Abstract
Background
Little is known about fertility choices and pregnancy outcome rates among HIV-infected women in the current combination ART era.
Objective
To describe trends and factors associated with live-birth and abortion rates among HIV-positive and high-risk HIV-negative women enrolled in the Women’s Interagency HIV Study (WIHS) in the United States.
Study Design
We analyzed longitudinal data collected from October 1st 1994 to September 30th 2012 through WIHS. Age-adjusted rates per 100 person-years (PY) live-births, and induced abortions were calculated by HIV serostatus over four time periods. Poisson mixed effects models containing variables associated with live-births and abortions in bivariable analyses (p<0.05) generated adjusted incidence rate ratios (aIRRs) and 95% confidence intervals.
Results
There were 1,356 pregnancies among 2,414 women. Among HIV-positive women, age-adjusted rates of live-birth increased from 1994-1997 to 2006-2012 (2.85/100PY to 7.27/100PY, p-trend<0.0001). Age-adjusted rates of abortion in HIV-positive women remained stable over these time periods (4.03/100PY to 4.29/100PY, p-trend=0.09). Significantly lower live-birth rates occurred among HIV-positive compared to HIV-negative women in 1994-1997 and 1997-2001, however rates were similar during 2002-2005 and 2006-2012. Higher CD4+ T cells/mm3 (≥350 aIRR=1.39 [1.03-1.89] versus <350) was significantly associated with increased live-birth rates, while combination antiretroviral treatment (cART) use (aIRR=1.35 [0.99-1.83]) was marginally associated with increased live-birth rates. Younger age, having a prior abortion, condom use and increased parity were associated with increased abortion rates among both HIV-positive and HIV-negative women. CD4+ T-cell count, cART use, and viral load were not associated with abortion rates.
Conclusions
Unlike earlier periods (pre-2001) when live-birth rates were lower among HIV-positive women, rates are now similar to HIV-negative women, potentially due to improved health status and cART. Abortion rates remain unchanged illuminating a need to improve contraceptive services.
Keywords: Abortion, Antiretroviral therapy, ART, HIV, live-birth, pregnancy
Introduction
Pregnancy and family planning among women living with HIV involves complex decision-making and clinical management 1, 2. Considerable improvements in the treatment and care of HIV-positive women has led to increased life expectancy and improved health 3, 4. Additionally, improved clinical management of pregnant women has led to near elimination of perinatal HIV transmission among those on effective combination antiretroviral treatment (cART) throughout pregnancy 5-7. The potential of cART to reduce maternal-to-child transmission of HIV has affected the reproductive decisions of women living with HIV, with more women now choosing to have children 8-11. However, family planning is often incompletely addressed within the current HIV care paradigm. Many pregnancies occurring among HIV-positive women, similar to the general population, are unplanned. Though data are scant, it has been estimated that up to 80% of pregnancies occurring among HIV-positive women in the United States (US) are unintended 12-14, compared to approximately 50% in the general population. This highlights the importance of understanding reproductive health needs of this cohort and providing targeted family planning options as part of routine HIV care.
It is still unclear how pregnancy rates and outcomes have changed over the past 20 years among HIV-positive women, spanning the introduction of cART, compared to HIV-negative women. A 1994-2002 Women's Interagency HIV Study (WIHS, an ongoing multicenter prospective cohort study of HIV infection and outcomes among women with and without HIV) analysis found pregnancy rates of 7.4 and 15.2/100 person-years among HIV-positive and high-risk negative women, respectively 11. In a more recent 2002-2009 WIHS study, Linas et al reported that HIV infection was associated with a 40% reduction in pregnancy incidence among HIV-positive versus HIV-negative women adjusting for age, number of sexual partners, contraception, parity and alcohol use 15.
This study aims to describe trends in pregnancy and pregnancy outcomes, including live-birth and abortion, over the past 20 years in HIV-positive and negative women enrolled in the WIHS cohort. We further determine factors associatedwith live-births and abortion, specifically focusing on the role of HIV viral load and cART, to better understand the impact of improved immune function and other factors in pregnancy outcomes.
Materials and Methods
We performed a longitudinal analysis of WIHS data collected between October 1st 1994 to September 30th 2012 16. HIV-positive and high-risk negative women were recruited from similar sites with more than half of the participants living below the federally defined level of poverty and frequency matched based on demographics and key risk factors for acquiring HIV, such as drug use and number of partners, with recruitment targets adjusted when imbalances arose16, 17. Enrollment for WIHS began in 1994 with 6 sites (Bronx, Brooklyn, Chicago, Washington D.C., Los Angeles, San Francisco), and has continued with 6 month visits using trained interviewers, where visits include detailed questionnaires including ART use, medical history, and medication use, a clinical examination and comprehensive laboratory testing (including CD4 T-cell count and HIV viral load). WIHS had replenishment enrollment in 2001-2002, 2011-2012 and 2013-2015, now with a total of 9 US sites. Data from the 6 original sites are included in this study. IRB approval was obtained from each WIHS site prior to study enrollment. Data for this evaluation utilized de-identified data.
