Abstract
BACKGROUND
We have previously described our technique of Robotic-Assisted Giant Paraesophageal Hernia Repair (RA-GPEHR). The purpose of this study was to report our initial experience, early outcomes and learning curve with RA-GPEHR using a four-arm robotic platform.
METHODS
24 consecutive patients presenting with symptomatic giant paraesophageal hernias (GPEH) underwent RA-GPEHR from April 2011 to February 2014. Peri-operative data and short-term patient outcomes were assessed by retrospective review of a prospectively maintained database.
RESULTS
Median age was 62 years (range 44 – 84). 15 (63%) patients underwent fundoplication and 9 (37%) gastropexy. Median procedure time was 277 minutes (range:185–485) and decreased steadily over the experience. There were no intra-operative complications or surgical mortality. No patients experienced dysphagia in the early post-operative period.
CONCLUSIONS
RA-GPEHR is safe, with reported short-term operative and functional outcomes similar to conventional laparoscopic approaches. The initial learning curve appears relatively short for experienced minimally invasive esophageal surgeons.
INTRODUCTION
Minimally invasive repair of giant para-esophageal hernias (GPEH) has been established as a safe and durable approach with acceptable rates of morbidity and minimal mortality (1). The learning curve may be considerable and the technical aspects of these operations can be demanding, requiring extensive adhesiolysis, hernia sac dissection and esophageal mobilization within the “distant” and limited confines of the mediastinum, where maintaining visualization for extended periods of time can be challenging. Technological innovations of current robotic surgical systems, including improved instrument dexterity, additional arms allowing for self “first”-assistance and stable optics under direct operator control, may be of particular advantage to the minimally invasive surgeon within such confined anatomic spaces.
Although published reports of robotic assisted approaches to these operations are early, scarce, and limited in scope, they do suggest a technical advantage, particularly during mediastinal dissection and crural repair (2–4). Also, these studies are variable in their reporting of complications and operative outcomes. Finally, the learning curve for these operations also remains largely unaddressed.
The purpose of this study was to review an early single-institution experience with RA-GPEHR with particular emphasis on identifying learning curves based on operative times and complication profiles. These outcomes may help inform institutional guidelines for certification and credentialing of surgeons performing these procedures. We also present a review of literature with early single institution reports for RA-GPEHR.
MATERIALS AND METHODS
Consecutive patients presenting to a single institution for repair of giant paraesophageal hernias (GPEH), defined here as Type III hiatal hernias with ≥ 30% of stomach identified within the thorax on imaging studies, were reviewed. Patients were pre-operatively assessed by esophagoscopy and contrast esophagram. Symptomatology was identified by patient history and included findings of dysphagia, regurgitation, early satiety, history of aspiration and/or associated pneumonias, and postprandial chest pain.
Demographic, perioperative, and outcome data were collected from review of patient charts. Complications were graded according to the Common Terminology Criteria for Adverse Events (CTCAE v. 3.0). Our Internal Review Board granted a waiver for retrospective studies.
Our technique of RA-GPEHR has been adapted from previously described standard laparoscopic approaches (1, 5). A detailed description of our RA-GPEHR has been published (6). Briefly, the primary steps of the procedure include reduction of the stomach from the hernia space, sac excision with high mediastinal dissection, gastric fat pad dissection to adequately expose the gastroesophageal junction, establishment of sufficient intraabdominal esophageal length with or without gastroplasty, tension-free approximation of the hiatus with or without use of mesh, and performance of a fundoplication or gastropexy. A 4-arm robotic platform was used for all operations (DaVinci Surgical System, Intuitive Surgical, Sunnyvale, CA).
RESULTS
24 patients with a median age of 62 years underwent RA-GPEHR between April 2011 and February 2014. Demographics, peri-operative data, and complications are summarized in Table I. The majority of patients were women (19/24, 79%) and underwent fundoplication (15/24, 63%), the majority of which had Nissen procedures (14/24, 58%). Mesh was used in only 2 patients (2/24, 8%), and only 1 patient (4%) required wedge gastroplasty. The median age of patients receiving fundoplication was significantly less compared to those undergoing gastropexy (59 years vs. 82 years, p-value 0.000002). Two cases were reoperations, both for previous failed repairs of intra-thoracic stomach, one with mesh and Nissen fundoplication, and one with neither fundoplication nor gastropexy.
Table 1.
