Abstract
Objective
Mortality trends of rheumatoid arthritis (RA) are largely unknown over the past decade when new drugs and management strategies have been adopted to effectively treat RA.
Methods
Using The Health Improvement Network, an electronic medical record database representative of the UK general population, we identified patients with incident RA and up to five individuals without RA matched for age, sex and year of diagnosis between 1999 and 2014. The RA cohort was divided in two sub-cohorts based on the year of RA diagnosis: the early cohort (1999–2006) and the late cohort (2007–2014). We compared mortality rates, HRs (using a Cox proportional hazard model) and rate differences (using an additive hazard model) between RA and non-RA cohorts adjusting for potential confounders.
Results
Patients with RA diagnosed between 1999 and 2006 had a considerably higher mortality rate than their comparison cohort (ie, 29.1 vs 18.0 deaths/1000 person-years), as compared with a moderate difference in patients with RA diagnosed between 2007 and 2014 and their comparison cohort (17.0 vs 12.9 deaths/1000 years). The corresponding absolute mortality rate differences were 9.5 deaths/1000 person-years (95% CIs 7.5 to 11.6) and 3.1 deaths/1000 person-years (95% CI 1.5 to 4.6) and the mortality HRs were 1.56 (95% CI 1.44 to 1.69) and 1.29 (95% CI 1.17 to 1.42), respectively (both p values for interaction <0.01).
Conclusion
This general population-based cohort study indicates that the survival of patients with RA has improved over the past decade to a greater degree than in the general population. Improved management of RA and its associated comorbidities over recent years may be providing a survival benefit.
INTRODUCTION
Rheumatoid arthritis (RA) is a chronic systemic inflammatory disease associated with premature mortality.1 Over the past 15 years, new drugs (eg, biologics) and management strategies (eg, ‘treat-to-target’ and early RA intervention) have been actively adopted to effectively treat RA.2–5 Furthermore, increasing recognition of the cardiovascular sequelae of RA has led to the recommendation and implementation of corresponding prevention strategies.6 However, whether these perceived improvements in RA care in recent years have translated to improved survival among these patients remains unknown.
A few studies have examined the mortality trends in patients with RA diagnosed up to 2004 (ie, the early period of biological use) and found no improvement when compared with early RA cohorts.7,8 However, no data are available on the mortality trends among patients with RA diagnosed in the late 2000’s and beyond. Indeed, trends among the more recent RA cohorts would be directly relevant, as the long-term benefits (eg, improvement in mortality) arising from the perceived improvement in RA care that began in the late 1990’s and early 2000’s can finally be realised at the population level.2–4,9
To address this key knowledge gap in the field, we conducted a population-based cohort study to examine the secular trend of all-cause mortality among patients with RA between 1999 and 2014. As all-cause mortality in the UK has declined substantially over the past decades, these background mortality trends need to be incorporated when assessing excess mortality trends in patients with RA. Thus, we assessed whether the rate of improvement in all-cause mortality among patients with RA and among individuals without RA from the general population differed in the two calendar-time sub-cohorts, based on the year of RA diagnosis (ie, 1999–2006 (early cohort) and 2007–2014 (late cohort)).
METHODS
Data source
The Health Improvement Network (THIN) is an electronic medical record (EMR) database from general practitioners (GPs) in the UK. It contains health information on approximately 10.2 million patients from 580 general practices in the UK. Specifically, health information is recorded on site at each practice using a computerised system with quality control procedures to maintain high data completion rates and accuracy. The information includes socio-demographics, anthropometrics, lifestyle factors, details from GP visits, diagnoses from specialists’ referrals and hospital admissions and results of laboratory tests. The READ classification system is used to code specific diagnoses10 and a drug dictionary based on data from the Multilex classification system is used to code drugs.11 Approximately 95% of the UK population is registered with a general practice and prior research has shown that THIN is representative of the UK population in terms of patient demographics and the prevalence of common illnesses.12
Study design and cohort definition
We conducted a matched cohort study to examine the secular trends of all-cause mortality among patients with incident RA, compared with individuals without RA. We identified all individuals aged between 18 and 89 years who had a first-ever diagnosis of RA defined by at least one READ code for RA between 1 January 1999 and 31 December 2014. READ codes for RA have been previously validated in the UK General Practice Research Database, with a positive predictive value (PPV) of around 80%.13,14 In our alternative definition of RA, we identified individuals who had a first-ever diagnosis of RA using READ codes followed by at least one prescription for a disease-modifying anti-rheumatic drug (DMARD) within 1 year of diagnosis.15 This definition was found to have a specificity of 96% against the 1987 American College of Rheumatology Criteria for RA. For the alternative definition, the date of the first DMARD prescription was deemed as the index date. In addition, RA cohort members were required to have ≥1 year of continuous enrolment and at least one GP visit within the year prior to cohort entry. We then grouped the RA cohort into two calendar time-based cohorts, using the year of diagnosis, that is, early cohort (1999–2006) and late cohort (2007–2014), to evaluate changes in mortality.
