Abstract
Recognizing and understanding the potentially powerful roles that religiousness and spirituality (RS) may serve in the prevention and amelioration of disease, as well as symptom management and health related quality of life, significantly enhances research and clinical efforts across many areas of behavioral medicine. This article examines the knowledge established to date and suggests advances that remain to be made. We begin with a brief summary of the current knowledge regarding RS as related to three exemplary health conditions: (a) cardiovascular disease; (b) cancer; and, (c) substance abuse. We then focus on particular concerns for future investigations, emphasizing conceptual issues, possible mediators and moderators of relationships or effects, and methodology. Our discussion is framed by a conceptual model that may serve to guide and organize future investigations. This model highlights a number of important issues regarding the study of links between RS and health: (a) RS comprise many diverse constructs, (b) the mechanisms through which RS may influence health outcomes are quite diverse, and (c) a range of different types of health and health relevant outcomes may be influenced by RS. The multidimensional nature of RS and the complexity of related associations with different types of health relevant outcomes present formidable challenges to empirical study in behavioral medicine. These issues are referred to throughout our review and we suggest several solutions to the presented challenges in our summary. We end with a presentation of barriers to be overcome, along with strategies for doing so, and concluding thoughts.
Keywords: Religion, Spirituality, Cardiovascular disease, Cancer, Substance use
Introduction
Approximately 80 % of people worldwide identify with a religious group, and many who do not identify with a particular faith still hold some religious or spiritual beliefs: among the unaffiliated, 7 % of Chinese, 30 % of French, and 68 % of US adults share a belief in God or a higher power (Hackett et al., 2012). About 60 % of American adults regularly report to feel a deep sense of ‘spiritual peace and well-being’ (Pew Research Center, 2014). Nevertheless, social scientists have historically distanced themselves from religious and spiritual matters in the context of clinical research and practice (Delaney et al., 2007). This limited attention may be because academic scientists, on average, are less religious than the general population (Ecklund & Scheitle, 2007) and may therefore be less comfortable with this area of inquiry.
The daunting methodological challenges inherent in this field of study may also deter research. Foremost among these challenges is the question of defining the core constructs (i.e., religiousness and spirituality). Over recent decades, many theorists and researchers have endeavored to develop satisfactory definitions of “religiousness” and “spirituality” (Oman, 2013). In spite of these efforts, the achievement of this goal remains elusive. The history of this issue reveals that defining the terms ‘religiousness’ and ‘spirituality’ (and any distinctions drawn between them) generates disagreement, leading to alternative proposed definitions, in a continuing cycle. Further complicating the matter, as Miller and Thoresen (2003) wisely noted “We suspect that any scientific operational definition of spirituality is likely to differ from what a believer means when speaking of the spiritual” (p. 27). Thus, a discussion of the many competing perspectives regarding unique and overlapping aspects of RS is beyond the scope of this article, but interested readers are urged to consult reviews of efforts to define these constructs (e.g., Oman, 2013; Miller & Thoresen, 2003).
Given that this article provides an overview of the current state of the field, we are limited in our review to the usage of terms chosen by the authors of the original studies. Thus, we have elected to use the term “RS” to allow a broad scope. As a consequence, our review reflects this heterogeneity. In our conceptual model, we make the point that RS comprise many specific components and we suggest that future studies should carefully define the aspects of RS on which they intend to focus. RS collectively represents a constellation of important affective, behavioral, and cognitive variables that may affect the feelings, actions, and thoughts of people in ways that influence important health-related outcomes.
In the context of behavioral medicine, RS have shown possible influences on many important outcomes, including lower mortality (Powell et al., 2003). RS are associated with mental health variables (Koenig, 2012) as well as salutary health behaviors (Benjamins, 2006; Salmoirago-Blotcher et al., 2011) and are linked to a number of improved health and health-relevant outcomes among individuals with a variety of conditions such as cardiovascular disease (Chida et al., 2009), cancer (Laubmeier et al., 2004), and substance abuse (Geppert et al., 2007). Although characterized as “controversial” (Blumenthal et al., 2007; p. 506), peer-reviewed research appears to indicate a magnitude of associations between RS and health outcomes ranging from “small” to “large” (Hwang et al., 2011). These findings have important implications for a better understanding of how RS and health-relevant variables and outcomes may be related.
Recognizing and understanding the powerful role that RS may serve in the prevention and amelioration of disease as well as symptom management will advance many areas of behavioral medicine. This article examines: (a) the knowledge to date; and, (b) what remains to be done. To orient readers who may not be familiar with this research we begin with a brief summary and critical review of the current evidence regarding RS in relation to (a) cardiovascular disease; (b) cancer; and, (c) substance abuse. These conditions represent important health concerns, and the most significant research involving important RS constructs has been conducted in these areas. Those seeking a more comprehensive review of the literature in these and related areas are encouraged to consult the citations on which our review is based as well as sources that provide more comprehensive reviews (e.g., Ellison & Hummer, 2010; Koenig et al., 2001, 2012). We then focus on future investigations, emphasizing conceptual issues, possible mediators and moderators, and methodological challenges. We end with barriers, strategies for overcoming them, and concluding thoughts.
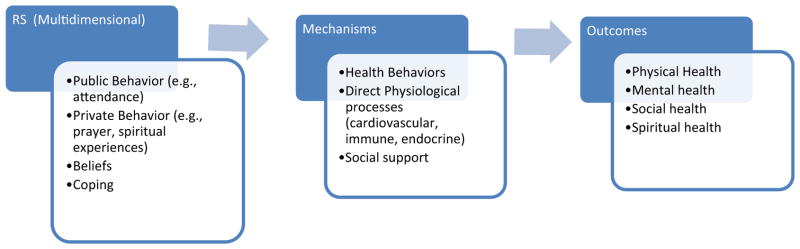
Our discussion is framed by a general conceptual model that may be a useful guide in future efforts to study the complex relationships among RS and health outcomes (Fig. 1). This model is derived from, and similar to, a number of proposed models (e.g., Fitchett & Canada, 2010; Lee & Newberg, 2005; Levin & Vanderpool, 1989; Masters, 2008; Oman & Thoresen, 2005; see Aldwin et al., 2014, for an overview of models). The present model illustrates important issues regarding links between RS and health: (a) RS comprise many diverse and varied constructs, (b) the mechanisms through which RS may influence health-related outcomes are likewise varied, and (c) a range of health-relevant outcomes may be influenced by RS. We note here that we include some of the many dimensions of RS recognized as potentially important in the context of health (Fetzer/NIA, 1999). In some cases, some of these dimensions, such as RS coping, may function as mediators of the effects of other aspects of RS on downstream behavior or health (Aldwin et al., 2014). The multidimensional nature of RS and the complexity of its associations with different types of health endpoints present formidable challenges to empirical study.
Fig. 1.
Illustrations of the potential mechanisms by which religiousness and spirituality (RS) may influence health and health-related outcomes. Note This illustration presents examples of some of the most widely-researched RS dimensions, mechanisms and health-related outcomes rather than attempting to provide exhaustive lists
RS and health research: current findings and critique
RS and cardiovascular disease
Cardiovascular disease (CVD) is the leading cause of death worldwide and accounts for one out of three deaths in the US (Mozaffarian et al., 2016). In the past two decades the importance of psychosocial factors in the pathogenesis, prevention, and treatment of CVD has received increasing attention (Rozanski, 2014), including studies that have extensively investigated physiological changes relevant to CVD and associated with several RS dimensions. These studies documented multiple beneficial effects associated with certain RS dimensions (e.g., private spiritual practices and intrinsic religiosity), such as higher levels of cardiac autonomic control (Berntson et al., 2008) and lower blood pressure reactivity to stressors (Masters et al., 2004). Based on this evidence, we might expect to find a consistent protective association between RS and CVD outcomes at the population level. Instead, the current epidemiological evidence suggests a more complex picture.
Much research examining associations between RS and cardiovascular outcomes has focused on the association between RS and cardiovascular mortality. The evidence from rigorously designed population studies and from a seminal meta-analysis suggested the existence of an independent association between organizational religiosity (i.e., religious service attendance) and CVD mortality (Chida et al., 2009; Hummer et al., 1999; Oman et al., 2002). In addition, adherence to orthodox practices has been associated with reduced cardiovascular mortality and morbidity in Jewish populations (Friedlander et al., 1986; Goldbourt et al., 1993). In both of these studies, associations were independent of important confounding/mediating variables (such as coronary risk factors). Other studies, however, (e.g., Hummer et al., 1999; Oman et al., 2002) did not adjust for important coronary risk factors (i.e., diabetes, hypertension, and dyslipidemia).
More recent studies published after the meta-analysis by Chida et al. (2009) offer a different picture. Two longitudinal analyses conducted in a large cohort of healthy, older women enrolled in the Women’s Health Initiative (WHI) did not find a protective association between religious affiliation, organizational religiosity, religious coping (Schnall et al., 2010) or private religious practice (Salmoirago-Blotcher et al., 2013) and CVD mortality. Similar findings were reported in a prospective cohort study involving 5000 healthy men and women enrolled in the Multi-Ethnic Study of Atherosclerosis (MESA) (Feinstein et al., 2010). In both the WHI and MESA cohorts, point estimates actually showed a higher risk of CVD among the more religiously involved.
