Abstract
PURPOSE
18F-fluoroestradiol (FES) positron emission tomography (PET) scans measure regional estrogen binding, and 18F-fluorodeoxyglucose (FDG) PET measures tumor glycolytic activity. We examined quantitative and qualitative imaging biomarkers of progression-free survival in breast cancer patients receiving endocrine therapy.
EXPERIMENTAL DESIGN
Ninety patients with breast cancer from an estrogen receptor positive, HER2-negative primary tumor underwent FES PET and FDG PET scans prior to endocrine therapy (63% aromatase inhibitor, 22% aromatase inhibitor and fulvestrant, 15% other). Eighty-four had evaluable data for progression-free survival prediction.
RESULTS
Recursive partitioning with fivefold internal cross-validation used both FES PET and FDG PET measures to classify patients into three distinct response groups. FDG PET identified 24 patients (29%) with low FDG uptake, suggesting indolent tumors. These patients had a median progression-free survival of 26.1 months (95% confidence interval 11.2-49.7). Of patients with more FDG-avid tumors, 50 (59%) had high average FES uptake, and 10 (12%) had low average FES uptake. These groups had median progression-free survival of 7.9 (5.6-11.8) and 3.3 months (1.4-not evaluable), respectively. Patient and tumor features did not replace or improve the PET measures’ prediction of progression-free survival. Prespecified endocrine resistance classifiers identified in smaller cohorts did not individually predict progression-free survival.
CONCLUSION
A wide range of therapy regimens are available for treatment of ER+ metastatic breast cancer, but no guidelines are established for sequencing these therapies. FDG PET and FES PET may help guide the timing of endocrine therapy and selection of targeted and/or cytotoxic chemotherapy. A multicenter trial is ongoing for external validation.
Keywords: Breast cancer, FES PET, FDG PET, endocrine therapy, estrogen receptor
Introduction
Patients with distant metastatic breast cancer from an estrogen receptor positive (ER+) primary tumor are rarely cured but often live for many years with their disease (1). Clinical management of these patients is not standardized, but generally involves a series of endocrine therapy treatment regimens, cytotoxic chemotherapy, and additional targeted agents (2, 3). Many patients achieve a durable response to endocrine therapy with few toxicities; however, not all patients benefit from endocrine therapy, and most responding tumors eventually become refractory (4). The primary biomarkers for directing therapy for these patients are in vitro assays of hormone receptor (ER, PgR) expression. Beyond binary ER classification, higher levels of tumor ER expression are associated with greater clinical benefit from endocrine therapy (5).
In vivo imaging using 18F-fluoroestradiol (FES) PET measures regional estrogen binding in breast cancer tumors (6), and FES uptake quantitation has good agreement with ER expression measured by immunohistochemistry (7, 8). Early clinical studies summarized FES uptake in a single field-of-view (FOV) to predict clinical response to endocrine therapy (9-11). We extend that approach by using FES PET imaging to evaluate quantitative and qualitative ER expression at multiple disease sites in a torso survey performed immediately following the single FOV scan, and by including FDG uptake to distinguish between indolent tumors and those that are metabolically aggressive (12). Prior clinical studies with FES PET imaging prior to endocrine therapy showed promising results, even with small sample sizes and limited follow-up (9-11). Our primary goal for this work was to assess imaging classifiers suggested by prior research as predictors of response to endocrine therapy in a larger cohort with mature time-to-event endpoints. We explore these imaging biomarkers and patient/disease characteristics as predictors of progression-free survival (PFS), overall survival (OS), and clinical benefit (6+ months on endocrine therapy without progressive disease).
Materials and Methods
Patients
Study participants were recruited from the University of Washington Medical Center and the Seattle Cancer Care Alliance (UWMC/SCCA). Eligible patients were planning endocrine therapy for primary, recurrent, or metastatic breast cancer, and had an ER-expressing primary tumor. Each patient provided informed consent for one of four prospective, observational FES PET studies evaluating: (1) heterogeneity of FES uptake in patients with advanced breast cancer, (2) agreement of FES uptake to in vitro assay of ER, (3) FES uptake as a predictor of therapy response, or (4) patients with newly diagnosed stage IV disease to be treated with endocrine therapy. Use of FES was carried out under the University of Washington Radioactive Drug Research Committee (1-3) or NCI IND #79005 approval (4).