As obstetrical care was received outside of the study, pregnancy outcomes and associated dates were reported by the participant. Outcomes were classified as: induced abortion for those who terminated the pregnancy, live-birth for a baby born alive, and non-viable for spontaneous abortion, ectopic pregnancy or still-birth.
Women were included in this analysis if they attended at least two WIHS visits. Women not at risk for pregnancy due to history of hysterectomy, tubal ligation or bilateral oophorectomy and women over the age of 45 were excluded/censored from analysis.
Rates for induced abortion, live-birth, non-viable pregnancy and all pregnancy outcomes combined were the number of pregnancies divided by the person-years at-risk over the entire study, stratified by time: 1994-1997, 1998-2001, 2002-2005, 2006-2012. Pregnancy rates per 100 person-years were directly adjusted using the population age distribution of women with pregnancy outcomes in 1996, similar to the methods used in the prior publication by Massad in 200411. Due to the zero birth rate among older age groups, 95% confidence intervals (CI) for directly age adjusted rates are based on a modified gamma distribution 18. The Mantel-Haenszel chi-square quantified whether age adjusted pregnancy rates differed by HIV serostatus within each time period 19. Trend tests evaluated trends in adjusted rates by time interval by serostatus.
Bivariable associations between covariates (both baseline variables and time-varying) and live-birth and abortion were determined using a Poisson regression model with an offset for years in each risk group. Baseline covariates of interest were recorded at the participant’s first WIHS visit and included race/ethnicity, income, marital status, education, employment status, insurance status, WIHS site, number of male sexual partners, parity, history of abortion, prior sexually transmitted infection, and year of first cART, where cART was defined as 3 or more antiretroviral drugs used concurrently by self-report . Time-varying covariates reflect activity for the time since the last WIHS visit and included contraception use, characterized as hormonal or long-acting reversible contraceptive (LARC) including intrauterine contraception and implants compared to none or other method use (condoms, withdrawal, diaphragm). Condom use was dichotomized into any condom use since the last visit versus no use. Alcohol use was dichotomized into self-report of 0 to 7 drinks compared to more than 7 drinks per week. Current cigarette smoking and illicit drug use (marijuana/hash, crack/cocaine, methamphetamine or intravenous drug use) were positive if the individual reported any use since the last visit. A time-varying composite for chronic medical conditions (stroke, myocardial infarction, diabetes, hypertension, deep vein thrombosis, pulmonary embolus (PE), cancer or tuberculosis (TB)) was created. HIV-specific factors were incorporated for the HIV-positive cohort and included use of cART at the visit, viral load (categorized as <4 and ≥4 log10 copies or 10,000), and CD4+ T-cell count (<350 and ≥350 cells/mm3). Categorization for viral load and CD4+ T-cell count was determined a priori based upon clinical significance and the approximate median value for the WIHS cohort in 2004 based on prior publications11.
Poisson mixed effects models with a random intercept and offset for years since last visit were created to evaluate multivariate associations with live-birth or abortion including all variables with significance by bivariable association (p<0.05), crude unadjusted incidence rate ratios (cIRR), and adjusted incidence rate ratios (aIRR) with 95% confidence intervals were obtained.
Results
Among 4346 (1089 HIV-negative, 3232 HIV-positive, 25 seroconverters) women enrolled in WIHS during the study period, about 56% (n=2414) were included in this analysis. Of the 1952 women excluded, 36% (n=707) were older than 45 years, 61% % not at risk for pregnancy (n=568 hysterectomy, n=608 tubal ligation, n=7 bilateral oophoretomy), and 3% were excluded for other reasons (n=13 HIV sereoconverters, n=25 did not have 2 eligible visits to analyze, n=4 pregnancy outcome data was incomplete). This analysis included 1,750 HIV-positive and 664 HIV-negative women with a total of 1,356 pregnancies reported over 16,670 person-years (8.13/100 PY, unadjusted). Of these pregnancies, 586 (43.2%) ended in live-birth, 469 (34.6%) in abortion, and 301 (22.2%) in a non-viable pregnancy. Supplemental tables 1a and 1b show that about 50% were African American, single, had at least a high school education, and were employed and insured. Over one-half of the women had a prior abortion and over one-half had at least 1 live-birth. HIV-positive women were older than HIV-negative women. Contraception use, other than condoms, among among all women was low at approximately 15% of included visits. HIV-positive women were on cART during about half of study visits, and for over 60% of all visits viral loads were satisfactorily suppressed (<4 log10 copies/ml) and CD4+ T-cell counts adequate (≥350 cell/ mm3).