Among studies that focused on relations between RS and cardiovascular morbidity (i.e., non-fatal cardiovascular events), Colantonio et al. (1992) did not find significant associations between organizational religiosity and risk of stroke among older non-institutionalized individuals. A prospective study conducted among a select group of myocardial infarction (MI) survivors who were at risk for a second MI due to their high rates of depression and social isolation did not show associations between organizational religiosity, private religious practice, or spiritual experiences and all-cause mortality or risk of recurrent MI (Blumenthal et al., 2007).
Overall, positive associations between RS and CVD were found in studies conducted among younger healthy individuals (Chida et al., 2009; Friedlander et al., 1986; Goldbourt et al., 1993; Hummer et al., 1999; Oman et al., 2002). We note that studies with null or negative findings extensively adjusted for coronary risk factors as well as a wealth of confounding and mediating variables that were not considered or available in earlier studies.
Taken together, the above findings indicate that despite the earlier meta-analytical finding of an independent association between RS and CVD outcomes (Chida et al., 2009), the current evidence linking RS and cardiovascular mortality and morbidity remains inconclusive, and more research is needed examining, for example, whether associations are consistent across different subgroups (healthy vs. unhealthy individuals, age and gender subgroups), and different follow-up durations.
RS and cancer
Cancer is the second leading cause of death in the US, accounting for 23 % of total deaths in 2013 (Centers for Disease Control and Prevention, 2013). After a cancer diagnosis, many patients report that RS are important to their adjustment (Asgeirsdottir et al., 2013). Religious coping is one component of RS that has been studied in cancer patients (see Lavery & O’Hea, 2010; Thune-Boyle et al., 2006 for reviews). Approximately 66 % of cancer patients report using prayer to cope with their illness (Ross et al., 2008) and 84 % of advanced cancer patients report relying on their religious beliefs to cope (Vallurupalli et al., 2012). Positive religious coping (PRC) includes a sense of love, compassion, secure partnership with the divine, and a spiritual connection to others (Pargament et al., 2011). Negative religious coping (NRC), or spiritual struggle, is characterized by spiritual conflicts, a strained relationship with the divine, and doubt in one’s religious beliefs (Pargament et al., 2011).
PRC is much more prevalent than NRC (Hebert et al., 2009) but has shown mixed relationships with various types of psychological well-being in cancer patients (Gall et al., 2011). Many studies suggest that PRC is associated with better emotional, interpersonal, and global functioning (Agarwal et al., 2010; Gall, 2004), better overall quality of life (Tarakeshwar et al., 2006), and greater growth (Urcuyo et al., 2005). However, PRC has also been associated with greater transplant concerns in multiple myeloma patients (Sherman et al., 2009) and more physical symptoms in advanced cancer patients (Tarakeshwar et al., 2006). These findings may reflect a religious coping mobilization effect in which religious resources are specifically accessed in the context of life stress (Cummings & Pargament, 2010).
However, religious coping has also demonstrated a negative relationship with mental health in cancer patients. Though endorsed at far lower rates than PRC, NRC is consistently associated with greater psychological distress, including higher levels of depression and lower levels of life satisfaction and quality of life (Hebert et al., 2009), higher levels of anxiety and poorer physical health (Sherman et al., 2009), and worse mental health (Pérez & Smith, 2015) and adjustment to illness (Exline et al., 2011). These findings highlight the importance of considering the potential for both positive and negative outcomes of religious coping in this population.
Recent meta-analyses of 1341 effects drawn from over 44,000 patients with cancer demonstrated an overall positive relationship between RS and self-reported measures of health outcomes (Park et al., 2015) but the strength of that relationship varied as a function of both the RS dimension and the physical (Jim et al., 2015), mental (Salsman et al., 2015), and social (Sherman et al., 2015) outcomes assessed. The strongest relationships were found between affective dimensions of RS (e.g., sense of meaning, purpose, or connection to a source larger than oneself) and mental health outcomes, whereas behavioral RS constructs (e.g., service attendance, prayer and meditation) showed few significant associations with health, except for a modest positive relationship with social health outcomes. These meta-analyses represent the most comprehensive summary and synthesis of the role of RS for patients and survivors managing the experience of cancer. However, more than 90 % of the studies were cross-sectional and more than 50 % failed to account for relevant covariates or confounds.
Additional research is needed to clarify the nature of relationships between RS and patient well-being (see Schreiber & Brockopp, 2012; Visser et al., 2010 for reviews). Though many studies control for demographic (e.g., Tarakeshwar et al., 2006), disease (e.g., Hebert et al., 2009), and other RS constructs (e.g., Gall et al., 2011), analysis of mediators and moderators will provide a more nuanced understanding of the relationships between RS and outcomes in cancer patients.
Additional research is also needed to advance the understanding of the relationship between RS and disease-related outcomes such as morbidity, mortality, or disease progression and to determine if RS interventions can play a role in changing the trajectory of mental and physical health of cancer patients (Kaplar et al., 2004). In systematic reviews of RS and cancer mortality or progression, there are consistent failures to support the hypotheses that RS slows cancer progression, and inadequate evidence to support the hypothesis that RS protects against cancer mortality (Powell et al., 2003). A review of 18 studies examining the risk for cancer in Christian and non-Christian samples concluded that lifestyle factors explained the reduced risk for cancer associated with a Christian affiliation (Hoff et al., 2008). This finding is consistent with research indicating that RS beliefs and practices are associated with health behaviors associated with reduced cancer risk such as lower levels of smoking and alcohol use (Rew & Wong, 2006), greater use of preventive health services and cancer screening (Benjamins & Brown, 2004), and greater adherence to health behaviors (Park et al., 2008). Such findings suggest that RS may be part of a profile associated with reduced risk for cancer.
RS and substance abuse
Globally, 240 million people suffer from alcohol use disorder, one billion smoke tobacco products, and 15 million inject drugs (Gowing et al., 2015). Substance abuse is a systemic problem, directly affecting the health and well-being of the abusing individuals and their families, and indirectly reaching into society through crime and violence, work absenteeism and unemployment, child abuse and neglect, motor vehicle accidents, and homelessness, all of which impact physical health (Office of National Drug Control Policy, 2000; SAMHSA, 2008). Many theoretical arguments for why RS “should” be related to lower levels of substance abuse have been advanced. A smaller but respectable literature empirically supports the notion that RS provide protection against substance abuse, especially RS beliefs established during childhood (Porche et al., 2015). These studies identify differences in risk for substance abuse and confirm indirect relationships between RS and substance abuse. A few experimental studies even demonstrate a possible causal relationship between RS and changes in substance use (e.g., DeWall et al., 2014).
There is overwhelming consensus that religiosity, particularly attendance and often spirituality, are negatively related to alcohol, tobacco, and illicit substance use across the U.S. and other countries (El Ansari et al., 2014; Hatta, 2010; Hayatbakhsh et al., 2014; Kovaks et al., 2011; Rasic et al., 2011; Wang et al., 2015). Recent comprehensive reviews concluded that RS consistently negatively predicted substance use, possibly due in part to prohibitions against alcohol and other substance use inherent in some religions (Geppert et al., 2007; Kub & Solari-Twadell, 2013; Walton-Moss et al., 2013; Yeung et al., 2009); however, many cited studies did not control for possible confounds such as income or education. Findings were less clear for spirituality (Geppert et al., 2007; Walton-Moss et al., 2013). Very few cited studies found nonsignificant relationships between RS and substance abuse, and none reported a positive relationship, but many were cross-sectional in design, and their definitions and measurements of RS varied widely.
Some of the stronger study designs include twin studies, longitudinal studies, and experimental studies. In twin studies, Kendler and Myers (2009) found that the inverse relationship between religious service attendance and both alcohol and tobacco use became stronger over time; however, Button et al. (2010) showed that religiosity moderated the relationship between genetic factors and alcohol use only in adolescent twins—reduced genetic variance for problem alcohol use with increasing levels of religiosity for both males and females—but religiosity did not moderate alcohol use for either gender in early adulthood. Other longitudinal findings demonstrated that religious coping (Brechting & Giancola, 2007), church attendance (Jessor et al., 2006), high religiosity (White et al., 2006), and high or increasing RS in an inpatient population (Conner et al., 2009) predict lower or decreasing substance use rates.
There is intriguing evidence of a causal relationship between RS and substance use whereby increases in RS predict decreased substance abuse. Perhaps the strongest evidence for effects of RS on substance use includes a series of studies that methodically progressed from cross-sectional through longitudinal to experimental designs (DeWall et al., 2014), in which the amount of prayer in which participants engaged was experimentally increased and predicted both an increase in overall religiosity and a decrease in alcohol use.
In summary, there is strong evidence for an inverse relationship between RS and substance abuse and accumulating evidence for causal effects of RS on substance use and abuse in that increases in RS have predicted reduced substance use in controlled experimental studies. Much research on substance use has separated religiosity and spirituality. Generally, there appears to be less evidence for a protective relationship for spirituality.