Enrolled patients were planning to receive one of the following standard of care treatments: tamoxifen +/− ovarian suppression, aromatase inhibitor (AI) +/− fulvestrant (with ovarian suppression in pre-menopausal patients) or fulvestrant or ovarian suppression alone. A washout period of 6-8 weeks for tamoxifen or fulvestrant was required prior to FES PET imaging, since these agents block the tracer from binding to the receptor. No washout period was required for AIs. Some patients were switching from a non-steroidal to a steroidal AI due to lack of response or disease progression following initial response or clinical benefit. In other cases, AI was continued and fulvestrant was added. Patient treatment was selected in advance of FES PET; referring physicians had access to imaging results, but FES PET was not used to make treatment decisions.
In vitro assays
Primary tumor immunohistochemistry results were obtained by chart review when possible. For samples analyzed at the UWMC/SCCA, positive staining in >5% cells indicated a positive result. Slides or tissue blocks were requested for re-analysis when necessary.
PET imaging
Patients underwent FDG and FES studies prior to or shortly following initiation of or changes to endocrine therapy. Imaging was performed with a GE ADVANCE PET or GE Discovery STE PET/CT scanner operating in the high sensitivity mode. The two scanners have nearly identical PET components, providing comparable quantitative PET data. For the 90 patients in the primary analysis, all but 3 FES scans were performed using the GE ADVANCE PET scanner; FDG scans for those 3 patients and an additional 12 were performed on the DSTE PET/CT. Rigorous cross-calibration was performed between the two PET scanners, for overall scale factor and resolution matching, using the NEMA-NU2 image quality phantom (13).
FDG imaging
2-[F-18]fluoro-2-deoxy-D-glucose (FDG) was produced on site by University of Washington radiochemists according to established techniques, with quality control testing done on every batch (14). FDG imaging was done according to standard clinical procedures. Briefly, regardless of which machine was used, a dose of 260-370 MBq (7-10 mCi) of FDG was administered intravenously following a minimum 4 hour fast. Patients rested comfortably for 45-60 minutes in a supine position prior to FDG PET scanning. For the PET/CT device, a low dose CT scan provided data for attenuation correction. On the ADVANCE, 3-minute attenuation scans were constructed for each of 5 FOVs. Each emission scan was 7 minutes per FOV. Attenuation or CT-corrected emission data was reconstructed by standard filtered back-projection after correction for scattered and random coincidences. Reconstruction used a 10 mm Hanning Filter producing a 128 pixel × 128 pixel × 35 slice imaging volume, yielding a reconstructed in-plane spatial resolution of 4.29 mm. A subset of scans were also reconstructed using iterative methods (ordered-subset expectation maximization); comparisons of SUV quantification are described in an online supplement.
FES imaging
16α-18F-fluoro-17β-estradiol (FES) was prepared locally by the PET Radiochemistry Group at the University of Washington using established methods for synthesis and quality assurance. All tracer characteristics, including specific activity and the total mass of FES in the injectate, were well within established ranges, as previously described (15, 16). Per protocol, following a 25 minute attenuation scan (or low dose CT scan on the PET/CT), a dose of 148-222 MBq (4-6 mCi) FES was infused intravenously in a volume of 20 mL isotonic phosphate buffered saline containing less than 15% of ethanol by volume over 2 minutes and dynamic imaging was performed for 60 minutes over a 15 cm body region containing the most prominent tumor sites, starting at the beginning of infusion. Following the dynamic data collection, a neck-to-pelvis torso survey covering 5 × 15 cm axial FOVs was performed using 5-minute emission and 3-minute post-injection attenuation scans (or low dose CT on the PET/CT) per FOV. Although dynamic scans were performed to maintain a consistent protocol, ongoing analysis of FES data showed that static torso scans were sufficient for measuring FES uptake and allowed analysis of total disease burden. Therefore static measurements from a torso sweep have become the focus of future analysis. Attenuation or CT-corrected emission data was reconstructed according to the same specifications as the FDG scans, described above.
