Abstract
Background:
This study aimed to use a mixed-method approach to investigate affecting factors on the performance of Community Health Workers (CHW) in Iran’s villages.
Methods:
This study was conducted during 2014–2015 with a mixed method in three phases of literature review, Delphi technique and developing a rich picture. Overall, in order to finalize the affecting factors and their relationships between qualitative content analysis, Delphi technique, AHP technique and Focus Group Discussion were used, respectively.
Results:
Affecting factors on CHW performance were divided into four main categories, 10 sub-themes and 35 contents. Increase in the level of people’s awareness, disease patterns, demographic structure and lifestyle were placed in four priorities respectively on the basis of importance.
Conclusion:
To the most extent CHW cannot face current needs of rural communities. It challenges equitable access to healthcare services and also conflicts with the primary philosophy of CHW presence in rural areas. CHW can be used in two forms; either as an assistant to rural family physicians or with the same previous functions.
Keywords: Affecting factors, CHW, Performance, Rural areas, Iran
Introduction
The primary objective of health system is to improve the accessibility of underserved groups and to reduce rural and urban inequalities in benefiting health care outcomes (1). Hence, after the Islamic Revolution in Iran, the government increased its focus on rural areas and established primary health care system. Iran’s Primary Health Care (PHC) System was developed for the provision of health services in rural centers and health houses in which CHW performs in the most basic level (2). CHW is currently the most vital health service delivery agent in Iran’s health system. Significant results in the society’s health status are the achievements of high effectiveness in CHW performance (3), especially improvement in the health of mothers and children and in most health indicators during the last 40 yr (2). However, in the best circumstances, if a structure designed according to the existing needs remains unchanged, it gradually loses its responsiveness to the needs in course of changing conditions (4–7). Currently, primary health care networks in rural areas are facing several challenges in meeting the population needs (8–10). Based on the findings, CHWs in Iran have faced new challenges in the trend of health care and their abilities in terms of skills and educational competencies has led to decrease in their productivity and effectiveness in response to current needs of the community which is constantly changing, consequently it has resulted in decline in the inclination the community to approach them for receiving services (2). CHW’s activities in the primary years of the plan was commensurate to the needs of the community, however, today, it requires other health care plans to address non-communicable diseases, prevention and control of high-risk behavior and lifestyle improvement (11). Literature state that inappropriate training is caused by decrease in the level of motivation and self-confidence and poor performance is due to absence, low quality of performance, weakness in managerial and organizational affairs (12). Moreover, lack of occupational vision has negative effect on the performance of CHWs and had resulted in significant decline (13, 14).