Future directions, anticipated barriers, and research recommendations
The findings from cardiovascular disease, cancer, and substance abuse are provocative and suggest a potential benefit of RS on multiple physical health and health-relevant outcomes. However, these data are complex and thus greater understanding is needed in a number of areas. More precise identification and understanding of the mediators through which RS may impact physical health and the conditions under which these relationships may be strengthened or attenuated is needed. Additionally, more methodologically rigorous studies are essential to reduce the potency and frequency of alternative explanations for significant results such as bias, confound, or chance. Studies that include prospective designs as well as experimental (RCT) approaches, strong sampling methods, adequate control for established protective factors, psychometrically robust measures of RS and health outcomes, and appropriate statistical analyses with adequate power for moderator analyses, are needed to advance this field (Rosmarin et al., 2011). Finally, the field would benefit from the use of stronger organizing frameworks or models.
Conceptualizations
Too often, researchers fail to clearly operationalize RS constructs and use RS measures that are confounded with their outcomes of interest or have poor psychometrics. Although a number of conceptualizations of RS have been advanced, surprisingly few studies that use RS variables explicitly use these conceptualizations (Rosmarin et al., 2011). We advocate for more consistency, both across and within studies, careful conceptualization of RS variables, and greater consideration of the theoretical models within which they are embedded.
Initially, researchers tended to conceptualize RS as separate constructs. However, starting in the 2000’s, conceptualization of the domains moved toward seeing R and S as interrelated (Hill et al., 2000). This helped formulate many of the models being tested in research (Aldwin et al., 2014). In adolescent health, Cotton et al. (2006) built on Pargament’s model for adults (Pargament et al., 2001), that separates the distal and proximal aspects of religion. This conceptualization identified that distal “behaviors” (e.g., church attendance) often used to describe the concept of “religion” in research should be separated from the “functions” of religion (e.g., the provision of meaning and peace) that identify the role of “spirituality.” The separation of behavior from function allows researchers to identify individual domains without completely separating the concepts of religion and spirituality (Hill & Pargament, 2008). Conceptualizations of religion developed by health psychology researchers may have implications for links between RS and health. These conceptualizations include concepts of meaning making (Park, 2012), reappraisal (Dezutter et al., 2011), sense of community (LaPierre, 1994), sense of reverence (Ai et al., 2011), and relief of existential distress (Magyar-Russell et al., 2014).
Sophistication in measurement has advanced over the past 20 years, but a concerning trend has emerged. Rather than using a simple single item measure (e.g., service attendance frequency), more studies have moved to using a single survey measure to assess RS, a positive development. However, authors often provide no rationale for their selection of a particular RS measure. In many papers, RS variables are not fully conceptualized, operationalized, or thoroughly integrated in a model of the study, and study outcomes may be related to RS, but RS variables are often not formally integrated into the conceptual framework.
Within the area of RS measurement, progress is occurring. A recent and broadly accepted self-correction occurred with the updating of the domains of a widely used instrument, the FACIT-Sp. This instrument initially conceptualized RS as a two factor model: meaning/peace and faith (Peterman et al., 2002). However, further study of the two factor structure indicated that the meaning/peace component was too closely related to anxiety and that separating this instrument into three domains–meaning, peace, and faith–provides more informative constructs and better psychometric properties (Peterman et al., 2014). In addition to moving away from a two factor model of the FACIT-Sp, care should be taken to avoid using the measure as a predictor of well-being outcomes—a common misuse which confounds predictor and outcome variables (Park et al., 2015).
Mechanisms
Researchers should draw on theory to clearly delineate the processes and mechanisms through which different aspects of RS might influence health. Many pathways have been proposed to explain how religion and spirituality may exert salutary influences on well-being (Clements & Ermakova, 2012; Fitchett & Canada, 2010; Lee & Newberg, 2005; Levin & Vanderpool, 1989; Masters, 2008; Oman & Thoresen, 2005; Park, 2007; see Aldwin et al., 2014, for a review). As Fig. 1 illustrates, these pathways are diverse, and different aspects of RS may affect different aspects of health by influencing the practice of health behaviors, through direct influences on physiological processes, or through the provision of social support.
RS appear to promote a healthier lifestyle. Large-scale epidemiological studies have demonstrated that health behaviors partially mediate the effects of service attendance on physical health, including mortality (e.g., Koenig & Vaillant, 2009). RS have been linked to lower levels of cigarette smoking (e.g., Whooley et al., 2002) and higher levels of preventive health behaviors [e.g., flu shots, cholesterol screening, breast self-exams, mammograms, pap smears, and prostate screening (Benjamins & Brown, 2004)]. Preventive health behaviors have also been linked to RS in many other samples, including a nationally representative sample of Presbyterian women (Benjamins et al., 2006), a large national population of community-dwelling women (Salmoirago-Blotcher et al., 2011), a state-wide representative study of Texas residents (Hill et al., 2007), and a sample of disenfranchised elderly African Americans (Aaron et al., 2003). RS have been related to lower levels of risky health behaviors in diverse samples including inner-city cocaine-using methadone-maintained patients (Avants et al., 2006) and pregnant women in Appalachia (Jesse & Reed, 2006). A nationally representative sample of African Americans showed that different dimensions of RS, including religious beliefs (Debnam et al., 2012a), religious involvement (Holt et al., 2014b), and religious coping (Holt et al., 2014a) were related to health behaviors, including diet, exercise, and smoking.
RS may also influence health through direct influences on important clinical measures and physiological processes (Hill et al., 2014). Some aspects of RS are related to cardiovascular reactivity (Masters et al., 2005), levels of cardiac autonomic control (Berntson et al., 2008), and immune functioning (Ai et al., 2010). These effects may be due to various functions of RS, including induction of relaxation response or a generally calmer demeanor, provision of coping resources when encountering stress (Clements & Ermakova, 2012), or induction of greater positive affect (Park, 2012).
Another important function of RS is the provision of social support. When studies of the service attendance-mortality link control for its influence, relations between attendance and mortality often become substantially weaker (George et al., 2002), indicating that social support mediates at least some of the relationship of RS with health. However, effects of RS-related social support are inconsistent (George et al., 2002), and it appears that although this type of social support is consistently related to mortality, it often functions as an independent predictor rather than as a mediator. Aspects of social support specific to religion appear to be qualitatively different than non-religious social support (Krause, 2008), and may have more potent effects on health (Hayward & Elliott, 2009). In a nationally representative sample of older adults, congregational social support in particular led to a sense of belongingness and satisfaction with one’s health (Krause & Wulff, 2005) and in a national sample of African Americans, religious social support predicted fruit and vegetable consumption, physical activity, and alcohol use over and above general social support (Debnam et al., 2012b).
Moderators
We also advocate attending to potential moderators of the effects of RS on health outcomes. The high levels of within-group variability on health outcomes among individuals with high levels of RS suggests that moderating factors may play critical roles in these linkages, and some research has demonstrated the importance of moderator effects (e.g., Musick et al., 1998; Sternthal et al., 2012). Paying additional attention to moderators will greatly increase the power and meaning of research by identifying characteristics of individuals or groups for whom certain dimensions of RS are particularly potent and those for whom they have much less influence.
Sociodemographics have been shown to be important moderators in RS-health linkages. Not only are specific RS dimensions more prevalent in certain groups, but the associations between RS and health outcomes in these groups may be stronger. RS may be especially related to health among older adults, women, those from specific religious groups, minorities, and those with less education. A study of maternal caregivers of chronically ill children found few relations of religious salience and prayer with quality of life and health symptoms (Banthia et al., 2007). However, taking education and income into account, the relationships became statistically significant, such that prayer was associated with fewer health symptoms and better quality of life among less educated maternal care-givers, and unrelated in those with more education.
Such effects can be complicated. Analyses of a recent nationally representative sample in the US demonstrated moderated mediation such that the mediational pathway of social support linked religious involvement and beneficial health effects only among African Americans (Assari, 2013). New analytic techniques of mediated moderation and moderated mediation (e.g., Muller et al., 2005; Preacher et al., 2007) provide powerful tools for researchers to understand these relationships, but it is critical that researchers consider moderators in order to use these tools. By identifying key moderating variables, research can provide a better understanding of the specific contexts and groups for whom RS is beneficial and under what conditions that benefit occurs, yielding important information for future interventions.
Methodological considerations
The empirical study of RS is inherently difficult, fraught with problematic methodological and even philosophical issues. The discussion above highlighted a major difficulty encountered when attempting to study RS: the conceptualization(s) of RS. Given the difficulty of reaching consensus on this basic concern, it is not surprising that other challenges present at nearly every step in an investigation. Assuming that a reasonable definition for RS can be agreed upon, the problems of how to rigorously measure and operationalize RS as well as disentangle RS from other factors (i.e., culture, socio-economic status, education, personality, family, philosophical and theological views) remain. Further, since it is not possible to randomly assign individuals to particular RS beliefs or views, establishing strong causal inference becomes nearly impossible with particular variables. Finally, as we describe below, some behavioral medicine scholars take the position that even if investigators were successful in overcoming these formidable problems, the practical implications of RS research are extraordinarily limited because it is unethical to use the findings to inform treatment choices or interventions.
