Abstract
For HIV-infected parents, deciding whether and how to disclose their illness to their children is a major stressor. In China, due to significant HIV stigma, disclosure distress is acute. Our objective was to understand HIV-infected parents' concerns regarding disclosure of their HIV status to their children. HIV-infected parents (N = 10) were recruited to attend a 3-session nursing intervention. In our post-hoc analysis, progress notes from each session were analyzed for themes to illuminate parental decision-making processes. By the end of the intervention, all parents had considered the importance of HIV disclosure and stated that they felt somewhat prepared to disclose. Primary themes included (a) severe stigma experienced by fathers who were sexually active with men, (b) need for both parents to agree on plans for disclosure, and (c) parents' fears about the consequences of disclosure. Parents living with HIV can benefit from nurse-delivered interventions during parental HIV disclosure decision-making.
Keywords: children, China, disclosure, HIV, intervention, nursing, parent
Globally, there are more than 33 million people living with HIV (PLWH), with an estimated 780,000 infections in China (World Health Oragnization, Joint United Nations Programme on HIV/AIDS, & United Nations International Children's Emergency Fund, 2010). For Chinese PLWH, social stigma is a critical concern (Ministry of Health People's Republic of China Joint United Nations Programme on HIV/AIDS World Health Organization, 2015). The Chinese government is committed to curbing the spread of HIV as it has recognized the serious health, economic, and security challenges the epidemic poses (Li et al., 2011). In 2004, a State Council HIV/AIDS Working Committee was assembled as part of the government's ongoing effort to address the epidemic. Based on recommendations from this council, national legislation was passed to establish HIV treatment and testing centers throughout China and to provide widespread free antiretroviral therapy (ART) and care for children affected by HIV (Ministry of Health People's Republic of China Joint United Nations Programme on HIV/AIDS World Health Organization, 2006). There is currently a window of opportunity for clinicians to intervene with psychosocial support in conjunction with the Chinese government's ongoing efforts. Increasing numbers of individuals are seeking testing and initiating ART at local infectious disease clinics; this population is both accessible to researchers and amenable to behavioral intervention.
Of the individuals seeking testing and initiating ART, many are fathers who are married to women but who also identify as men who have sex with men (MSM; Guo, Li, & Stanton, 2011). Same-sex sexual behaviors have a compounding effect on the stigma related to HIV and complicate the issue of parental HIV disclosure in traditionally close-knit Chinese families (Yang et al., 2015). A primary concern for HIV-infected parents all over the world is the issue of making a decision about whether to, when to, and how to disclose their HIV status to their children (Simoni et al., 2015). In China in particular, parents face many culturally specific barriers to disclosure, and these include a child's maturity, mental burden of the diagnosis, stigma, and isolation (Kyaddondo, Wanyenze, Kinsman, & Hardon, 2013; Yang et al., 2015). In addition, HIV-infected parents are concerned about critical moments in their children's life stages (e.g., preparing for college entrance exams, finding a life partner, having a baby), and often desire to wait for the best time to disclose their serostatus.
Background
Globally, HIV-infected parents face similar difficulties when they consider whether to disclose their status to their children. For example, in Uganda, HIV-infected parents are afraid of discrimination from the community, and experience shame and guilt related to unprotected intercourse and loss of societal privileges (Kyaddondo et al., 2013). However, without disclosure, they also lose access to the health care system, societal resources, and potential treatment because they did not express their need for HIV care (Kyaddondo et al., 2013). In the United States, HIV-infected mothers not only worry about their children's situations but also about their own conditions. These women are stressed about the role of mother, which is especially true for women who have weaker attachment with their children (Murphy, Marelich, Armistead, Herbeck, & Payne, 2010). In addition, HIV-infected mothers also tend to be faced with low social economic status, high perceived stigma, and high risk behavior. In particular, mothers with younger children worry about the developmental maturity of their children and whether the children can keep the secret inside the family if disclosure were to occur (Murphy et al., 2010). The majority of HIV-infected parents in the United States (around 60%) have not revealed their serostatus to their children (Murphy et al., 2010). The only study to report rates in China indicated that 77% of Chinese parents had not revealed their serostatus to their children (Zhou, Zhang, Li, & Kaljee, 2013).
In fact, the majority of disclosure studies on HIV-infected parents have been conducted in the United States, with little specific information about either mothers or fathers in low-resource settings (Qiao, Li, & Stanton, 2013). The limited research that has been done on parental disclosure in China has indicated that the majority of HIV-infected parents were reluctant to disclose their serostatus (Qiao et al., 2013). Currently, the literature is inconclusive about the impact of disclosure versus non-disclosure globally (Gachanja & Burkholder, 2016; Yang et al., 2015). Some studies reported positive outcomes of disclosure, such as enhanced family support, improved maternal quality of life, increased ART adherence, effective household functioning, and enhanced child mental stability (Murphy, Armistead, Marelich, Payne, & Herbeck, 2011; Murphy, Roberts, & Herbeck, 2013). Other studies have demonstrated no psychological impact following disclosure (Simoni, Davis, Drossman, & Weinberg, 2000). Still other reports have shown detrimental emotional effects of disclosure, such as decreased parental self-esteem and mental distress (Yang et al., 2016), as well as increased externalizing behaviors in adolescent children, including use of cigarettes, alcohol, marijuana, and harder drugs (e.g., stimulants, inhalants, hormones, crack, heroin; Li et al., 2009). Documented factors affecting these outcomes included the age of the child who was informed about parental HIV, whether other children in the family were also informed (and when), how the disclosure event went, and parental demands for secrecy (Murphy et al., 2010). Other potential influencing factors included maturity of the children, perceived stigma of the HIV-infected parents, and the atmosphere in the family (Qiao et al., 2013). Non-disclosure has also been associated with negative outcomes, such as increased anxiety in children and lack of support for HIV-infected parents (Murphy et al., 2011). They also suggested that anxiety might be due to children sensing something was wrong in the family but feeling unable to ask about matters they believed they are not supposed to know about. When HIV-infected parents create a wall of silence in the family in an effort to protect children, unintended negative consequences may occur, such as decreased family dialogue and interactions (Ishikawa, Pridmore, Carr-Hill, & Chaimuangdee, 2010).
