Abstract
Background
Teens often have inadequate asthma self-management and control. However, little is known of their perceptions of or rationales for self-management behaviors.
Objectives
To explore how teens self-manage asthma, including experiences, perceptions, responses to and reporting of symptoms.
Methods
A case-based, qualitative-descriptive design was used. Data were collected from minority and non-minority teens with controlled and uncontrolled asthma and their respective parents (N=28). There were four data-collection points, including: (1) a primary teen interview; (2) parent interview; (3) two-week self-management voice-diary; and (4) follow-up teen interview, incorporating symptom-response card-sorting to map symptoms and associated self-management responses. Seventy data sources were included in the analysis.
Results
Teens thought of their asthma symptoms as normal or unusual relative to their personal baseline symptom pattern; Those with uncontrolled asthma normalized higher levels of asthma symptoms than their counterparts with controlled asthma. Second, teens’ decisions to treat symptoms of asthma with rescue medication were based on perceived benefits, burdens and accessibility of treatment balanced against perceived normalcy of symptoms. Teens with uncontrolled asthma had substantially higher treatment thresholds and delayed responses to symptoms compared to controlled peers. Third, teens never reported perceived normal symptoms of asthma to parents or providers, who were thus only aware of unusual or visible/audible symptoms.
Conclusions
Teen’s perceptions of symptoms and understanding of what is normal is the basis for self-management decisions. Improving self-management will likely entail modifying perceptions of symptoms and benefits/burdens of treatment to achieve healthier self-management patterns.
Keywords: Adolescent, Asthma, Medication compliance, Qualitative research, Self-management, Symptom assessment
Introduction
Self-management is central to controlling asthma and preventing morbidity and mortality [1, 2]. Clinicians and researchers report that many teens with asthma have inadequate self-management and therefore suboptimal asthma control [3, 4]. Of these, minority teens often have greater disease severity, higher rates of uncontrolled asthma, and worse outcomes than non-minority peers [5].
While it is reported that teens often ignore and undertreat treat symptoms [5–7], little is known of their perceptions of self-management, or rationales underlying self-management responses [8–10]. It is also unknown how perceptions and experiences may differ between those with controlled versus uncontrolled asthma, or between minority versus non-minority teens. Understanding teens’ self-management requires not only assessing behaviors, but also understanding the diverse experiences and ways of thinking that are the basis for behaviors [8, 11]. Therefore, the purpose of this study was to explore teens’ experiences and perceptions of asthma self-management. Specific aims were (1) to explore how teens manage their asthma and what is important to them from the perspective of teens and their parents; and (2) to compare self-management between minority and non-minority teens with controlled and uncontrolled asthma.
Methods
The Teens’ Experiences of Asthma study (TEA Study) was approved by the University of Rochester Institutional Review Board [12]. A case-based, qualitative-descriptive design was used [13]. Cases, constructed around teen-parent dyads, contained four data-points collected over a one-month time period. Each dyad comprised one teen and a respective parent. Data from each case included: (1) a first open-ended teen interview; (2) a parent interview; followed by (3) a two-week self-management voice-diary; and concluding with (4) a second teen interview incorporating symptom-response (S/R) card-sorting to map each teen’s usual pattern of asthma symptoms and respective self-management behaviors [14].
Setting, sample and sampling method
Dyads were recruited from the Pediatric Pulmonary Department (n=5), prior study subjects (n=5), surrounding community (n=4), and Emergency Department (n=1) of a medical center in Upstate NY. Subjects were recruited from a variety of settings to increase diversity of perspectives. A two-step criterion-based purposeful sampling strategy was used [15]: dyads were first selected for controlled (50%) versus uncontrolled persistent asthma, and then by African American or Hispanic/Latino racial minority (50%) versus non-minority status [16]. Eligible teens were English-speaking, ages 13 to 17, with mild, moderate or severe persistent asthma, and no other major medical/psychiatric diagnoses. Eligible parents were English-speaking, living with the teen, and involved in their asthma management. Sample size was determined by data saturation [13, 17]. In total, 115 dyads were screened over eight months. Eighteen met eligibility and criterion sampling requirements: two declined to participate; one could not be reached after screening. Parental consent and permission, and teen assent, were obtained for fifteen. After initial consent, contact was lost with one dyad who were homeless and could not be reached for interviews. A total of 14 dyads (28 participants) completed all phases, yielding 42 interviews (28 teen; 14 parent), 14 voice-diaries, and 14 card-sorts.
Data collection
Interviews were conducted in participants’ homes by the first author. Participants were unacquainted or minimally acquainted with the interviewer, but were aware of the interviewer’s background and reasons for conducting the study.
First Teen and Parent Interview
Demographic data and measures of asthma severity and control were obtained prior to first interviews. Demographics included subject age, gender, years with asthma, prescribed asthma medications, approximate household income, smoking status, housing type, insurance type, parent employment and marital status. Severity and control were obtained by self-reported frequency of symptoms, nighttime wakening, activity limitations, rescue inhaler use, and oral steroid use. Asthma was classified as mild, moderate or severe persistent, and controlled versus uncontrolled according to the National Heart Lung and Blood Institute (NHLBI) guidelines [16]. Open-ended semi-structured interviews took approximately one hour. Topics explored were perceptions of and experiences with asthma self-management in different contexts, usual symptoms, responses, and rationales. Parents and teens were asked similar questions. Interview protocols can be seen online (Supplemental Data 1 and 2).
Voice-diary
Teens made daily diary recordings (1 to 8 minutes) about their self-management for two weeks. A guide was provided (Supplemental Data 3), but teens could elect to discuss any asthma related topic. Diaries were designed to capture concurrent experiences, symptoms, responses, and thinking.