Although daunting, these difficulties are neither insurmountable nor unique to RS as they are common in many of the social sciences. The study of personality factors and marital relationships carry many of the same conceptual and methodological obstacles. It is our view that, these difficulties notwithstanding, the study of RS in behavioral medicine has made significant methodological progress. Some of these advances were noted earlier in our discussion of RS research in the areas of cardiovascular disease, cancer, and substance use. Figure 1 also provides a simple yet elegant approach to organizing research in this area. It is now commonly recognized that RS is multidimensional and the associations are unlikely to be the same across different RS dimensions and different dependent variables. Consequently, it makes very little sense to ask whether RS is related to health, and, fortunately, virtually no one conducting research in this area would now ask this question so broadly (though many outside the field continue to conceptualize RS in this unidimensional manner). Of much greater interest to current scientific thinking is the question of “which dimensions of RS are related to which health-relevant outcomes through what theoretical mechanisms for which groups of people?” This level of specificity for the independent, dependent, mediating, and moderating variables represents a significant advance.
Large scale longitudinal investigations have provided some of the most compelling evidence regarding relations among RS constructs and behavioral medicine variables. We encourage more work of this type. However, many of these investigations were conceptualized around other primary variables, and findings regarding RS were ancillary to the major purpose of the investigation. Stronger evidence will accrue when investigators conduct large-scale longitudinal work that features RS variables as the primary constructs of study. Such work, when done systematically, would: (a) carefully consider what covariates to measure to limit confounding, (b) measure at multiple time points, (c) include consideration of possible mediators and moderators, and, (d) include behavioral medicine variables chosen specifically for reasons related to the primary RS questions. This work, grounded in existing or developing theoretical models of dimensions of RS and with careful consideration of relevant dependent variables including particular biomarkers, will best establish the basis for a successfully developing field of investigation.
For many years, RS research, whether cross-sectional or longitudinal, remained strictly observational. How can one randomize or manipulate RS variables? Indeed, some RS constructs defy either randomization or manipulation and must simply be measured. But others are, within certain limits, amenable to such treatments. For example, it is quite possible to study the effects of spiritual meditation, prayer, or other RS behavioral variables (e.g., scripture reading) on stress reactivity in the laboratory by: (a) including only participants willing to be randomly assigned to one of these conditions; (b) using random assignment and including specifically designed controls; and (c) exposing participants to a stressor and measuring stress responses (e.g., Wachholtz & Pargament, 2005, 2008, Wachholtz et al., 2015). Such studies, as is true of all laboratory studies, are limited in terms of many aspects of generalizability, but they do provide a method for experimentally manipulating RS variables in a controlled environment. These studies may be useful in examining mediating constructs and therefore may not only shed light on health-relevant outcomes but may also enhance understanding of the mechanisms responsible for those outcomes. In similar fashion, use of new technologies associated with ecological momentary assessment can be advantageous in ascertaining whether effects seen in the lab are found in the natural setting.
The idea of studying behavioral aspects of RS in the lab leads to consideration of an obvious corollary. Though much of RS experience is internal and best measured by self-report, behavioral manifestations of RS are worthy targets for study. Including behavioral measures of RS variables will balance the literature by providing data of a different type from other (non-self-report) sources. Observer ratings of time spent in daily scripture study, service attendance, or spiritually motivated activities (e.g., serving in a soup kitchen as the manifestation of a spiritual calling to serve the disadvantaged) can provide access to RS data that have been rarely obtained.
Finally, we encourage greater sophistication and understanding of the basic theological tenets that underlie many RS beliefs (see also the discussion of religious culture below). An enlightened understanding of these constructs, the so-called insider’s point of view (Cohen & Kitayama, 2007), is likely to produce stronger theoretical lines of research that will have greater practical salience. As one example of how understanding theology may impact research, it may be presumed that individuals who believe that God is ultimately in control of their health display an external locus of health control and are characterized by passive coping strategies. This is often not the case (e.g., Masters & Wallston, 2005; Umezawa et al., 2012) because many of those who believe God is in control also believe that God has charged them with the responsibility to engage in certain behaviors, some health related. These individuals hold two apparently contradictory statements to be simultaneously true: that is, God is in control of health and individuals are responsible for healthy behavior. Although perhaps counter-intuitive to a behavioral medicine professional, such a view is quite understandable to many believers.
Implications
Cultural aspects of RS
Cohen (2009) argues that religion, itself, has the defining characteristics to be considered a culture, and that various religions differ in many ways along culturally-relevant dimensions. Hill et al. (2000) stated that religions provide their adherents with their basic view of reality, or world view, and prescribe ways to live and behave within this reality. The potential influence of religions on the lives of believers is quite encompassing and, therefore, likely to influence many relevant psychological and behavioral concepts. Yet current behavioral medicine studies in this area are characterized by a near-complete neglect of this level of understanding and analysis. Psychological and behavioral medicine studies are usually based on the assumption that RS variables can be meaningfully understood apart from their cultural (religious) underpinnings, what Geertz (1983) referred to in another context as the view from nowhere. Masters and Hooker (2013) argued that such an approach is not only limiting but likely to lead to erroneous conclusions, and offer examples to highlight this point.
RS variables need to be considered within the religious culture in which they are embedded. If this is done, a much deeper and more sophisticated and nuanced understanding of RS in relation to behavioral medicine will be gained. Religious cultures are quite foreign to many social scientists and, as is often the case when encountering unfamiliar cultures, fear and reluctance to engage the culture with an even hand and open mind may arise. It will take time to develop the systematic and sustained types of investigations that can produce the sorts of findings we envision, but this type of effort will greatly advance the entire field.
Interventions
We noted earlier the criticism that whatever successes may occur regarding theoretical or research findings, RS is not worthy of significant attention because its practical applications are severely limited. Essentially, this argument holds that because health professionals may not be able to encourage or discourage religious involvement, belief, or practice, there is no useful outcome that can be produced from the study of RS in terms of clinical practice in behavioral medicine (see Sloan & Bagiella, 2001, 2002; Sloan et al., 2000 for more complete discussion). Although we are quite sympathetic to concerns about improper use of religion or spirituality in behavioral medicine, we do not agree with those who say it has no place in health care, given the large proportions of people who consider RS as quite important to them.
Hooker et al. (2016) recently reported on a feasible and acceptable behavioral medicine intervention, in this case for patients with heart failure, that encourages patients to explore their own sense of RS and seek meaning, purpose or forgiveness within their own spiritual framework. Examples of related work can be found in that of Djuric et al. (2009) for obese African American breast cancer survivors, Holt et al. (2009a; b) addressing prostate cancer screening among church-attending African American men, and Delaney et al. (2011) for community dwelling adults with CVD. Substantial public health benefits could be gained through collaboration between the behavioral medicine community and local and national religious leaders to develop behavioral medicine interventions that are religiously sensitive and that can be delivered in the context of the religious community. RS informed interventions are: (a) appropriate when delivered with proper sensitivity and understanding; and (b) potentially of significant public health benefit.
Funding
A final implication concerns the lack of funding for RS and behavioral medicine research. It is our distinct impression, based on reviews of projects funded by NIH and discussions with NIH staff, that there is, with few exceptions, reluctance to fund research projects that feature RS as a primary focus. This is perhaps due to concerns regarding separation of church and state, though the courts have agreed that funding research in this area is not a violation (Miller & Thoresen, 2003), or it may be due to other reasons including a perceived lack of importance of the topic by social scientists who may have received little or no training in it (Schafer et al., 2011). Given the large numbers of citizens who find RS concerns of substantial importance and whose lives are influenced by these concerns, we believe it is a significant opportunity missed when reasonable levels of funding are not available. These consequences will multiply across the academic and research generations. New faculty may be advised to append their RS measures onto studies designed to answer other questions rather than make RS a central focus of their research careers because, they are warned, they will fail to be funded and thus not progress through the tenure and review systems. We encourage funding organizations to take seriously the evidence and issues discussed in this article and consider ways to improve the funding climate in this important area.
Summary
In this brief article, we provided an overview of how RS relates to health and health-relevant outcomes by reviewing links of RS within the context of major health domains to illustrate how important RS factors are in these areas. We are hopeful that we are not “preaching to the choir” but rather reaching behavioral medicine researchers and practitioners who may or may not be particularly high in RS themselves, but who may not be aware of this large body of information on RS and health, which tends to lie outside the mainstream. RS connects with health across myriad topics, disease and health domains, and outcomes, and we desire to help build bridges with researchers in other areas who may be interested in integrating RS factors into their work. Towards that end, we described important directions for future research to follow, along with some of the challenges and barriers and a number of potential ways to surmount them. We are confident that addressing these issues in virtually any area of behavioral medicine research will yield more complete, valid, and useful findings.