For the comparison cohorts corresponding to each RA cohort, we matched up to five individuals without RA based on age, sex and calendar year of entry (ie, the index date). If there were more than five non-RA matches available per subject with RA, we assigned each a random number and randomly selected five among these, whereas we selected all available non-RA matches in cases where there were fewer than five matches. The non-RA subjects were also required to have ≥1 year of continuous enrolment and to have at least one GP visit within the year prior to cohort entry.
Assessment of outcome
The outcome of this study was all-cause mortality, defined by the death date recorded in THIN. Registering of death triggers an update in the Personal Demographics Service. This is the national database that holds patient demographic data for the National Health Service. The change in patient status to ‘dead’ is immediately updated in the patient’s EMR. This is an automated process which requires no input by the practice staff in THIN. Previous studies have shown that the mortality data from THIN agree well with national death rates in the UK.12
Assessment of covariates
From the THIN database we obtained covariate information prior to the index date on socio-demographic and anthropometric characteristics (ie, age, sex, date of birth, body mass index (BMI)), lifestyle factors (ie, alcohol consumption and cigarette smoking), medication use (ie, diuretic, angiotensin II receptor antagonists, angiotensin-converting-enzyme inhibitor, calcium channel blockers, β-blocker and low-dose aspirin) and comorbidities (ie, myocardial infarction, congestive heart failure, cerebrovascular disease, peripheral vascular disease, dementia, chronic obstructive pulmonary disease, ulcer, liver disease, diabetes without complications, diabetes with complications, renal disease, rheumatologic disease, cancer and AIDS). The presence of comorbidities was defined using READ codes as recorded by GPs. Based on this comorbidity list, we calculated the adapted Charlson comorbidity score.16 All medication was assessed within 1 year prior to the index date; socio-demographic and anthropometric characteristics were assessed using the most recent available data prior to the index date and comorbidities were assessed any time prior to the index date. We assessed health service usage by calculating the number of GP visits in the year prior to the index date.
Statistical analysis
We compared the baseline characteristics of individuals in the RA cohorts and corresponding non-RA cohorts. Person-years of follow-up for each subject were computed as the amount of time from the index date to the first of the following events: death, disenrollment from the THIN database or the end of follow-up (either 31 December 2006 for the early cohort or 31 December 2014 for the late cohort, ensuring that the follow-up time was equal between the two cohorts to allow for a fair comparison). We calculated the all-cause mortality rate for each sub-cohort and plotted Kaplan-Meier mortality curves for them.
We used a Cox proportional hazard model to examine the relation of RA to all-cause mortality for each time-specific RA cohort, adjusting for the number of GP visits, BMI, smoking status (ie, non-smokers, ex-smokers and current-smokers), alcohol consumption (ie, non-drinkers, ex-drinkers and current-drinkers), comorbidities and medication use. We also examined the difference in all-cause mortality between the RA cohorts and comparison cohorts using an additive hazard model in which the hazard was modelled as a linear function of RA status.17 The effect estimate generated from the model can be interpreted as the number of excess deaths attributable to RA per 1000 person-years. To evaluate whether the relationship between RA and all-cause mortality varied according to time, we combined the two RA cohorts and tested an interaction term (ie, RA status X sub-cohort) in the multivariable regression model. Given the predilection of RA among women, we also analysed the mortality trends according to sex.