FDG PET and PET/CT Image analysis
FDG images were processed as for a typical clinical scan, corrected for radioactive decay of the tracer, and normalized to the injected dose and body weight. This results in regional standardized uptake values (SUVs): SUV = A/(ID/BW) where A is the tissue tracer uptake in microcuries per gram for the hottest pixel in the tumor (SUVmax), ID is the injected dose in millicuries, and BW is the body weight in kilograms. SULmax was also calculated, normalized by lean body mass instead of body weight. Lesions identified on FDG PET were corroborated by CT and/or other imaging.
FES PET Qualitative assessment
Qualitative (visual) assessment of FES was performed using attenuation-corrected torso images. Active sites of disease visualized on the clinical FDG PET scan or CT scan were matched to the FES torso scan using a rigid co-registration/fusion module (PMOD Technologies Ltd, Zurich, Switzerland). Each disease site was evaluated as positive or negative for FES uptake, compared to normal tissue background. These qualitative assessments were summarized at the patient level as presence/absence of any site(s) qualitatively negative for FES uptake. Qualitative assessments were conducted by a single experienced observer with simultaneous access to both FES and FDG images. Three experienced readers evaluated a subset of 19 cases, with no disagreements on scan-level qualitative assessment (16).
FES PET Quantitative Assessment
For quantitative assessment of FES uptake, lesions were identified and localized using the FDG scan matched to the FES scan, as described above. A cubic region-of-interest was drawn on 3 adjacent planes (approximately 3 cc total volume) to identify the area with greatest FES uptake for each disease site. Up to 3 lesions were quantified on the summed dynamic scan, and all lesions recorded on the clinical FDG scan (other than liver lesions) were quantified on the static torso survey. Partial-volume correction was not applied because only sites 1.5 cm3 or greater were included. FES uptake was quantified as the standardized uptake value (SUV, or SUL with lean body mass (LBM) correction) on both the 30-60 min summed images of the dynamic scan and for the torso survey. For each lesion, region-of-interest mean and maximum SUV and SUL were recorded, with LBM estimated from height (cm) and weight (kg) (17). Results of a “draw-redraw” reader study in a subset of scans showed excellent agreement for SUV quantitation for both FES and FDG PET (18).
Study Treatment and Monitoring of Response
Clinical follow-up and response assessment followed standard of care at UW/SCCA and included additional clinical FDG PET scans, conventional imaging (e.g. CT, MRI, bone scan), serum tumor markers, and evaluation of symptoms, as deemed appropriate by the treating physician. Progression-free survival (PFS) was measured from the date of the FES PET scan to the date of progressive disease or death from any cause. For patients who did not experience progressive disease or were lost to follow-up more than 4 months before death, PFS was censored at the date of the last radiographic assessment that did not show progressive disease, or at surgery for patients receiving neoadjuvant endocrine therapy. Overall survival was measured from the date of FES PET scan until death, and was censored at the last date the patient was known to be alive. Clinical benefit was defined as 6 or more months on endocrine therapy without progressive disease or death (PFS6), and was missing if a patient had <6 months of follow-up.
Statistical methods
Imaging biomarkers evaluated as predictors of PFS, OS, and 6-month response
A primary aim of this study was to validate FES SUV ≤1.5 as a classifier to identify patients who would be unlikely to benefit from endocrine therapy. The cutpoint of FES SUV ≤1.5 (for the average uptake for up to 3 lesions in the dynamic scan field-of-view, “FES dynSUV”) had been reported by our group as a threshold under which patients were unlikely to benefit from endocrine therapy (11). While the average uptake for up to three lesions is likely a good patient-level summary (18), subsequent development of FES PET measures has suggested alternative parameterizations to optimize performance of FES quantitative biomarkers. These alternatives include the use of SUVs measured on the torso survey (19, 20), lean body mass adjustments (15), and log-transformation prior to averaging to limit the influence of extreme measurements (21).