Footnotes
Compliance with ethical standards
Conflict of interest Crystal L. Park, Kevin S. Masters, John M. Salsman, Amy Wachholtz, Andrea D. Clements, Elena Salmoirago-Blotcher, Kelly Trevino, and Danielle M. Wischenka declare that they have no conflict of interest.
Human and animal rights and Informed consent All procedures followed were in accordance with ethical standards of the responsible committee on human experimentation (institutional and national) and with the Helsinki Declaration of 1975, as revised in 2000. Informed consent was obtained from all patients for being included in the study.
References
- Aaron K, Levine D, Burstin H. African American church participation and health care practices. Journal of General Internal Medicine. 2003;18:908–913. doi: 10.1046/j.1525-1497.2003.20936.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agarwal M, Hamilton JB, Crandell JL, Moore CE. Coping strategies of African American head and neck cancer survivors. Journal of Psychosocial Oncology. 2010;28:526–538. doi: 10.1080/07347332.2010.498456. [DOI] [PubMed] [Google Scholar]
- Ai AL, Pargament K, Kronfol Z, Tice TN, Appel H. Pathways to postoperative hostility in cardiac patients: Mediation of coping, spiritual struggle and interleukin-6. Journal of Health Psychology. 2010;15:186–195. doi: 10.1177/1359105309345556. [DOI] [PubMed] [Google Scholar]
- Ai AL, Wink P, Shearer M. Secular reverence predicts shorter hospital length of stay among middle-aged and older patients following open-heart surgery. Journal of Behavioral Medicine. 2011;34:532–541. doi: 10.1007/s10865-011-9334-8. [DOI] [PubMed] [Google Scholar]
- Aldwin CM, Park CL, Jeong YJ, Nath R. Differing pathways between religiousness, spirituality, and health: A self-regulation perspective. Psychology of Religion and Spirituality. 2014;6:9–21. [Google Scholar]
- Asgeirsdottir GH, Sigurbjörnsson E, Traustadottir R, Sigurdardottir V, Gunnarsdottir S, Kelly E. “To cherish each day as it comes”: A qualitative study of spirituality among persons receiving palliative care. Supportive Care in Cancer. 2013;21:1445–1451. doi: 10.1007/s00520-012-1690-6. [DOI] [PubMed] [Google Scholar]
- Assari S. Race and ethnicity, religion involvement, church-based social support and subjective health in United States: A case of moderated mediation. International Journal of Preventive Medicine. 2013;4:208–217. [PMC free article] [PubMed] [Google Scholar]
- Avants SK, Marcotte D, Arnold R, Margolin A. Spiritual beliefs, world assumptions, and HIV risk behavior among heroin and cocaine users. Psychology of Addictive Behaviors. 2006;17:159–162. doi: 10.1037/0893-164x.17.2.159. [DOI] [PubMed] [Google Scholar]
- Banthia R, Moskowitz JT, Acree M, Folkman S. Socioeconomic differences in the effects of prayer on physical symptoms and quality of life. Journal of Health Psychology. 2007;12:249–260. doi: 10.1177/1359105307074251. [DOI] [PubMed] [Google Scholar]
- Benjamins MR. Religious influences on preventive health care use in a nationally representative sample of middle-age women. Journal of Behavioral Medicine. 2006;29:1–16. doi: 10.1007/s10865-005-9035-2. [DOI] [PubMed] [Google Scholar]
- Benjamins MR, Brown C. Religion and preventive health care utilization among the elderly. Social Science and Medicine. 2004;58:109–118. doi: 10.1016/s0277-9536(03)00152-7. [DOI] [PubMed] [Google Scholar]
- Benjamins MR, Trinitapoli J, Ellison CG. Religious attendance, health maintenance beliefs, and mammography utilization: Findings from a nationwide survey of Presbyterian women. Journal for the Scientific Study of Religion. 2006;45:597–607. [Google Scholar]
- Berntson GG, Norman GJ, Hawkley LC, Cacioppo JT. Spirituality and autonomic cardiac control. Annals of Behavioral Medicine. 2008;35:198–208. doi: 10.1007/s12160-008-9027-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumenthal JA, Babyak MA, Ironson G, Thoresen C, Powell L, Czajkowski S, et al. Spirituality, religion, and clinical outcomes in patients recovering from an acute myocardial infarction. Psychosomatic Medicine. 2007;69:501–508. doi: 10.1097/PSY.0b013e3180cab76c. [DOI] [PubMed] [Google Scholar]
- Brechting EH, Giancola PR. A longitudinal study of coping strategies and substance use in adolescent boys. Journal of Child & Adolescent Substance Abuse. 2007;16:51–67. [Google Scholar]
- Button TM, Hewitt JK, Rhee SH, Corley RP, Stallings MC. The moderating effect of religiosity on the genetic variance of problem alcohol use. Alcoholism, Clinical and Experimental Research. 2010;34:1619–1624. doi: 10.1111/j.1530-0277.2010.01247.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Centers for Disease Prevention and Control. Deaths: Final data for 2013. Atlanta, GA: 2013. http://www.cdc.gov/nchs/data/nvsr/nvsr64/nvsr64_02.pdf. [Google Scholar]
- Chida Y, Steptoe A, Powell LH. Religiosity/spirituality and mortality. A systematic quantitative review. Psychotherapy and Psychosomatics. 2009;78:81–90. doi: 10.1159/000190791. [DOI] [PubMed] [Google Scholar]
- Clements A, Ermakova A. Surrender to God and stress: A possible link between religiosity and health. Psychology of Religion and Spirituality. 2012;4:93–107. [Google Scholar]
- Cohen AB. Many forms of culture. American Psychologist. 2009;63:194–204. doi: 10.1037/a0015308. [DOI] [PubMed] [Google Scholar]
- Cohen D, Kitayama S. Cultural psychology: This stanza and the next. In: Kitayama S, Cohen D, editors. Handbook of cultural psychology. New York: Guilford; 2007. pp. 847–851. [Google Scholar]
- Colantonio A, Kasl SV, Ostfeld AM. Depressive symptoms and other psychosocial factors as predictors of stroke in the elderly. American Journal of Epidemiology. 1992;136:884–894. doi: 10.1093/aje/136.7.884. [DOI] [PubMed] [Google Scholar]
- Conner BT, Anglin MD, Annon J, Longshore D. Effect of religiosity and spirituality on drug treatment outcomes. The Journal of Behavioral Health Services & Research. 2009;36:189–198. doi: 10.1007/s11414-008-9145-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cotton S, Zebracki K, Rosenthal SL, Tsevat J, Drotar D. Religion/spirituality and adolescent health outcomes: A review. Journal of Adolescent Health. 2006;38:472–480. doi: 10.1016/j.jadohealth.2005.10.005. [DOI] [PubMed] [Google Scholar]
- Cummings JP, Pargament KI. Medicine for the spirit: Religious coping in individuals with medical conditions. Religions. 2010;1:28–53. [Google Scholar]
- Debnam K, Holt CL, Clark EM, Roth DL, Foushee HR, Crowther M, et al. Spiritual health locus of control and health behaviors in African Americans. American Journal of Health Behavior. 2012a;36:360–372. doi: 10.5993/AJHB.36.3.7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Debnam K, Holt CL, Clark EM, Roth DL, Southward P. Relationship between religious social support and general social support with health behaviors in a national sample of African Americans. Journal of Behavioral Medicine. 2012b;35:179–189. doi: 10.1007/s10865-011-9338-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Delaney C, Barrere C, Helming M. The influence of a spirituality-based intervention on quality of life, depression, and anxiety in community-dwelling adults with cardiovascular disease. Journal of Holistic Nursing. 2011;29:21–32. doi: 10.1177/0898010110378356. [DOI] [PubMed] [Google Scholar]
- Delaney HD, Miller WR, Bisonó AM. Religiosity and spirituality among psychologists: A survey of clinician members of the American Psychological Association. Professional Psychology: Research and Practice. 2007;38:538–546. [Google Scholar]
- DeWall CN, Pond RJ, Carter EC, McCullough ME, Lambert NM, Fincham FD, Nezlek JB. Explaining the relationship between religiousness and substance use: Self-control matters. Journal of Personality and Social Psychology. 2014;107:339–351. doi: 10.1037/a0036853. [DOI] [PubMed] [Google Scholar]
- Dezutter J, Wachholtz A, Corveleyn J. Prayer and pain: The mediating role of positive reappraisal. Journal of Behavioral Medicine. 2011;34:542–546. doi: 10.1007/s10865-011-9348-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Djuric Z, Mirasolo J, Kimbrough L, Brown DR, Deibrun LK, Canar L, et al. A pilot trial of spirituality counseling for weight loss maintenance in African American breast cancer survivors. Journal of the National Medical Association. 2009;101:552–564. doi: 10.1016/s0027-9684(15)30940-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ecklund EH, Scheitle CP. Religion among academic scientists: Distinctions, disciplines, and demographics. Social Problems. 2007;54:289–307. [Google Scholar]