For all analyses, missing values for covariates (ie, BMI, alcohol consumption and smoking status) were imputed by a sequential regression method based on a set of covariates as predictors (IVEware for SAS (V.9.2); SAS Institute, Cary, North Carolina, USA).18
To assess the robustness of the study findings, we performed a series of sensitivity analyses. First, we evaluated the potential impact of an imperfect diagnosis of RA on our study findings by varying the PPV of RA diagnosis from 80% (ie, our primary definition’s accuracy) and higher (which would correspond to our alternative definition’s accuracy).19 In contrast, negative predictive value of our RA definition (probability of not having RA, when there is no RA diagnosis in the GP medical record) is expected to be extremely high because the incidence rate of RA is very low (<0.1%/year). We also performed the analysis using smoking status, alcohol consumption and BMI variables collected within 2 years prior to index date. Finally, we repeated our analyses excluding patients who were on a DMARD before the first diagnosis of RA and extending the period to 3 years of observation without a diagnosis of RA.
RESULTS
The early cohort consisted of 10 126 patients with incident RA and 50 546 matched individuals without RA. During the follow-up period, 936 and 2968 individuals died in the RA and non-RA cohorts, respectively. The median age at death was 77.0 and 78.4 years, respectively. In the late cohort of 10 769 patients with incident RA and 53 749 matched individuals without RA, 605 and 2293 died during the follow-up period, with a median age at death of 77.9 and 78.4 years, respectively. The mean follow-up time in the two comparison cohorts was similar, with 3.2 years of follow-up in the early cohorts and 3.3 years in the late cohorts.
As shown in table 1, there was no apparent difference in age, sex, BMI, alcohol consumption and medication use between RA and non-RA subjects in the early cohorts at baseline; however, patients with RA were more likely to be smokers and had more comorbidities than their non-RA comparators. Similar findings were also observed among subjects in the late cohorts. DMARD use was 65% in the early cohort and 81% in the late cohort. Of these DMARD-treated RA cases, 68% and 85% received methotrexate, respectively.
Table 1.
Baseline characteristics of participants according to calendar time-based sub-cohorts and RA status
| Characteristics | 1999–2006 | 2007–2014 | ||
|---|---|---|---|---|
| RA cohort (n=10 126) | Non-RA cohort (n=50 546) | RA cohort (n=10 769) | Non-RA cohort (n=53 749) | |
| Sex (% of men) | 29.7 | 29.7 | 31.4 | 31.4 |
| Age (years) | 60+15 | 60+15 | 59±15 | 59±15 |
| BMI (kg/m2) | 26.7+5.3 | 26.4+5.1 | 27.6±5.8 | 27.2±5.5 |
| Smoking status (%) | ||||
| Non-smoker | 43.8 | 50.0 | 47.4 | 56.1 |
| Ex-smoker | 20.4 | 16.6 | 30.2 | 24.2 |
| Current smoker | 24.6 | 18.7 | 22.0 | 17.6 |
| Missing | 11.3 | 14.7 | 0.4 | 2.1 |
| Alcohol drinking (%) | ||||
| Non-drinker | 18.9 | 15.9 | 19.9 | 16.6 |
| Ex-drinker | 1.5 | 1.0 | 3.1 | 2.2 |
| Current drinker | 59.7 | 60.5 | 66.6 | 68.4 |
| Missing | 19.4 | 22.7 | 10.4 | 12.8 |
| Medication use (%) | ||||
| Diuretics | 21.5 | 18.3 | 17.5 | 14.9 |
| Angiotensin II receptor antagonists | 3.5 | 3.2 | 7.4 | 6.3 |
| Angiotensin-converting enzyme inhibitor | 12.7 | 13.3 | 12.2 | 11.8 |
| Calcium channel blockers | 11.6 | 10.4 | 13.7 | 12.9 |
| β-blocker | 13.6 | 12.9 | 14.0 | 13.0 |
| Low-dose aspirin | 10.8 | 10.1 | 15.8 | 14.6 |
| Charlson Comorbidity Index | 1.3±0.8 | 0.2±0.8 | 1.4±0.9 | 0.4±0.9 |
BMI, body mass index; RA, rheumatoid arthritis.
Figure 1 depicts the cumulative all-cause mortality during the follow-up among RA and non-RA cohorts according to calendar year. While patients with RA had higher mortality rates than individuals without RA in either the early or the late cohorts, the magnitude of difference in mortality was smaller in the late cohorts compared with that in the early cohorts. The age-matched, sex-matched and entry time-matched HR for all-cause mortality from RA was 1.66 (95% CI 1.54 to 1.79) in the early cohorts as compared with 1.35 (95% CI 1.23 to 1.48) in the late cohorts (table 2), indicating that the decline in the all-cause mortality rate over time was greater among patients with RA than among individuals without RA. The multivariable-adjusted HR of all-cause mortality from RA remained larger in the early cohorts (1.56, 95% CI 1.44 to 1.69) compared with that in the late cohorts (1.29, 95% CI 1.17 to 1.42) (p for interaction <0.01) (table 2).