RA-GPEH patient demographics and operative data.
| Variable | Number (%), or median (range) |
|---|---|
| Total Patients | 24 |
| Fundoplication | 15 (63%) |
| Nissen | 14 (58%) |
| Toupet | 1 (4%) |
| Gastropexy | 9 (38%) |
| Mesh Used | 2 (8%) |
| Gastroplasty Required | 1 (4%) |
| Median Age years | 62 (44–84) |
| Fundoplication | 59 (44–73) |
| Gastropexy | 82 (71–84) |
| Female | 19 (79%) |
| Operative Time minutes | 277 (185–485) |
| 1st half (12 pts.) | 355 (185–485) |
| 2nd half (12 pts.) | 257 (201–411) |
| First 5 cases | 385 (233–485) |
| Last 5 cases | 241 (218–287) |
| Fundoplication | 320 (201–485) |
| Gastropexy | 237 (185–418) |
| LOS days | 4 (1–14) |
| Estimated Blood Loss mL | 25 (15–300) |
| Complications | |
| Patients with ≤ Grade 2 | 5 (21%) |
| Patients with ≥ Grade 3 (Major) | 4 (17%) |
| Specific Complications by Grade (CTCAE v. 4.0) | |
| Total Grade 2* | |
| Ileus | 2 (8%) |
| Constipation | 1 (4%) |
| Cardiac Ischemia/Infarction | 1 (4%) |
| Urinary Retention | 1 (4%) |
| Diarrhea | 1 (4%) |
| Total Grade 3# | |
| Pulmonary Embolus | 1 (4%) |
| Septic Thrombophlebitis | 1 (4%) |
| C. Difficile Colitis | 1 (4%) |
| Diarrhea | 1 (4%) |
| Hypoglycemia | 1 (4%) |
| Total Grade 4 | |
| Acute Lung Injury | 1 (4%) |
Two Grade 2 complications occurred in one patient.
Three Grade 3 complications occurred in one patient.
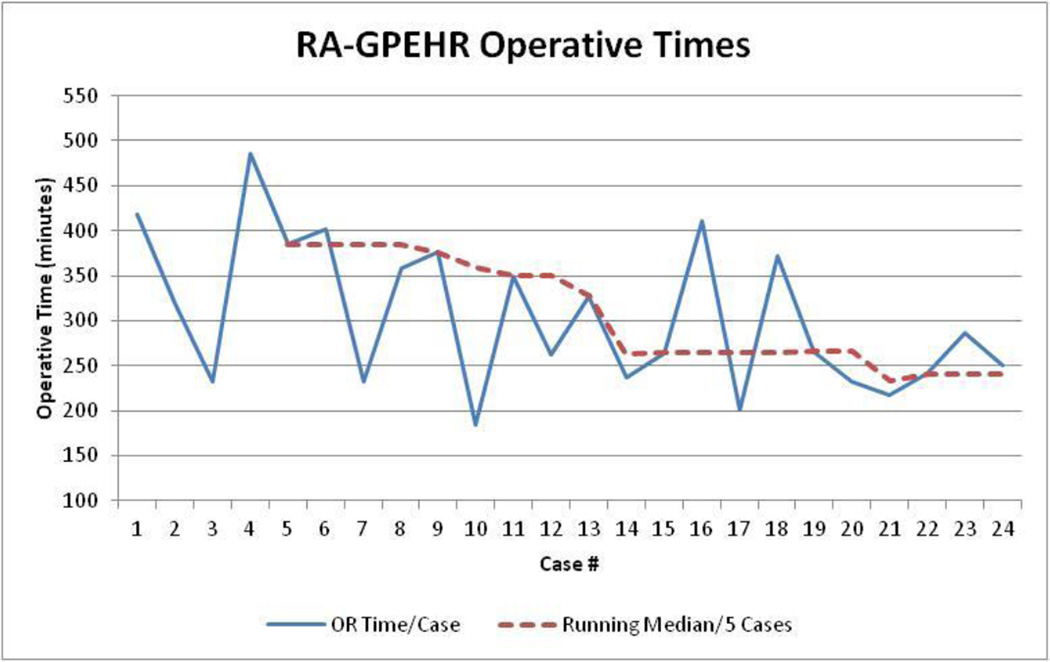
Median operative time decreased by 98 minutes between the first and second half of the series, which is clinically relevant although not statistically significant (Mean 334 vs 275 minutes, P = 0.079). As clinically anticipated, median operative time was also shorter for patients undergoing gastropexy compared to fundoplication (237 vs 320 minutes, P = 0.204). Running median operative time per five cases is shown in Figure 1. There were no conversions to open procedures. Lengths of stay between the first and second half of cases were not significantly different (Mean 5 vs. 3.9 days, p-value 0.44).
Figure 1.