Literature indicate various constraints and they mainly address certain aspects of CHW challenges, hence, there is an urgent necessitate in Iran to identify and study them and provide an in-depth understanding (2).Therefore, the present study aimed to use a mixed-methods approach to investigate affecting factors on CHW performance in rural community of Iran.
Methods
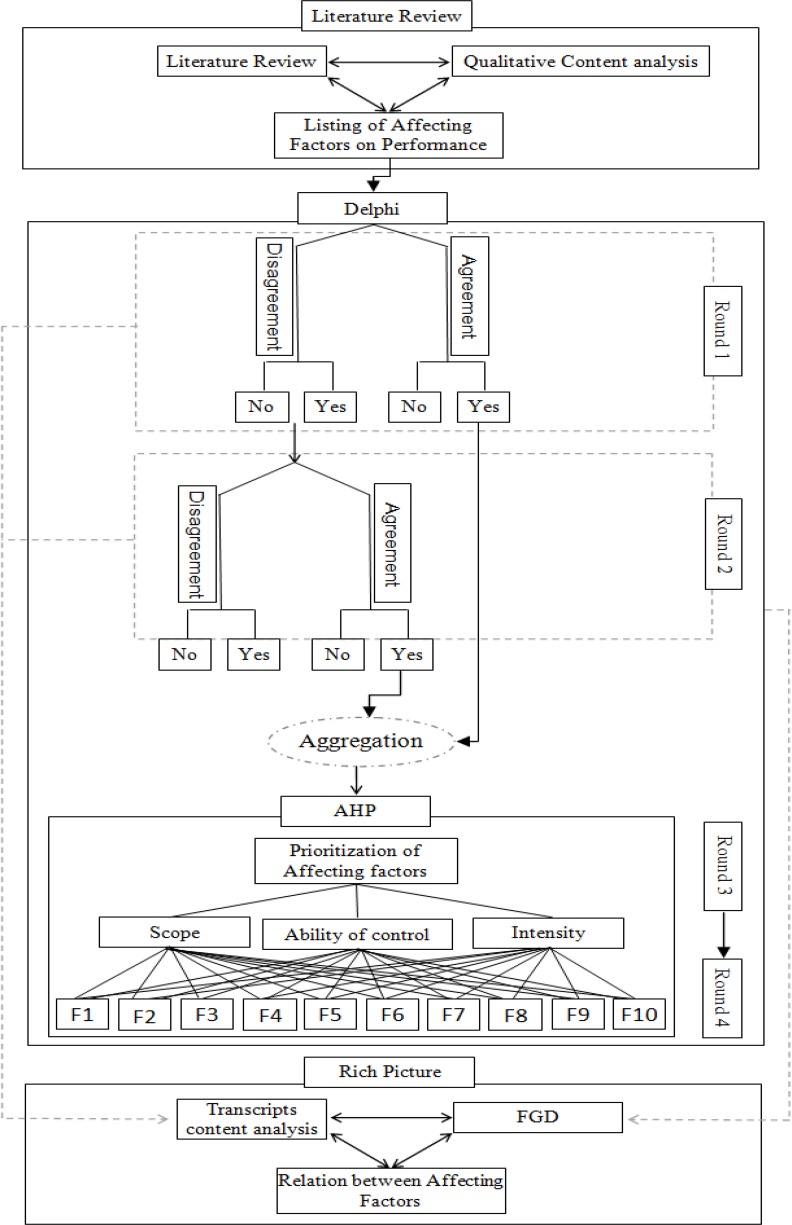
The present study was conducted during 2014–2015 with a mixed method in three phases of literature review, Delphi technique and rich picture for showing the relationships between factors (Fig. 1).
Fig. 1:
Study framework
Phase 1: literature Review
Aiming to extract affecting factors on the performance of CHW in three steps a list of the factors was developed.
I. Extraction of Previous Studies
The relevant studies were extracted including scientific articles, books, published and unpublished reports and etc. Articles were collected with Narrative method by two independent research groups. The keywords included Persian words and their English equivalents of Behvarz, Health Worker and lay health workers, auxiliary health workers, community health worker in Google Scholar, Iranian Scientific Information Database (SID), Magiran, PubMed, and web of knowledge in data banks in the first six months of 2014.
II. Qualitative Content Analysis
Each article was reviewed independently by two researchers and in order to perform a more comprehensive data extraction, all qualitative themes and data which were relevant to the research objective were extracted. Subsequently, discussion and agreement of the researchers about the extracted themes of an article led to formation of primary themes. Finally, the primary themes of all articles were integrated with each other in one document.
I. Themes Integration
The primary themes integrated were discussed in meetings between all the researchers and the head of the team. The irrelevant themes were omitted and new sub-themes were added, additionally, theme contents were changed based on the integration. The classification was designed with the aim of having complete separate classes from each other.
Phase 2: Delphi
According to the preliminary framework prepared in previous steps, as Fig. 1 shows, Delphi technique was used in an expert panel to finalize the affecting factors (15) followed by integration of Delphi and Analytic Hierarchy Process (AHP) (16) to prioritize the factors from expert panel point of view.
Given that the validity of a Delphi study depends on the combination of experts in the panel, a list of various stakeholders and policy makers related to the topic were selected at first and 30 of them were selected on the basis of knowledge and experience, their willingness to cooperate, having enough time and effective communication skills (17).
Delphi technique in the present study has four rounds from which rounds one and two are related to preparation and finalization of the factors. Rounds three and four include prioritization of the factors on the level of their influence on CHW performance. Before entering the stage of using the Delphi technique the developed framework of affecting factors in the previous step became a form with questions that provided Yes/No answers and open questions.
Round 1
At the beginning, the designed form was sent to the experts. The form structure allowed the experts to reply Yes/No and in case elaborate on their answers.
After examining replies in this stage, results were in two groups; those who agree and disagree. Agree ones are the groups which at least 70% of responses for one option was Yes/No and on the contrary in “the disagree group” less than 70% of responses to an option was Yes/No.