Figure 1.
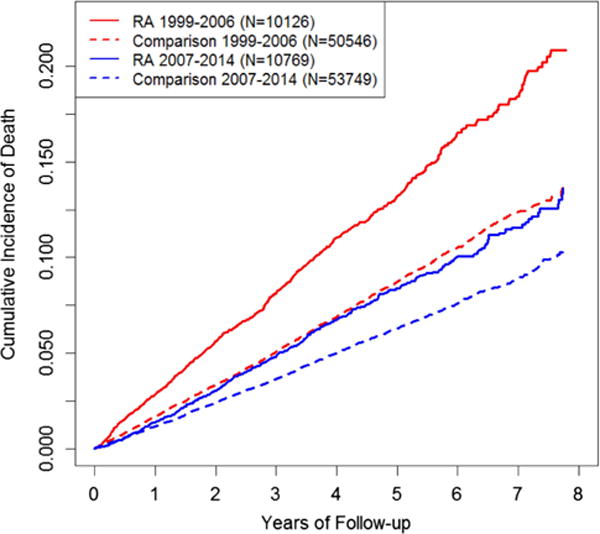
Graph showing the cumulative mortality of patients with rheumatoid arthritis (RA) and corresponding individuals without RA in early versus late cohorts (1999–2006 vs 2007–2014, respectively).
Table 2.
Association between RA and all-cause mortality according to time period
| 1999–2006 | 2007–2014 | p for interaction | |||
|---|---|---|---|---|---|
| RA cohort (n=10 126) | Non-RA cohort (n=50 546) | RA cohort (n=10 769) | Non-RA cohort (n=53 749) | ||
| Mean follow-up (person-years) | 3.18±2.13 | 3.25±2.15 | 330±2.18 | 330±2.21 | |
| Deaths (n) | 936 | 2968 | 605 | 2293 | |
| Death rate/1000 PYs (95% CI) | 29.1 (27.2 to 30.1) | 18.0 (17.4 to 18.7) | 17.0 (15.7 to 18.4) | 12.9 (12.4–13.5) | |
| Age-matched, sex-matched and entry year-matched rate ratio (95% CI) | 1.66 (1.54 to 1.79) | 1.00 (Ref) | 1.35 (1.23 to 1.48) | 1.00 (Ref) | <0.01 |
| Multivariable-adjusted rate ratio (95% CI)* | 1.56 (1.44 to 1.69) | 1.00 (Ref) | 1.29 (1.17 to 1.42) | 1.00 (Ref) | <0.01 |
| Age-matched, sex-matched and entry year-matched rate difference/1000 PYs (95% CI) | 11.0 (9.0 to 13.0) | 0.0 (Ref) | 4.1 (2.6 to 5.6) | 0.0 (Ref) | <0.01 |
| Multivariable-adjusted rate difference/1000 PYs (95% CI)* | 9.5 (7.5 to 11.6) | 0.0 (Ref) | 3.1 (1.5 to 4.6) | 0.0 (Ref) | <0.01 |
In addition to the matching variables, multivariable models were adjusted for the number of GP visits, BMI, smoking status (ie, non-smokers, ex-smokers and current smokers), alcohol consumption (ie, non-drinkers, ex-drinkers and current drinkers), comorbidities and medication use prior to the index date.
BMI, body mass index; GP, general practitioner; PY, person-year; RA, rheumatoid arthritis.
A significant improvement in the excess mortality rate in patients with RA was also observed over the two time periods. The difference in mortality rate between patients with RA and individuals without RA was 11.0 deaths per 1000 person-years (95% CI 9.0 to 13.0) in the early cohorts and 4.1 deaths per 1000 person-years (95% CI 2.6 to 5.6) in the late cohorts (p for interaction <0.01). The corresponding multivariable-adjusted rate difference remained higher in the early cohorts than in the late cohorts (p for interaction <0.01). The mortality trends among patients with RA and its effect modification by time period was significant among both women and men (table 3). In our analysis using an alternative definition of RA (READ code plus the use of a DMARD), the baseline characteristics remained similar between groups (see online supplementary eTable 1). The multivariable-adjusted HRs and rate differences were similarly larger in the early cohorts than in the late cohorts (table 4).