RA-GPEHR operative times
Four patients (17%) had major complications. These included a patient with severe but self-limited non-infectious diarrhea requiring readmission for hydration, and a patient with unexplained acute lung injury requiring intubation that resolved within 24 hours. A diabetic patient was found to be severely hypoglycemic with mental status changes and hypotension at the first post-operative clinic visit and required concentrated dextrose intravenously. The patient was eating a normal soft diet and had no dysphagia or other reported post-operative symptoms. The fourth patient was an 82-years-old male with significant CAD who had post operative NSTEMI with mild elevation in troponin. This was successfully managed medically and patient was discharged home on POD 10.
DISCUSSION
This study has several limitations. However, it highlights that RA-GPEHR can be safely adopted with comparable results by surgeons familiar with minimally invasive repair of paraesophageal hernias. There is a clear trend towards improved operative times as operator experience grows while maintaining shorter lengths of stay and EBL as compared to open approach. These results are safely reproducible as noted by other authors as well. The decision to perform fundoplication vs. gastropexy was based on patient symptomatology with dysphagia and pain being the primary symptoms in gastropexy group whereas GERD, regurgitation and aspiration were primary presenting complaints in fundoplication group. 18/24 (75%) had history of previous abdominal surgeries, however, this was not a deterrent to robotic approach and there were no conversions to open approach. There was excellent resolution of symptoms as assessed by QOL analysis pre and post repair with only two patients requiring PPIs on follow up.
Reports of RA-GPEHR, including the current study, are limited to retrospective single institutional series and are summarized in Table 2. The first series was reported by Ruurda et al., although no operative description and little clinical data was given (4). In a follow-up report from the same institution, Draaisma et al. reported on 40 patients undergoing RA-GPEHR with one-year follow-up (2). Overall, this institutional series had a low operative time (Median 127 (Range 80–210 min) with most patients not receiving a fundoplication. Of note, the authors report three reoperations in the early post-operative period, including an open drainage and repair of an esophageal perforation and early failed cruroplasty with re-herniation of stomach. Braumann et al. reported limited results of these operations in two publications covering 14 patients (7). While there is some discrepancy in the times reported between the two studies, the length of operation was consistent with other reports. Complications were not reported in these studies.
Table 2.
Literature Review
| Author, Year | Study Type | Approach | N | Fundoplication | Mesh | OR Time min | EBL | Complications | LOS | Comments |
|---|---|---|---|---|---|---|---|---|---|---|
| Ruurda, 2005a | Retrospective Case- Series |
32 | NR | NR | 130 (85–210) | NR | 28.1% | 5 (2–39) | Esophageal perforation converted | |
| Draaisma, 2008a | Retrospective Case- Series |
RA-GPEHR | 40 | 10 Nissen 2 Toupet 1 Dor |
0 | 127 (80–210) | 50 (70– 100) |
20.0% | 4.5 (2– 39) |
Esophageal perforation converted, 3 (7.5%) reoperations w/in 30 days |
| Braumann, 2005b | Retrospective, Case- series |
RA-GPEHR | 6 | 4 Dor | 0 | 222.5 (170– 285) |
NR | 0% | 4.5 (4–5) | Manuscript unclear on number of patients |
| Braumann, 2008b | Retrospective, Case- Series |
RA-GPEHR | 14 | 0 | 134(80–240) | NR | 6.5 | OR time incorrectly reported, patients not reported? |
||
| Seetharamaiah, 2013 | Retrospective, Case- series |
RA-GPEH | 19 | 3 Nissen | 16 | 184.5±96.2(76 –395)* |
NR | 10.5% | 4.3(2– 22)* |
ACell, fibrin glue (Evicel) 9 cases, post-op complications not reported |
| Gehrig, 2013 | Retrospective, Comparative Case- Control |
Open CLS RA-GPEHR |
13 17 12 |
6 9 6 |
3 7 5 |
134±52(65– 241)* 168±42(130– 290)* 172±31(115– 220)* |
250±19 1(50– 600)* 24±42(0 –150)* 33±85(0 –300)* |
46.2% 11.8% 8.3% |
12±3.7(6 –20)* 7±1.6(5– 10)* 8±3.9(5– 19)* |
Compared open surgery, conventional laparoscopy, and robotic laparoscopy, post-op bleeding in RA group required laparotomy |
| Sarkaria, current study | Retrospective Case- Series |
RA-GPEHR | 24 | 14 Nissen 1 Toupet 9 Gastropexy |
2 | 277 | 25 (15– 300) |
17% Major 33% Overall |
4 (1–14) |
Results are median and range unless otherwise noted
Reported as mean
Overlapping patient cohorts
Overlapping patient cohorts
In a series of 19 patients, Seetharamajah et al. reported similar times (Mean 184.5±96.2 min) and preferentially used biological mesh in the majority of cases without a fundoplication (8). There was one conversion to an open repair in a patient who presented emergently with compromise of the gastric wall requiring partial gastrectomy. Post-operative complications are not clearly delineated, although one patient developed dysphagia two days after surgery and was treated successfully with repeated endoscopic pneumatic dilation.