Second Teen Interview
Follow-up questions, derived from review of teens’ diaries and first interviews, were used to further explore asthma experiences. Each teen completed a Symptom/Response (S/R) card-sort [14]. A list of each teen’s asthma symptoms and responses to symptoms was derived from their first interview and voice-diary. Items were written in the teens own words on 3×5″ index cards, one item per card. Teens first reviewed and corrected cards as needed to reflect their experience. Using the cards, teens then mapped their usual symptom pathway, placing self-management responses adjacent to symptoms triggering that response. Lastly, they discussed their pattern of asthma symptoms and self-management responses within varying contexts, applied it to specific situations (e.g., home, school, sports, etc.), and explained rationales for self-management behaviors. Interviews were open-ended, lasting approximately 1 hour.
Data Analysis
Recorded interviews and voice diaries were transcribed, verified, and uploaded into ATLAS.ti, along with card-sort images. In total, 70 sources of data were included in the analyses. First coding cycle was in vivo and open coding [18]. Next, process coding was used to identify patterns and processes of self-management within and across cases [18, 19]. Lastly, codes were synthesized to develop themes from the data and refine key ideas. S/R card sorts were first analyzed within cases by examining images in conjunction with associated narratives, and then coded across cases with attention to similarities and differences in symptom-response pathways and underlying thought processes. Analysis was performed by JM and coding decisions reviewed and themes developed with HR, SN, and AB.
Validity and Trustworthiness
Measures to maximize validity and trustworthiness of findings included: (1) writing of structured memos after each interview and during data analysis; (2) member checking for the purposes of clarifying, extending, and exploring convergent/divergent views; and (3) peer-debriefing with experienced asthma and qualitative researchers [13]. Substantiating quotes in this manuscript are marked “T” (teen) or “P” (parent), followed by the case number to increase transparency.
Results
Demographics
As seen in Table 1, household income ranged from $10,000 to $170,000 (mean 60,000; SD 39,170): 21.4% of dyads were below poverty level; 50% were low-income; and 57.1% had public insurance [20]. Many teens reported having had asthma since they were born (mean 10.93 years; SD 4.65), with an unclear age of diagnosis.
TABLE 1.
Demographics
| Teen N (%) | Parent N (%) | |
|---|---|---|
| Race/Ethnicity | ||
| African American | 4 (28.6%) | 5 (35.7%) |
| Bi-racial | 4 (28.6%) | 2 (14.1%) |
| Caucasian | 5 (35.7%) | 7 (50%) |
| Hispanic/Latino | 1 (7.14%) | – |
| Female gender | 7 (50%) | 12 (86%) |
| Teen age | ||
| 13–15 | 8 (57.1%) | |
| 16–17 | 6 (42.9%) | |
| Taking ICS | 11 (79%) | |
| NHLBI Asthma Severity | ||
| Mild persistent | 3 (21.4%) | |
| Moderate persistent | 8 (57.1%) | |
| Severe persistent | 3 (21.4%) | |
| NHLBI Asthma Control | ||
| Controlled | 7 (50%) | |
| Not controlled | 7 (50%) |
Severity and Control
By retrospective assessment of symptom frequency, using NHLBI criteria, teens were found to have mild (21.4%), moderate (57.1%), and severe persistent asthma (21.4); of these, 50% classified as uncontrolled [16]. In contrast, review of interview and diary data (baseline, concurrent, and 1-month) indicated that a much higher percentage of sample teens had uncontrolled asthma (86%), with greater severity (7.1% mild; 50% moderate; 42.9% severe) than revealed on standard screening.
Key Findings
Both parent and teen data supported three key findings relating to assessing, managing and communicating asthma symptoms: (1) Teens conceptualized asthma symptoms as normal or unusual relative to baseline symptom patterns; (2) Within a given context, teens decided when to treat with rescue medication by weighing symptom normalcy versus benefits, burdens and accessibility of treatment; and (3) Teens did not report normal symptoms of asthma to parents or providers.
Assessing: Teens conceptualize symptoms as “Normal” or “Unusual”
Symptoms that occurred regularly, and that were without obvious negative consequences, were often referred to as normal symptoms. Teens did not consider their normal symptoms to be serious or concerning. As one boy expressed,
It’s just my normal back of the mind symptoms. If it’s something like [wheezing] I usually won’t deal with it, because it happens so often. (T09)
Teens had variable definitions of normal that aligned closely with their baseline asthma control. For example, those with uncontrolled asthma often considered daily wheezing normal, whereas better-controlled teens did not. Because normal symptoms were not considered serious, they were overlooked, ignored, and quickly forgotten.
Based on parents’ and teens’ descriptions of symptoms, we identified five key components in assessment of normalcy: (1) Is this kind of symptom normal for me?; (2) Is it happening more often than usual?; (3) How bad is it?; (4) Is it getting better or worse?; and (5) Is it lasting longer than usual? These are described below, with substantiating teen and parent quotes presented in Table 2.
TABLE 2.