Table 3.
Association between RA and all-cause mortality by sex and time period
| 1999–2006 | 2007–2014 | p for interaction | |||
|---|---|---|---|---|---|
| RA cohort | Non-RA cohort | RA cohort | Non-RA cohort | ||
| Men | 3006 | 14 992 | 3382 | 16 878 | |
| Death rate/1000 PYs (95% CI) | 37.0 (33.2 to 41.0) | 23.0 (21.6 to 24.3) | 22.3 (19.6 to 25.3) | 17.8 (16.7 to 19.0) | |
| Multivariable-adjusted rate ratio (95% CI)* | 1.51 (1.32 to 1.72) | 1.00 (Ref) | 1.21 (1.04 to 1.41) | 1.00 (Ref) | 0.02 |
| Multivariable-adjusted rate difference/1000 PYs (95% CI)* | 12.1 (7.4 to 16.8) | 0.0 (Ref) | 3.5 (0.1 to 6.9) | 0.0 (Ref) | <0.01 |
| Women | 7120 | 35 554 | 7387 | 36 871 | |
| Death rate/1000 PYs (95% CI) | 25.8 (23.7 to 27.9) | 16.0 (15.3 to 16.7) | 14.7 (13.2 to 16.3) | 10.8 (10.2 to 11.4) | |
| Multivariable-adjusted rate ratio (95% CI)* | 1.60 (1.44 to 1.77) | 1.00 (Ref) | 1.34 (1.19 to 1.52) | 1.00 (Ref) | <0.01 |
| Multivariable-adjusted rate difference/1000 PYs (95% CI)* | 8.5 (6.2 to 10.8) | 0.0 (Ref) | 2.9 (1.2 to 4.6) | 0.0 (Ref) | <0.01 |
In addition to the matching variables, multivariable models were adjusted for the number of GP visits, BMI, smoking status (ie, non-smokers, ex-smokers and current smokers), alcohol consumption (ie, non-drinkers, ex-drinkers and current drinkers), comorbidities and medication use prior to the index date.
BMI, body mass index; GP, general practitioner; PY, person-year; RA, rheumatoid arthritis.
Table 4.
Association between DMARD-treated RA and all-cause mortality according to time period
| 1999–2006 | 2007–2014 | p for interaction | |||
|---|---|---|---|---|---|
| RA cohort (n=5775) | Non-RA cohort (n=28 653) | RA cohort (n=7922) | Non-RA cohort (n=39 059) | ||
| Mean follow-up (PYs) | 3.20±2.13 | 3.21±2.15 | 3.38±2.19 | 3.32±2.20 | |
| Deaths (n) | 415 | 1353 | 381 | 1528 | |
| Death rate/1000 PYs (95% CI) | 22.5 (20.4 to 24.8) | 14.7 (13.9 to 15.5) | 14.2 (12.8 to 15.7) | 11.8 (11.2 to 12.4) | |
| Age-matched, sex-matched and entry year-adjusted rate ratio (95% CI) | 1.54 (1.37 to 1.72) | 1.00 (Ref) | 1.21 (1.08 to 1.36) | 1.00 (Ref) | <0.01 |
| Multivariable-adjusted rate ratio (95% CI)* | 1.50 (1.33 to 1.69) | 1.00 (Ref) | 1.15 (1.02 to 1.29) | 1.00 (Ref) | <0.01 |
| Age-matched, sex-matched and entry year-adjusted rate difference/1000 PYs (95% CI) | 7.8 (5.5 to 10.0) | 0.0 (Ref) | 2.4 (0.9 to 3.9) | 0.0 (Ref) | <0.01 |
| Multivariable-adjusted rate difference/1000 PYs (95% CI)* | 5.5 (3.0 to 8.0) | 0.0 (Ref) | 1.5 (−0.1 to 3.2) | 0.0 (Ref) | <0.01 |
In addition to the matching variables, multivariable models were adjusted for the number of GP visits, BMI, smoking status (ie, non-smokers, ex-smokers and current smokers), alcohol consumption (ie, non-drinkers, ex-drinkers and current drinkers), comorbidities and medication use prior to the index date.
BMI, body mass index; DMARD, disease-modifying anti-rheumatic drug; GP, general practitioner; PY, person-year; RA, rheumatoid arthritis.