Round 2
The disagree options in addition to the points of view of experts about each one of them were again sent to all experts without any statistical information like the first round and the results were then analyzed.
At the end of this step agree group for Yes from round one and two were integrated and agree group for No of rounds one and two plus disagree group of round two were omitted from the study. The affecting factors were finalized through this way into four main categories, ten themes and 35 sub-themes.
Round 3
In this step of Delphi technique process finalized categories of affecting factors on CHW performance were placed in AHP for a pairwise comparison on a quintet scale (equal, moderate, strong, very strong, and extreme) and were sent back to the experts. They were asked to compare affecting factors two by two based on the criteria of intensity, size and ability to control and leave their comments if any at all.
Round 4
In the second step of the integrated process of Delphi technique and AHP, finalized categories of affecting factors accompanied with average obtained weights from the first step was sent back to the same experts. In this step, they were asked to revise their responses with regard to the collected information of round three and include their comments. At the end of this step in order to evaluate the level of convergence between the two steps (rounds) t-test was used to examine the level of assurance through checking the differences between averages of standard deviations obtained from each step (P>0.05). Given the lack of significant difference between the average values of the two stages of the analysis, average values obtained in the second round of Delphi-AHP was entered to Expert choice software as the final result of prioritization of factors affecting CHW performance.
Phase 3: Rich picture
The factors have complex relationships and to precisely define their connections and influences a rich picture was used. Firstly, the written points of view were analyzed and a preliminary picture was drawn. Thereafter, a number of the experts were invited to focus group discussions.
The group discussions were led by one of the researchers of the ministry HRM office and two HR staffs were responsible to take notes. In two FGD sessions of 45 and 60 min the attendees reached consensus followed by agreed saturation of information. In the first session the research question was raised and the obtained results after the analysis of the experts’ points of view in previous steps were discussed as well as the relationships between the factors. The discussions were recorded and transcribed. In the second session, the results of the first session were elaborated and finalized. Noting the existing guidelines they were portrayed into a rich picture (18).
Results
Phase 1: literature Review
With regard to the research objective 19 articles were selected and related conceptual elements in the selected studies were extracted and a list of 55 affecting factors was prepared as primary themes.
Phase 2: Delphi
I. Participations
The expert panel included eight policy makers from the headquarter of MOHME who were four manager (two from HRH area and two from public health area) and four expert staff from deputy of public health. Other participants were 22 managers and seven experts from out of the head quarter who were from public health deputies of medical universities (environmental experts), five managers of health centers and 10 expert staffs of public health deputies. Most of the participants were male (57%).
II. Round 1
Twenty five participants responded to the first form (83% responding rate). In this round 58% of factors scored more than 70% and were grouped as agree (22 Yes and 10 No) and the rest of factors (23 themes) were grouped as disagree.
III. Round 2
From 25 participants in the first round 22 experts responded to the second form (88% responding rate). From disagree group 16 factors scored more than 70% (13 Yes and 3 No). On the whole, by omitting the agree groups for No in rounds one and two and disagree groups in the second round and also integration of agree groups for Yes in both rounds affecting factors on CHW performance are finalized as below:
The affecting factors on CHW performance are classified in four main categories.These themes are organized into 10 sub-themes and 35 contents as shown in Table 1.
Table 1:
Factors affecting CHW performance
| Main themes | Sub-themes | Content |
|---|---|---|
| Compatibility of services with health-demographic transition | Change in demographic structure |
|
| Change in lifestyle |
|
|
| Change in disease patterns |
|
|
| Acceptability of services with regard to change in attitudes and expectations of rural communities | Increase in the level of people’s awareness and expectations |
|
| Poor compatibility of training contents with changed role of CHW |
|
|
| CHW motivation and expectations | Increase in the range and scope of CHW assigned activities |
|
| CHW’s job motivation |
|
|
| Increase in Beaverz’s expectation contrary to primary policies in selection of CHW as a local workforce |
|
|
| Team communication and organization | Supportive-supervisory barriers |
|
| Neglecting CHW role in rural family physician plan |
|
1) Demographic-Health Transition
One of the principle factors agreed by all the experts relates to two major transitions in Iran which happened during the last 30 years. Due to migration to cities and reduction in fertility, population pyramid has changed from a complete young structure to a relatively old structure. On the one hand, “declining trend in unwanted fertility rates and population growth due to good and effective performance of CHW plus settled family control principles have led to reduction in vulnerable population including pregnant women and children for CHW specially trained to serve this group”. In CHW training plan, there is no place for delivering complex services to the elderly. Accordingly, Experts believe that “Handling non-communicable diseases, especially in elderlies, is mainly in the area of physicians and health professionals and is beyond the expertise, ability and knowledge of current CHW. He/she does not have the essential information, facilities and capabilities for treating and following up the emerging diseases.”