The intention of keeping HIV infection a secret is often to protect HIV-affected children from depression, discrimination, bullying, and potential embarrassment; however, an unintended side effect may be inadvertently distancing these HIV-affected children from professional helpers such as teachers, health care providers, and/or social workers (Ishikawa et al., 2010).
We conducted a pilot randomized controlled trial (RCT) of an intervention for parental HIV disclosure support, to assist parents in China through the disclosure decision-making process (Simoni et al., 2015). During this RCT, detailed progress notes were kept from each intervention session, which detailed parental concerns related to disclosure. These progress notes contained rich qualitative data describing the parents' decision-making process, concerns, and stressors. This data provided insight into HIV-infected parents' individual thought processes and allowed for better understanding and tailoring of future interventions.
Method
Aim
We aimed to understand parents' concerns regarding HIV disclosure to children that were raised while the parents underwent a disclosure support intervention.
Design
Data were collected from December 2013 through April 2015 in Shanghai, China as part of a larger RCT. For the RCT, participant inclusion criteria were: (a) HIV-infected parent of an HIV-uninfected child (ages 13–25 years) who did not know about the parent's infection, (b) receiving clinical care at the Shanghai Public Health Clinical Center (SPHCC), (c) physically well enough to attend study sessions at the clinic, and (d) without psychological or cognitive impairment (as informally assessed by medical providers) that would prevent participation.
The U.S.-based team included researchers experienced in clinical psychology, social work, and nursing and provided a week-long training for nurse interventionists and local study staff at SPHCC. During the training, research ethics, interview skills, data collection techniques, intervention protocols, and study procedures were delivered and discussed. Quality assurance checks were conducted with pilot participants to ensure that interventionists were adhering to the manualized protocol. The interventionists were supervised by the U.S.-based research team during the audio-recorded sessions to ensure fidelity of the intervention delivered.
Study staff met with study candidates to explain research procedures, answer issues related to the project, and obtain written consent. The 20 enrolled HIV-infected parents were randomly assigned to either the disclosure-support counseling intervention or the treatment-as-usual group. Ten HIV-infected parents assigned to the intervention group attended a weekly three-session nursing counseling intervention over the course of 3–4 weeks, with a follow-up assessment at 3 months.
For our study, progress notes of each intervention session for participants randomly assigned to the intervention condition (n = 10) were used as data for content analysis. During intervention sessions, study participants shared concerns regarding disclosure to their children as well as their previous experiences of disclosure without preparation, which was documented thoroughly by the nurse interventionist in progress notes. Sessions were also audio-recorded with participant consent. We explored the nurse interventionist notes using content analysis (Denis, 2014; Price et al., 2014), which focused on the experiences of a small number of participants rather than those of a larger group, with the goal of giving voice to those whose stories had not been heard in published literature. Specifically, we explored themes related to the sharing of sensitive personal information within families in China, a setting of low mental-health resources and high HIV-related stigma (Li et al., 2009). We also explored the concerns affecting parental decisions about serostatus disclosure (Yang et al., 2015; Yang et al., 2016).
Ethical Considerations
Our study was approved by the University of Washington, Yale University, and SPHCC Human Subjects Review Boards. Any identifiable information obtained in the study will remain confidential. When the results of the research have been published or discussed in conferences, no information has been included that would reveal the participants' identities. The research staff also disclosed to study participants that they were free to choose not to participate and were free to withdraw from the study at any time during its course without penalty. We began data collection after securing written consent from the participants.
Intervention
The intervention included three components: (a) assessment; (b) decision-making and support; and (c) disclosure, planning, and action. The individualized assessment comprehensively considered the family's history, experiences with disclosure, communication skills, coping resources, and factors likely to affect disclosure (e.g., familial, psychological, social, cultural, and medical issues). The second component of decision-making and support focused on developing communication skills and strategies, with role-play and practice outside of the sessions as necessary. Costs and benefits of disclosure were considered along with the range of disclosure options (see Table 2). Several materials, including a pros and cons chart of disclosure and a disclosure continuum worksheet, were used to stimulate discussions of possible plans and consequences. In the third component, parents were encouraged to formulate and practice a disclosure plan for later use.
Table 2.