In our sensitivity analysis varying the PPVs of our RA definition at 80%, 85%, 90% and 95%, the corresponding corrected relative risks for mortality were 1.69, 1.65, 1.61 and 1.58 in the early cohorts and 1.32, 1.30, 1.28 and 1.27 in the late cohorts, respectively, thus suggesting that our observed results with an 80% PPV are conservative. When we repeated our analyses using smoking status, alcohol consumption and BMI variables assessed within 2 years prior to the index date, the multivariable-adjusted HR of all-cause mortality for RA remained larger in the early cohorts (1.84, 95% CI 1.51 to 2.24) compared with that in the late cohorts (1.33, 95% CI 1.14 to 1.56), whereas the difference in the mortality rate between patients with RA and individuals without RA was 12.8 deaths per 1000 person-years (95% CI 8.5 to 17.2) in the early cohorts and 2.7 deaths per 1000 person-years (95% CI 1.3 to 4.1) in the late cohorts (p for interaction <0.01). When we repeated our analyses by excluding patients who were on a DMARD before the first diagnosis of RA and extending the period to 3 years of observation without a diagnosis of RA, the multivariable-adjusted HR of all-cause mortality for RA remained larger in the early cohorts (1.71, 95% CI 1.39 to 2.11) compared with that in the late cohorts (1.38, 95% CI 1.14 to 1.67), whereas the difference in the mortality rate between patients with RA and individuals without RA was 10.4 deaths per 1000 person-years (95% CI 6.2 to 14.6) in the early cohorts and 2.5 deaths per 1000 person-years (95% CI 0.3 to 4.8) in the late cohorts (p for interaction <0.01).
DISCUSSION
In this general population-based cohort study from 1999 to 2014, we found that all-cause mortality from RA has improved to a greater degree than the background improvement of the general population. There were 10 excess deaths per 1000 person-years due to RA in the early period, which reduced to 3 excess deaths during the late period. As a relative risk, patients with RA had a 56% higher risk of all-cause mortality during the early period and a 29% higher risk during the late period compared with individuals without RA. These improvements in RA mortality trends appeared similar among men and women. Similar trends were noted in our DMARD-treated RA cohorts. These findings suggest substantial survival improvement among patients with RA in recent years.
Our mortality rate estimates were highly congruent with those from previous population-based incident RA cohort studies.7,8 For example, all-cause mortality rate of our early RA cohort (29.1/1000 person-years) was quite similar to that of the inception RA cohorts from Rochester Olmsted County where RA occurred between 1995 and 2000 (ie, 24/1000 person-years).7 The Norfolk Arthritis Register RA study population at baseline was several years younger than that of our study or the Olmsted County study, which was reflected in their slightly lower mortality rates (21 and 20 deaths/1000 person-years in the inception RA cohorts of 1995–1999 and of 2000–2004, respectively).8 Regardless, the mortality rate in our late RA cohort was lower (ie, 17.0/1000 person years) than both studies. These consistencies with previous population-based incident RA cohort studies provide further support for the validity of our findings, thereby allowing us to extend the previous benchmark mortality data7,8 to the most recent incident RA cohort available to date. These data collectively suggest that the perceived improvements in RA care since the late 1990s and early 2000s may have been translated into a survival benefit in the past decade.
In addition to the aforementioned increasing use of biological DMARDs, there has also been effective use of conventional DMARDs with appropriate dosing and mode of administration, as well as effective combination therapy. For example, a recent UK study has reported a tripling in methotrexate prescriptions between 2001 and 2012 and a 156% annual increase in the use of tumour necrosis factor inhibitors.20 Furthermore, the early and effective intervention for RA to help prevent permanent damage has been increasingly adopted and treat-to-target strategies have been widely advocated.2–5 Collectively, all of these measures have reduced the disease activity of RA and seem to have led to an improvement in the longevity of patients with RA, as observed in our study.