2) Service acceptability according to change in rural attitudes and expectation
Increase in health literacy level along with increased access to mass media has resulted in change of rural attitudes, expectations and behaviors. Besides, access to physicians through rural family physicians has resulted in decrease to visit CHW and increased willingness to visit physicians out of referral route in hope of receiving services with higher quality. In fact based on experts’ views; “educated rural people have little inclination to follow CHW who has lower education.”
3) CHW Motivation and Expectations
Demographic transition and the growing trend of rural population expectations from CHW in addition to repetition of tasks resulting from the integration of new primary health care plans are causing pressure on CHW for provision of services that they are not trained for. According to the literature, “CHW feels an inequality in this respect since they should stay in villages until retirement and they believe that this means exclusion from urban facilities and living with limited facilities of rural life. Moreover, unlike other employees they do not have promotion opportunity in their career.”
4) Organization and Team Communications:
Policy makers’ personal preference and lack of supervision are emphasized issues. As in rural family physician plan overlap or inconsistency in the tasks of health service delivery team is highlighted. According to the experts, “physicians and CHW do their work separately and do not interact with each other. In fact, CHW would not be informed of the patient who visits a doctor and this prevents her from following up the patients’ cases”.
Moreover, there is a quite weak monitoring and supervision system on CHW. Experts said “In order to eliminate training defects and job problems, observers of health houses only visit and mention the errors and suffice to that level of supervision. They pay little attention to educating those regarding scientific and practical deficiencies so that they become able to tackle problems they face in the health houses.”
IV. Round 3
To prioritize the factors based on AHP, from 22 participants in finalization of the factors, 18 participants responded to the AHP forms (81% responding rate). Inconsistency ratio of pair comparisons is less than 1% which indicates significant accuracy of this paired comparison.
V. Round 4
In round 4 all 18 respondents of the previous step responded to the second AHP form (100% responding rate). Since inconsistency ratio of pair comparisons is less than 1% therefore the two by two comparisons of the factors is acceptable.
As Table 2 shows, based on considered criteria weighted scores of affecting factors on CHW performance was calculated and the results indicate that increase in the level of people’s awareness and expectations (0.2078) ‘Change in disease patterns (0.1966) ‘Change in demographic structure (0.1608) and Change in lifestyle (0.1587) are placed in four priorities respectively on the basis of importance and on the whole they cover 70% of the scores and are of the most prominent factors on CHW performance.
Table 2:
Weights and ranks of attributes, by AHP
| Criteria | Weights (C1, C2, C3) | Factors | Weights (A1, A2, A3) | Global | Adj. wgts. (C1,2,3*A1,2,3) | Rank | ||
|---|---|---|---|---|---|---|---|---|
| Intensity | Ability to control | Scope | ||||||
| Change in demographic structure | 0.0998 | 0.2588 | 0.2716 | 0.6302 | 0.1608 | 3 | ||
| Change in lifestyle | 0.1699 | 0.1143 | 0.149 | 0.4332 | 0.1587 | 4 | ||
| Intensity | 0.637 | Change in disease patterns | 0.1699 | 0.1738 | 0.2716 | 0.6153 | 0.1966 | 2 |
| Increase in the level of people’s awareness and expectations | 0.2539 | 0.1738 | 0.108 | 0.5357 | 0.2078 | 1 | ||
| Ability to control | 0.1047 | Poor compatibility of training contents with changed role of CHW | 0.0686 | 0.0737 | 0.0252 | 0.1675 | 0.0579 | 5 |
| Increase in the range and scope of CHW assigned activities | 0.0686 | 0.0477 | 0.0252 | 0.1415 | 0.0552 | 6 | ||
| CHW’s job motivation | 0.0686 | 0.0312 | 0.0184 | 0.1182 | 0.0517 | 7 | ||
| Scope | 0.2583 | Increase in Beaverz’s expectation contrary to primary policies in selection of CHW as a local workforce | 0.0434 | 0.0737 | 0.0252 | 0.1423 | 0.0419 | 8 |
| Supportive-supervisory barriers | 0.0365 | 0.0312 | 0.053 | 0.1207 | 0.0402 | 9 | ||
| Neglecting CHW role in rural family physician plan | 0.021 | 0.0218 | 0.053 | 0.0958 | 0.0293 | 10 | ||
