Abstract
Background
The optimal pre-operative alpha-blockade strategy is debated for patients undergoing laparoscopic adrenalectomy for pheochromocytomas. We evaluated the impact of selective versus non-selective alpha-blockade on intra-operative hemodynamics and post-operative outcomes.
Methods
We identified patients having laparoscopic adrenalectomy for pheochromocytomas from 2001-2015. As a marker of overall intra-operative hemodynamics, we combined systolic blood pressure (SBP) >200, SBP <80, SBP <80 AND >200, pulse >120, vasopressor infusion, and vasodilator infusion into a single variable. Similarly, the combination of vasopressor infusion in the post-anesthesia care unit (PACU) and need for intensive care unit (ICU) admission provided an overview of post-operative support.
Results
We identified 52 patients undergoing unilateral laparoscopic adrenalectomy for pheochromocytoma. Selective alpha-blockade (i.e. Doxazosin) was performed in 35% (n=18), and non-selective blockade with Phenoxybenzamine was performed in 65% (n=34). Demographics and tumor characteristics were similar between groups. Patients blocked selectively were more likely to have a SBP <80 (67%) than those blocked with phenoxybenzamine (35%) (p=0.03), but we found no significant difference in overall intra-operative hemodynamics between patients blocked selectively and non-selectively (p=0.09). Post-operatively, however, patients blocked selectively were more likely to require additional support with vasopressor infusions in the PACU or ICU admission (p=0.02). Hospital stay and complication rates were similar.
Conclusion
Laparoscopic adrenalectomy for pheochromocytoma is safe regardless of the pre-operative alpha-blockade strategy employed, but patients blocked selectively may have a higher incidence of transient hypotension during surgery and a greater need for post-operative support. These differences did not result in longer hospital stay or increased complications.
Keywords: Pheochromcytoma, Phenoxybenzamine, Doxazosin, Alpha-blockade, Adrenalectomy
Introduction
Pheochromocytomas are rare catecholamine secreting tumors that usually originate in the adrenal medulla. Surgical extirpation is curative, but can be associated with rapid and severe blood pressure fluctuations in the operating room. Laparoscopic adrenalectomy, first described in the early 1990s, is associated with less pain, less morbidity, and a quicker recovery, and is considered the gold standard surgery for benign adrenal lesions (1-5).
Intra-operative hemodynamic instability during adrenalectomy for pheochromocytomas places patients at significantly increased risk for major morbidity (6). Alpha-receptor blockade and volume expansion are the mainstays of pre-operative preparation in order to help minimize intra-operative instability or at least make catecholamine fluctuations easier to control (7). However, the optimal alpha-blockade strategy is debated (8). Phenoxybenzamine provides irreversible inhibition of both alpha-1 and alpha-2 receptors. Although its half-life is 24 hours, it requires administration two to three times daily because new receptors are constantly being produced. Non-selectively blocked patients often experience more side effects such as nasal congestion and inhibition of postural reflexes resulting in orthostatic hypotension. Selective alpha-1 receptor blockade with newer agents like doxazosin provides an alternative. Although the half-life is similar (22 hours), sustained release formulations allow once daily dosing. Selective alpha-1 blockers cause fewer side effects, which are largely driven by alpha-2 inhibition. However, their inhibition is competitive and may be overcome with large surges in catecholamines, especially during manipulation of a pheochromocytoma. Therefore, selective blockade may not offer as much protection against perioperative hemodynamic instability as non-competitive blockade.
Previous studies have evaluated the impact of selective versus non-selective alpha-blockade on intra-operative and post-operative outcomes, but these investigations have many limitations. For instance, some studies compared groups of patients undergoing mixed proportions of laparoscopic and open adrenalectomy (9-11), and others failed to correct for tumor size variations between groups (9, 12). Another study examined outcomes across two institutions with different practices and populations (13). In order to minimize confounding variables, we compared outcomes across two similar populations receiving the same operation. We aimed to compare the effects of selective versus non-selective alpha-blockade on intra-operative hemodynamic instability and post-operative support requirements in patients exclusively undergoing laparoscopic adrenalectomy for pheochromocytoma.