Our study has several strengths and limitations. First, our study is a general population-based cohort study; thus, our findings are likely to be generalisable. Second, unlike previous studies that adjusted for age and sex for standardised mortality ratios,7 we adjusted for several potential confounders prior to RA diagnosis (ie, obesity, smoking, comorbidities and medication use), thereby reducing a potential residual confounding effect. Third, using incident RA cases minimises the selection bias that may underestimate the risk of death if prevalent RA cases were included in the analysis.21 However, uncertainty surrounding diagnostic accuracy is a potential concern. The overall accuracy of using EMRs to assess important outcomes appears to be high as reflected in many validation studies,22–26 including that of our RA diagnosis.13,14 The improving trend over the two periods was also evident using our more specific alternative definition (ie, a physician-recorded diagnosis of RA plus the use of a DMARD).15 Furthermore, our sensitivity analysis varying the PPVs of our RA definition showed that our observed results are likely conservative and the aforementioned close agreement with previous population-based incident RA cohort studies7,8 also lends support to the validity of our findings. We did not have sufficient detail on the cause of death in a number of cases in our dataset, precluding investigations on the cause of death in this cohort. Nevertheless, the overall all-cause mortality trends are critically important in their own right, as mortality represents the overall net health outcome of various benefits and risks associated with disease management.27 Furthermore, our data did not allow for the assessment of the natural history of RA presentation, calling for future studies on this topic. Finally, it would also be valuable for future studies to assess to what extent the improved survival among patients with RA is directly attributable to the improvement of RA management and disease activity.
In conclusion, this general population-based cohort study indicates that the survival of patients with RA has improved over the past decade to a greater degree than in the general population. These data provide a key benchmark for the perceived improvement in RA care during the biological era.
Acknowledgments
Funding This project was supported in part by the NIH grant P60-AR-047785.
Footnotes
Handling editor Tore K Kvien
Competing interests None declared.
Provenance and peer review Not commissioned; externally peer reviewed.
Data sharing statement The data for this specific analysis will be shared if asked.
References
- 1.Dadoun S, Zeboulon-Ktorza N, Combescure C, et al. Mortality in rheumatoid arthritis over the last fifty years: systematic review and meta-analysis. Joint Bone Spine. 2013;80:29–33. doi: 10.1016/j.jbspin.2012.02.005. [DOI] [PubMed] [Google Scholar]
- 2.O’Dell JR. Therapeutic strategies for rheumatoid arthritis. N Engl J Med. 2004;350:2591–602. doi: 10.1056/NEJMra040226. [DOI] [PubMed] [Google Scholar]
- 3.Singh JA, Saag KG, Bridges SL, et al. 2015 American College of Rheumatology Guideline for the Treatment of Rheumatoid Arthritis. Arthritis Care Res (Hoboken) 2016;68:1–25. doi: 10.1002/acr.22783. [DOI] [PubMed] [Google Scholar]
- 4.Smolen JS, Landewé R, Breedveld FC, et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifying antirheumatic drugs: 2013 update. Ann Rheum Dis. 2014;73:492–509. doi: 10.1136/annrheumdis-2013-204573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ward MM. Decreases in rates of hospitalizations for manifestations of severe rheumatoid arthritis, 1983–2001. Arthritis Rheum. 2004;50:1122–31. doi: 10.1002/art.20158. [DOI] [PubMed] [Google Scholar]
- 6.Peters MJ, Symmons DP, McCarey D, et al. EULAR evidence-based recommendations for cardiovascular risk management in patients with rheumatoid arthritis and other forms of inflammatory arthritis. Ann Rheum Dis. 2010;69:325–31. doi: 10.1136/ard.2009.113696. [DOI] [PubMed] [Google Scholar]
- 7.Gonzalez A, Maradit Kremers H, Crowson CS, et al. The widening mortality gap between rheumatoid arthritis patients and the general population. Arthritis Rheum. 2007;56:3583–7. doi: 10.1002/art.22979. [DOI] [PubMed] [Google Scholar]
- 8.Humphreys JH, Warner A, Chipping J, et al. Mortality trends in patients with early rheumatoid arthritis over 20 years: results from the Norfolk Arthritis Register. Arthritis Care Res (Hoboken) 2014;66:1296–301. doi: 10.1002/acr.22296. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Saunders SA, Capell HA, Stirling A, et al. Triple therapy in early active rheumatoid arthritis: a randomized, single-blind, controlled trial comparing step-up and parallel treatment strategies. Arthritis Rheum. 2008;58:1310–17. doi: 10.1002/art.23449. [DOI] [PubMed] [Google Scholar]
- 10.National Health Service (NHS) Read codes: NHS connecting for health. http://www.connectingforhealth.nhs.uk/systemsandservices/data/uktc/readcodes.
- 11.First Databank. Multilex drug data file. http://www.firstdatabank.co.uk/8/multilex-drug-data-file.