Impact of Intervention on Disclosure
| Family types | Disclosure continuum plan |
N | |
|---|---|---|---|
| Before first intervention session | After third intervention session | ||
| Harmonious family (Good family relationships) | Partial disclosure | Key disclosure | 3 |
| Partial disclosure | Indirect disclosure | 1 | |
| Indirect disclosure | Key disclosure | 3 | |
| Single-parent family | Vague disclosure | Key disclosure | 1 |
| Partial disclosure | Key disclosure | 1 | |
| Indifferent family (Disconnected family relationships) | Vague disclosure | Partial disclosure | 1 |
Intervention contents:
First intervention. The study participant shared his/her experiences of when and how s/he knew about his/her HIV diagnosis and to whom s/he had disclosed. The nurse interventionist briefly discussed the target child's situation, including the child's age, developmental stage, and his/her personality. Then, the interventionist and the parent discussed the pros and cons of disclosure to the child. During this session, the interventionist provided psychoeducation to enhance parent-child communication and assigned use of appropriate communication strategies as homework.
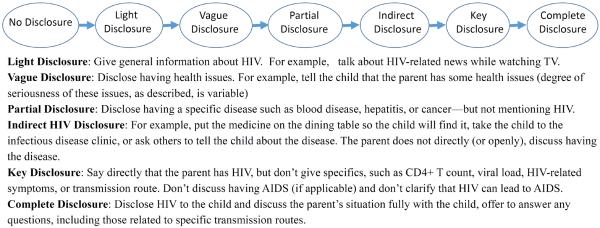
Second intervention. The interventionist engaged the parent in a collaborative discussion about the potential reactions of their children during the disclosure process. The research team created a handout of developmentally appropriate and typical communication abilities and reactions of children ranging from 13-to-25 years of age for parents to feel more prepared about what to anticipate. Parents were asked to share how the child reacted in previous major events inside the family. In addition, the interventionist taught the parent about a disclosure continuum that ranged from no disclosure to complete and open disclosure with behaviorally specific descriptions of stages in between. For homework, the parent was asked to think about where s/he would like to be on the continuum in the near and later future.
Third intervention. In the last session, the interventionist assisted the parent to come up with a plan to achieve the desired stage on the continuum. Parents role-played the disclosure event with the interventionist, including answering potential questions from their children and anticipating possible reactions. The interventionist helped the parents troubleshoot potential barriers to taking steps toward where they wanted to be on the continuum, and on completion of the intervention parents were encouraged to enact the plan discussed.
Nurse interventionists wrote progress notes after each intervention session to understand the HIV-infected parents' opinions/feelings of the disclosure decision as they discussed what might happen after disclosure. At that time, parents were also encouraged to talk about their stigma experiences and changes in parent-child relationships before and after being diagnosed with HIV. Sample questions included: What were your concerns as a parent before receiving an HIV diagnosis and how did they change after receiving your HIV diagnosis?, “How do stressors affect your sleep?, and What were your relationships like with your child(ren) and spouse/partner before receiving an HIV diagnosis and how did they change after receiving your diagnosis? The nurse interventionist also asked participants whether they had ever thought about revealing their serostatus to their children and about their thought processes related to the issue. The HIV-infected parents largely led the conversations, with the nurse interventionist prompting the discussion when needed. The parents were informed that the success of their contributions was not based on whether they chose to disclose their HIV status but rather on their having carefully considered their disclosure options in order to make an informed decision.
Each counseling session took from 1 to 2 hours and was conducted in a private hospital room by a nurse interventionist. Three trained nurse interventionists conducted the intervention. After each counseling session, the nurse interventionist wrote detailed progress notes to reflect the content of the counseling session. Progress notes were compiled based on handwritten notes taken during the session, in conjunction with reviewing the session tapes. Additional procedures for this intervention study have been described in greater detail by Simoni et al. (2015).
Data Analysis
A data analysis team, including several bilingual researchers proficient in content analysis, conducted the data analysis. The team included one China-based clinician who was involved in recruiting participants and one U.S.-based nurse scientist who had worked with the HIV-infected Chinese population for more than 10 years and had extensive experience with qualitative research. Qualitative content analysis was conducted using an Excel spreadsheet to help researchers code and analyze the data.
For each participant, the notes from the three sessions were analyzed in order. Then, data were read word by word to derive codes, First, the exact words from the text that appeared to capture key thoughts or concepts were highlighted (Hsieh & Shannon, 2005). Next, the team approached the text by making notes of first impressions, thoughts, and initial analysis, with coding schema managed via Excel spreadsheets. After initially coding the data into broad categories by topic, we generated reports for each topic and included key quotations from participants to understand the range of responses. As this process continued, labels for codes emerged that were reflective of more than one key thought. Finally, we grouped relevant quotations under each theme. The authors worked on the coding assignments separately and discussed the coding to resolve any disagreements in the understanding and meaning of patterns observed in series of meetings. These often came directly from the text and then became the initial coding scheme (Hsieh & Shannon, 2005). The investigators later assigned codes and organized general patterns observed into themes based on how descriptive codes were related and linked. In the last step, quotations were picked from the progress notes and translated into English for publication.