Methods
We performed a retrospective comparative cohort study of patients undergoing adrenalectomy from 2001 to 2015 at a single institution. We identified patients in a prospectively maintained adrenal database, and the University of Wisconsin Institutional Review Board approved the study. Patients with histologically confirmed pheochromocytomas were included. Planned open (n=2) and bilateral (n=1) adrenalectomies were excluded, and one patient who underwent a reoperative laparoscopic adrenalectomy following a prior partial adrenalectomy was also excluded. Patients were categorized into two groups based on pre-operative alpha-blockade strategy. We compared patients blocked selectively to those blocked non-selectively with phenoxybenzamine. We examined patient and tumor characteristics, intra-operative hemodynamics, and post-operative outcomes between groups.
All patients were alpha-blocked prior to adrenalectomy. Selective alpha-blockade included terazosin, prazosin, and doxazosin, and non-selective alpha-blockade consisted only of phenoxybenzamine. Alpha-blockade initiated prior to surgical referral was continued with the same agent. Otherwise, patients started on an alpha-blocker at the discretion of the operating surgeon. For those initiated on alpha-blockade by the surgeon, the starting dose was either 10 mg of phenoxybenzamine three times daily or 1–2 mg of doxazosin daily. Following initiation of alpha-blockade with either selective or non-selective agents, doses were titrated to blood pressures of 120/80 mmHg. Additionally, patients receiving phenoxybenzamine were titrated to the point of developing orthostatic hypotension, which suggested loss of the baroreceptor reflex and achievement of complete blockade. This side effect was not experienced with selective blockade. After alpha-blockade was achieved, a beta-blocker added additional heart rate control when necessary. Hydration and increased salt intake was encouraged the week before surgery. Adequate alpha-blockade, based on measured blood pressure, was required before adrenalectomy.
In the operating room all patients received an arterial line for blood pressure monitoring and indwelling urinary catheters to measure urine output. The anesthesiologist established access with at least two well-functioning peripheral intravenous lines. Central access was left to the discretion of the anesthesiologist. Once monitoring and access was sufficient, a transabdominal laparoscopic adrenalectomy was performed. Anesthesiologists determined the thresholds for treating patient hemodynamics and decided whether to use fluid or vasoactive drugs. At the conclusion of surgery, vasopressors were weaned as soon as physiologically safe. Patients recovered in the post-anesthesia care unit prior to admission to the general ward. Admission to the intensive care unit (ICU) only occurred when patient physiology, hemodynamic monitoring, and hospital policy demanded a higher level of care.
Patient and tumor characteristics were recorded prospectively. Intra-operative hemodynamic profiles were retrospectively abstracted from anesthesia records. Anesthesia records at our institution do not record specific systolic blood pressures (SBP) above 200 mmHg, therefore any SBP greater than 200 mmHg was considered to be 200 mmHg for the purpose of calculating the SBP range intra-operatively. When estimated blood loss was recorded as “minimal,” we assigned it a value of 0 ml.
The primary outcome was intra-operative hemodynamic instability, and the secondary outcome was post-operative support. As a marker of overall intra-operative hemodynamic instability, we created a composite variable assigning 1 point for each of the following markers of instability: SBP > 200, SBP < 80, SBP < 80 AND > 200, pulse > 120, vasopressor infusion, and vasodilator infusion. Similarly, we constructed a post-operative composite variable as an appraisal of necessary post-operative support assigning 1 point for either vasopressor infusion in the post-anesthesia care unit or the need for ICU admission. Other outcome variables included length of stay and complications.
Descriptive statistics included frequency and percent for nominal variables and median and interquartile range (IQR) for continuous variables. Nominal variables were compared with Chi-squared tests, while the Mann-Whitney U test compared continuous variables. A p value less than 0.05 defined statistical significance. Statistical analyses were performed with SPSS 23 (IBM, Chicago, IL).