Pregnancy outcome rates over time by HIV serostatus
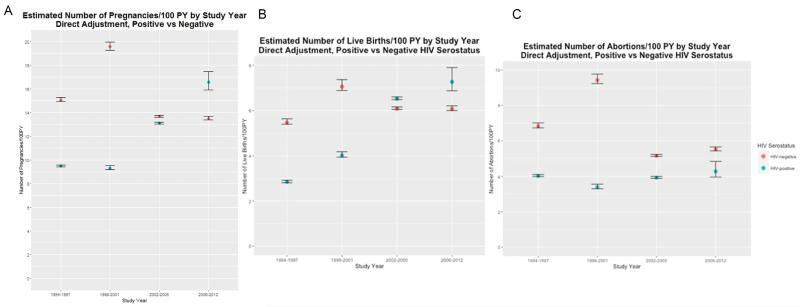
For all-pregnancy outcomes combined, age-adjusted rates (Supplemental Table 2, Figure 1A) among HIV-positive women demonstrated a non-significant increasing trend over time (p-trend=0.088). While the overall age-adjusted rates were lower among HIV-positive women compared to HIV-negative women, significantly lower rates occurred during 1994-1997 and 1998-2001 for HIV-positive women compared to HIV-negative, whereas rates during 2002-2005 and 2006-2012 were similar to HIV-negative women.
Figure 1.
Age-adjusted rate estimates of all pregnancies (Figure 1A), live-birth (Figure 1B) and abortion (Figure 1C) from 1994 to 2012 among high-risk HIV-negative (red) and HIV-positive (blue) women enrolled in the Women’s Interagency HIV study (WIHS)
Similar results were seen in age-adjusted live-birth rates. There was a significant increase observed over time (Figure 1B, HIV-positive p-trend<0.0001) for HIV-positive women, with no significant change observed among HIV-negative women (p-trend=0.76). The overall age-adjusted live-birth rate was lower for HIV-positive compared to HIV-negative women, with significantly lower rates at earlier time periods (1994-1997, 1998-2001) and no significant difference at the later time periods (2002-2005, 2006-2012).
Age-adjusted abortion rates remained relatively stable over time (Figure 1C, HIV-positive p-trend=0.093) with age-adjusted rates remaining between 3.4 and 4.4/100 person-years. While age-adjusted abortion rates among HIV-negative women decreased over time (p-trend=0.0015), the rates for HIV-positive women were significantly lower during the earlier time periods (1994-1997, 1998-2001) with no difference at periods (2002-2005, 2006-2012). Of the 301 pregnancies (181 HIV positive and 120 HIV negative) that ended in non-viable pregnancies, there was no difference in the overall age-adjusted non-viable pregnancy rate between HIV negative and HIV positive (p=0.611) and no significant trend over the years of observation (p-trend = 0.534 and 0.149 for HIV positive and HIV negative, respectively).
Associations with live birth rates
Bivariable associations are presented in Supplemental Table 3. Notably, among HIV-negative and HIV-positive women, income, insurance status, and contraception use were not associated with live-birth rates. For HIV-positive women, cART use (cIRR=1.69, 95%CI 1.32-2.16), lower viral loads (<4 log10 copies/ml cIRR=2.90, 95%CI 2.17-3.87 versus ≥4 log10 copies/ml) and higher CD4+ T-cell counts (≥350 cells/mm3 cIRR=2.70, 95%CI 2.00-3.57 versus <350 cells/mm3) were associated with increased live-birth rates in crude analyses.
In multivariable models among HIV-negative women (Table 1), those living with a partner (versus married, aIRR=1.65, 95%CI 1.07-2.54), and with less than a high-school education (aIRR=1.38, 95%CI 1.02-1.85) had higher live-birth rates, while older age (≥35 aIRR=0.22, 95%CI 0.14-0.35 versus <25), history of abortion (aIRR=0.73, 95%CI 0.55-0.98), using condoms (aIRR=0.55, 95%CI 0.41-0.73), marijuana (aIRR=0.57, 95%CI 0.39-0.84) or drug use (aIRR=0.32, 95%CI 0.15-0.66) were associated with decreased live-birth rates. For HIV-positive women (Table 1), older age (≥35 aIRR=0.14, 95%CI 0.08-0.23 versus <25), alcohol consumption (drinking more than 7 versus <7 drinks per week, aIRR=0.47, 95%CI 0.22-0.97), using condoms (aIRR=0.73, 95%CI.56-0.97), and CD4+ T-cell count <350 cells/mm3 (aIRR=0.72, 95%CI 0.53-0.97, versus ≥350 cells/mm3) were associated with lower live-birth rates. There was a non-significant trend towards increased live-birth rates among those using cART compared to non-users (aIRR=1.35, 95%CI 0.99-1.83) in the multivariable model that included variables such as CD4+ T-cell count and viral load. In multivariate models for both HIV-positive and HIV-negative women, time period was not significantly associated with live-birth.
Table 1.