Another proposed alternative parameterization is the ratio of FES SUVmax and FDG SUVmax. Weighting the FES uptake by metabolic aggressiveness (as measured by FDG SUV) could serve as an “index of differentiation” (22). In addition, since both FDG and FES uptake measures are similarly impacted by partial-volume effects, the ratio of FES to FDG uptake measures minimizes tumor partial volume effects. Therefore, we prospectively defined additional patient-level measures to test for associations with PFS, OS, and PFS6:
-
1)
Geometric mean of FES SULmean (lean body mass adjusted SUV) for the 3 lesions with the highest FDG SUVmax in the torso scan (FES SULmean3, cutpoint 1.0)
For the torso scan portion of the FES PET sequence, a SULmean of 1.0 or 1.1 was found to be roughly equivalent to the dynamic scan SUVmean of 1.5 (18). The geometric mean was used to accommodate log transformation. The average value for 3 lesions was selected because within-patient FES uptake did not vary greatly by lesion (18), and assessment of a large number of lesions does not improve quantitation in settings such as the RECIST criteria for measuring treatment response (23). The 3 lesions with highest FDG uptake were selected as the most relevant for therapy selection, since targeting of an indolent FES-avid lesion would not be successful therapy if an aggressive, resistant lesion remained.
-
2)
Presence/absence of lesion(s) with FES SULmean ≤ 1 and FDG SUVmax > 5
The classification of the presence/absence of aggressive lesions was based on the threshold for low FES SULmean (11, 18) and an arbitrary threshold of 5 for a “high” FDG SUVmax.
-
3)
Presence/absence of tumor site(s) qualitatively negative for FES uptake
The qualitative assessment of FES uptake was assessed as a straightforward measure that would take less time to assess than quantitative measures. Again the focus was on identifying FES-negative lesions hypothesized to be resistant to endocrine therapy.
Analysis plan
The primary analysis evaluated the incremental value of summary imaging measures for predicting progression-free survival (PFS). First, Cox proportional hazards regression was used to evaluate patient characteristics (age), disease characteristics (months since primary cancer diagnosis, number of tumors in the torso scan, number of prior treatment regimens for metastatic disease, presence/absence of visceral disease), and tumor characteristics (PgR, histology) as potential predictors. Then each imaging biomarker was assessed for additional contributions. Secondary response measures were overall survival (OS) and clinical benefit (PFS6). Predictors were evaluated using Cox proportional hazards regression and logistic regression, with all tests two-sided.
Exploratory analyses used tree-based methods to identify clinically important subgroups potentially identified by combinations of factors (24). Patient characteristics, disease history, tumor histology, and imaging biomarkers were assessed as predictors of PFS using recursive partitioning, choosing splits based on reduction of a one-step deviance (25) and pruning to minimize cross-validation prediction error (26). Statistical analyses were conducted using SAS/STAT software, version 9.4 (SAS Institute, Inc., Cary, NC), including the %ICC9 macro (27) (for concordance analysis reported in the online supplement), and R version 3.1.3 (R Foundation for Statistical Computing, Vienna, Austria), including the rpart() package.
Results
FES PET scans were conducted in 110 patients scheduled for initiation of or change in endocrine therapy, between January 2000 and January 2011. Ninety-one patients’ scans were from an earlier series evaluating between- and within-patient FES uptake heterogeneity (18), and 19 were previously described in a single-center IND study (16). Twenty patients were excluded from this analysis. Thirteen had HER2+ disease. Four others received additional or alternate therapy, 2 had adverse events (pneumonia, surgical complications) soon after imaging, and one did not have dynamic FES PET data. Approximately 35 of the remaining patients appeared in a prior analysis (11), but that study examined objective response rather than PFS, OS, or PFS6.
Patient and disease characteristics are described in Table 1 for the 90 patients eligible for response analysis. The mean age at the time of FES PET was 56 years (standard deviation 11 years), and patients ranged in age from 28-79 years old. Time from breast cancer diagnosis to FES PET ranged from 0 months to over 20 years, with a median of 4 years and 0-5 prior chemotherapy regimens for metastatic disease. The number of tumors identified by FES PET and FDG PET was 1-16, with a median of 5 tumors per patient. Sixty-seven patients had a date of progression identified, with no deaths as PFS events. The 57 deaths recorded included 11 patients whose PFS was censored (at 0-7 months).
Table 1.