Rigor and Trustworthiness
In our project, trustworthiness of the findings was evaluated throughout the intervention process. Interpretations of progress notes were validated with a subset of participants to confirm the interpretation of the data via triangulation (Sandelowski, 2008). Credibility was established through the triangulation process. Each data analysis team member independently generated two new progress notes from the randomly selected audio recording and compared them to the initially written corresponding progress notes to ensure the accuracy of the notes. Also, we continually consulted with our Chinese colleagues who worked with this population regarding our interpretations of the data to assure that the findings reflected their extensive experiences with HIV-affected parents. To assure dependability, we strictly followed the interview schedule so that all the participants were assessed in the same time frame (Graneheim & Lundman, 2004).
Findings
The average age of the participants was 45.8 ± 4.67 years of age. Seven fathers and three mothers participated in the intervention (see Table 1). Eight participants reported that they had likely acquired HIV through sexual transmission (of whom 7 were MSM), and two reported that they had become infected through blood transfusions. Seven of the participants reported harmonious relationships with all members of the family, two were single-parent families, and one participant reported having disconnected family relationships, in which the couple did not communicate but were still married. Table 2 details the associations between strength of family relationships and degree of disclosure, demonstrating that if the family's bond was not strong and the relationship between children and parents was not close, the degree of disclosure was minimal and the process was slow. Also, parents who had two or more children were more likely not to disclose to the younger child compared to the older child.
Table 1.
Demographic Data
| Sample (n = 10) | |
|---|---|
| M (SD) or % | |
| Age (years) | 40–55 (45.8) |
|
| |
| Gender (female) | 3 (30) |
|
| |
| Number of children | |
|
| |
| 1 | 8 (80%) |
|
| |
| 2 | 2 (20%) |
|
| |
| Gender of the target child for disclosure | |
|
| |
| Female | 1 (10%) |
|
| |
| Male | 9 (90%) |
|
| |
| Employment/Occupation | |
|
| |
| Unemployed | 4 (40%) |
|
| |
| Currently working | 6 (60%) |
|
| |
| Income* | |
|
| |
| Below Average | 8 (80%) |
|
| |
| Above Average | 2 (20%) |
|
| |
| Marital Status | |
|
| |
| Married | 8 (80%) |
|
| |
| Sexual orientation | |
|
| |
| MSM/Bisexual | 7 (70%) |
|
| |
| Heterosexual | 3 (30%) |
Note. SD = standard deviation; MSM = men who have sex with men.
Average income in Shanghai is approximately equal to $666 USD/month (¥ 4,000RMB).
Emergent Themes
The primary themes that emerged from counseling sessions were (a) severe stigma experienced by fathers who were sexually active with men, (b) need for both parents to agree on plans for disclosure, and (c) parents' fears about the consequences of disclosure.
Severe stigma of fathers who were sexually active with men. Fathers in our sample reported wanting to be good parents and role models in their children's lives. In their efforts to accomplish this, several fathers changed the details about how they acquired HIV during the disclosure process, sometimes using it as an opportunity to educate the children about the risk of HIV. A 40-year-old married male participant with a 16-year-old son had planned to disclose his HIV status to the son, but only after the son had passed his college entrance exam. Upon going through the intervention, he decided to disclose earlier, after the family's upcoming summer vacation. However, he said that the real transmission route would be kept a secret. “I will tell my son that I got the disease from prostitution, not from homosexual activity,” he said. The participant believed that by disclosing in this way, he would cause his son to pay more attention to his own sexual activities and be more careful about his relationships.
Fathers who acquired HIV via having sex with men reported worrying more about revealing their sexual behavior and their identities as gay/bisexual men than about revealing their status as HIV-infected individuals. Many participants reported that their major dilemma in considering parental disclosure was that their child would likely ask about the transmission route and they would be at a loss for what to say. One 41-year-old divorced father with a 15-year-old daughter reported, “Even if I disclose my HIV status to my daughter, the transmission route will not be included.”
Need for both parents to agree on plans for disclosure. In this study, three participants had spouses who were also HIV-infected and who shared their concerns regarding disclosure. One 44-year-old mother with two children described her and her husband's experience with the painful process of disclosure. The couple had a 16-year-old daughter and an 8-year-old son. About 2 years prior to the study, after the mother became very sick, the father decided to disclose, without consulting his wife, to the daughter but not the son. After the disclosure, they observed that their daughter did not interact with her younger brother as much as she had before. In addition, she decided not to get married and planned instead to work at a funeral home. The couple regretted that they had not discussed when and how to disclose before the disclosure event, as they interpreted the daughter's “abnormal” career choice and withdrawn behavior as resulting in part from the disclosure event. The mother was hoping that during the study intervention, the couple could learn how to disclose in a more deliberate way, so they would have a better outcome for their son.
In another case, a 43-year-old HIV-infected mother had a 22-year-old son and wanted to disclose her status to him. However, the child's father insisted that disclosure would make their son afraid to talk to his mother; therefore, she deferred disclosing. After three intervention sessions, the mother shared,
My husband and I agree that we will disclose either when my son is married or has a child. Or if I become very sick and hospitalized, we will disclose to him. I will be the one who will do the initial disclosure and my husband will support him along the process.
Another mother shared, “My husband and I agreed not to disclose. We don't know what the benefits of disclosure are.” Many of our participants shared that if the parents agreed to disclose, they needed to disclose together, and be united in the decision to disclose.