Results
Between 2001 and 2015, 52 patients underwent a unilateral, transabdominal laparoscopic adrenalectomy for a histologically confirmed pheochromocytoma. No procedures were converted to an open approach. Selective alpha-blockade was performed in 35% (n=18) of cases, while non-selective blockade with phenoxybenzamine was performed in 65% (n=34). The majority of the first 26 patients (92%) were blocked non-selectively while the majority of the second 26 patients (62%) were blocked selectively. The selectively blocked group included 12 (66.7%) patients prepared with doxazosin, 5 (27.8%) with prazosin, and 1 (5.6%) with terazosin. Age, gender, Charlson comorbidity index (14), body mass index, tumor laterality, tumor size, and hormone profiles were similar between the two groups (Table 1). Tumor sizes ranged from 1 to 9.5 cm.
Table 1. Patient and Tumor Characteristics.
| Variable | Selective Alpha-Blockade n=18 | Non-selective Alpha-Blockade n=34 | P |
|---|---|---|---|
| Age, median (IQR), years | 55 (26) | 53 (23.5) | 0.77 |
| Gender, n (%) | 0.24 | ||
| Male | 5 (27.8) | 15 (44.1) | |
| Female | 13 (72.2) | 19 (55.9) | |
| Tobacco Use, n (%) | 6 (33.3) | 10 (29.4) | 0.77 |
| Diabetes Mellitus, n (%) | 3 (16.7) | 7 (20.6) | 0.73 |
| Charlson Comorbidity Index, median (IQR) | 1.5 (3.0) | 2.0 (1.5) | 0.89 |
| Body Mass Index, median (IQR) | 26.5 (11.3) | 28.3 (7.6) | 0.86 |
| Familial, n (%) | 2 (11.1) | 6 (17.6) | 0.53 |
| Tumor Laterality, n (%) | 0.82 | ||
| Right | 8 (44.4) | 14 (41.2) | |
| Left | 10 (55.6) | 20 (58.8) | |
| Tumor size, median (IQR), cm | 3.3 (2.7) | 3.5 (2.2) | 0.60 |
| Duration of blockade, median (IQR), weeks | 5 (2) | 6 (4) | 0.05 |
| Pre-operative SBP, median (IQR), mmHg | 128 (23) | 128 (47.5) | 0.21 |
| Pre-operative Pulse, median (IQR) | 78 (9) | 80 (15) | 0.59 |
| Incidental, n (%) | 9 (50.0) | 2 (5.9) | <0.001 |
| Elevated Metanephrines, n (%) | 15 (83.3) | 28 (82.4) | 1.0 |
| Elevated Normetanephrines, n (%) | 8 (44.4) | 7 (20.6) | 0.11 |
| Beta-Blocker, n (%) | 6 (33.3) | 17 (50.0) | 0.25 |
| Calcium Channel Blocker, n (%) | 2 (11.8) | 3 (9.7) | 0.82 |
| Metyrosine, n (%) | 0 (0) | 1 (2.9) | 0.35 |
IQR- inter-quartile range, SBP- systolic blood pressure
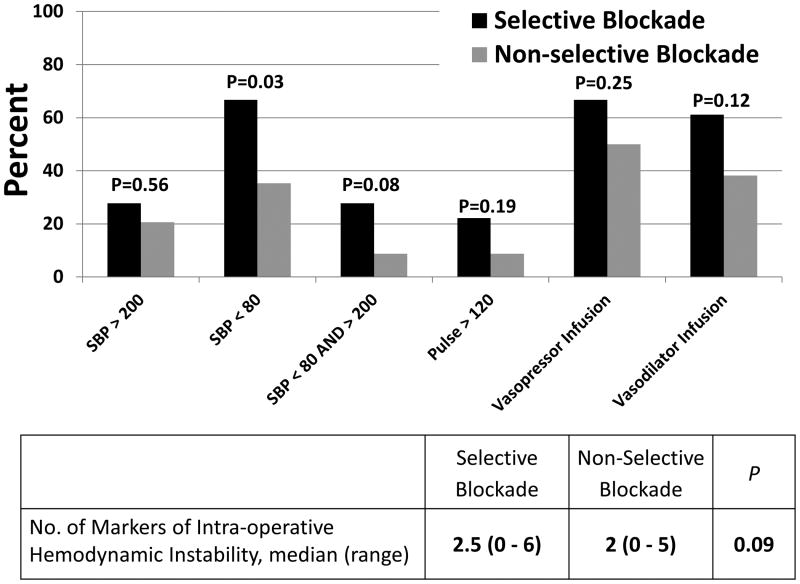