Teens’ assessment of symptom normalcy by symptom characteristics
|
Symptom Type: Is this kind of symptom normal for me? |
T09: Coughing is, like a pretty big milestone because it’s just a lot less usual than the rest of these symptoms—because chest tightness, wheezing, those are all kind of like, non-stop, … most of the time I don’t notice them. (NWC) T06: It wasn’t that bad. I didn’t wheeze, it was just shortage of breath and trying to catch my breath back. (NWC) T11: [Wheezing] is noticeable. I mean you hear it and it’s like, ‘Uh oh.’ (WC) T12: there’s this weird feeling that I get—it’s different than a normal tightness, and it makes it harder to breathe than normal tightness is. (WC) T10: I’m getting like a tightness in my chest but I don’t go to the nurse for it cause I was like that’s normal you know, that’s normal for me so I was ok with it… I think something like [coughing]—that’s normal. (WC) P07: I think she pays attention to it depending on how the cough is. (NWC) |
|
Symptom Frequency: Is it happening more often than usual? |
T15: [Symptoms] like two times [a day is ok] three times is getting there, four times is just too much…it’s just going out of hand now, it’s just too many times a day. (VPC) T04: If I do my [rescue] inhaler and I have to do it an hour later, it’s like, “What was that? Like it shouldn’t be that quick.” I usually try and do my inhaler like twice a day… like once in the morning, once in the afternoon. Three times a day I feel like it’s kind of pushing it. It’s like, “Wow! I have to do this three times a day. That’s a lot. … I’d like to go back to my old normal where I could only do my inhaler once a day (NWC) T09: [If it happens] every day for a prolonged amount of time. It’s more another one of those red flags where this is unusual for my asthma symptoms (VPC)) T05: Normally [symptoms] stay away for a good, good five, six hours…. if you had them continuously—like now, five minutes from now, five minutes from that, two minutes from that, three minutes from that, that shows something changed … and that it’s a problem (NWC) |
|
Symptom Severity: How bad is it? |
T05: It depends on how bad the cough gets (NWC) P01: When it’s not that bad, she can breath in cool air…if it’s bad… she takes her pump. It’s not as bad as it was…so she’s good. As long as she can maintain, she’s fine. (VPC) T09: I had like a tight chest and I, was wheezing a little …but it wasn’t a problem. I mean …it wasn’t, inhibiting me from really doing anything. It’s just noticeable… wheezing is the least severe …then coughing …then more severe would be coughing where you could taste the blood …and it’s more painful and your chest gets tighter and tighter (VPC) P13: overall, she doesn’t really worry much unless it’s to the point where she almost can’t function. (NWC) T10: When I’m just a little short of breath… that’s fine cause I know that’s normal for me. … I get shorted of breath or something like that and its unreasonable, it’s very like harsh on me, then yes that’s a problem. (WC) T04: I didn’t have the normal tightness in my chest that I usually do…this was really tight, so it wasn’t a normal thing. … my normal used to be no problem with asthma but in the past 6 months it’s changed to just being ‘oh it’s a little bit tight’… so I just I’ve learned to live with a little bit of like pain. (NWC) T08: My chest is tightened up, unusually tight (WC) |
|
Symptom Duration and Progression Is it getting better or worse? Is it lasting longer than usual? |
T07: Mine [are] normal if they go away quicker. (NWC) P13: Even if she had to use her inhaler every day. and the tightness went away, she’d be fine with it. …[unless] it got to a point where it wasn’t going away. (WC) T05: it’s not a big concern to me unless the problems are progressing … (NWC) T02: My asthma symptoms were coming, and it was like, getting worse … if you let it go on, it could get worse (WC) T04: I was in the normal amount of pain when I went to use my inhaler, it’s like the pain hadn’t increased, but when I did my inhaler, I wasn’t getting as much relief as I normally do. (NWC) T10: You won’t really notice, it would be like “okay, it’s going away,” (WC) T14: It would normally get better in five minutes. (WC) T12: It usually goes away pretty quickly. |
Notes: WC=Well-controlled; NWC=Not well-controlled; VPC=Very poorly-controlled
Is this kind of symptom normal for me?
Certain types of symptoms were considered normal, whereas others were not. In general private symptoms (e.g. mild chest tightness, mild shortness of breath) were tolerated more than those that were public (e.g. audible wheezing and coughing). Teens indicated public symptoms caused greater embarrassment and were harder to hide. Most (86%) accepted some level of chest tightness as normal. Often, coughing was not recognized as a symptom of asthma. As one teen explained, “I wouldn’t put it as a symptom…[it’s a] cold obviously….I just don’t think I’ve ever like had an asthma cough” (T11).
Is it happening more often than usual?
Frequency of symptoms was also assessed relative to each teen’s baseline pattern. Symptom frequency aligning with the teen’s usual pattern was considered normal; frequency exceeding the baseline pattern was considered unusual and concerning.
How bad is it?
Severity was assessed by degree of discomfort experienced, and extend to which symptoms interfered with activities. Universally, symptoms causing greater discomfort (e.g. severe chest pain, severe shortness of breath), or interfering with important activities (e.g. sports, social activities) were less tolerated.
Is it getting better or worse? Is it lasting longer than usual?
Symptoms with spontaneous resolution were considered less concerning than those that persisted or worsened. Worsening was a major indicator symptoms were no longer normal. Symptoms lasting longer than usual were also considered unusual.
Summary
Symptoms were viewed as normal or unusual relative to each teen’s baseline pattern. Teens regularly assessed whether symptoms fell within, or exceeded, their usual type, frequency, severity, duration and progression of asthma symptoms. Consistently, teens with uncontrolled asthma normalized greater severity, frequency and duration of symptoms than peers with controlled asthma. Those with poorly controlled asthma accepted very high levels of symptoms for extended periods before considering it unusual.
Managing: Deciding how to respond—“It’s like weighing the pros and cons”
Teens’ management of symptoms incorporated a range of non-pharmacologic (e.g. waiting, slowing down, drinking water, holding breath) to pharmacologic responses (e.g. taking cold medicine, using inhaler). Most (86%) preferred non-pharmacologic strategies when possible, as using a rescue inhaler signified to teens that their asthma was less controlled. Each teen identified a specific point in their usual symptom pathway at which they typically used rescue medication. This point was designated the treatment threshold. As one boy explained his decisions of when to treat symptoms, “It’s less of the amount [of symptoms] or if it’s constant—it’s more just if it reaches that threshold …” (T09).
Individual treatment thresholds were based on personal cost-benefit analyses, in which teens weighed three components: (1) symptom normalcy versus (2) the benefits/burdens, and (3) accessibility of treatment. Based on their prior experiences and current symptom context, teens treated if symptoms were unusual or sufficiently bothersome, and benefits outweighed burdens of medicating, and medication was considered accessible. Figure 1 depicts the decision-making pathway that teens used to determine when to treat asthma symptoms with rescue medication.
FIGURE 1.