Parents' fears about the consequences of disclosure. Parents may worry and feel particularly helpless when they need to reveal serostatus due to emergency conditions, such as developing HIV-related complications or being admitted to a hospital. One 45-year-old married father with a 15-year-old son worried that his child might not able to accept that his parent was sick and as a result decided not to disclose at all at the end of three intervention sessions. This decision was made after careful consideration of all relevant pros and cons. In the end, the father believed that the risks involved in disclosure were greater than the benefits. In addition, the parents wanted to preserve the family's “harmonious” dynamics for a while longer. They were afraid that a disclosure would destroy that harmony.
A 49-year-old married father with a 14-year-old son had a hard time initially identifying any benefit to disclosure. He initially believed that not disclosing his own status was protecting his son from bad news. However, as a result of the intervention, he was beginning to come to terms with the necessity of disclosing to his son eventually. He said,
I am worried that as I get older I will develop chronic diseases. Once I get sick, my son will figure it out for himself eventually anyway. Then, he might not be able to accept that I have this [disease]. Then he will be very upset and will not want to get married.
Discussion
Whether or not to disclose a parental HIV serostatus is a difficult choice. Parents generally want to protect their children from any possible harm. At the same time, parents may also need to obtain support from their children. As a result, deciding whether to, how to, and when to disclose becomes one of the hardest tasks for HIV-infected parents. When parents hesitate to disclose their serostatus, it is often because they worry there will be adverse effects for the child, (e.g., discrimination, exposing transmission route, child refusal, social isolation for the family), and especially that it might be disappointing and cause psychological stress (Yang et al., 2015). Indeed, some research has suggested that, at least initially, children may be shocked; however, many children also have become treatment supporters after the initial period of shock (Tiendrebeogo et al., 2013; Zhou et al., 2013).
In a Chinese cultural context, disclosure is further complicated by familial role expectations. For example, the oldest child is expected to support the family if the father is disabled, introducing additional implications of parental HIV disclosure (Laidlaw, Wang, Coelho, & Power, 2010). S/he then will take care of the younger siblings (for example, by cooking for the family and taking younger siblings to school). In our study, we encountered an example of the negative impact on the older child, her life expectations, and the sibling relationship as a result of a disclosure without careful preparation. Parents described that when the older sister was told about the parents' serostatus, she was asked to become the caregiver to her younger brother, so there would be a smoother transition in case her parents should become disabled. From this, she concluded that her parents wanted her to drop her previous role of sibling. Accordingly, she stopped all enjoyable interactions with her brother.
Few studies have discussed the process of how and when parents with HIV disclose their serostatus to their children (Kennedy et al., 2010). In our limited sample, many of the two-parent families agreed to and supported the disclosure process. These two-parent families tended to discuss and agree on when and how to disclose. Furthermore, the participants were more willing to disclose when they had good relations with their children (Liamputtong, Haritavorn, & Kiatying-Angsulee, 2012). Harmonious families provided strong support to their members, and the more support HIV-infected parents received, the more willing they were to discuss their serostatus to their children (see Table 2; Zhou et al., 2013).
Discrimination against MSM in China causes many fathers to conceal their same-sex sexual behaviors (Guo et al., 2011). In Shanghai, where the study was conducted, many fathers acquired HIV via having sex with men, reflecting transmission trends in urban areas of China (Zhang et al., 2015). Transmission route and sexual orientation were identified by our participants as barriers to disclosure to any family member, including a child. These factors were therefore discussed during the intervention as well as how to respond to related inquiries during the disclosure process. After the intervention, several fathers stated that they had decided to disclose their serostatus to their families at some point in the future. In particular, one of them decided to disclose within the 2 months following a family vacation. Others said they would look for the right time to broach the topic, for example, after the child got into college, started his or her first career, or even much later, after the child had decided to start his/her own family. However, the real transmission route would not be disclosed under any of these scenarios. Some parents said they would not necessarily disclose details but would give hints as to where they got the disease.
HIV-infected parents are constantly weighing the risks and benefits of disclosure. When there is no obvious and immediate benefit, such as improving the parent-child relationship, parents are likely to put off disclosing their status (Simoni et al., 2015). At the same time, parents know that it might ultimately cause more harm if they wait to disclose until they are very ill (Van Tam et al., 2012). It is, therefore, important for parents to prepare for disclosure in advance. Not only can this ease their anxiety, it can also reduce stress if a need to disclose arises suddenly and unexpectedly.
In the review of the global HIV disclosure literature, some studies have emphasized how the meaning and process of disclosure differs considerably across settings (Obermeyer, Baijal, & Pegurri, 2011). Some HIV-infected individuals might weigh the risks and benefits of disclosure (Shushtari, Sajjadi, Forouzan, Salimi, & Dejman, 2014). Most often, they will keep their HIV status a secret for as long as possible (Zhou et al., 2013) in the absence of professional intervention or other assistance with disclosure (Maiorana et al., 2012). Therefore, innovative work on best practices for disclosure in the context of Chinese culture where HIV stigma is pervasive is urgently needed (Zhou et al., 2013). The limited relevant research conducted in China demonstrated that revealing an HIV diagnosis to family members was a difficult issue and the source of significant emotional suffering for HIV-infected individuals (Li et al., 2009). At the same time, several studies have shown that disclosing HIV status to offspring reinforced parent-child relationships and enhanced health care assistance, strengthening the parent's will to live (Li et al., 2009).