Operative time was similar between groups (median, 99 minutes for selective blockade versus 93 minutes for non-selective blockade, p=0.99) as was estimated blood loss (median, 40 ml for selective blockade versus 100 ml for non-selective blockade, p=0.08). Intra-operatively, the initial, highest, and lowest SBP were similar between groups (Table 2). Although patients blocked selectively were no more likely to have a SBP > 200 mmHg during the case (27.8% for selective blockade versus 20.6% for non-selective blockade, p=0.56), they were more likely to have their SBP drop below 80 mmHg than those blocked with phenoxybenzamine (66.7% for selective versus 35.3% for non-selective, p=0.03). Although there was variation in the amounts of crystalloid and colloid fluids administered, urine output was similar between groups (median output 313 ml for selective blockade versus 200 for non-selective blockade, p=0.14) indicating similar volume status. When evaluating intra-operative hemodynamic instability as a single variable, the overall hemodynamic profiles revealed that the two blockade strategies did not result in significantly different instability (Figure 1).
Table 2. Intra-operative Hemodynamic and Support Variables.
| Variable | Selective Alpha-Blockade n=18 | Non-selective Alpha-Blockade n=34 | P |
|---|---|---|---|
| Central Venous Access, n (%)n=51 | 12 (66.7) | 19 (55.9) | 0.45 |
| Initial SBP, median (IQR), mmHg | 136.5 (35.5) | 130 (23.5) | 0.36 |
| Highest SBP, median (IQR), mmHg | 190 (28.0) | 175 (35.5) | 0.07 |
| Lowest SBP, median (IQR), mmHg | 76.5 (11.5) | 80 (17.5) | 0.07 |
| SBP range (Highest SBP – Lowest SBP), median (IQR), mmHg | 114.5 (41) | 107 (44.5) | 0.03 |
| SBP > 200 mmHg, n (%) | 5 (27.8) | 7 (20.6) | 0.56 |
| No. times SBP > 200 mmHg, median (IQR) | 0 (1) Mean- 0.75 |
0 (0) Mean- 0.33 |
0.54 |
| SBP < 80 mmHg, n (%) | 12 (66.7) | 12 (35.3) | 0.03 |
| No. times SBP < 80 mmHg, median (IQR) | 1 (2.0) Mean- 1.6 |
0 (2.5) Mean- 1.3 |
0.12 |
| Cases with SBP > 200 and < 80 mmHg, n (%) | 5 (27.8) | 3 (8.8) | 0.08 |
| Pulse > 120, n (%) | 4 (22.2) | 3 (8.8) | 0.19 |
| No. times pulse > 120, median (IQR) | 0 (0) Mean- 0.31 |
0 (0) Mean- 0.57 |
0.23 |
| Vasopressor infusion, n (%) | 12 (66.7) | 17 (50.0) | 0.25 |
| Vasodilator infusion, n (%) | 11 (61.1) | 13 (38.2) | 0.12 |
| Volume crystalloid, median (IQR), ml | 2250 (1150) | 2750 (1750) | 0.06 |
| Volume colloid, median (IQR), ml | 0 (0) Mean- 47 |
0 (13) Mean- 108 |
0.02 |
| Estimated blood loss, median (IQR), ml | 40 (94) Mean- 83 |
100 (75) Mean- 136 |
0.08 |
| Blood transfusion, n (%) | 0 (0) | 2 (5.9) | 0.19 |
| Urine output, median (IQR), ml | 313 (188) | 200 (245) | 0.14 |
SBP- systolic blood pressure, IQR- inter-quartile range
Figure 1. Markers of Intra-operative Hemodynamic Instability.