Significant predictors from multivariable model of live birth rate among HIV-negative and HIV-positive women in the WIHS
| HIV-negative | HIV-positive | |||||
|---|---|---|---|---|---|---|
| Variable | aIRR* | 95%CI | aIRR* | 95%CI | ||
| Age 25-29 vs <25 | 0.59 | 0.39 | 0.89 | 0.87 | 0.55 | 1.40 |
| Age 30-34 vs <25 | 0.46 | 0.30 | 0.70 | 0.52 | 0.32 | 0.84 |
| Age >=35 vs <25 | 0.22 | 0.14 | 0.35 | 0.14 | 0.08 | 0.23 |
| Living with Partner vs Married | 1.65 | 1.07 | 2.54 | ------ | ------ | ------ |
| <HS vs >=HS | 1.38 | 1.02 | 1.85 | ------ | ------ | ------ |
| Prior Abortion vs No | 0.73 | 0.55 | 0.98 | ------ | ------ | ------ |
| >=7 drinks/week vs <7 | ------ | ------ | ------ | 0.47 | 0.22 | 0.97 |
| Use Condom vs No | 0.55 | 0.41 | 0.73 | 0.73 | 0.56 | 0.97 |
| Marijuana Use vs No | 0.57 | 0.39 | 0.84 | ------ | ------ | ------ |
| Drug Use vs No | 0.32 | 0.15 | 0.66 | ------ | ------ | ------ |
| cART Use vs No | ------ | ------ | ------ | 1.35** | 0.99 | 1.83 |
| CD4+ T-cell count <350 vs >=350 | ------ | ------ | ------ | 0.72 | 0.53 | 0.97 |
HS = high school; vs=versus, CI=confidence interval, cART=combined antiretroviral therapy
aIRR, adjusted incidence rate ratio;
p=0.058
Poisson mixed model with random intercept for each subject included all variables with significant bivariable models for HIV-positive or negative (p<0.05);
Other variables controlled for in model: race, marital status, education, employment status, WIHS site, prior abortions, number of sexual partners, year, current smoking, alcohol use (>=7 drinks/week verses <7 drinks per week); marijuana use, drug use, prior sexually transmitted infection (STI), any health related issues, and for HIV-positive: viral load and first year on cART.
Variable not included in model as significant in bivariate analysis: income, insurance status, number of male sex partners, previous STI, contraception use
Associations with abortion rate
Bivariable associations with abortion rate are presented in Supplemental Tables 3a and 3b. Notably, among HIV-negative and HIV-positive women, income, marital status, insurance status, contraception use, and number of male sex partners were not associated with abortion rates. For HIV-positive women, cART use was significantly associated with reduced abortion rates (cIRR=0.61, 95%CI 0.44-0.85) while lower viral loads (<4 log10 copies/ml cIRR=1.43, 95%CI 1.03-1.98 versus ≥4 log10 copies/ml) and higher CD4+ T-cell counts (≥350 vs <350 cells/mm3 cIRR=1.82, 95%CI 1.32-2.50) were each significantly associated with increased abortion rates.
Multivariable models for abortion rates for HIV-negative and HIV-positive women are presented in Tables 2. Among HIV-negative women, older age was associated with decreased abortion rates (≥35 versus <25, aIRR=0.07, 95%CI 0.04-0.13), while increased parity (≥3 versus 0, aIRR=3.14, 95%CI 1.66-5.93), having a history of abortion (aIRR=1.56, 95%CI 1.06-2.30), and use of condoms (aIRR=2.18, 95%CI 1.58-3.01) were associated with increased rates of abortion. Further, study site was also associated with abortion rate, with significantly fewer abortions among participants at the Washington, D.C. and Chicago sites compared to the Bronx site (aIRR=0.47, 95%CI 0.22-0.99 and aIRR=0.18, 95%CI 0.06-0.52, respectively).
Table 2.
Significant predictors from multivariable model of abortion rate among HIV-negative and HIV-positive women in the WIHS
| HIV-negative | HIV-positive | |||||
|---|---|---|---|---|---|---|
|
| ||||||
| Variable | aIRR* | 95%CI | aIRR* | 95%CI | ||
| Age 25-29 vs <25 | 0.49 | 0.33 | 0.74 | 0.44 | 0.26 | 0.76 |
| Age 30-34 vs <25 | 0.27 | 0.17 | 0.43 | 0.29 | 0.16 | 0.51 |
| Age >=35 vs <25 | 0.07 | 0.04 | 0.13 | 0.14 | 0.07 | 0.25 |
| Brooklyn vs Bronx | ------ | ------ | ------ | 1.96 | 1.07 | 3.59 |
| DC vs Bronx | 0.47 | 0.22 | 0.99 | ------ | ------ | ------ |
| Chicago vs Bronx | 0.18 | 0.06 | 0.52 | ------ | ------ | ------ |
| Baseline Parity 1-2 vs 0 | 2.55 | 1.54 | 4.23 | 1.73 | 0.99 | 3.03 |
| Baseline Parity >=3 vs 0 | 3.14 | 1.66 | 5.93 | 2.64 | 1.41 | 4.93 |
| Prior Abortion vs No | 1.56 | 1.06 | 2.30 | 1.72 | 1.16 | 2.55 |
| Prior STI vs No | ------ | ------ | ------- | 0.63 | 0.43 | 0.92 |
| Use Condom vs No | 2.18 | 1.58 | 3.01 | 2.40 | 1.52 | 3.79 |
HS = high school; vs=versus, CI=confidence interval, STI= sexually transmitted infection vs=versus, CI=confidence interval
aIRR, adjusted incidence rate ratio;
Poisson mixed model with random intercept for each subject included all variables with significant bivariable models for HIV-positive or negative (p<0.05); Other variables controlled for in model: race, year, site, education, employment status, alcohol use, any health related issue, drug use, prior STI, and for HIV-positive women: cART use, CD4+ T-cell count, first year on cART, viral load.