A study in China demonstrated that children who had been told of their parents' serostatus did present with mental and social difficulties; however, continued support from the HIV-infected parents and additional support from extended family members (e.g., grandparents or other relatives) could improve the children's school grades and life quality (Xu, Wu, Rou, Duan, & Wang, 2010). There is an urgent need for practical interventions to assist parents throughout the decision-making process of HIV disclosure, particularly interventions that occur in the Chinese cultural context, where customs often treat the family as one unit. These cultural norms highlight the need for family-based interventions (Yoshioka & Schustack, 2001), which have been shown to be practical and successful for families affected by chronic diseases (Li et al., 2011).
Parents' ideas about HIV disclosure, couples' relationships, communication pathways with children, and openness of the family are all factors bearing on the disclosure decision (Murphy et al., 2011). In China, parental sexual orientation and acquisition of HIV via same-sex behaviors greatly affects decision-making about disclosure. Therefore, improving health care providers' awareness of their own attitudes toward same-sex behaviors may be beneficial. Many studies have been devoted to decreasing Chinese health care workers' stigmatization of people with same-sex sexual behaviors (Li et al., 2011). Decreased stigma by providers can function as a first step to decreasing stigma in health care environments generally.
Lessons Learned
Findings from our participants' stories and our qualitative data analysis suggest several points that may be helpful to consider in the disclosure decision-making process. First, while all parents had difficulty with disclosure, fathers who were MSM were especially reluctant to disclose due to the potential for exposure of the transmission route. Second, participants asserted that an agreement between the parents was important for a disclosure decision. Third, parents expressed a great deal of fear regarding consequences of disclosure. In addition, demographic characteristics of the HIV-infected parents (e.g., father or mother and MSM status) may indicate unique concerns to be addressed during the intervention.
In Figure 1, we list seven disclosure continuum points based on participant reporting and post-session outcomes for three types of family structures. Participants reported that, for HIV-infected parents, the following were helpful in the disclosure process: seeking professional help, establishing a close relationship with the child, understanding the disclosure continuum, staying calm, expecting changes after disclosure, and being aware that unintentional disclosure may do harm. In addition, it can be helpful to anticipate the possibility that children may be hurt by the news that a parent is HIV infected and their ability to communicate with others, inside or outside the family, can be severely impacted. Presenting disclosure stages to parents as a continuum can be helpful for their understanding of options for disclosure. Additionally, providers can assist parents to anticipate their children's responses and questions following disclosure.
Figure 1.
Seven disclosure stages.
Limitations
There were several limitations to this study. First, the study was conducted in Shanghai, a major metropolitan area where HIV-infected parents may have experiences with HIV disclosure that are less generalizable to rural or less urban populations. Therefore, a replication study conducted in other areas of China may be helpful. Second, there were more HIV-infected fathers in this study than mothers, who may have had different experiences based on their gender and parental roles. Finally, because the study design did not dyad pair fathers, mothers, sons, and daughters for randomization, the results may be variable for different pairings, which we were not powered to examine.
Conclusions
In China, PLWH are severely stigmatized; thus, there is a need for family members to provide mutual support, respect, and assistance. HIV-infected parents have special concerns about disclosing to their children in order to gain that support. We analyzed progress notes of a disclosure-support intervention, generating three primary themes from HIV-infected parents' disclosure decision-making processes. Taken together, findings from our study suggest that HIV-infected parents can benefit from professional nurse-delivered interventions during the parental HIV disclosure decision-making process to support their thought processes about how and when to disclose.
Key Considerations.
A primary concern for HIV-infected parents all over the world is the issue of making a decision about whether to, when to, and how to disclose their HIV status to their children.
Chinese HIV-infected parents worry about stigma and discrimination for themselves and their children, rejection from their children, confidentiality, and additional consequences for their children such as psychological distress.
There is an urgent need for practical interventions to assist parents through the decision-making process of their HIV disclosure, particularly interventions that account for the cultural context in China, where customs often highlight family as one unit.
HIV-infected parents can benefit from professional nurse-delivered interventions during the parental HIV disclosure decision-making process to support thought processes about how and when to disclose.
Acknowledgements
We gratefully acknowledge all study participants, without them it would not have been possible to complete this project. Also, we thank the Community Advisory Board, Beautiful Life, research assistants at the Fudan University School of Nursing, and the clinic staff at Shanghai Public Health Clinical Center, specifically Chengen Pan, Mingfong Shi, and Yan Lu for their support and help with this project. Research reported in this publication was supported by the NICHD, NINR and NIMH of the NIH, under Award Numbers [R21HD074141], [K23NR14107], [F31MH099925], [K24MH093243].
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest Statement Lin Zhang, Wei-Ti Chen, Joyce P. Yang, Jane M. Simoni, Chengshi Shiu, Meijuan Bao, Jing Zhang, Meiyan Sun, Yang Qiu and Hongzhou Lu report no financial interests or potential conflicts of interest.