- 12.Blak BT, Thompson M, Dattani H, et al. Generalisability of The Health Improvement Network (THIN) database: demographics, chronic disease prevalence and mortality rates. Inform Prim Care. 2011;19:251–5. doi: 10.14236/jhi.v19i4.820. [DOI] [PubMed] [Google Scholar]
- 13.Rodríguez LA, Tolosa LB, Ruigómez A, et al. Rheumatoid arthritis in UK primary care: incidence and prior morbidity. Scand J Rheumatol. 2009;38:173–7. doi: 10.1080/03009740802448825. [DOI] [PubMed] [Google Scholar]
- 14.Watson DJ, Rhodes T, Cai B, et al. Lower risk of thromboembolic cardiovascular events with naproxen among patients with rheumatoid arthritis. Arch Intern Med. 2002;162:1105–10. doi: 10.1001/archinte.162.10.1105. [DOI] [PubMed] [Google Scholar]
- 15.Thomas SL, Edwards CJ, Smeeth L, et al. How accurate are diagnoses for rheumatoid arthritis and juvenile idiopathic arthritis in the general practice research database? Arthritis Rheum. 2008;59:1314–21. doi: 10.1002/art.24015. [DOI] [PubMed] [Google Scholar]
- 16.Khan NF, Perera R, Harper S, et al. Adaptation and validation of the Charlson Index for Read/OXMIS coded databases. BMC Fam Pract. 2010;11:1. doi: 10.1186/1471-2296-11-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rod NH, Lange T, Andersen I, et al. Additive interaction in survival analysis: use of the additive hazards model. Epidemiology. 2012;23:733–7. doi: 10.1097/EDE.0b013e31825fa218. [DOI] [PubMed] [Google Scholar]
- 18.Raghunathan TE, Lepkowski JM, Van Hoewyk J, et al. A multivariate technique for multiply imputing missing values using a sequence of regression models. Surv Methodol. 2001;27:85–95. [Google Scholar]
- 19.Lash TL, Fox MP, Fink AK. Applying quantitative bias analysis to epidemiologic data. New York: Springer; 2009. [Google Scholar]
- 20.Harty L, O’Toole G, FitzGerald O. Profound reduction in hospital admissions and musculoskeletal surgical procedures for rheumatoid arthritis with concurrent changes in clinical practice (1995–2010) Rheumatology (Oxford) 2015;54:666–71. doi: 10.1093/rheumatology/keu340. [DOI] [PubMed] [Google Scholar]
- 21.Choi HK, Nguyen US, Niu J, et al. Selection bias in rheumatic disease research. Nat Rev Rheumatol. 2014;10:403–12. doi: 10.1038/nrrheum.2014.36. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.García Rodríguez LA, Varas-Lorenzo C, Maguire A, et al. Nonsteroidal anti-inflammatory drugs and the risk of myocardial infarction in the general population. Circulation. 2004;109:3000–6. doi: 10.1161/01.CIR.0000132491.96623.04. [DOI] [PubMed] [Google Scholar]
- 23.Martín-Merino E, García-Rodríguez LA, Massó-González EL, et al. Do oral antimuscarinic drugs carry an increased risk of acute urinary retention? J Urol. 2009;182:1442–8. doi: 10.1016/j.juro.2009.06.051. [DOI] [PubMed] [Google Scholar]
- 24.Hall GC. Validation of death and suicide recording on the THIN UK primary care database. Pharmacoepidemiol Drug Saf. 2009;18:120–31. doi: 10.1002/pds.1686. [DOI] [PubMed] [Google Scholar]
- 25.Meal A, Leonardi-Bee J, Smith C, et al. Validation of THIN data for non-melanoma skin cancer. Qual Prim Care. 2008;16:49–52. [PubMed] [Google Scholar]
- 26.Martín-Merino E, Ruigómez A, Johansson S, et al. Study of a cohort of patients newly diagnosed with depression in general practice: prevalence, incidence, comorbidity, and treatment patterns. Prim Care Companion J Clin Psychiatry. 2010;12:PCC 08m00764. doi: 10.4088/PCC.08m00764blu. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Prasad V. But how many people died? Health outcomes in perspective. Cleve Clin J Med. 2015;82:146–50. doi: 10.3949/ccjm.82a.14058. [DOI] [PubMed] [Google Scholar]