Gehrig et al. compared cohorts of patients undergoing RA-GPEHR, conventional laparoscopic GPEHR, and open GPEHR (3). They showed feasibility and safety of robotic approach as compared to open and laparoscopic approaches. Overall, they reported an increase operative time for robotic and laparoscopic approaches as compared to open repair (Mean 172±31 vs. 168±42 vs. 134±52 min); however, they reported improved blood loss (33±85 vs. 24±42 vs. 250±191 cc) and shorter hospital stay (5 days less) for robotic and laparoscopic approaches as compared to open repair.
CONCLUSIONS
For surgeons proficient with LA-GPEHR, transition to a robotic approach is safe and has a reasonably short learning curve. Short-term data from several early single institution case series are encouraging and show at least comparable operative outcomes to those with LA-GPEHR. Additionally, superior ergonomics and self-assist feature with the fourth robotic arm improves operator efficiency and enhances surgeon’s capability to perform technically challenging mediastinal dissection. Higher cost associated with RA-GPEHR remains a potential significant detractor to this approach, especially in the current relative infancy of robotic technology. While decreasing costs can be expected with future development of robotic platforms, broad utilization of these approaches in the immediate healthcare environment may be limited until further high quality clarification of their fiscal impact is apparent.
Acknowledgments
This research was funded in part through the National Institutes of Health/National Cancer Institute (NIH/NCI) Cancer Center Support grant P30 CA0008748.
REFERENCES
- 1.Luketich JD, Nason KS, Christie NA, Pennathur A, Jobe BA, Landreneau RJ, et al. Outcomes after a decade of laparoscopic giant paraesophageal hernia repair. The Journal of thoracic and cardiovascular surgery. 2010;139(2):395–404. e1. doi: 10.1016/j.jtcvs.2009.10.005. PubMed PMID: 20004917; PubMed Central PMCID: PMC2813424. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Draaisma WA, Gooszen HG, Consten EC, Broeders IA. Mid-term results of robot-assisted laparoscopic repair of large hiatal hernia: a symptomatic and radiological prospective cohort study. Surgical technology international. 2008;17:165–170. PubMed PMID: 18802897. [PubMed] [Google Scholar]
- 3.Gehrig T, Mehrabi A, Fischer L, Kenngott H, Hinz U, Gutt CN, et al. Robotic-assisted paraesophageal hernia repair--a case-control study. Langenbeck's archives of surgery / Deutsche Gesellschaft fur Chirurgie. 2013;398(5):691–696. doi: 10.1007/s00423-012-0982-0. PubMed PMID: 22846911. [DOI] [PubMed] [Google Scholar]
- 4.Ruurda JP, Draaisma WA, van Hillegersberg R, Borel Rinkes IH, Gooszen HG, Janssen LW, et al. Robot-assisted endoscopic surgery: a four-year single-center experience. Digestive surgery. 2005;22(5):313–320. doi: 10.1159/000088628. PubMed PMID: 16192731. [DOI] [PubMed] [Google Scholar]
- 5.Nason KS, Luketich JD, Witteman BP, Levy RM. The laparoscopic approach to paraesophageal hernia repair. Journal of gastrointestinal surgery : official journal of the Society for Surgery of the Alimentary Tract. 2012;16(2):417–426. doi: 10.1007/s11605-011-1690-8. PubMed PMID: 22160778; PubMed Central PMCID: PMC4114521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Karush J, Sarkaria IS. Robotic-Assisted Giant Paraesophageal Hernia Repair and Nissen Fundoplication. Operative Techniques in Thoracic and Cardiovascular Surgery. 18(3):204–214. [Google Scholar]
- 7.Braumann C, Menenakos C, Rueckert JC, Mueller JM, Jacobi CA. Computer-assisted laparoscopic repair of "upside-down" stomach with the Da Vinci system. Surgical laparoscopy, endoscopy & percutaneous techniques. 2005;15(5):285–289. doi: 10.1097/01.sle.0000183254.81560.e8. PubMed PMID: 16215489. [DOI] [PubMed] [Google Scholar]
- 8.Seetharamaiah R, Romero RJ, Kosanovic R, Gallas M, Verdeja JC, Rabaza J, et al. Robotic repair of giant paraesophageal hernias. JSLS : Journal of the Society of Laparoendoscopic Surgeons / Society of Laparoendoscopic Surgeons. 2013;17(4):570–577. doi: 10.4293/108680813X13654754534594. PubMed PMID: 24398199; PubMed Central PMCID: PMC3866061. [DOI] [PMC free article] [PubMed] [Google Scholar]