Variable considered but not included in model as significant in bivariable analysis: income, marital status, insurance status, number of male sex partners, prior non-viable pregnancy, contraception use), current cigarette smoking, current marijuana use.
For HIV-positive women, abortion rates were negatively associated with age (≥35 versus <25, aIRR=0.14, 95%CI 0.07-0.25) and positively associated with prior abortion (aIRR=1.72, 95%CI 1.16-2.55), study site (Brooklyn versus Bronx, aIRR=1.96, 95%CI 1.07, 3.59), and condom use (aIRR=2.40, 95%CI 1.52-3.79). Prior self-reported sexually transmitted infection was associated with decreased abortion rates (aIRR=0.63, 95%CI 0.43-0.92). Time-period, cART use, CD4+ T-cell count and viral load were not associated with abortion rates in the multivariate model.
Discussion
Although reduced pregnancy and live-birth rates have been the reported among HIV-positive versus HIV-negative women 11, 20 during the earlier HIV epidemic, we demonstrate that in the current cART era these rates have increased among HIV-positive women and are now comparable to rates among HIV-negative women. Studies in sub-Saharan Africa have suggested a similar trend towards increasing pregnancy rates with ART use 21, however this trend among women in developed countries has not been previously demonstrated. Increased contraception, sterilization and sexual abstinence may have led to initial drops in pregnancy rates among those living with HIV 22, perhaps driven by fear of transmission, poor overall health status, and stigma. Increases in pregnancy and live-birth rates may be reflective of improved fecundability, improved health, and changing fertility intentions. Fertility intention may be influenced by overall improvement in perceived wellbeing, life expectancy, reduced fear of perinatal HIV transmission, and more positive attitudes about pregnancy among HIV care providers and communities. Women with lower CD4+ T-cell counts, higher viral loads and not using cART continued to have lower live-birth rates. Further, while age-adjusted live-birth rates were significantly increased, when factors such as cART use, viral load and CD4+ T-cell count were included in our models, time period was no longer associated with live-birth rate. This suggests that HIV-related clinical factors play a central role in the increased trend. Interestingly, although cART use, CD4 count, and viral load were significant in the bivariate analysis, after including them in the multivariable model and also adjusting for other important covariates, only CD4 +T-cell count was significantly associated with increased live births rates.
Approximately half of all pregnancies in the US are unintended; among those, 40% will end in induced abortion 23. Estimates for unintended pregnancy among women living with HIV may be much higher 24. A 2014 study among HIV-positive pregnant women found 23% had an unplanned pregnancy, 58% were ambivalent, and only 19% reported a planned pregnancy 14. Previous analysis from the WIHS cohort had documented reduced abortion rates during the early HIV epidemic 11 in conjunction with fewer overall pregnancies. While our data and others have shown a decrease in abortion rates over the last decade among HIV-negative women 25, we demonstrate that the rate among those living with HIV has not altered. Notably, cART use, CD4+ T-cell count, and viral load were not associated with abortion rates among HIV-positive women, suggesting that for many women the complex decision-making regarding pregnancy continuation and abortion may not be strongly influenced by their HIV disease state. Similar to previous literature, predictors of abortion among both HIV-positive and HIV-negative high-risk women include younger age, increased parity and history of having had an abortion 23, 25, 26. These high-risk groups should be targeted for contraceptive counseling.
Condoms were the dominant form of contraception in our cohort. Given high, typical-use pregnancy rates of 18%/year with condom use 27, condoms alone have limited utility for unintended pregnancy prevention. Use of other contraceptives among our cohort was low, with women reporting either a hormonal or a LARC method at only 15% of visits. Ineffective contraception use with a high reliance on condoms alone among WIHS participants has previously been reported, where HIV positive women in this cohort have not experienced an increase in LARC use seen in HIV-negative women28. As contraceptive use was not associated with live-birth rates, we can conclude that many women may be offered or choose less effective methods, do not use them consistently or correctly, and continue with pregnancy when contraceptives fail. Previous studies have demonstrated poor utilization of the most effective long-term contraceptives among women living with HIV 28, despite increasing uptake nationally 29. Long-acting contraceptive options, such as intrauterine devices (IUDs) and contraceptive implants, are safe for HIV-positive and at-risk women, have high continuation rates, and reduce unintended pregnancy rates 30, 31. With potentially increased health engagement among women in HIV care, opportunities for integrated family planning services must be sought to reduce barriers to safe contraception. Educational messaging must shift from condom use alone to encourage dual protection, with a hormonal or LARC method for pregnancy prevention and concurrent use of condoms for effective sexually transmitted infection (STI) and HIV prevention. Novel approaches may be needed to successfully integrate reproductive health services into HIV care.