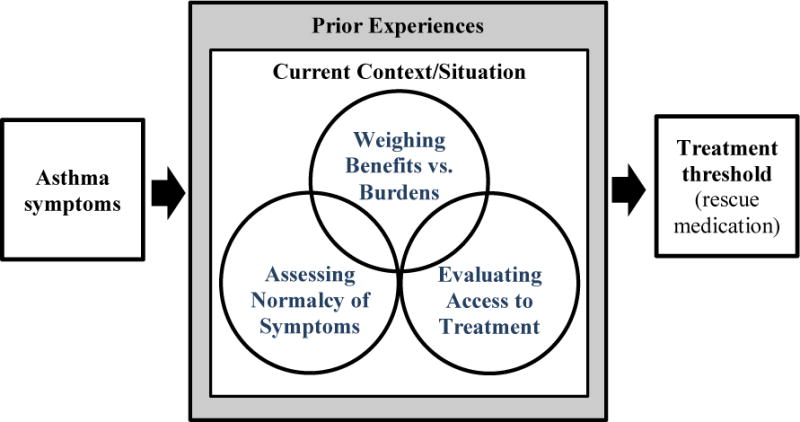
Process for deciding when to treat asthma symptoms with rescue medication
Assessing normalcy of symptoms
Based on past experiences and the five criteria described previously, teens indicated they were able to identify which symptoms were unusual and would likely lead to serious repercussions if untreated, and which could safely be ignored. As one boy expressed,
Wheezing’s very common. It doesn’t restrict anything I do, and based on past experiences, I know that there’s a decent chance that it won’t actually turn into anything or it’ll solve itself out. (T09)
In general, teens indicated they needed a rescue inhaler if symptoms were unusual, interfered with activity, didn’t resolve spontaneously, or became worse. One girl explained it this way,
I take a deep breath and reassess … how am I feeling right now? I’m like ok…those [symptoms] are normal. Are they worse? Are they less? Can I take a deep breath? Is it too tight? Does it feel okay? …There’s kind of like a mental scale going on in my brain…(T04)
Weighing benefits vs. burdens
Based on prior experiences and current context (i.e. school vs. home), teens weighed the benefits and burdens of using/not using rescue medication. Disadvantages of medicating included disrupting activities (leaving class, losing a game, interrupting a movie), being left behind by peers, and missing out on fun activities. As one girl said:
I wanna get in as much [fun] as I possibly can. And you have to stop and take [your inhaler] … It’s really not that big of a deal, but for a teenager it is, and then you have to walk away from your friends, be like I gotta go do my inhaler … and they go off and do something else. (T04)
Other disadvantages included medication side-effects (e.g. shaking), feelings that inhalers didn’t work (i.e. immediately), and fears of overusing medications. Often, teens felt their asthma was more controlled when they were able to withstand symptoms and minimize medication use, and less controlled if they had to use a rescue inhaler. Many (86%) expressed concerns about becoming dependent/addicted. Withholding medication when symptomatic was seen as helping to avoid dependence:
I think it’s bad for me… I don’t wanna get addicted to it …I don’t wanna always have to depend on it. (T15)
Teens consistently used their prior experiences to estimate whether symptoms were likely to get worse or resolve spontaneously. Symptoms considered likely to resolve spontaneously were ignored, whereas worsening symptoms were generally treated. Many described waiting it out. As one said,
I’ll wait a little bit [see] if it’ll go away, if not I’ll go up and take [my inhaler]… if it’s slowly getting worse then I can wait probably like 30 minutes but if it’s getting bad really fast I have to go immediately. (T13)
Evaluating access to treatment
In determining when to treat, teens considered accessibility of medication. Difficulty accessing treatment increased the overall burden of medicating. The more inconvenient it was to get/use medication, the more likely teens were to delay treatment and tolerate symptoms. Reported barriers included having to leave class, presence of strangers, insufficient support (teacher, nurse, coach, friends), lack of privacy, and greater physical distance to inhaler. One girl remarked, “Like, it depends where I’m at. If I’m outside I probably won’t run in the house and try to find it” (T01).
Going to the school-nurse was another commonly reported barrier. One girl commented, “It’s like the walk of shame to go to the nurse’s office…and you wait forever just to get your inhaler, and they ask you a million questions…it’s more hassle than it’s worth, I guess.” (T04)
Conversely, access was improved by having an inhaler nearby, ability to use it without disrupting activities, sufficient privacy, and having support from friends, teachers, and coaches. While most of the teens were comfortable using inhalers in front of peers (n=11), the younger girls were not (n=3).
Treatment Thresholds
Sorting by a priori criterion (asthma control), we found that teens with uncontrolled asthma had substantially higher treatment thresholds (greater delay in treatment) for responding to symptoms than teens with controlled asthma. Furthermore, uncontrolled teens used more non-pharmacologic measures (e.g. cool cloth, holding breath, hitting chest) to manage symptoms than those with better control, and delayed using medication longer. Comparison of S/R card-sort data for teens with well-controlled, not-well-controlled, and very-poorly-controlled asthma show marked differences in treatment thresholds between groups (Fig. 2). Teens with better controlled asthma accepted far lower levels of symptoms before treating, compared to teens with not well-controlled and very poorly-controlled asthma. This finding was substantiated in corresponding narratives (Table 3), which also revealed that controlled teens and their parents perceived symptoms as being serious and requiring early treatment, whereas uncontrolled teens and their parents were more accepting of symptoms, less willing to use medication, and more likely to prioritize alternative symptom management strategies.
FIGURE 2.
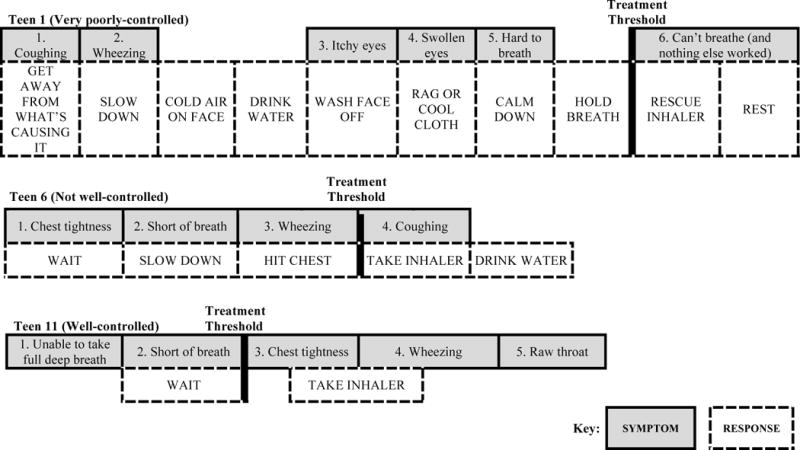
Comparison of Treatment Thresholds between teens with very poorly-controlled, not well-controlled and well-controlled asthma using Symptom-Response card sorting
TABLE 3.