Patient and disease characteristics as recorded at time of FES PET scan, and clinical outcomes (n=90).
| N (%) | |
|---|---|
| Age | |
| <50 years | 26 (29%) |
| ≥ 50 years | 64 (71%) |
| Sex | |
| Female | 88 (98%) |
| Male | 2 (2%) |
| Menopausal status | |
| Pre-menopausal | 14 (16%) |
| Post-menopausal/male | 76 (84%) |
| Time since breast cancer diagnosis | |
| <2 months | 22 (24%) |
| 2 months - 5 years | 31 (34%) |
| >5 years | 37 (41%) |
| Primary tumor PgR | |
| Positive or weakly positive | 72 (80%) |
| Negative | 14 (16%) |
| Not assessed | 4 (4%) |
| Histology of primary breast cancer | |
| Ductal | 66 (73%) |
| Lobular | 17 (19%) |
| Ductal and lobular | 6 (7%) |
| Unknown | 1 (1%) |
| Visceral disease at time of scan | |
| Liver, lung, stomach lesion(s) | 14 (16%) |
| No liver, lung, stomach lesion(s) | 76 (84%) |
| Endocrine therapy following FES PET | |
| Aromatase inhibitor | 56 (62%) |
| Aromatase inhibitor + fulvestrant | 20 (22%) |
| Tamoxifen | 9 (10%) |
| Ovarian suppression only | 2 (2%) |
| Fulvestrant | 2 (2%) |
| Unknown | 1 (1%) |
| Progression-free survival | |
| Events | 67 (74%, range 1-50 months) |
| Censored | 23 (26%, range 0-54 months) |
| Overall survival | |
| Events (deaths) | 57 (63%, range 5-128 months) |
| Censored | 33 (37%, range 3-130 months) |
| Clinical benefit | |
| PFS > 6 months | 47 (52%, 60% of assessed) |
| PFS ≤ 6 months | 31 (34%) |
| Not assesseda | 12 (13%) |
| mean (standard deviation), range |
|
| FES dynSUV | 2.73 (1.80), 0.50-9.62 |
| FES SULmean3b | 1.80 (1.35), 0.17-6.67 |
| FES SUVmax3b | 2.84 (1.79), 0.57-8.79 |
| FDG SULmax3b | 3.69 (2.43), 0.77-15.16 |
| FDG SUVmax3b | 5.78 (3.74), 1.25-22.95 |
| FES/FDG ratio3c | 0.92 (0.29), 0.34-1.71 |
7 patients had surgery or chemotherapy within 6 months of FES PET scan and without disease progression; 5 others were lost to follow-up within 6 months of FES PET scan
FES SULmean3 = , geometric mean for up to 3 lesions in torso sweep with highest FDG SUVmax. Others are similarly constructed geometric means.
FES/FDG ratio3 = , average of square root of measure for up to 3 lesions in torso sweep with highest FDG SUVmax
PgR progesterone receptor
PFS progression-free survival
FES dynSUV average of FES SUVmean of up to 3 lesions in the dynamic field of view
Imaging classifiers of endocrine resistance
Table 2 shows the distributions for four proposed classifiers of endocrine resistance. Measures based on the quantitative FES and FDG PET had 20-29% rate of predicted endocrine resistance. The rate was lower for the qualitative reads, with lesions lacking FES uptake above background detected in only 12 of 90 scans (13%, 95% confidence interval 8%-22%). More than half of patients (51/90) had tumors with sufficiently high FES uptake for all 4 classifiers to indicate likely response to endocrine therapy; in contrast, classification of likely nonresponders among the remaining patients varied greatly. Detailed measures of agreement are reported in an online supplement.
Table 2.
Descriptive statistics for predefined classifiers for endocrine resistance (n=90).
| Classifier | description | N (%) |
|---|---|---|
| FES dynSUV ≤ 1.5 | FES dynSUV = average of FES SUVmean for up to 3 lesions in the dynamic field-of-view |
24/90 (27%) |
| FES SULmean3 ≤ 1 | (see Table 1)a | 26/90 (29%) |
| any low FES/FDG | any low FES/FDG = presence of any lesion with FES SULmean ≤ 1 and FDG SUVmax > 5 |
17/88a (19%) |
| qualitative FES neg | qualitative FES neg = presence of any lesion lacking FES uptake above background (qualitative read) |
12/90 (13%) |
2 patients had FDG PET scan from outside sites, used to locate lesions but not for uptake quantification; to calculate SULmean3 for these patients, 3 lesions were selected at random (from 5, 8 lesions).
