiol. 2003;32(3):128–132. doi: 10.1007/s00256-002-0603-z. [DOI] [PubMed] [Google Scholar]
- 31.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Annals of the rheumatic diseases. 1957;16(4):494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Williams PT. Increases in weight and body size increase the odds for hypertension during 7 years of follow-up. Obesity (Silver Spring) 2008;16(11):2541–2548. doi: 10.1038/oby.2008.396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Eriksson-Hogling D, Andersson DP, Backdahl J, et al. Adipose tissue morphology predicts improved insulin sensitivity following moderate or pronounced weight loss. Int J Obes (Lond) 2015 doi: 10.1038/ijo.2015.18. [DOI] [PubMed] [Google Scholar]
- 34.Manson JE, Stampfer MJ, Hennekens CH, Willett WC. Body weight and longevity. A reassessment. JAMA : the journal of the American Medical Association. 1987;257(3):353–358. [PubMed] [Google Scholar]
- 35.Manson JE, Bassuk SS, Hu FB, Stampfer MJ, Colditz GA, Willett WC. Estimating the number of deaths due to obesity: can the divergent findings be reconciled? J Womens Health (Larchmt) 2007;16(2):168–176. doi: 10.1089/jwh.2006.0080. [DOI] [PubMed] [Google Scholar]
- 36.Nguyen US, Niu J, Choi HK, Zhang Y. Commentary: effect of obesity on mortality: comment on article by Banack and Kaufman. Epidemiology. 2014;25(1):2–3. doi: 10.1097/EDE.0000000000000010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Zou G. A modified poisson regression approach to prospective studies with binary data. Am J Epidemiol. 2004;159(7):702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 38.Han TS, Lean ME. A clinical perspective of obesity, metabolic syndrome and cardiovascular disease. JRSM Cardiovasc Dis. 2016;5 doi: 10.1177/2048004016633371. 2048004016633371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Winter Y, Pieper L, Klotsche J, Riedel O, Wittchen HU. Obesity and Abdominal Fat Markers in Patients with a History of Stroke and Transient Ischemic Attacks. J Stroke Cerebrovasc Dis. 2016 doi: 10.1016/j.jstrokecerebrovasdis.2015.12.026. [DOI] [PubMed] [Google Scholar]
- 40.Walther G, Obert P, Dutheil F, et al. Metabolic Syndrome Individuals With and Without Type 2 Diabetes Mellitus Present Generalized Vascular Dysfunction: Cross-Sectional Study. Arteriosclerosis, thrombosis, and vascular biology. 2015 doi: 10.1161/ATVBAHA.114.304591. [DOI] [PubMed] [Google Scholar]
- 41.DeSilva JM, Bonne-Annee R, Swanson Z, et al. Midtarsal break variation in modern humans: Functional causes, skeletal correlates, and paleontological implications. American journal of physical anthropology. 2015;156(4):543–552. doi: 10.1002/ajpa.22699. [DOI] [PubMed] [Google Scholar]
- 42.Gill SV, May-Benson TA, Teasdale A, Munsell EG. Birth and developmental correlates of birth weight in a sample of children with potential sensory processing disorder. BMC pediatrics. 2013;13:29. doi: 10.1186/1471-2431-13-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gravante G, Russo G, Pomara F, Ridola C. Comparison of ground reaction forces between obese and control young adults during quiet standing on a baropodometric platform. Clinical biomechanics. 2003;18(8):780–782. doi: 10.1016/s0268-0033(03)00123-2. [DOI] [PubMed] [Google Scholar]
- 44.DeVita P, Rider P, Hortobagyi T. Reductions in knee joint forces with weight loss are attenuated by gait adaptations in class III obesity. Gait & posture. 2016;45:25–30. doi: 10.1016/j.gaitpost.2015.12.040. [DOI] [PubMed] [Google Scholar]
- 45.Christensen R, Henriksen M, Leeds AR, et al. Effect of weight maintenance on symptoms of knee osteoarthritis in obese patients: a twelve-month randomized controlled trial. Arthritis care & research. 2015;67(5):640–650. doi: 10.1002/acr.22504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Neogi T, Guermazi A, Roemer F, et al. Association of Joint Inflammation With Pain Sensitization in Knee Osteoarthritis: The Multicenter Osteoarthritis Study. Arthritis Rheumatol. 2016;68(3):654–661. doi: 10.1002/art.39488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bindawas SM. Relationship between frequent knee pain, obesity, and gait speed in older adults: data from the Osteoarthritis Initiative. Clin Interv Aging. 2016;11:237–244. doi: 10.2147/CIA.S100546. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Murphy L, Schwartz TA, Helmick CG, et al. Lifetime risk of symptomatic knee osteoarthritis. Arthritis and rheumatism. 2008;59(9):1207–1213. doi: 10.1002/art.24021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Batsis JA, Zbehlik AJ, Barre LK, Mackenzie TA, Bartels SJ. The impact of waist circumference on function and physical activity in older adults: longitudinal observational data from the osteoarthritis initiative. Nutr J. 2014;13:81. doi: 10.1186/1475-2891-13-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.