Differences in symptom perception and response between teens with controlled vs. uncontrolled asthma
| Controlled Asthma | Uncontrolled asthma | |
|---|---|---|
| Teen | T08: Every symptom is serious—you need to do something about it. … you never want to wait—you gotta take your albuterol. | T15: So when I get the chest pain, I breathe in some cold air, … and I’ll use a cold washcloth. I’ll drink some water when my chest tightens… [and] wait. Then if I start to cough, I’ll slow down my breathing. …Then if I start wheezing I’ll take a shower and sit in the steam, and relax. Then I’ll take my inhaler. … I usually try and wait it out. … Cause if I take it right away, then I’ll always rely on it. But if I wait it out … then I feel like my lungs get like tougher or something. |
| T02: Asthma is like, serious… I make sure that I notice my asthma symptoms early before it gets really bad, and when I do have asthma symptoms I make sure I take my Albuterol asthma pump. | T05: You have to suck this up and try and get through. I have tried to grow some sort of tolerance to [symptoms]…. I think that if you’re able to work out everything without taking any medication that is a positive thing…using that pump you become dependent on it…. I just think that if, I think that if I’m less dependent on it, I’ll be able to cope more—it’s like wow, these symptoms are way less, I notice this a lot less, and I need to take it less. Progressively doing that you get used to [symptoms]…. | |
| Parent | P08: I believe that all the symptoms are serious, because wheezing is showing you like, okay something’s starting to act up let’s get control of that now. | P15: I really think that a lot of it is mind control…sometimes you’re just out of breath and it’s ok. I say to him, if you can take a deep breath in through your nose and slowly let it out through your mouth and you feel like you’re getting what you need for oxygen, you’re ok. If a person’s having a hard time breathing, they’re leaning forward, and gasping out of their mouth. [Don’t] automatically go for your inhaler…albuterol is very habit forming. |
| P02: She’s really on top of it… she always has it with her in case … You have to take care of yourself…. you have to make sure you see the signs before it gets worse. | P05: He was saying he felt like he might pass out, and I could see him struggling…the muscles in the neck and the chest straining on breathing And he was grabbing his chest like this and rocking, at the same time even though he was that severe—I told him, I can take you [to the hospital] but I don’t know what they’re going to do for you…. I don’t know why your chest is hurting ….I’m thinking it’s going to be a wasted effort to go….sometimes, if you feel something and you focus on it, it seems like it’s bigger than what it is. |
Uncontrolled teens further revealed that their ability to tolerate symptoms had increased substantially over time, such that it required a higher level of symptoms to cause concern, discomfort, or interfere with activity. As one boy said,
T09: I was more concerned when I was younger… I didn’t have as much experience as I do now.…My ability of tolerating low-level symptoms like wheezing, chest tightness, that’s increased. …I can think back like twenty times I’ve had these exact symptoms and pretty much the same scenario. …That’ll result in me like not using the inhaler as many times as I might when I was younger.
Many also expressed intentionally tying to tolerate symptoms. This was referred to as “training your lungs” and “toughing it out,” similar to the fitness concept of “no pain no gain.” Teens explained it this way:
T10: If the [symptoms] are not like serious, you should be able to tough it out… [Don’t take] medications just for a small symptom—build the strength up in your lungs… It’s just shortness of breath, you’re fine, just slow down.
T05: [My goal is] getting to a point where my tolerance is so high that it doesn’t feel like I’m living with asthma anymore. That would be a huge thing because if I’m able to tolerate asthma as if it’s not asthma and be like a regular person–that puts me a cut above a regular person. …Having symptoms and not being bothered…that would be great.
Communicating: Teens don’t report normal symptoms—“It’s not that important”
Normalizing also affected how teens reported symptoms. Teens indicated they only told parents about unusual symptoms, specifically those exceeding their treatment threshold or interfering with activities. As one girl explained, “I don’t really think it’s that bad” (T14). In general, teens reported when they felt their asthma was less controlled than usual, or when they had to use their inhaler more often, again referencing baseline patterns. Thus, teens with regular symptoms often reported as being asymptomatic because symptoms did not exceed normal:
T02: I’m not gonna remember normal things because I do it every day… It has to be like something major. And nothing major happens every day. And if it does happen every day, I’m not gonna remember it because it’s normal for me.
T04: Everyone has a different normal—normal might be having chest tightness like 3 times a day—so when the doctor says are there any asthma symptoms, they’ll be like no, when there really are.
Teens indicated their parents were often unaware of their normal symptoms. In response, many parents monitored for overtly visible or audible symptoms as a means of assessing asthma control. One parent remarked, “I think his asthma is pretty good—I don’t know for sure…He’s had the symptoms for so long that he might be like, ‘I’m Okay,’ … [because] it’s normal. That’s why I try to watch him….” (P12). Because teens didn’t report normal symptoms, only unusual (teen reported) or audible/visible symptoms (parent reported) were communicated to providers. Providers were thus unaware of teens’ normal symptoms and actual symptom frequency.
Discussion
Findings from this study support prior research showing that teens tend to ignore, undertreat, and underreport asthma symptoms [4, 21–23]. While it is established that teens minimize symptoms, avoid medication and often don’t report worsening symptoms, thought processes and perceptions driving these behaviors have not been fully explored. Our data suggest that individual thresholds for recognizing, responding to, and reporting symptoms are based on perceived symptom severity and teens’ concepts of normalcy relative to personal baseline, a finding that has not previously been reported in asthma literature.