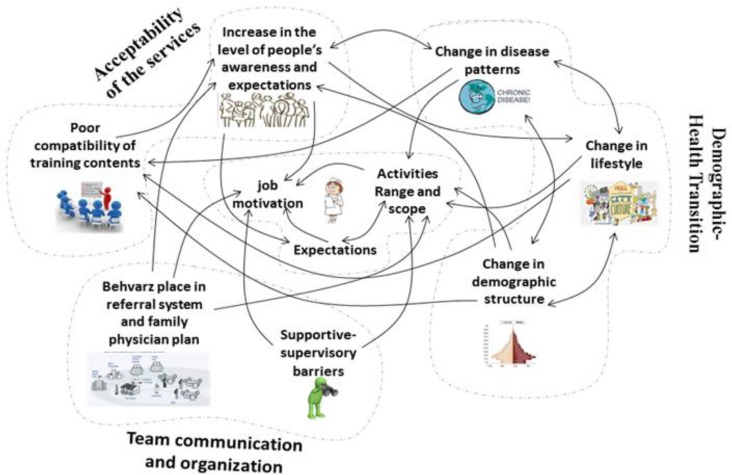
Phase 3: Rich Picture
As illustrated in Fig. 2, on the right side, there are factors relating to “Demographic-Health Transition”. This picture shows that factors of this class have mutual relation with each and also on the other factors. For instance, “Change in demographic structure” on one side has a mutual relation with “Change in lifestyle” and “Change in disease patterns” and on the other hand has effects on “Activities Range and scope”, “Increase in the level of people’s awareness and expectations”, “CHW expectations” and “Poor compatibility of training contents”. In the middle of the rich picture, there are factors relating to “CHW motivation and expectations” affected by the other factors. In other parts of the rich picture there are “Team communication and organization” and “Acceptability the services” in which their relationships has been shown.
Fig. 2:
Rich picture of the relationships between affecting factors on CHW performance
Discussion
The present study applied different methods including content analysis of the literature and using experts’ views to identify four factors affecting the performance of CHW. Through utilizing AHP model and a rich picture most significant affecting factors and their relationships were identified and finalized. Similarly, a study identified seven factors affecting CHWs’ performance through a review of studies (19). The present study addressed nature of career, training plans and needs and applied mechanisms in the evaluation of CHW’s performance and feed-backing system. This study was a cross-sectional study in a period of time while another study elaborates the fact that demographic and epidemiologic changes in Iran causes the emergence of new priorities in the related health plans, therefore, Iranian health care network is also affected which would lead to significant changes in the society’s structure and culture, especially in rural society(20). Consequently, CHW became a passive agent conveying the same old abilities for service delivery. Some studies indicate the significant effect of the mentioned changes on CHW performance (20, 21) putting the affecting factors in two categories; those relating to “demographic transition” and/or “services acceptability”. CHW’s roles remained the same or were not appropriately developed along with the other changes. Nevertheless, no attention has been paid to these changes.
A view to the results from Delphi technique and AHP indicate that the main priorities are included in the below two categories. The first priority which is “Increase in the level of people’s awareness and expectations” places in “Acceptability of services with regard to change in attitudes and expectations of rural communities” and the rest of the priorities (Change in disease patterns, Change in demographic structure, and Change in lifestyle) places in “health-demographic transition” and this overlap represents the comprehensiveness of the final results.
These affecting factors with regard to universal health coverage must be discussed (UHC). It means that reaching UHC in the area of human resources requires attention to all aspects including accessibility, availability, acceptability and quality (AAAQ) of human resources (22–24). Although, CHW existence brings availability of services, increase in the level of people’s awareness and expectations has distorted the acceptability of delivered services and consequently it is probable to decrease the accessibility of services as well due to lack of sufficient numbers of alternative service providers in most cases. Moreover, change in disease patterns, Change in demographic structure and Change in lifestyle as the second category of factors challenges the quality of services. Noting the ability of CHW for responding to the health needs of the society, as inferred CHWs, it is more of preventive rather than curative approach (25). In fact, as explicitly stated in the study, CHW does not have the required skills to effectively deliver services according to current community needs (2). Since based on a study CHWs are usually selected without any previous experiences or training about health in the community (26), in most countries they receive limited trainings as Prasad states that in India only three months and in Brazil six to eight months training is necessary to start the occupation (19).