This figure graphically displays the proportion of patients in each alpha-blockade group that experienced each of 6 markers of intra-operative hemodynamic instability. The chart compares the median sum of individual markers to provide an overview of hemodynamic instability. SBP- systolic blood pressure.
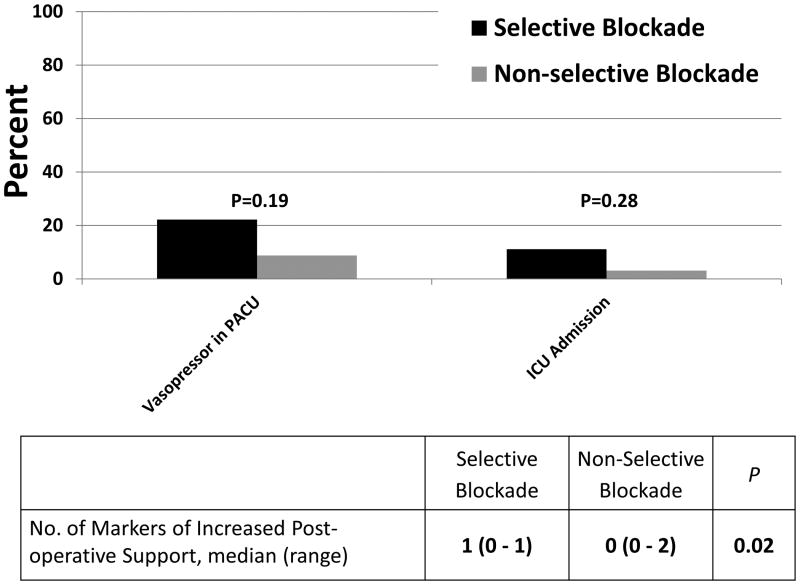
Post-operatively, patients recovered well requiring little support. The median length of stay was 1 day for both groups (p=0.18). Although most patients were weaned from vasopressor infusions prior to leaving the operating room, a minority of patients required vasopressors in recovery (Table 3). When we examined vasopressor requirements in the recovery room and the need for ICU admission as a single variable, analysis revealed that patients blocked selectively required more post-operative support (Figure 2). Overall complication rates were similar between groups (11.1% for selective versus 11.8% for non-selective, p=0.94). Seven complications were noted in 6 patients and included respiratory insufficiency (n=2), pneumonia (n=1), pneumothorax (n=1), bleeding from the liver (n=1), splenic injury (n=1), and delirium (n=1).
Table 3. Post-operative Outcomes.
| Variable | Selective Alpha-Blockade n=18 | Non-selective Alpha-Blockade n=34 | P |
|---|---|---|---|
| Vasopressor infusion in PACU, n (%) | 4 (22.2) | 3 (8.8) | 0.19 |
| ICU admission, n (%) | 2 (11.1) | 1 (3.2) | 0.28 |
| Length of stay, median (IQR), days | 1 (2) | 1 (0) | 0.18 |
| Complication, n (%) | 2 (11.1) | 4 (11.8) | 0.72 |
PACU- Post-anesthesia care unit, ICU- Intensive care unit, IQR- inter-quartile range
Figure 2. Markers of Post-operative Support.
This figure graphically displays the proportion of patients in each alpha-blockade group that experienced a marker of increased post-operative support. The chart compares the median sum of individual markers to provide an overview of required post-operative support. PACU- Post-anesthesia care unit, ICU- Intensive care unit.