Normalization is often a functionally adaptive response, and has been reported with other chronic diseases (e.g. diabetes, end-stage renal, chronic pain, mental illness) [24–27]. Over time, individuals with chronic illness develop a new sense of normal, which helps to minimize personal disruptions caused by illness and the sense of oneself as being less healthy than others [28, 29]. Teens with asthma often report anxiety, depression, and social isolation [23, 30, 31]. For these teens, normalizing symptoms and avoiding medication may decrease feelings of being different and minimize psychosocial burdens of disease. Normalization could explain why symptomatic teens often self-report as asymptomatic, and delay or decline to treat [3, 32]. Similarly, it could explain why older teens and those living with asthma longer tolerate higher levels of symptoms and have worse control than those who are younger and less experienced [5, 33, 34].
Further, we found that in addition to normalizing, teens frequently did not treat their symptoms—often because benefits of treatment did not outweigh perceived burdens, which is consistent with prior reports [6, 35, 36]. For most teens, taking rescue medication was equated with being out of control. Ontologically, this makes sense, given the terminology of “rescue medication.” Needing “rescue” implies being out of control. Interestingly, the terminology and tradition of correlating rescue medication use with control derives from clinical standards, where frequency of inhaler use is an accepted proxy measure for control. Simply stated, needing more rescue medication is equivalent to having less asthma control. It then logically follows that using less rescue medication equates with better asthma control. Thus, by building tolerance, normalizing symptoms, and minimizing need for rescue medication, teens can increase sense of being in control of their asthma.
Albeit psychologically functional, normalizing and abstaining from medication use have undesirable ramifications for asthma management. Clinical assessment of asthma severity and control relies heavily upon subjective report of symptoms and inhaler use [16, 21]. If teens don’t report normal symptoms and avoid medication use, self-report is unlikely to accurately reflect symptom frequency, leading to misclassification of control, under-use of control medications, and suboptimal outcomes.
Important differences were identified in symptom perceptions and treatment thresholds between teens with controlled versus uncontrolled asthma. Consistent with prior evidence, teens with better control regarded symptoms as more serious, responded sooner, and used fewer non-pharmacologic symptom-management strategies [37–40]. Conversely, higher thresholds for treatment corresponded with greater symptom tolerance, delayed treatment patterns, and poorer control. This suggests that how teens conceptualize and respond to asthma symptoms may be a primary determinant of self-management and control [3, 4, 22, 41]. It is also noteworthy that in discussing usual symptom management strategies, teens infrequently referenced control medications, typically prioritizing other ways of handling symptoms. Paucity of references to control medications may reflect lack of perceived importance to teens, and may help to explain poor adherence. Further research is needed to determine if patterns of perceptions and responses are modifiable, and if modification in treatment thresholds is associated with improved asthma outcomes. Interventions targeting illness and self-management perceptions, perceived norms, and medication beliefs using established theoretical approaches to behavior modification (e.g. Common-Sense Models of Illness, Social Cognitive theory, Theory of Reasoned Action) may be warranted [10, 38].
No clear differences were identified between African American and Hispanic/Latino teens and Caucasian teens’ perceptions and experiences with asthma and its management. Irrespective of race, those with controlled asthma conceptualized and responded to symptoms similarly, as did those with uncontrolled asthma. Prior studies, however, have demonstrated significant differences in perceptual accuracy of symptoms between these groups, with a strong association between inaccurate symptom perception and diminished asthma control. [22, 42]. It is possible that, by purposely sampling for equal representation of controlled/uncontrolled asthma in each group we may have limited ability to identify trends in ethnic/minority self-management and symptom perception. Further research is warranted to explore associations between race/ethnicity, symptom perceptions, self-management behaviors, and asthma control.
Clinical Implications
Recognizing teens’ tendency to normalize, undertreat, and underreport symptoms, clinicians and researchers should consider screening for normal symptoms. Uncovering usual patterns of symptoms and responses can facilitate discussions about teens’ current management strategies, identify barriers to adequate self-management, and enable shared goal-setting and decision-making [14]. Incorporating objective measures (e.g. spirometry, symptom monitoring devices) may also be needed to increase the accuracy of symptom assessments [43].
Helping teens manage more effectively will likely entail minimizing cumulative burdens while maximizing personal benefits of treatment [28]. Prescribing backup inhalers to keep in multiple locations (e.g. bedside, kitchen/living area, schoolbag) may be helpful in improving access. Explicit discussion of how rescue inhalers work may help uncover and minimize fears of dependency, side-effects, and feelings that inhalers do not work.
Regular reinforcement of asthma pathophysiology, along with short and long-term goals of treatment is also needed. Many teens in this study expressed feelings that symptoms did not matter as long as they were tolerable, and were unaware of the long-term consequences of undertreating. Emphasizing that symptoms are a sign of inflammation, and that uncontrolled inflammation leads to remodeling (i.e. scarring the lungs) may help teens make more informed treatment choices, and underscore the importance of using preventive medications. Similarly, it may be necessary to address misconceptions that abstaining from medication makes lungs “tougher.” Ultimately, highlighting personal benefits of treatment for each teen will be critically important to shifting the scales towards more effective self-management. Demonstrating how improved asthma control can positively impact important activities (e.g. improved sports performance, decreased sick time, reduce likelihood of missing out on fun activities) will likely be beneficial.
Limitations
Although we sampled for equal representation of controlled/uncontrolled asthma, the study contained fewer truly “well-controlled” teens than intended. Interviews and diaries often revealed higher frequency and severity of symptoms than self-reported using the standard screening measures. To address this, in analyzing our data, we approached asthma control as a spectrum, comparing responses between teens with better versus poorer control, rather than as a dichotomous categorical variable. Second, while the study sample comprised 50% minority individuals, only two participants were of Hispanic/Latino ethnicity; this may have limited ability to identify racial and ethnic differences in self-management. Lastly, non-English-speaking teens and those with confounding comorbidities were excluded from the sample; further research into similarities and differences between these groups may be warranted.