- El Ansari W, Vallentin-Holbech L, Stock C. Predictors of illicit drug/s use among university students in Northern Ireland, Wales and England. Global Journal of Health Science. 2014;7:18–29. doi: 10.5539/gjhs.v7n4p18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ellison CG, Hummer RA, editors. Religion, families, and health: Population-based research in the United States. New Brunswick, NJ: Rutgers University Press; 2010. [Google Scholar]
- Exline JJ, Park CL, Smyth JM, Carey MP. Anger toward God: Social-cognitive predictors, prevalence, and links with adjustment to bereavement and cancer. Journal of Personality and Social Psychology. 2011;100:129–148. doi: 10.1037/a0021716. [DOI] [PubMed] [Google Scholar]
- Feinstein M, Liu K, Ning H, Fitchett G, Lloyd-Jones DM. Burden of cardiovascular risk factors, subclinical atherosclerosis, and incident cardiovascular events across dimensions of religiosity: The multi-ethnic study of atherosclerosis. Circulation. 2010;121:659–666. doi: 10.1161/CIRCULATIONAHA.109.879973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitchett G, Canada AL. The role of religion/spirituality in coping with cancer: Evidence, assessment, and intervention. In: Holland JC, Breitbart WS, Jacobson PB, Lederberg MS, Loscalzo MJ, McCorkle R, editors. Psychooncology. 2. New York: Oxford University Press; 2010. pp. 440–446. [Google Scholar]
- Friedlander Y, Kark JD, Stein Y. Religious orthodoxy and myocardial infarction in Jerusalem—a case control study. International Journal of Cardiology. 1986;10:33–41. doi: 10.1016/0167-5273(86)90163-4. [DOI] [PubMed] [Google Scholar]
- Gall TL. Relationship with God and the quality of life of prostate cancer survivors. Quality of Life Research. 2004;13:1357–1368. doi: 10.1023/B:QURE.0000040789.49691.59. [DOI] [PubMed] [Google Scholar]
- Gall TL, Charbonneau C, Florack P. The relationship between religious/spiritual factors and perceived growth following a diagnosis of breast cancer. Psychology and Health. 2011;26:287–305. doi: 10.1080/08870440903411013. [DOI] [PubMed] [Google Scholar]
- Geertz C. Local knowledge: Further essays in interpretive anthropology. New York: Basic Books; 1983. [Google Scholar]
- George L, Ellison C, Larson D. Explaining the relationships between religious involvement and health. Psychological Inquiry. 2002;13:190–200. [Google Scholar]
- Geppert C, Bogenschutz MP, Miller WR. Development of a bibliography on religion, spirituality and addictions. Drug and Alcohol Review. 2007;26:389–395. doi: 10.1080/09595230701373826. [DOI] [PubMed] [Google Scholar]
- Goldbourt U, Yaari S, Medalie JH. Factors predictive of long-term coronary heart disease mortality among 10, 059 male Israeli civil servants and municipal employees. A 23-year mortality follow-up in the Israeli Ischemic Heart Disease Study. Cardiology. 1993;82:100–121. doi: 10.1159/000175862. [DOI] [PubMed] [Google Scholar]
- Gowing LR, Ali RL, Allsop S, Marsden J, Turf EE, West R, Witton J. Global statistics on addictive behaviours: 2014 Status report. Addiction. 2015;110:904–919. doi: 10.1111/add.12899. [DOI] [PubMed] [Google Scholar]
- Hackett C, Grim B, Stonawski M, Skirbekk V, Potancokova M, Abel G. The global religious landscape. 2012 Retrieved Jan 1, 2016, from http://www.pewforum.org/global-religious-landscape.aspx.
- Hatta ZA. Religion and drug dependency: A comparative study of Malay male youth in Malaysia. Journal of Religion & Spirituality In Social Work: Social Thought. 2010;29:337–348. [Google Scholar]
- Hayatbakhsh R, Clavarino A, Williams GM, Najman JM. Maternal and personal religious engagement as predictors of early onset and frequent substance use. The American Journal on Addictions. 2014;23:363–370. doi: 10.1111/j.1521-0391.2014.12113.x. [DOI] [PubMed] [Google Scholar]
- Hayward RD, Elliott M. Fitting in with the flock: Social attractiveness as a mechanism for well-being in religious groups. European Journal of Social Psychology. 2009;39:592–607. [Google Scholar]
- Hebert R, Zdaniuk B, Schulz R, Scheier M. Positive and negative religious coping and well-being in women with breast cancer. Journal of Palliative Medicine. 2009;12:537–545. doi: 10.1089/jpm.2008.0250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill TD, Ellison CG, Burdette AM, Musick MA. Religious involvement and healthy lifestyles: Evidence from the survey of Texas adults. Annals of Behavioral Medicine. 2007;34:217–222. doi: 10.1007/BF02872676. [DOI] [PubMed] [Google Scholar]
- Hill PC, Pargament KI. Advances in the conceptualization and measurement of religion and spirituality: Implications for physical and mental health research. American Psychologist. 2008;58:64–74. doi: 10.1037/0003-066x.58.1.64. [DOI] [PubMed] [Google Scholar]
- Hill PC, Pargament KI, Hood RW, McCullough ME, Swyers JP, Larson DB, Zinnbauer BJ. Conceptualizing religion and spirituality: Points of commonality, points of departure. Journal for the Theory of Social Behaviour. 2000;30:51–77. [Google Scholar]
- Hill TD, Rote SM, Ellison CG, Burdette AM. Religious attendance and biological functioning a multiple specification approach. Journal of Aging and Health. 2014;26:766–785. doi: 10.1177/0898264314529333. [DOI] [PubMed] [Google Scholar]
- Hoff A, Johannessen-Henry CT, Ross L, Hvidt NC, Johansen C. Religion and reduced cancer risk: what is the explanation? A review. European Journal of Cancer. 2008;44:2573–2579. doi: 10.1016/j.ejca.2008.08.001. [DOI] [PubMed] [Google Scholar]
- Holt CL, Clark EM, Debnam KJ, Roth DL. Religion and health in African Americans: The role of religious coping. American Journal of Health Behavior. 2014a;38:190–199. doi: 10.5993/AJHB.38.2.4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt CL, Roth DL, Clark EM, Debnam K. Positive self-perceptions as a mediator of religious involvement and health behaviors in a national sample of African Americans. Journal of Behavioral Medicine. 2014b;37:102–112. doi: 10.1007/s10865-012-9472-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holt CL, Wynn TA, Litaker MS, Southward P, Jeames S, Schulz E. A comparison of a spiritually based and non-spiritually based educational intervention for informed decision making for prostate cancer screening among church-attending African-American men. Urologic Nursing. 2009a;29:249–258. [PMC free article] [PubMed] [Google Scholar]
- Holt CL, Wynn TA, Southward P, Litaker MS, Jeames S, Schulz E. Development of a spiritually based educational intervention to increase informed decision making for prostate cancer screening among church-attending African American men. Journal of Health Communication: International Perspectives. 2009b;14:590–604. doi: 10.1080/10810730903120534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hooker SA, Ross K, Masters KS, Park C, Hale AE, Allen LA, Bekelman DB. Denver spirited heart: Mixed methods pilot study of a psychospiritual intervention for heart failure patients. Journal of Cardiovascular Nursing. 2016 doi: 10.1097/JCN.0000000000000337. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hummer RA, Rogers RG, Nam CB, Ellison CG. Religious involvement and U.S. adult mortality. Demography. 1999;36:273–285. [PubMed] [Google Scholar]
- Hwang K, Hammer JH, Cragun RT. Extending religion-health research to secular minorities: Issues and concerns. Journal of Religion and Health. 2011;50:608–622. doi: 10.1007/s10943-009-9296-0. [DOI] [PubMed] [Google Scholar]
- Jesse DE, Reed PG. Effects of spirituality and psychosocial well-being on health risk behaviors in Appalachian pregnant women. Journal of Obstetric, Gynecologic, and Neonatal Nursing. 2006;33:739–747. doi: 10.1177/0884217504270669. [DOI] [PubMed] [Google Scholar]
- Jessor R, Costa FM, Krueger PM, Turbin MS. A developmental study of heavy episodic drinking among college students: The role of psychosocial and behavioral protective and risk factors. Journal of Studies on Alcohol. 2006;67:86–94. doi: 10.15288/jsa.2006.67.86. [DOI] [PubMed] [Google Scholar]
- Jim HS, Pustejovsky JE, Park CL, Danhauer SC, Sherman AC, Fitchett G, et al. Religion, spirituality, and physical health in cancer patients: A meta-analysis. Cancer. 2015;121:3760–3768. doi: 10.1002/cncr.29353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kaplar M, Wachholtz A, O’Brien W. The effect of religious and spiritual interventions on the biological, psychological, and spiritual outcomes of oncology patients. Journal of Psychosocial Oncology. 2004;22:39–49. [Google Scholar]