Discussion
Laparoscopic adrenalectomy for pheochromocytomas is safe, but the optimal pre-operative alpha-receptor blockade strategy is controversial. Prior studies on this topic compared heterogeneous groups and dissimilar practices. The current study investigated the impact of selective versus non-selective alpha-blockade on perioperative outcomes in patients with pheochromocytomas who underwent laparoscopic adrenalectomy. Both groups were similar in terms of patient demographics, comorbidities, and tumor characteristics. Additionally, patients in each group appeared to be completely and similarly alpha-blocked prior to surgery based on their initial intraoperative blood pressures. Overall, intra-operative hemodynamics were not significantly different between the two groups. Patients blocked selectively required slightly more post-operative support, but this requirement did not translate into increased complications or a longer length of stay.
In the current study, intra-operative hypertensive episodes (SBP > 200 mmHg) occurred in a similar proportion of patients in both groups. Several prior studies have also shown no difference in intra-operative hypertensive episodes or peak SBP during tumor handling (9, 10, 12). On the other hand, Weingarten and colleagues (13) reported that the total intra-operative time spent at pressures above 200 mmHg did not differ between groups, but they did demonstrate that the mean peak SBP was significantly greater for the group blocked selectively. This study, however, compared patients at two different institutions and selective blockade was more common in a patient population with a higher body mass index (13). Yet others have also reported more episodes of intra-operative hypertension in patients blocked selectively (11, 15). Zhu and colleagues (16) reported higher, but not hypertensive, mean SBP during anesthesia in patients blocked selectively, but blood pressures during tumor handling were similar (16). The current study may have had insufficient numbers to identify increased hypertensive episodes in selectively blocked patients, but the lack of a noted difference could also reflect the exclusion of confounding variables. Other major predictors of hypertensive episodes have included open procedures and large tumor size (15), and the current study did not include open procedures and tumor size was equivalent between groups.
Another difference we found compared to prior studies was a higher proportion of patients that experienced hypotensive episodes (SBP < 80 mmHg) in the selectively blocked group. We also noted a greater range of intra-operative SBPs in the selectively blocked group. In contrast, Zhu and colleagues (16) reported a wider range of intra-operative SBP in non-selectively blocked patients (16). The reason for the increased hypotensive episodes and greater intra-operative SBP variability is not readily apparent. Because the number of patients was small, it is possible that hypotensive episodes appeared more common in selectively blocked patients due to the impact of outliers or confounding factors. Based on the intra-operative fluid requirements and urine output, patients appeared similarly well hydrated. Patients blocked selectively also did not have greater estimated blood loss to explain more hypotensive episodes. Besides hydration status and blood loss, another possible confounding factor is anesthesiologist bias. Perhaps, anesthesiologists were more concerned about hypertensive episodes in patients blocked selectively and treated higher blood pressures more aggressively. However, we did not see more liberal use of vasodilator infusions in the selectively blocked group, suggesting that if a treatment bias is present, it is small.
Despite the increase in hypotensive episodes, wider range of intra-operative SBPs and non-significant trends in other individual operative hemodynamic parameters, our data demonstrate that overall, hemodynamic instability was not significantly different for each pre-operative alpha-blockade strategy. This conclusion is based on the similarity between the composite variable that took several markers of hemodynamic instability into account. Our findings are in agreement with many others who have failed to identify a difference in overall hemodynamic instability based on the type of pre-operative blockade (9, 10, 12). In contrast, our results disagree with other investigations that report improved intra-operative stability with phenoxybenzamine (11, 13, 15). After a thorough review of previously published studies on the subject, Van der Zee and colleagues (8) concluded that no clearly superior alpha-blockade strategy exists. However, they do suggest that intra-operative hemodynamics appear to be slightly more stable in patients blocked non-selectively (8).