This study has several limitations. Information on pregnancy outcomes and covariates were based on self-report and are thus prone to potential misclassification; however self-reported data used in other WIHS studies has been strongly correlated with clinical outcomes and several personal self-reported questions gathered throughout the WIHS cohort may not be routinely available in clinical chart reviews or provider generated database evaluations. Study intervals of six months for assessment of time-varying covariates limited our ability to evaluate changes during those intervals; however this is likely to be more generalizable to data that could be collected in a clinical setting. Moreover, we do not have reliable data on pregnancy intention or abortion access. Eligibility criteria in this longitudinal cohort potentially limits external validity. The average age of our cohort is relatively advanced, thus results may not reflect the younger HIV-positive or high-risk HIV-negative women or those with perinatally-acquired HIV. Lastly, we dichotomized CD4 T-cell count and viral load based on predetermined values to reflect poor HIV control, however other lower cut-offs are often used for defining virologic suppression.
In conclusion, we demonstrate that overall pregnancy rates are now similar between HIV-positive and high-risk HIV-negative women, possibly due to improved health status among HIV-positive women coupled with shifting attitudes due to reduced risk of maternal-to-child transmission. With that said, abortion rates have remained consistent and do not appear to be associated with HIV related health variables, indicating that unintended pregnancy among all individuals need to be addressed. Given high failure rates with condom use alone, dual protection with hormonal contraceptives or nonhormonal IUDs should be strongly encouraged for women seeking contraception. Integrating reproductive health services into HIV clinical care can reduce barriers and improve care for high-risk women and provide an important opportunity to address family planning and safe conception practices.
Supplementary Material
Table 1a: Description of baseline characteristics by HIV serostatus
Table 1b: Description of time-varying covariate characteristics by serostatus
Table 2. Unadjusted and age-adjusted pregnancy, live-birth and abortion rates by time period and HIV serostatus
Table 3a: Crude bivariable associations of baseline covariates with live-birth and abortion rates among HIV-negative and HIV-positive women
Table 3b: Crude bivariable associations of time-varying covariates with live-birth and abortion rates among HIV-negative and HIV-positive women
Condensation.
Live-birth rates among HIV-positive women have increased over 2 decades, are now similar to HIV-negative women and associated with ART use.
Acknowledgements
Data in this manuscript were collected by the Women’s Interagency HIV Study (WIHS). The contents of this publication are solely the responsibility of the authors and do not represent the official views of the National Institutes of Health (NIH). WIHS (Principal Investigators): UAB-MS WIHS (Michael Saag, Mirjam-Colette Kempf, and Deborah Konkle-Parker), U01-AI-103401; Atlanta WIHS (Ighovwerha Ofotokun and Gina Wingood), U01-AI-103408; Bronx WIHS (Kathryn Anastos), U01-AI-035004; Brooklyn WIHS (Howard Minkoff and Deborah Gustafson), U01-AI-031834; Chicago WIHS (Mardge Cohen and Audrey French), U01-AI-034993; Metropolitan Washington WIHS (Mary Young and Seble Kassaye), U01-AI-034994; Miami WIHS (Margaret Fischl and Lisa Metsch), U01-AI-103397; UNC WIHS (Adaora Adimora), U01-AI-103390; Connie Wofsy Women’s HIV Study, Northern California (Ruth Greenblatt, Bradley Aouizerat, and Phyllis Tien), U01-AI-034989; WIHS Data Management and Analysis Center (Stephen Gange and Elizabeth Golub), U01-AI-042590; Southern California WIHS (Joel Milam), U01-HD-032632 (WIHS I – WIHS IV). The WIHS is funded primarily by the National Institute of Allergy and Infectious Diseases (NIAID), with additional co-funding from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD), the National Cancer Institute (NCI), the National Institute on Drug Abuse (NIDA), and the National Institute on Mental Health (NIMH). Targeted supplemental funding for specific projects is also provided by the National Institute of Dental and Craniofacial Research (NIDCR), the National Institute on Alcohol Abuse and Alcoholism (NIAAA), the National Institute on Deafness and other Communication Disorders (NIDCD), and the NIH Office of Research on Women’s Health. WIHS data collection is also supported by UL1-TR000004 (UCSF CTSA) and UL1-TR000454 (Atlanta CTSA). Dr. Haddad’s effort is supported by the NICHD (1K23HD078153-01A1).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts of interest: There are neither competing interests nor conflicts of interest among any of the investigators or authors.
This research was presented at the AIDS 2016 conference in Durban, South Africa, July 18-22, 2016.
Contributor Information
Lisa B. HADDAD, Emory University, School of Medicine, Department of Gynecology and Obstetrics, Atlanta, GA..
Kristin M. WALL, Emory University, Rollins School of Public Heath, Department of Epidemiology, Atlanta, GA..
Christina C. MEHTA, Emory University, Rollins School of Public Heath, Department of Biostatistics and Bioinformatics, Atlanta, GA..
Elizabeth T. GOLUB, Johns Hopkins Bloomberg School of Public Heath, Department of Epidemiology, Baltimore, MD..
Lisa RAHANGDALE, University of North Carolina School of Medicine, Department of Obstetrics and Gynecology, Chapel Hill, NC..
Mirjam-Colette KEMPF, University of North Carolina School of Medicine, Department of Obstetrics and Gynecology, Chapel Hill, NC..