Despite limitations, our findings are likely to be useful to those working with teens, as they shed light on underlying perceptual and behavioral patterns directly linked to self-management. Understanding how teens perceive and experience asthma can highlight areas of intervention need, contribute to development of programs tailored to these needs, and contribute to improved health outcomes.
Supplementary Material
References
- 1.Centers for Disease Control [CDC] Asthma prevalence, disease characteristics, and self-management education-United States, 2001–2009. DHHS publication; 2011. [Google Scholar]
- 2.Rand CS, Wright RJ, Cabana MD, Foggs MB, Halterman JS, Olson L, et al. Mediators of asthma outcomes. J Allergy Clincal Immunol. 2012;129(3 Suppl):S136–41. doi: 10.1016/j.jaci.2011.12.987. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rhee H, Belyea MJ, Ciurzynski S, Brasch J. Barriers to asthma self-management in adolescents: relationships to psychosocial factors. Pediatr Pulmonol. 2009;44(2):183–91. doi: 10.1002/ppul.20972. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Britto MT, Byczkowski TL, Hesse EA, Munafo JK, Vockell ALB, Yi MS. Overestimation of impairment-related asthma control by adolescents. J Pediatr. 2011;158(6):1028–30. doi: 10.1016/j.jpeds.2011.01.034. [DOI] [PubMed] [Google Scholar]
- 5.Bruzzese JM, Stepney C, Fiorino EK, Bornstein L, Wang J, Petkova E, et al. Asthma self-management is sub-optimal in urban Hispanic and African American/Black early adolescents with uncontrolled persistent asthma. J Asthma. 2012;49(1):90–7. doi: 10.3109/02770903.2011.637595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.George M, Campbell J, Rand C. Self-management of acute asthma among low-income urban adults. J Asthma. 2009;46(6):618–24. doi: 10.1080/02770900903029788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Koster ES, Philbert D, de Vries TW, van Dijk L, Bouvy ML. “I just forget to take it”: asthma self-management needs and preferences in adolescents. J Asthma. 2015;52(8):831–7. doi: 10.3109/02770903.2015.1020388. [DOI] [PubMed] [Google Scholar]
- 8.Mammen J, Rhee H. Adolescent asthma self-management: a concept analysis and operational definition. Pediatr Allergy Immunol Pulmonol. 2012;25(4):180–9. doi: 10.1089/ped.2012.0150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rich M, Lamola S, Amory C, Schneider L. Asthma in life context: Video Intervention/Prevention Assessment (VIA) Pediatr. 2000;105(3 Pt 1):469–77. doi: 10.1542/peds.105.3.469. [DOI] [PubMed] [Google Scholar]
- 10.Koster ES, Philbert D, Winters NA, Bouvy ML. Adolescents’ inhaled corticosteroid adherence: the importance of treatment perceptions and medication knowledge. J Asthma. 2015;52(4):431–6. doi: 10.3109/02770903.2014.979366. [DOI] [PubMed] [Google Scholar]
- 11.Koster ES, Raaijmakers JA, Vijverberg SJ, Maitland-van der Zee AH. Inhaled corticosteroid adherence in paediatric patients: the PACMAN cohort study. Pharmacoepidemiol Drug Saf. 2011;20(10):1064–72. doi: 10.1002/pds.2228. [DOI] [PubMed] [Google Scholar]
- 12.Department of Health and Human Services, editor. [DHHS] DoHaHS. Code of Federal Regulations: Protection of Human Subjects. 2009. pp. 1–14. [Google Scholar]
- 13.Maxwell JA. Qualitative Research Design: an Interactive Approach. Thousand Oaks, CA: Sage; 2012. [Google Scholar]
- 14.Mammen J, Norton S, Rhee H, Butz A. New approaches to qualitative interviewing: Development of a card sort technique to understand subjective patterns of symptoms and responses. Int J Nurs Stud. 2016 doi: 10.1016/j.ijnurstu.2015.12.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Patton MQ. Qualitative Research & Evaluation Methods. 3rd. Thousand Oaks, CA: Sage; 2002. [Google Scholar]
- 16.National Heart Lung and Blood Institues [NHLBI] Expert Panel Report 3: Guidelines for the diagnosis and management of asthma. Bethesda, Md: National Asthma Education and Prevention Program; 2007. [Google Scholar]
- 17.Marshall C, Rossman G. Designing Qualitative Research. 5. London: SAGE; 2011. [Google Scholar]
- 18.Saldaña J. The Coding Manual for Qualitative Researchers. 2nd. Washington, DC: Sage; 2013. [Google Scholar]
- 19.Ayres L, Kavanaugh K, Knafl KA. Within-case and across-case approaches to qualitative data analysis. Qual Health Res. 2003;13(6):871–83. doi: 10.1177/1049732303013006008. [DOI] [PubMed] [Google Scholar]
- 20.US Department of Housing and Urban Development [US DoHUD] Uniform Relocation Assistance and Real Property Acquisition Policies Act of 1970 (Uniform Act or URA) - FY 2011 Low Income Limits. 2011 Available from: http://www.huduser.org/portal/datasets/ura/ura11/RelocAct.html.