References
- Denis P. New patterns of disclosure: How HIV-positive support group members from KwaZulu-Natal speak of their status in oral narratives. Medical History. 2014;58(2):278–297. doi: 10.1017/mdh.2014.23. doi:10.1017/mdh.2014.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gachanja G, Burkholder GJ. A model for HIV disclosure of a parent's and/or a child's illness. PeerJ. 2016;4:e1662. doi: 10.7717/peerj.1662. doi:10.7717/peerj.1662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Graneheim UH, Lundman B. Qualitative content analysis in nursing research: Concepts, procedures and measures to achieve trustworthiness. Nurse Education Today. 2004;24(2):105–112. doi: 10.1016/j.nedt.2003.10.001. doi:10.1016/j.nedt.2003.10.001. [DOI] [PubMed] [Google Scholar]
- Guo Y, Li X, Stanton B. HIV-related behavioral studies of men who have sex with men in China: A systematic review and recommendations for future research. AIDS and Behavior. 2011;15(3):521–534. doi: 10.1007/s10461-010-9808-7. doi:10.1007/s10461-010-9808-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qualitative Health Research. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. doi:10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- Ishikawa N, Pridmore P, Carr-Hill R, Chaimuangdee K. Breaking down the wall of silence around children affected by AIDS in Thailand to support their psychosocial health. AIDS Care. 2010;22(3):308–313. doi: 10.1080/09540120903193732. doi:10.1080/09540120903193732. [DOI] [PubMed] [Google Scholar]
- Kennedy DP, Cowgill BO, Bogart LM, Corona R, Ryan GW, Murphy DA, Schuster MA. Parents' disclosure of their HIV infection to their children in the context of the family. AIDS and Behavior. 2010;14(5):1095–1105. doi: 10.1007/s10461-010-9715-y. doi:10.1007/s10461-010-9715-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kyaddondo D, Wanyenze RK, Kinsman J, Hardon A. Disclosure of HIV status between parents and children in Uganda in the context of greater access to treatment. Journal of Social Aspects of HIV/AIDS Research Alliance (SAHARA J) 2013;10(Suppl. 1):S37–S45. doi: 10.1080/02664763.2012.755323. doi:10.1080/02664763.2012.755323. [DOI] [PubMed] [Google Scholar]
- Laidlaw K, Wang D, Coelho C, Power M. Attitudes to ageing and expectations for filial piety across Chinese and British cultures: A pilot exploratory evaluation. Aging & Mental Health. 2010;14(3):283–292. doi: 10.1080/13607860903483060. doi:10.1080/13607860903483060. [DOI] [PubMed] [Google Scholar]
- Li L, Lin C, Ji G, Sun S, Rotheram-Borus MJ, Ji G. Parents living with HIV in China: Family functioning and quality of life. Journal of Child Family Studies. 2009;18(1):93–101. doi: 10.1007/s10826-008-9210-5. doi:10.1007/s10826-008-9210-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li X, Huang L, Wang H, Fennie KP, He G, Williams AB. Stigma mediates the relationship between self-efficacy, medication adherence, and quality of life among people living with HIV/AIDS in China. AIDS Patient Care and STDs. 2011;25(11):665–671. doi: 10.1089/apc.2011.0174. doi:10.1089/apc.2011.0174. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liamputtong P, Haritavorn N, Kiatying-Angsulee N. Living positively: The experiences of Thai women living with HIV/AIDS in central Thailand. Qualitative Health Research. 2012;22(4):441–451. doi: 10.1177/1049732311421680. doi:10.1177/1049732311421680. [DOI] [PubMed] [Google Scholar]
- Maiorana A, Koester KA, Myers JJ, Lloyd KC, Shade SB, Dawson-Rose C, Morin SF. Helping patients talk about HIV: Inclusion of messages on disclosure in prevention with positives interventions in clinical settings. AIDS Education and Prevention. 2012;24(2):179–192. doi: 10.1521/aeap.2012.24.2.179. doi:10.1521/aeap.2012.24.2.179. [DOI] [PubMed] [Google Scholar]
- Ministry of Health People's Republic of China Joint United Nations Programme on HIV/AIDS World Health Organization . 2005 Updates on the HIV/AIDS epidemic and response in China. Beijing: 2006. Retrieved from http://data.unaids.org/publications/external-documents/rp_2005chinaestimation_25jan06_en.pdf. [Google Scholar]
- Ministry of Health People's Republic of China Joint United Nations Programme on HIV/AIDS World Health Organization 2014 China AIDS Response Progress Report. 2015 Retrieved from http://www.unaids.org.cn/en/index/topic.asp?id=1030&classname=Statements%20and%20Updates&class=2.