Roksana KARIM, University of Southern California, Keck School of Medicine, Department of Preventative Medicine, Los Angeles, CA..
Rodney WRIGHT, Albert Einstein College of Medicine, Department of Obstetrics and Gynecology, Bronx, NY..
Howard MINKOFF, Maimonides Medical Center, Department of Obstetrics and Gynecology, Brooklyn, NY..
Mardge COHEN, Departments of Medicine, John H. Stroger Jr. Hospital of Cook County and Rush University, Chicago, IL..
Seble KASSAYE, Georgetown University School of Medicine, Department of Medicine, Division of Infectious Diseases and Travel Medicine, Washington DC..
Deborah COHAN, University of California San Francisco School of Medicine, Department of Obstetrics and Gynecology, San Francisco, CA..
Igho OFOTOKUN, Emory University, School of Medicine, Department of Medicine, Division of Infectious Diseases Atlanta, GA..
Susan E. COHN, Northwestern University Feinberg School of Medicine, Department of Medicine, Division of Infectious Diseases, Chicago, IL..
References
- 1.STANWOOD NL, COHN SE, HEISER JR, PUGLIESE M. Contraception and fertility plans in a cohort of HIV-positive women in care. Contraception. 2007;75:294–8. doi: 10.1016/j.contraception.2006.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Panel on Treatment of HIV-Infected Pregnant Women and Prevention of Perinatal Transmission. Recommendations for Use of Antiretroviral Drugs in Pregnant HIV-1- Infected Women for Maternal Health and Interventions to Reduce Perinatal HIV Transmission in the United States. .
- 3.PALELLA FJ, JR., DELANEY KM, MOORMAN AC, et al. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. HIV Outpatient Study Investigators. The New England journal of medicine. 1998;338:853–60. doi: 10.1056/NEJM199803263381301. [DOI] [PubMed] [Google Scholar]
- 4.MAY M, GOMPELS M, DELPECH V, et al. Impact of late diagnosis and treatment on life expectancy in people with HIV-1: UK Collaborative HIV Cohort (UK CHIC) Study. BMJ (Clinical research ed) 2011;343:d6016. doi: 10.1136/bmj.d6016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.EUROPEAN COLLABORATIVE S Mother-to-child transmission of HIV infection in the era of highly active antiretroviral therapy. Clinical infectious diseases : an official publication of the Infectious Diseases Society of America. 2005;40:458–65. doi: 10.1086/427287. [DOI] [PubMed] [Google Scholar]
- 6.PALELLA FJ, JR., BAKER RK, MOORMAN AC, et al. Mortality in the highly active antiretroviral therapy era: changing causes of death and disease in the HIV outpatient study. Journal of acquired immune deficiency syndromes. 1999;2006:43–27. doi: 10.1097/01.qai.0000233310.90484.16. [DOI] [PubMed] [Google Scholar]
- 7.MANDELBROT L, TUBIANA R, LE CHENADEC J, et al. No perinatal HIV-1 transmission from women with effective antiretroviral therapy starting before conception. Clin Infect Dis. 2015;61:1715–25. doi: 10.1093/cid/civ578. [DOI] [PubMed] [Google Scholar]
- 8.BLAIR JM, HANSON DL, JONES JL, DWORKIN MS. Trends in pregnancy rates among women with human immunodeficiency virus. Obstetrics and gynecology. 2004;103:663–8. doi: 10.1097/01.AOG.0000117083.33239.b5. [DOI] [PubMed] [Google Scholar]
- 9.HUNTINGTON SE, THORNE C, BANSI LK, et al. Predictors of pregnancy and changes in pregnancy incidence among HIV-positive women accessing HIV clinical care. AIDS (London, England) 2013;27:95–103. doi: 10.1097/QAD.0b013e3283565df1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.SHARMA A, FELDMAN JG, GOLUB ET, et al. Live birth patterns among human immunodeficiency virus-infected women before and after the availability of highly active antiretroviral therapy. American journal of obstetrics and gynecology. 2007;196:541, e1–6. doi: 10.1016/j.ajog.2007.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.MASSAD LS, SPRINGER G, JACOBSON L, et al. Pregnancy rates and predictors of conception, miscarriage and abortion in US women with HIV. AIDS (London, England) 2004;18:281–6. doi: 10.1097/00002030-200401230-00018. [DOI] [PubMed] [Google Scholar]
- 12.KOENIG LJ, ESPINOZA L, HODGE K, RUFFO N. Young, seropositive, and pregnant: epidemiologic and psychosocial perspectives on pregnant adolescents with human immunodeficiency virus infection. American journal of obstetrics and gynecology. 2007;197:S123–31. doi: 10.1016/j.ajog.2007.03.004. [DOI] [PubMed] [Google Scholar]
- 13.SUTTON MY, PATEL R, FRAZIER EL. Unplanned pregnancies among HIV-infected women in care-United States. J Acquir Immune Defic Syndr. 2014;65:350–8. doi: 10.1097/QAI.0000000000000054. [DOI] [PubMed] [Google Scholar]