For example, in 1992, during an EMRO specialized meeting regarding elderly care, regional health strategies for the elderly were determined for a period of a decade by the integration of elderly care in healthcare service delivery systems including a major part of it in primary health care (PHC) with emphasis on rural residents. However, with regard to the CHW role in Iran’s PHC, they have not acquired the essential skills to deliver elderly care. Even more, Iran used Australia’s elderly care guidelines and still did not mention the role of CHW in elderly care (27, 28). Most developed and developing countries not only face these two transitions of health-demographic and service acceptability, but created significant and deep effects on the performance and roles of community health workers in response to community needs. The consequences of these measures are evident in many studies (29, 30). For instance, dealing with change in disease patterns and increase of chronic diseases in United States of America resulted in organizing training programs for CHWs with the aim of controlling chronic disease risk factors. Each state has a specifically designed content and focus due to the emergence of diverse factors in different states. With the implementation of these training programs the CHWs became able to considerably decrease cardiovascular risks in women. Also, their advices were effective with regard to physical inactivity and the increasing trend of disease risk factors (blood hypertension, cholesterol, etc) and nutrition patterns (29, 31, 32). Conducted studies in India’s rural and urban areas indicate that it is possible to respond to the emergent need of communities in controlling a number of chronic disease risk factors with rapid training of health workers. Some of these factors are morbid obesity, cholesterol, and high blood sugar (33, 34). Important to state that in other areas of the world such as Africa there is a critical need for constant training of CHWs in emerging communicable diseases, Malaria and AIDS (35). In a national study in Iran regarding some risk factors such as diabetes and hypertension it reveals that interventional measures of trained CHW results in the diminution of this factors (36). However, CHW does not have the capacity to face all current needs of rural residents even with training or acquiring higher degrees. For example, CHW has limitations facing with chronic and emerging diseases. Prasad study indicates that since CHWs are selected from among the local residents they usually have primary level of education (8 to 10 yr of school) and they can be trained in this level (19). One study in South Africa based on a survey on nurses states that they do not accept CHWs in referral system as agents to deliver services since they do not receive specialized trainings and education (37).
This matter challenges equitable access to health services as one of the main elements of PHC and on the other hand, these limitations have affected CHW performance and have faded the basic philosophy of CHW presence as the only PHC service deliverer and rural community advocate.
Conclusion
Care process in communities has rapidly changed and these changes results in increased complexity in this process and new challenges emerge in service delivery to respond to the health needs of communities. Therefore, continuation of achievements gained by CHW plan requires fundamental revision in the content of the plan in line with environmental changes including the community’s health transition, population pyramid changes and etc. Bearing the aforementioned and according to the findings of the present study the following is recommended:
Applying various set of policies in different situations might be an appropriate response to confront these issues. One of these policies could be using extra clinical workforces (midwives, public health graduates, etc) had academic training to handle most of these challenges. Another policy could be using CHW in relatively advantaged rural areas as a complementary assistant to family physician in order to build a comprehensive communication with the population and following up the community under cover and also using CHW in underserved rural areas same way as before providing the revision of training contents and redefinition of health care services packages.
Ethical considerations
Ethical issues (Including plagiarism, informed consent, misconduct, data fabrication and/or falsification, double publication and/or submission, redundancy, etc.) have been completely observed by the authors.
Acknowledgments
We are sincerely grateful of the expert panel, managers and expert staff in Iran’s ministry of health and medical education and the ones in medical universities for their assistance through our discussions and for sharing their valuable opinions which elevated our work. The authors declare that there is no conflict of interests.