- Murphy DA, Armistead L, Marelich WD, Payne DL, Herbeck DM. Pilot trial of a disclosure intervention for HIV+ mothers: The TRACK program. Journal of Consulting and Clinical Psychology. 2011;79(2):203–214. doi: 10.1037/a0022896. doi:10.1037/a0022896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy DA, Marelich WD, Armistead L, Herbeck DM, Payne DL. Anxiety/stress among mothers living with HIV: Effects on parenting skills and child outcomes. AIDS Care. 2010;22(12):1449–1458. doi: 10.1080/09540121.2010.487085. doi:10.1080/09540121.2010.487085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy DA, Roberts KJ, Herbeck DM. Adolescent response to having an HIV-infected mother. AIDS Care. 2013;25(6):715–20. doi: 10.1080/09540121.2013.769495. doi:10.1080/09540121.2013.769495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Obermeyer CM, Baijal P, Pegurri E. Facilitating HIV disclosure across diverse settings: A review. American Journal of Public Health. 2011;101(6):1011–1023. doi: 10.2105/AJPH.2010.300102. doi:10.2105/AJPH.2010.300102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Price JE, Phiri L, Mulenga D, Hewett PC, Topp SM, Shiliya N, Hatzold K. Behavior change pathways to voluntary medical male circumcision: Narrative interviews with circumcision clients in Zambia. PLoS One. 2014;9(11):e111602. doi: 10.1371/journal.pone.0111602. doi:10.1371/journal.pone.0111602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qiao S, Li X, Stanton B. Disclosure of parental HIV infection to children: A systematic review of global literature. AIDS and Behavior. 2013;17(1):369–389. doi: 10.1007/s10461-011-0069-x. doi:10.1007/s10461-011-0069-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sandelowski M. Reading, writing and systematic review. Journal of Advanced Nursing. 2008;64(1):104–110. doi: 10.1111/j.1365-2648.2008.04813.x. doi:10.1111/j.1365-2648.2008.04813.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shushtari ZJ, Sajjadi H, Forouzan AS, Salimi Y, Dejman M. Disclosure of HIV status and social support smong people living with HIV. Iran Red Crescent Medical Journal. 2014;16(8):e11856. doi: 10.5812/ircmj.11856. doi:10.5812/ircmj.11856. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simoni JM, Davis ML, Drossman JA, Weinberg BA. Mothers with HIV/AIDS and their children: Disclosure and guardianship issues. Women and Health. 2000;31(1):39–54. doi: 10.1300/J013v31n01_03. doi:10.1300/J013v31n01_03. [DOI] [PubMed] [Google Scholar]
- Simoni JM, Yang JP, Shiu CS, Chen WT, Udell W, Bao M, Lu H. Nurse-delivered counselling intervention for parental HIV disclosure: Results from a pilot randomized controlled trial in China. AIDS. 2015;29(Suppl. 1):S99–S107. doi: 10.1097/QAD.0000000000000664. doi:10.1097/QAD.0000000000000664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tiendrebeogo G, Hejoaka F, Belem EM, Compaore PL, Wolmarans L, Soubeiga A, Ouangraoua N. Parental HIV disclosure in Burkina Faso: Experiences and challenges in the era of HAART. Journal of Social Aspects of HIV/AIDS Research Alliance (SAHARA J) 2013;10(Suppl. 1):S46–S59. doi: 10.1080/02664763.2012.755334. doi:10.1080/02664763.2012.755334. [DOI] [PubMed] [Google Scholar]
- Van Tam V, Larsson M, Pharris A, Diedrichs B, Nguyen HP, Nguyen CT, Thorson A. Peer support and improved quality of life among persons living with HIV on antiretroviral treatment: A randomised controlled trial from north-eastern Vietnam. Health and Quality of Life Outcomes. 2012;10:53. doi: 10.1186/1477-7525-10-53. doi:10.1186/1477-7525-10-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Oragnization, Joint United Nations Programme on HIV/AIDS, & United Nations International Children's Emergency Fund Towards universal access: Scaling up priority HIV/AIDS interventions in the health sector. 2010 Retreived from http://www.who.int/hiv/mediacentre/universal_access_progress_report_en.pdf.
- Xu T, Wu Z, Rou K, Duan S, Wang H. Quality of life of children living in HIV/AIDS-affected families in rural areas in Yunnan, China. AIDS Care. 2010;22(3):390–396. doi: 10.1080/09540120903196883. doi:10.1080/09540120903196883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang JP, Leu J, Simoni JM, Chen WT, Shiu CS, Zhao H. “Please don't make me ask for help”: Implicit social support and mental health in chinese individuals living with HIV. AIDS and Behavior. 2015;19(8):1501–1509. doi: 10.1007/s10461-015-1041-y. doi:10.1007/s10461-015-1041-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang JP, Xie T, Simoni JM, Shiu CS, Chen WT, Zhao H, Lu H. A mixed-methods study supporting a model of chinese parental HIV disclosure. AIDS and Behavior. 2016;20(1):165–173. doi: 10.1007/s10461-015-1070-6. doi:10.1007/s10461-015-1070-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoshioka MR, Schustack A. Disclosure of HIV status: Cultural issues of Asian patients. AIDS Patient Care and STDs. 2001;15(2):77–82. doi: 10.1089/108729101300003672. doi:10.1089/108729101300003672. [DOI] [PubMed] [Google Scholar]
- Zhang F, Sun M, Sun J, Guan L, Wang J, Lu H. The risk factors for suboptimal CD4 recovery in HIV infected population: An observational and retrospective study in Shanghai, China. Bioscience Trends. 2015;9(5):335–341. doi: 10.5582/bst.2015.01107. doi:10.5582/bst.2015.01107. [DOI] [PubMed] [Google Scholar]
- Zhou Y, Zhang L, Li X, Kaljee L. Do Chinese parents with HIV tell their children the truth? A qualitative preliminary study of parental HIV disclosure in China. Child: Care, Health and Development. 2013;39(6):816–824. doi: 10.1111/j.1365-2214.2012.01394.x. doi:10.1111/j.1365-2214.2012.01394.x. [DOI] [PubMed] [Google Scholar]