In our study, patients generally did very well post-operatively, regardless of the type of alpha-blockade. When considering the combination of vasopressor support in the recovery room and ICU admission as a marker of post-operative support, our data demonstrate that patients blocked selectively needed slightly more support. In spite of the increased support requirements, hospital stays were equally short and complications few when compared to the non-selectively blocked group. Many other studies also have been unable to show a difference in post-operative outcomes based on pre-operative alpha-blockade strategy even when intra-operative hemodynamics were different (9-13, 15). Collectively, the current study and the existing literature fail to demonstrate the superiority of one strategy over the other in terms of operative outcomes. In patients having their pheochromocytomas resected laparoscopically, either strategy appears to be a safe option. In the absence of a clearly safer alpha-blockade strategy, secondary considerations like convenience, patient tolerance, and cost are important considerations in the choice of agent. Selective alpha-blockers are dosed less frequently and are generally tolerated without side-effects. Furthermore, 30 tablets (one month supply) of doxazosin range between $7 and $30, but 30 capsules (10-15 day supply) of phenoxybenzamine range from $7,100 to $7,600, yet the cost of the medication may not reflect the entirety of the cost implications of each strategy (17).
The current study does have limitations. First, despite having a relatively large number of patients with a rare disease, the sample remains small. The size of the groups precluded subgroup and multivariate analyses. Furthermore, we may have been underpowered to detect real differences in individual hemodynamic parameters as there were several non-significant trends noted between the two groups. To combat this limitation and to provide an overview of hemodynamic instability, a composite variable was constructed and compared between groups. Additionally, the retrospective nature of the study made it impossible to determine why a particular alpha-blocker was chosen over another. The choice of alpha-blockade was based on what the referring provider had initiated or on surgeon preference instead of being based on patient characteristics, but selection biases may be present. Lastly, the current study only evaluated patients undergoing laparoscopic adrenalectomy, so our results might not be generalizable to patients having open adrenalectomies. Despite these limitations, this study represents a single institution comparative cohort study of alpha-blockade strategies in a homogeneous population undergoing adrenalectomy with a similar technique.
Our results demonstrate that laparoscopic adrenalectomy for pheochromocytoma is safe regardless of the alpha-blockade strategy employed, but patients blocked selectively may have a higher incidence of transient hypotension during surgery and require slightly more post-operative support. While these differences did not result in a longer hospital stay or increased complications, they serve to caution surgeons against the widespread adoption of selective alpha-blockade without further investigation.
Synopsis.
The optimal pre-operative alpha-blockade strategy is debated for patients undergoing laparoscopic adrenalectomy for pheochromocytoma. Intra-operative hypotension and increased post-operative support were associated with selective blockade, but complications and hospital stay were similar between those blocked selectively and non-selectively.
Footnotes
Disclosures: No authors have anything to disclose.
Presented as a poster at the 37th annual meeting of the American Association of Endocrine Surgeons in Baltimore, Maryland April 10th, 2016
References
- 1.Gagner M, Lacroix A, Bolte E. Laparoscopic adrenalectomy in Cushing's syndrome and pheochromocytoma. The New England journal of medicine. 1992;327(14):1033. doi: 10.1056/NEJM199210013271417. [DOI] [PubMed] [Google Scholar]