- 14.RAHANGDALE L, STEWART A, STEWART RD, et al. Pregnancy intentions among women living with HIV in the United States. J Acquir Immune Defic Syndr. 2014;65:306–11. doi: 10.1097/QAI.0000000000000014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.LINAS BS, MINKOFF H, COHEN MH, et al. Relative time to pregnancy among HIV-infected and uninfected women in the Women's Interagency HIV Study, 2002-2009. AIDS (London, England) 2011;25:707–11. doi: 10.1097/QAD.0b013e3283445811. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.BARKAN SE, MELNICK SL, PRESTON-MARTIN S, et al. The Women's Interagency HIV Study. WIHS Collaborative Study Group. Epidemiology. 1998;9:117–25. [PubMed] [Google Scholar]
- 17.BACON MC, VON WYL V, ALDEN C, et al. The Women's Interagency HIV Study: an observational cohort brings clinical sciences to the bench. Clinical and diagnostic laboratory immunology. 2005;12:1013–9. doi: 10.1128/CDLI.12.9.1013-1019.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.TIWARI RC, CLEGG LX, ZOU Z. Efficient interval estimation for age-adjusted cancer rates. Stat Methods Med Res. 2006;15:547–69. doi: 10.1177/0962280206070621. [DOI] [PubMed] [Google Scholar]
- 19.WOOLSON RF, BEAN JA. Mantel-Haenszel statistics and direct standardization. Stat Med. 1982;1:37–9. doi: 10.1002/sim.4780010106. [DOI] [PubMed] [Google Scholar]
- 20.FORSYTH BW, DAVIS JA, FREUDIGMAN KA, KATZ KH, ZELTERMAN D. Pregnancy and birth rates among HIV-infected women in the United States: the confounding effects of illicit drug use. AIDS. 2002;16:471–9. doi: 10.1097/00002030-200202150-00020. [DOI] [PubMed] [Google Scholar]
- 21.MARSTON M, NAKIYINGI-MIIRO J, HOSEGOOD V, et al. Measuring the Impact of Antiretroviral Therapy Roll-Out on Population Level Fertility in Three African Countries. PloS one. 2016;11:e0151877. doi: 10.1371/journal.pone.0151877. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.WILSON TE, MASSAD LS, RIESTER KA, et al. Sexual, contraceptive, and drug use behaviors of women with HIV and those at high risk for infection: results from the Women's Interagency HIV Study. AIDS. 1999;13:591–8. doi: 10.1097/00002030-199904010-00008. [DOI] [PubMed] [Google Scholar]
- 23.FINER LB, ZOLNA MR. Declines in Unintended Pregnancy in the United States, 2008-2011. The New England journal of medicine. 2016;374:843–52. doi: 10.1056/NEJMsa1506575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.LINDSAY MK, GRANT J, PETERSON HB, WILLIS S, NELSON P, KLEIN L. The impact of knowledge of human immunodeficiency virus serostatus on contraceptive choice and repeat pregnancy. Obstetrics and gynecology. 1995;85:675–9. doi: 10.1016/0029-7844(95)00018-m. [DOI] [PubMed] [Google Scholar]
- 25.PAZOL K, CREANGA AA, JAMIESON DJ, CENTERS FOR DISEASE C, PREVENTION Abortion Surveillance - United States, 2012. MMWR Surveill Summ. 2015;64:1–40. doi: 10.15585/ss6410a1. [DOI] [PubMed] [Google Scholar]
- 26.FINER LB, ZOLNA MR. Unintended pregnancy in the United States: incidence and disparities, 2006. Contraception. 2011;84:478–85. doi: 10.1016/j.contraception.2011.07.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.TRUSSELL J. Contraceptive efficacy. Arch Dermatol. 1995;131:1064–8. [PubMed] [Google Scholar]
- 28.SUN M, PEIPERT JF, ZHAO Q, et al. Trends in contraceptive use among women with human immunodeficiency virus. Obstetrics and gynecology. 2012;120:783–90. doi: 10.1097/AOG.0b013e318269c8bb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.BRANUM AM, JONES J. Trends in long-acting reversible contraception use among U.S. women aged 15-44. NCHS Data Brief. 2015:1–8. [PubMed] [Google Scholar]
- 30.DIEDRICH JT, MADDEN T, ZHAO Q, PEIPERT JF. Long-term utilization and continuation of intrauterine devices. Am J Obstet Gynecol. 2015;213:822, e1–6. doi: 10.1016/j.ajog.2015.08.077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.REEVES MF, ZHAO Q, SECURA GM, PEIPERT JF. Risk of unintended pregnancy based on intended compared to actual contraceptive use. Am J Obstet Gynecol. 2016 doi: 10.1016/j.ajog.2016.01.162. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table 1a: Description of baseline characteristics by HIV serostatus
Table 1b: Description of time-varying covariate characteristics by serostatus
Table 2. Unadjusted and age-adjusted pregnancy, live-birth and abortion rates by time period and HIV serostatus
Table 3a: Crude bivariable associations of baseline covariates with live-birth and abortion rates among HIV-negative and HIV-positive women
Table 3b: Crude bivariable associations of time-varying covariates with live-birth and abortion rates among HIV-negative and HIV-positive women