- Kendler KS, Myers J. A developmental twin study of church attendance and alcohol and nicotine consumption: A model for analyzing the changing impact of genes and environment. The American Journal of Psychiatry. 2009;166:1150–1155. doi: 10.1176/appi.ajp.2009.09020182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenig HG. Religion, spirituality, and health: The research and clinical implications. ISRN Psychiatry. 2012;2012:1–33. doi: 10.5402/2012/278730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koenig HG, King D, Carson VB. Handbook of religion and health. 2. New York: Oxford University Press; 2012. [Google Scholar]
- Koenig HG, McCullough ME, Larson DB. Handbook of religion and health. New York: Oxford University Press; 2001. [Google Scholar]
- Koenig LB, Vaillant GE. A prospective study of church attendance and health over the lifespan. Health Psychology. 2009;28:117–124. doi: 10.1037/a0012984. [DOI] [PubMed] [Google Scholar]
- Kovaks E, Piko BF, Fitzpatrick KM. Religiosity as a protective factor against substance use among Hungarian high school students. Substance Use and Misuse. 2011;46:1346–1357. doi: 10.3109/10826084.2011.581322. [DOI] [PubMed] [Google Scholar]
- Krause N. The social foundation of religious meaning in life. Research on Aging. 2008;30:395–427. [Google Scholar]
- Krause N, Wulff KM. Church-based social ties, a sense of belonging in a congregation, and physical health status. International Journal for the Psychology of Religion. 2005;15:73–93. [Google Scholar]
- Kub J, Solari-Twadell PA. Religiosity/spirituality and substance use in adolescence as related to positive development: A literature review. Journal of Addictions Nursing. 2013;24:247–262. doi: 10.1097/JAN.0000000000000006. [DOI] [PubMed] [Google Scholar]
- Lapierre LL. A model for describing spirituality. Journal of Religion and Health. 1994;33:153–161. doi: 10.1007/BF02354535. [DOI] [PubMed] [Google Scholar]
- Laubmeier KK, Zakowski SG, Bair JP. The role of spirituality in the psychological adjustment to cancer: A test of the transactional model of stress and coping. International Journal of Behavioral Medicine. 2004;11:48–55. doi: 10.1207/s15327558ijbm1101_6. [DOI] [PubMed] [Google Scholar]
- Lavery ME, O’Hea EL. Religious/spiritual coping and adjustment in individuals with cancer: Unanswered questions, important trends, and future directions. Mental Health, Religion, & Culture. 2010;13:55–65. [Google Scholar]
- Lee BY, Newberg AB. Religion and health: A review and critical analysis. Zygon. 2005;40:443–468. [Google Scholar]
- Levin JS, Vanderpool HY. Is religion therapeutically significant for hypertension? Social Science and Medicine. 1989;29:69–78. doi: 10.1016/0277-9536(89)90129-9. [DOI] [PubMed] [Google Scholar]
- Magyar-Russell G, Brown IT, Edara IR, Smith MT, Marine JE, Ziegelstein RC. In search of serenity: Religious struggle among patients hospitalized for suspected acute coronary syndrome. Journal of Religion and Health. 2014;53:562–578. doi: 10.1007/s10943-013-9713-2. [DOI] [PubMed] [Google Scholar]
- Masters KS. Mechanisms in the relation between religion and health with emphasis on cardiovascular reactivity to stress. Research in the Scientific Study of Religion. 2008;19:91–115. [Google Scholar]
- Masters KS, Hill RD, Kircher JC, Benson TLL, Fallon JA. Religious orientation, aging, and blood pressure reactivity to interpersonal and cognitive stressors. Annals of Behavioral Medicine. 2004;28:171–178. doi: 10.1207/s15324796abm2803_5. [DOI] [PubMed] [Google Scholar]
- Masters KS, Hooker SA. Religiousness/spirituality, cardiovascular disease, and cancer: cultural integration for health research and intervention. Journal of Consulting and Clinical Psychology. 2013;81:206–216. doi: 10.1037/a0030813. [DOI] [PubMed] [Google Scholar]
- Masters KS, Wallston KA. Canonical correlation reveals important relations between health locus of control, coping, affect and values. Journal of Health Psychology. 2005;10:719–731. doi: 10.1177/1359105305055332. [DOI] [PubMed] [Google Scholar]
- Miller WR, Thoresen CE. Spirituality, religion, and health: An emerging research field. American Psychologist. 2003;58:24–35. doi: 10.1037/0003-066x.58.1.24. [DOI] [PubMed] [Google Scholar]
- Mozaffarian D, Benjamin EJ, Go AS, Arnett DK, Blaha MJ, Cushman M, et al. Heart disease and stroke statistics—2016 Update: A report from the American Heart Association. Circulation. 2016;133:e38–e360. doi: 10.1161/CIR.0000000000000350. [DOI] [PubMed] [Google Scholar]
- Muller D, Judd CM, Yzerbyt VY. When moderation is mediated and mediation is moderated. Journal of Personality and Social Psychology. 2005;89:852–863. doi: 10.1037/0022-3514.89.6.852. [DOI] [PubMed] [Google Scholar]
- Musick MA, Koenig HG, Hays JC, Cohen HJ. Religious activity and depression among community-dwelling elderly persons with cancer: The moderating effect of race. Journal of Gerontology B: Psychological Science and Social Science. 1998;53:218–227. doi: 10.1093/geronb/53b.4.s218. [DOI] [PubMed] [Google Scholar]
- Office of National Drug Control Policy. The national drug control strategy: 2000 Annual report. National Criminal Justice Reference Service; 2000. Report No. NCJ-180082 https://www.ncjrs.gov/ondcppubs/publications/policy/ndcs00/strategy2000.pdf. [Google Scholar]
- Oman D. Religious and spirituality: Evolving meanings. In: Paloutzian RF, Park CL, editors. Handbook of the psychology of religion and spirituality. 2. New York: Guilford; 2013. pp. 23–47. [Google Scholar]
- Oman D, Kurata JH, Strawbridge WJ, Cohen RD. Religious attendance and cause of death over 31 years. The International Journal of Psychiatry in Medicine. 2002;32:69–89. doi: 10.2190/RJY7-CRR1-HCW5-XVEG. [DOI] [PubMed] [Google Scholar]
- Oman D, Thoresen C. Do religion and spirituality influence health? In: Paloutzian RF, Park CL, editors. Handbook of the psychology of religion and spirituality. New York: Guilford; 2005. pp. 435–459. [Google Scholar]
- Pargament KI, Feuille M, Burdzy D. The brief RCOPE: Current psychometric status of a short measure of religious coping. Religion. 2011;2:51–76. [Google Scholar]
- Pargament KI, Tarakeshwar N, Ellison CG, Wulff KM. Religious coping among the religious: The relationships between religious coping and well-being in a national sample of Presbyterian clergy, elders, and members. Journal for the Scientific Study of Religion. 2001;40:497–513. [Google Scholar]
- Park CL. Religiousness/spirituality and health: A meaning systems perspective. Journal of Behavioral Medicine. 2007;30:319–328. doi: 10.1007/s10865-007-9111-x. [DOI] [PubMed] [Google Scholar]
- Park CL. Meaning, spirituality, and growth: Protective and resilience factors in health and illness. In: Baum AS, Revenson TA, Singer JE, editors. Handbook of health psychology. 2. New York: Sage; 2012. pp. 405–430. [Google Scholar]
- Park CL, Moehl B, Fenster JR, Suresh DP, Bliss D. Religiousness and treatment adherence in congestive heart failure patients. Journal of Religion, Spirituality & Aging. 2008;20:249–266. [Google Scholar]
- Park CL, Sherman AC, Jim HS, Salsman JM. Religion/spirituality and health in the context of cancer: Cross-domain integration, unresolved issues, and future directions. Cancer. 2015;121:3789–3794. doi: 10.1002/cncr.29351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pérez JE, Smith AR. Intrinsic religiousness and well-being among cancer patients: the mediating role of control-related religious coping and self-efficacy for coping with cancer. Journal of Behavioral Medicine. 2015;38:183–193. doi: 10.1007/s10865-014-9593-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterman AH, Fitchett G, Brady MJ, Hernandez L, Cella D. Measuring spiritual well-being in people with cancer: The functional assessment of chronic illness therapy—Spiritual Well-being Scale (FACIT-Sp) Annals of Behavioral Medicine. 2002;24:49–58. doi: 10.1207/S15324796ABM2401_06. [DOI] [PubMed] [Google Scholar]
- Peterman AH, Reeve CL, Winford EC, Salsman JM, Tsevat J, Cotton S, et al. Measuring meaning and peace With the FACIT–Spiritual Well-Being Scale: Distinction without a difference? Psychological Assessment. 2014;26:127–137. doi: 10.1037/a0034805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pew Research Center Religion in Public Life. Religious landscape study. Washington, DC: Pew Research Center; 2014. http://www.pewforum.org/religious-landscape-study/ [Google Scholar]
- Porche MV, Fortuna L, Wachholtz A, Torres-Stone R. Distal and proximal religiosity as protective factors for adolescent and emerging adult alcohol use. Religions. 2015;6:365–384. doi: 10.3390/rel6020365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Powell LH, Shahabi L, Thoresen CE. Religion and spirituality: Linkages to physical health. American Psychologist. 2003;58:36–52. doi: 10.1037/0003-066x.58.1.36. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Rucker DD, Hayes AF. Addressing moderated mediation hypotheses: Theory, methods, and prescriptions. Multivariate Behavioral Research. 2007;42:185–227. doi: 10.1080/00273170701341316. [DOI] [PubMed] [Google Scholar]