- 2.Brunt LM, Doherty GM, Norton JA, Soper NJ, Quasebarth MA, Moley JF. Laparoscopic adrenalectomy compared to open adrenalectomy for benign adrenal neoplasms. Journal of the American College of Surgeons. 1996;183(1):1–10. [PubMed] [Google Scholar]
- 3.Guazzoni G, Montorsi F, Bocciardi A, Da Pozzo L, Rigatti P, Lanzi R, et al. Transperitoneal laparoscopic versus open adrenalectomy for benign hyperfunctioning adrenal tumors: a comparative study. The Journal of urology. 1995;153(5):1597–600. [PubMed] [Google Scholar]
- 4.Lee J, El-Tamer M, Schifftner T, Turrentine FE, Henderson WG, Khuri S, et al. Open and laparoscopic adrenalectomy: analysis of the National Surgical Quality Improvement Program. Journal of the American College of Surgeons. 2008;206(5):953–9. doi: 10.1016/j.jamcollsurg.2008.01.018. discussion 9-61. [DOI] [PubMed] [Google Scholar]
- 5.Carr AA, Wang TS. Minimally Invasive Adrenalectomy. Surgical oncology clinics of North America. 2016;25(1):139–52. doi: 10.1016/j.soc.2015.08.007. [DOI] [PubMed] [Google Scholar]
- 6.Brunaud L, Nguyen-Thi PL, Mirallie E, Raffaelli M, Vriens M, Theveniaud PE, et al. Predictive factors for postoperative morbidity after laparoscopic adrenalectomy for pheochromocytoma: a multicenter retrospective analysis in 225 patients. Surgical endoscopy. 2016;30(3):1051–9. doi: 10.1007/s00464-015-4294-7. [DOI] [PubMed] [Google Scholar]
- 7.Pacak K, Eisenhofer G, Ahlman H, Bornstein SR, Gimenez-Roqueplo AP, Grossman AB, et al. Pheochromocytoma: recommendations for clinical practice from the First International Symposium. October 2005. Nature clinical practice Endocrinology & metabolism. 2007;3(2):92–102. doi: 10.1038/ncpendmet0396. [DOI] [PubMed] [Google Scholar]
- 8.van der Zee PA, de Boer A. Pheochromocytoma: a review on preoperative treatment with phenoxybenzamine or doxazosin. The Netherlands journal of medicine. 2014;72(4):190–201. [PubMed] [Google Scholar]
- 9.Prys-Roberts C, Farndon JR. Efficacy and safety of doxazosin for perioperative management of patients with pheochromocytoma. World journal of surgery. 2002;26(8):1037–42. doi: 10.1007/s00268-002-6667-z. [DOI] [PubMed] [Google Scholar]
- 10.Kocak S, Aydintug S, Canakci N. Alpha blockade in preoperative preparation of patients with pheochromocytomas. International surgery. 2002;87(3):191–4. [PubMed] [Google Scholar]
- 11.Agrawal R, Mishra SK, Bhatia E, Mishra A, Chand G, Agarwal G, et al. Prospective study to compare peri-operative hemodynamic alterations following preparation for pheochromocytoma surgery by phenoxybenzamine or prazosin. World journal of surgery. 2014;38(3):716–23. doi: 10.1007/s00268-013-2325-x. [DOI] [PubMed] [Google Scholar]
- 12.Bruynzeel H, Feelders RA, Groenland TH, van den Meiracker AH, van Eijck CH, Lange JF, et al. Risk Factors for Hemodynamic Instability during Surgery for Pheochromocytoma. The Journal of clinical endocrinology and metabolism. 2010;95(2):678–85. doi: 10.1210/jc.2009-1051. [DOI] [PubMed] [Google Scholar]
- 13.Weingarten TN, Cata JP, O'Hara JF, Prybilla DJ, Pike TL, Thompson GB, et al. Comparison of two preoperative medical management strategies for laparoscopic resection of pheochromocytoma. Urology. 2010;76(2):508 e6–11. doi: 10.1016/j.urology.2010.03.032. [DOI] [PubMed] [Google Scholar]
- 14.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. Journal of chronic diseases. 1987;40(5):373–83. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 15.Kiernan CM, Du L, Chen X, Broome JT, Shi C, Peters MF, et al. Predictors of hemodynamic instability during surgery for pheochromocytoma. Annals of surgical oncology. 2014;21(12):3865–71. doi: 10.1245/s10434-014-3847-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhu Y, He HC, Su TW, Wu YX, Wang WQ, Zhao JP, et al. Selective alpha1-adrenoceptor antagonist (controlled release tablets) in preoperative management of pheochromocytoma. Endocrine. 2010;38(2):254–9. doi: 10.1007/s12020-010-9381-x. [DOI] [PubMed] [Google Scholar]
- 17.www.goodrx.com. GoodRx, Inc. 2016 May 31; Available from: http://www.goodrx.com/