Prediction of response to endocrine therapy
PFS was assessed in 84 patients, excluding 2 patients without quantitative FDG PET and 4 patients followed only for OS. Analysis of PFS6 excluded an additional 8 patients censored for PFS before 6 months.
Before evaluating PET classifiers to predict PFS, we examined patient and disease characteristics. Using statistical significance (likelihood-ratio test p-value < 0.05) as a criterion, age, presence of visceral disease, number of prior chemotherapy regimens for metastatic disease, and tumor histology were dismissed as predictors of PFS in this cohort. Additional predictors associated with OS but not PFS in univariate models were PgR (hazard ratio 3.3 for negative, p=0.002), burden of disease as measured by log-transformed number of lesions (hazard ratio 1.8, p=0.002), and log-transformed number of months from cancer diagnosis to FES PET scan (hazard ratio 1.2, p=0.01). All remained statistically significant in a multivariable model predicting OS.
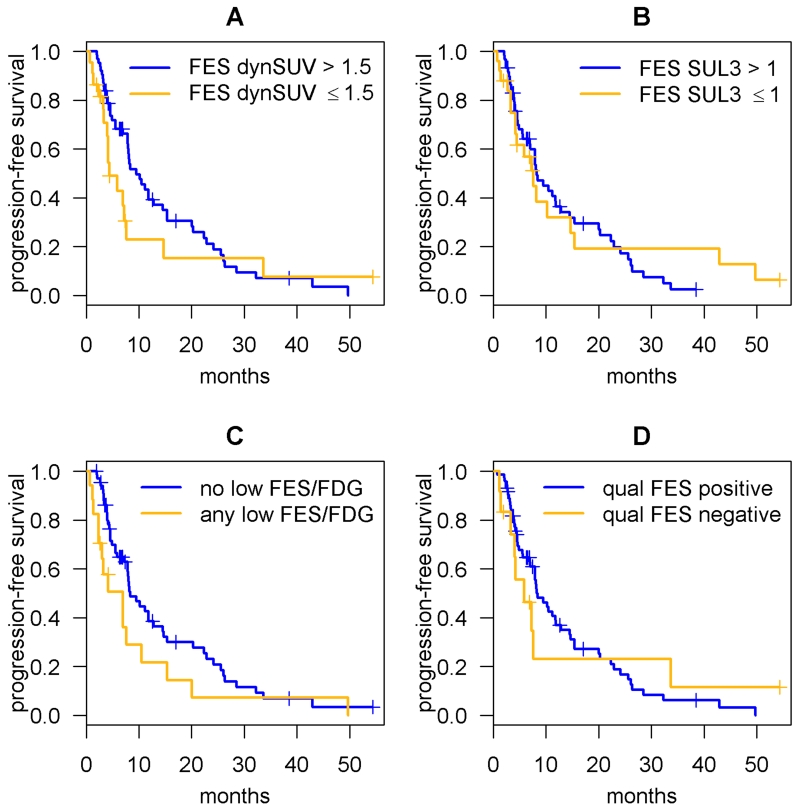
None of the four preselected binary PET classifiers predicted PFS (Figure 1, log-rank p>0.05). They also did not contribute beyond PgR, time since diagnosis, and number of lesions for predicting OS (likelihood-ratio p>0.10). Fully quantitative individual measures (without pre-specified cutpoints) are displayed in Figure S2 (online supplement), and do not show a strong association with clinical benefit (PFS6).
Figure 1.
Kaplan-Meier curves of progression-free survival (PFS) for prespecified quantitative imaging classifiers predicting endocrine response (N=84, p>0.05 for all). A. FES dynSUV = average of FES SUVmean of up to 3 lesions in the dynamic field-of-view B. FES SUL3 = geometric mean of FES SULmean (lean-body-mass adjusted FES SUVmean) for up to 3 lesions in torso sweep with highest FDG SUVmax C. any low FES/FDG = presence of any lesion with FES SULmean < 1 and FDG SUVmax > 5 D. qualitative FES neg = presence of any lesion lacking FES uptake above background (qualitative read).