- Rasic D, Kisely S, Langille DB. Protective associations of importance of religion and frequency of service attendance with depression risk, suicidal behaviours and substance use in adolescents in Nova Scotia, Canada. Journal of Affective Disorders. 2011;132:389–395. doi: 10.1016/j.jad.2011.03.007. [DOI] [PubMed] [Google Scholar]
- Rew L, Wong YJ. A systematic review of associations among religiosity/spirituality and adolescent health attitudes and behaviors. Journal of Adolescent Health. 2006;38:433–442. doi: 10.1016/j.jadohealth.2005.02.004. [DOI] [PubMed] [Google Scholar]
- Rosmarin DH, Wachholtz A, Ai A. Beyond descriptive research: Advancing the study of spirituality and health. Journal of Behavioral Medicine. 2011;34:409–413. doi: 10.1007/s10865-011-9370-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross LE, Hall IJ, Fairley TL, Taylor YJ, Howard DL. Prayer and self-reported health among cancer survivors in the United States, National Health Interview Survey, 2002. The Journal of Alternative and Complementary Medicine. 2008;14:931–938. doi: 10.1089/acm.2007.0788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rozanski A. Behavioral cardiology: Current advances and future directions. Journal of the American College of Cardiology. 2014;64:100–110. doi: 10.1016/j.jacc.2014.03.047. [DOI] [PubMed] [Google Scholar]
- Salmoirago-Blotcher E, Fitchett G, Hovey KM, Schnall E, Thomson C, Andrews CA, et al. Frequency of private spiritual activity and cardiovascular risk in postmenopausal women: The Women’s Health Initiative. Annals of Epidemiology. 2013;23:239–245. doi: 10.1016/j.annepidem.2013.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Salmoirago-Blotcher E, Fitchett G, Ockene JK, et al. Religion and healthy lifestyle behaviors among postmenopausal women: The Women’s Health Initiative. Journal of Behavioral Medicine. 2011;34:360–371. doi: 10.1007/s10865-011-9322-z. [DOI] [PubMed] [Google Scholar]
- Salsman JM, Pustejovsky JE, Jim HS, Munoz AR, Merluzzi TV, Park CL, et al. A meta-analytic approach to examining the correlation between religion/spirituality and mental health in cancer. Cancer. 2015;121:3769–3778. doi: 10.1002/cncr.29350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schafer RM, Handal PJ, Brawer PA, Ubinger M. Training and education in religion/spirituality within APA-accredited clinical psychology programs: 8 years later. Journal of Religion and Health. 2011;50:232–239. doi: 10.1007/s10943-009-9272-8. [DOI] [PubMed] [Google Scholar]
- Schnall E, Wassertheil-Smoller S, Swencionis C, Zemon V, Tinker L, O’Sullivan MJ, et al. The relationship between religion and cardiovascular outcomes and all-cause mortality in the Women’s Health Initiative Observational Study. Psychology and Health. 2010;25:249–263. doi: 10.1080/08870440802311322. [DOI] [PubMed] [Google Scholar]
- Schreiber JA, Brockopp DY. Twenty-five years later—What do we know about religion/spirituality and psychological well-being among breast cancer survivors? A systematic review. Journal of Cancer Survivorship. 2012;6:82–94. doi: 10.1007/s11764-011-0193-7. [DOI] [PubMed] [Google Scholar]
- Sherman AC, Merluzzi TV, Pustejovsky JE, Park CL, Fitchett G, Jim HS, et al. A meta-analytic review of religious or spiritual involvement and social health among cancer patients. Cancer. 2015;121:3779–3788. doi: 10.1002/cncr.29352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman AC, Plante TG, Simonton S, Latif U, Anaissie EJ. Prospective study of religious coping among patients undergoing autologous stem cell transplantation. Journal of Behavioral Medicine. 2009;32:118–128. doi: 10.1007/s10865-008-9179-y. [DOI] [PubMed] [Google Scholar]
- Sloan RP, Bagiella E. Religion and health. Health Psychology. 2001;20:228–229. doi: 10.1037//0278-6133.20.3.228. [DOI] [PubMed] [Google Scholar]
- Sloan RP, Bagiella E. Claims about religious involvement and health outcomes. Annals of Behavioral Medicine. 2002;24:14–21. doi: 10.1207/S15324796ABM2401_03. [DOI] [PubMed] [Google Scholar]
- Sloan RP, Bagiella E, VandeCreek L, Hover M, Casalone C, Hirsch Jinpu, et al. Should physicians prescribe religious activities? New England Journal of Medicine. 2000;342:1913–1916. doi: 10.1056/NEJM200006223422513. [DOI] [PubMed] [Google Scholar]
- Sternthal MJ, Williams DR, Musick MA, Buck AC. Religious practices, beliefs, and mental health: variations across ethnicity. Ethnicity and Health. 2012;17:171–185. doi: 10.1080/13557858.2012.655264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Serviced Administration [SAMHSA] Center for Substance Abuse Prevention. Substance abuse prevention dollars and cents: A cost-benefit analysis. Washington, DC: U.S. Government Printing Office; 2008. DHHS Publication No. (SMA) 07-4298. [Google Scholar]
- Tarakeshwar N, Vanderwerker LC, Paulk E, Pearce MJ, Kasl SV, Prigerson HG. Religious coping is associated with the quality of life of patients with advanced cancer. Journal of Palliative Medicine. 2006;9:646–657. doi: 10.1089/jpm.2006.9.646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thune-Boyle IC, Stygall JA, Keshtgar MR, Newman SP. Do religious/spiritual coping strategies affect illness adjustment in patients with cancer? A systematic review of the literature. Social Science and Medicine. 2006;63:151–164. doi: 10.1016/j.socscimed.2005.11.055. [DOI] [PubMed] [Google Scholar]
- Umezawa Y, Lu Q, You J, Kagawa-Singer M, Leake B, Maly RC. Belief in divine control, coping, and race/ethnicity among older women with breast cancer. Annals of Behavioral Medicine. 2012;44:21–32. doi: 10.1007/s12160-012-9358-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urcuyo KR, Boyers AE, Carver CS, Antoni MH. Finding benefit in breast cancer: Relations with personality, coping, and concurrent well-being. Psychology & Health. 2005;20:175–192. [Google Scholar]
- Vallurupalli MM, Lauderdale MK, Balboni MJ, Phelps AC, Block SD, Ng AK, et al. The role of spirituality and religious coping in the quality of life of patients with advanced cancer receiving palliative radiation therapy. The Journal of Supportive Oncology. 2012;10:81–87. doi: 10.1016/j.suponc.2011.09.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Visser A, Garssen B, Vingerhoets A. Spirituality and well-being in cancer patients: A review. Psycho-Oncology. 2010;19:565–572. doi: 10.1002/pon.1626. [DOI] [PubMed] [Google Scholar]
- Wachholtz A, Malone C, Pargament K. Effect of different meditation types on migraine headache medication use. Behavioral Medicine. 2015 doi: 10.1080/08964289.2015.1024601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wachholtz A, Pargament K. Is spirituality a critical ingredient of meditation? Comparing the effects of spiritual meditation, secular meditation, and relaxation on spiritual, psychological, cardiac, and pain outcomes. Journal of Behavioral Medicine. 2005;28:369–384. doi: 10.1007/s10865-005-9008-5. [DOI] [PubMed] [Google Scholar]
- Wachholtz A, Pargament K. Migraines and meditation: Does spirituality matter? Journal of Behavioral Medicine. 2008;31:351–366. doi: 10.1007/s10865-008-9159-2. [DOI] [PubMed] [Google Scholar]
- Walton-Moss B, Ray EM, Woodruff K. Relationship of spirituality or religion to recovery from substance abuse: A systematic review. Journal of Addictions Nursing. 2013;24:217–226. doi: 10.1097/JAN.0000000000000001. [DOI] [PubMed] [Google Scholar]
- Wang Z, Koenig HG, Al Shohaib S. Religious involvement and tobacco use in mainland China: A preliminary study. BMC Public Health. 2015;72:660–668. doi: 10.1186/s12889-015-1478-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White HR, McMorris BJ, Catalano RF, Fleming CB, Haggerty KP, Abbott RD. Increases in alcohol and marijuana use during the transition out of high school into emerging adulthood. Journal of Studies on Alcohol. 2006;67:810–822. doi: 10.15288/jsa.2006.67.810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whooley MA, Boyd AL, Gardin JM, Williams DR. Religious involvement and cigarette smoking in young adults: The CARDIA study. Archives of Internal Medicine. 2002;162:1604–1610. doi: 10.1001/archinte.162.14.1604. [DOI] [PubMed] [Google Scholar]
- Yeung JK, Chan Y, Lee BK. Youth religiosity and substance use: A meta-analysis from 1995–2007. Psychological Reports. 2009;105:255–266. doi: 10.2466/PR0.105.1.255-266. [DOI] [PubMed] [Google Scholar]