- 21.Protudjer JL, Kozyrskyj AL, Becker AB, Marchessault G. Normalization strategies of children with asthma. Qual Health Res. 2009;19(1):94–104. doi: 10.1177/1049732308327348. [DOI] [PubMed] [Google Scholar]
- 22.Rhee H, Belyea MJ, Elward KS. Patterns of asthma control perception in adolescents: associations with psychosocial functioning. J Asthma. 2008;45(7):600–6. doi: 10.1080/02770900802126974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rhee H, Fairbanks E, Butz A. Symptoms, feelings, activities and medication use in adolescents with uncontrolled asthma: lessons learned from asthma diaries. J Pediatr Nurs. 2013;29(1):39–46. doi: 10.1016/j.pedn.2013.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Babler E, Strickland CJ. Normalizing: Adolescent experiences living with type 1 diabetes. Diabetes Educ. 2015:351–60. doi: 10.1177/0145721715579108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Nicholas DB, Picone G, Selkirk EK. The lived experiences of children and adolescents with end-stage renal disease. Qual Health Res. 2011;21(2):162–73. doi: 10.1177/1049732310382789. [DOI] [PubMed] [Google Scholar]
- 26.Nilsen G, Anderssen N. Struggling for a normal life: Work as an individual self-care management strategy among persons living with non-malignant chronic pain. J Preven Assess Rehab. 2014;49(1):123–32. doi: 10.3233/WOR-131642. [DOI] [PubMed] [Google Scholar]
- 27.Ilic M, Reinecke J, Bohner G, Rottgers HO, Beblo T, Driessen M, et al. Protecting self-esteem from stigma: A test of different strategies for coping with the stigma of mental illness. Int J Soc Psychiatry. 2012;58(3):246–57. doi: 10.1177/0020764010392058. [DOI] [PubMed] [Google Scholar]
- 28.Rosen A, Ivarsson A, Nordyke K, Karlsson E, Carlsson A, Danielsson L, et al. Balancing health benefits and social sacrifices: a qualitative study of how screening-detected celiac disease impacts adolescents’ quality of life. BMC Pediatr. 2011;11:32. doi: 10.1186/1471-2431-11-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Nordyke K, Rosen A, Emmelin M, Ivarsson A. Internalizing the threat of risk–a qualitative study about adolescents’ experience living with screening-detected celiac disease 5 years after diagnosis. Health Qual Life Outcomes. 2014;12:91. doi: 10.1186/1477-7525-12-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Stewart M, Masuda JR, Letourneau N, Anderson S, McGhan S. “I want to meet other kids like me”: support needs of children with asthma and allergies. Issues Compr Pediatr Nurs. 2011;34(2):62–78. doi: 10.3109/01460862.2011.572638. [DOI] [PubMed] [Google Scholar]
- 31.Kaptein AA, Klok T, Moss-Morris R, Brand PLP. Illness perceptions: impact on self-management and control in asthma. Curr Opin Allergy Clin Immun. 2010;10(3):194–9. doi: 10.1097/ACI.0b013e32833950c1. [DOI] [PubMed] [Google Scholar]
- 32.Rhee H, Wenzel JA, Steeves RH. Adolescents’ psychosocial experiences living with asthma: A focus group study. J Pediatr Health Care. 2007;21(2):99–107. doi: 10.1016/j.pedhc.2006.04.005. [DOI] [PubMed] [Google Scholar]
- 33.Mosnaim G, Li H, Martin M, Richardson D, Belice PJ, Avery E, et al. Factors associated with levels of adherence to inhaled corticosteroids in minority adolescents with asthma. Ann Allergy Asthma Immunol. 2014;112(2):116–20. doi: 10.1016/j.anai.2013.11.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.McQuaid EL, Kopel SJ, Klein RB, Fritz GK. Medication adherence in pediatric asthma: Reasoning, responsibility, and behavior. J Pediatr Psychol. 2003;28(5):323–33. doi: 10.1093/jpepsy/jsg022. [DOI] [PubMed] [Google Scholar]
- 35.Buston KM, Wood SF. Non-compliance amongst adolescents with asthma: listening to what they tell us about self-management. Fam Prac. 2000;17(2):134–8. doi: 10.1093/fampra/17.2.134. [DOI] [PubMed] [Google Scholar]
- 36.Cohen R, Franco K, Motlow F, Reznik M, Ozuah PO. Perceptions and attitudes of adolescents with asthma. J Asthma. 2003;40(2):207–11. doi: 10.1081/jas-120017992. [DOI] [PubMed] [Google Scholar]
- 37.Cotton S, Luberto CM, Yi MS, Tsevat J. Complementary and alternative medicine behaviors and beliefs in urban adolescents with asthma. Complementary and alternative medicine behaviors and beliefs in urban adolescents with asthma. 2011;48(5):531–8. doi: 10.3109/02770903.2011.570406. [DOI] [PubMed] [Google Scholar]
- 38.George M, Topaz M, Rand C, Sommers ML, Glanz K, Pantalon MV, et al. Inhaled corticosteroid beliefs, complementary and alternative medicine, and uncontrolled asthma in urban minority adults. Inhaled corticosteroid beliefs, complementary and alternative medicine, and uncontrolled asthma in urban minority adults. 2014;134(6):1252–9. doi: 10.1016/j.jaci.2014.07.044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Berg J, Morphew T, Tran J, Kilgore D, Galant SP. Prevalence of complementary and alternative medicine usage in Vietnamese American asthmatic children. Prevalence of complementary and alternative medicine usage in Vietnamese American asthmatic children. 2015 [Google Scholar]
- 40.Lin SI, Tsai TH, Chou YJ, Huang N. Characteristics associated with utilization of asthma-related traditional Chinese medicine services among asthma children in Taiwan: A nationwide cohort study. Characteristics associated with utilization of asthma-related traditional Chinese medicine services among asthma children in Taiwan: A nationwide cohort study. 2015;2015:108961. doi: 10.1155/2015/108961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Rhee H, Belyea MJ, Halterman JS. Adolescents’ perception of asthma symptoms and health care utilization. 2011;25(2):105–13. doi: 10.1016/j.pedhc.2009.10.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Fritz GK, McQuaid EL, Kopel SJ, Seifer R, Klein RB, Mitchell DK, et al. Ethnic differences in perception of lung function: a factor in pediatric asthma disparities? 2010;182(1):12–8. doi: 10.1164/rccm.200906-0836OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Rhee H, Allen J, Mammen J, Swift M. Mobile phone-based asthma self-management aid for adolescents (mASMAA): a feasibility study. Patient Prefer Adher. 2014;8:63–72. doi: 10.2147/PPA.S53504. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