Because the prospectively planned analysis did not yield a clear answer for further development of biomarkers for endocrine therapy response, we conducted an exploratory analysis using data-driven criteria to select the “best” predictors of PFS. Predictors examined included patient (age) and clinical variables (PgR, number of lesions, visceral disease, number of prior chemotherapy regimens for metastatic disease), and imaging parameters (FES dynSUV, FES SULmean3, FES/FDG ratio3, qualitative FES). Additional imaging characteristics were included, each evaluated as a geometric mean for up to 3 lesions in the torso sweep with highest FDG SUVmax (FES SULmax3, FES SUVmax3, FDG SULmax3, FDG SUVmax3).
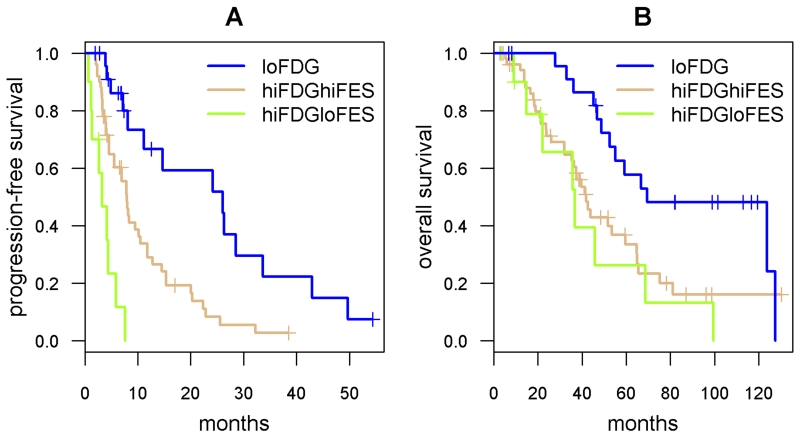
Recursive partitioning with equal costs for all covariates, selecting the number of splits that minimized the fivefold cross-validated prediction error (26), led to a model with FDG SULmax3 and FES dynSUV predicting PFS. Patients with low FDG uptake suggesting indolent tumors (FDG SULmax3 <2.2) had the most favorable PFS; among patients whose lesions were more FDG-avid, patients with FES-avid lesions had more favorable PFS on endocrine therapy. The FES dynSUV cutpoint of 1.47 was essentially the same as previously identified for predicting objective response (11). However, since dynamic FES PET protocols are not considered essential for quantification of FES uptake (15) and 30-minute summed images are not clinically practical for a single field-of-view, recursive partitioning was repeated without FES dynSUV, selecting FDG SULmax3 and FES SULmean3 (Table 3). Evaluated by Kaplan-Meier methods and the log-rank test, the three groups identified by recursive partitioning had markedly different PFS (Figure 2A, p<0.001). These groups also predicted OS (Figure 2B, p=0.01) and PFS6 (Table 3, Wald test, p<0.001).
Table 3.
Prediction of progression-free survival (PFS), overall survival (OS), and clinical benefit (PFS > 6 months on endocrine therapy) by a 3-level classifier based on FDG and FES PET results (“Group”). This classifier was selected by recursive partitioning with fivefold internal cross-validation as the best predictor of PFS among patient (age) and clinical variables (PgR, number of lesions, visceral disease, number of prior chemotherapy regimens for metastatic disease), and imaging parameters (FES SULmean3, FES/FDG ratio, qualitative FES, and alternate summaries such as FES SUVmax3).