References
- 1.Javanparast S, Heidari G, Baum F. (2011). Contribution of Community Health Workers to the Implementation of Comprehensive Primary Health Care in Rural Settings: Iran. Teasdale–Corti Global Health Research Partnership Program, Ottawa, Canada http://www.globalhealthequity.ca/electronic%20library/Iran%20Final%20Project%20Report.pdf. [Google Scholar]
- 2.Abbaszadeh A, Eskandari M, Borhani F. (2013). Changing the care process: A new concept in Iranian rural health care. Asian Nurs Res (Korean Soc Nurs Sci),7(1): 38–43. [DOI] [PubMed] [Google Scholar]
- 3.Arab M, Pourreza A, Akbari F, Ramesh N, Aghlmand S. (2007). Job satisfaction on primary health care providers in the rural settings. Iran J Public Health, 36(3): 64–70. [Google Scholar]
- 4.Ansaripoor S, Hasanzadeh A, Rohani M, Moghadas T. (2014). Job Satisfaction of Behvarzan Working in Isfahan University of Medical Sciences. Health Inf Manage,10(7): 1095–10105. [Google Scholar]
- 5.Mottaghi M, Rajabi Z, Kachuee Z. (2012). The Effect of Training in the Field Of Primary Health Care (PHC) on Knowledge of Kashan Health Workers (Behvarz) 2004–2011. Res Med Educ, 4(1): 34–42. [Google Scholar]
- 6.Javanparast S, Labonte R, Sanders D. (2011). Community health workers’ perspectives on their contribution to rural health and well-being in Iran. Am J Public Health, 101(12): 2287–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Azizi F, Gouya M, Vazirian P, Dolatshahi P, Habibian S. (2003). The diabetes prevention and control programme of the Islamic Republic of Iran. East Mediterr Health J, (5–6): 1114–1121. [PubMed] [Google Scholar]
- 8.Shakiba M, Haghdoost A, Majdzadeh S. (2015). The Application of Geographical Information System in Explaining Spatial Distribution of Low Birth Weight; a Case Study in North of Iran. Iran J Med Sci, 33(4): 220–225. [Google Scholar]
- 9.Sadrizadeh B. (2004). Primary health care experience in Iran. Iran Red Crescent Med J, 7(1): 79–90. [Google Scholar]
- 10.Manenti A. (2011). Health situation in Iran. Med J Islam Repub Iran, 25(1): 1–7. [Google Scholar]
- 11.Ardalan A, Mowafi H, Ardakani HM, Abolhasanai F, Zanganeh A-M, Safizadeh H, et al. (2013). Effectiveness of a primary health care program on urban and rural community disaster preparedness, Islamic Republic of Iran: A community intervention trial. Disaster Med Public Health Prep, 7(05): 481–90. [DOI] [PubMed] [Google Scholar]
- 12.Glenton C, Inger BS, Pradhan S, et al. (2010). The female community health volunteer programme in Nepal: Decision makers’ perceptions of volunteerism, payment and other incentives. Soc Sci Med, 70 (12): 1920–1927. [DOI] [PubMed] [Google Scholar]
- 13.Shadpour K. (2000). Primary health care networks in the Islamic Republic of Iran. East Mediterr Health J, 6(4): 822–825. [PubMed] [Google Scholar]
- 14.Sadeghikho Sh, Yazdani Sh, Rahbar M, Ahmadi M. (2014). Behvarzes Viewpoints on their Abilities in Delivering Health Services. Hakim Health Sys Res, 17(2): 102–107. [Google Scholar]
- 15.Kastein MR, Jacobs M, van der Hell RH, Luttik K, Touw-Otten FWMM. (1993). Delphi, the issue of reliability: A qualitative Delphi study in primary health care in the Netherlands. Technol Forecast Soc Change, 44(3): 315–323. [Google Scholar]
- 16.Gunhan S, Arditi D. (2005). Factors affecting international construction. J Constr Eng Manag, 131: 273–282. [Google Scholar]
- 17.Landeta J. (2006). Current validity of the Delphi method in social sciences. Technol Forecast Soc Change, 73(5):467–482. [Google Scholar]
- 18.Bell S, Morse S. (2013). How people use rich pictures to help them think and act. Syst Pract Action Res, 26(4):331–348. [Google Scholar]
- 19.Prasad BM, Muraleedharan VR. (2007). Community health workers: a review of concepts, practice and policy concerns. London School of Hygiene & Tropical Medicine, United Kingdom: http://www.hrhresourcecenter.org/hosted_docs/CHW_Prasad_Muraleedharan.pdf. [Google Scholar]
- 20.Jafari N, Abolhassani F, Naghavi M, Pourmalek F, Lakeh MM, Kazemeini H, et al. (2009). National burden of disease and study in Iran. Iran J Public Health, 38(Suppl. 1): 71–73. [Google Scholar]
- 21.Movahedi M, Hajarizadeh B, Rahimi A, Arshinchi M, Amirhosseini K, Haghdoost AA. (2009). Trends and geographical inequalities of the main health indicators for rural Iran. Health Policy Plan, 24(3): 229–237. [DOI] [PubMed] [Google Scholar]
- 22.Kinney ED. (2001). The International Human Right to Health: What Does This Mean for Our Nation and World? Indiana Law Rev, 34(4): 1457–1475. [PubMed] [Google Scholar]
- 23.Chatterjee P. (2011). Progress patchy on health-worker crisis. Lancet, 377(9764):456. [DOI] [PubMed] [Google Scholar]
- 24.Campbell J, Buchan J, Cometto G, David B, Dussault G, Fogstad H, et al. (2013). Human resources for health and universal health coverage: fostering equity and effective coverage. Bull World Health Organ, 91(11): 853–863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Keshvari M, Mohammadi E, Boroujeni AZ, Farajzadegan Z. (2012). Burnout: interpreting the perception of Iranian primary rural health care providers from working and organizational conditions. Int J Prev Med, 3(Suppl. 1): S79–S88. [PMC free article] [PubMed] [Google Scholar]
- 26.Jafari M, Maleki MR, Eyvazi M, Khodayari R, Ahadi B. (2013). The study of relationship between job burnout and performance in East Azerbaijan's health house workers. J Health Syst Res, 9(11): 1375–1384. [Google Scholar]
- 27.Andrews KJ. (2001). National strategy for an ageing Australia: An older Australia, challenges and opportunities for all. 1st ed Department of Health and Aged Care, Australia, pp.: 38–53. [Google Scholar]
- 28.Davis S, Bartlett H. (2008). Review Article: Healthy ageing in rural Australia: Issues and challenges. Australas J Ageing, 27(2): 56–60. [DOI] [PubMed] [Google Scholar]
- 29.Cherrington A, Ayala GX, Amick H, Allison J, Corbie-Smith G, Scarinci I. (2008). Implementing the community health worker model within diabetes management challenges and lessons learned from programs across the United States. Diabetes Educ, 34(5): 824–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.O'Brien MJ, Squires AP, Bixby RA, Larson SC. (2009). Role development of community health workers: an examination of selection and training processes in the intervention literature. Am J Prev Med, 37(6): S262–S269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Gary TL, Bone LR, Hill MN, Levine DM, McGuire M, Saudek C, et al. (2003). Randomized controlled trial of the effects of nurse case manager and community health worker interventions on risk factors for diabetes-related complications in urban African Americans. Prev Med, 37(1): 23–32. [DOI] [PubMed] [Google Scholar]
- 32.Noor HH. Role and Effectiveness of Community Health Workers Among Underserved US Populations [MS thesis]. Wright State University, Dayton, Ohio; 2012. [Google Scholar]
- 33.Dehghan A, Ghavami L, Ghahramani F, Bazrafshan M, Namavar S. (2012). Prevalence of Depression and its Relation with Larestan Rural Health Workers’ Performance in 2010: A Short Report. J Rafsanjan Univ Med scie, 11(1): 79–84. [Google Scholar]
- 34.Islam NS, Zanowiak JM, Wyatt LC, Kavathe R, Singh H, Kwon SC, et al. (2014). Diabetes prevention in the New York City Sikh Asian Indian community: a pilot study. Int J Environ Res Public Health, 11(5): 5462–5486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Tsolekile LP, Puoane T, Schneider H, Levitt NS, Steyn K. (2014). The roles of community health workers in management of non-communicable diseases in an urban township. Afr J Prim Health Care Fam Med, 6(1): E1–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Farzadfar F, Murray CJ, Gakidou E, Bossert T, Namdaritabar H, Alikhani S, et al. (2012). Effectiveness of diabetes and hypertension management by rural primary health-care workers (Behvarz workers) in Iran: a nationally representative observational study. Lancet, 379(9810): 47–54. [DOI] [PubMed] [Google Scholar]
- 37.Doherty TM, Coetzee M. (2005). Community health workers and professional nurses: defining the roles and understanding the relationships. Public Health Nurs, 22(4): 360–365. [DOI] [PubMed] [Google Scholar]