| Group | N (PFS) |
Median months PFS (95% confidence interval) |
N (OS) |
Median months OS (95% confidence interval) |
PFS >6 months (95% confidence interval) |
|---|---|---|---|---|---|
| FDG SULmax3 < 2.2 | 24 | 26.1 (11.2 – 49.7) |
24 | 69.5 (55.1 – NE) |
18/21 = 86% (65%, 95%) |
| FDG SULmax3 ≥ 2.2 FES SULmean3 ≥ 0.85 |
50 | 7.9 (5.6 – 11.8) |
53 | 41.9 (36.3 – 64.7) |
27/46 = 59% (44%, 72%) |
| FDG SULmax3 ≥ 2.2 FES SULmean3 < 0.85 |
10 | 3.3 (1.4 - NE) |
11 | 36.8 (22.1 – NE) |
1/9 = 11% (1%, 43%) |
N=88 for OS excludes 2 without FDG SULmax quantified
N=84 for PFS also excludes 4 without follow-up for progression
N=76 for clinical benefit also excludes 8 censored for progression before 6 months
FDG SULmax3 = geometric mean of FDG SULmax for 3 lesions in torso sweep with highest FDG SUVmax
FES SULmean = geometric mean of FES SULmean for 3 lesions in torso sweep with highest FDG SUVmax (see Table 1 footnotes)
NE = not evaluable
Figure 2.
Results of recursive partitioning to classify endocrine response (see Table 3). Kaplan-Meier curves: A. Progression-free survival (PFS) predicted by FES SULmean3 and FDG SULmax3 (log-rank test p<0.001). B. Overall survival (OS) predicted by FES SULmean3 and FDG SULmax3 (log-rank test p=0.01).
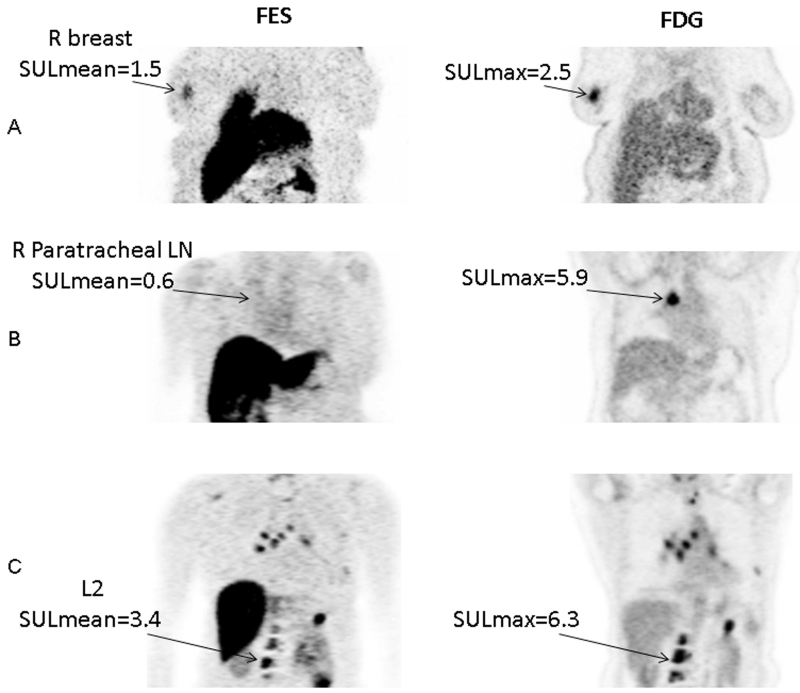
Twenty-four of the patients (27%) were identified by FDG PET as having indolent disease, with a median PFS of 26.1 months, 86% rate of clinical benefit (6+ months of response or stable disease on endocrine therapy), and median overall survival of over 5 years. A representative case is displayed in Figure 3A. FES PET was used to stratify the remaining patients’ expected benefit from endocrine therapy. Representative cases are displayed for patients with high FDG SULmax3 and high FES SULmean3 (Figure 3B), and high FDG SULmax3 and low FES SULmean3 (Figure 3C). The dramatic difference in median PFS detected through tree-based exploratory analysis (7.9 versus 3.3 months for high versus low FES SULmean3) appeared to apply to clinical benefit (59% versus 11%), but the groups did not differ in median OS (42 versus 37 months) (Table 3, Figure 2). When added to a Cox regression model predicting OS, the three-way PET classifier was an independent predictor beyond PgR, time since diagnosis, and number of lesions for predicting OS (likelihood-ratio p=0.046). Exclusion of the 5 patients with early stage disease did not affect the cutpoints for the 3-way classifier for PFS; additional sensitivity analyses applying recursive partitioning to OS and PFS6 endpoints, and models only considering SUVmax and SULmax imaging parameters, are described in the online supplement.
Figure 3.
Representative cases for the three classification groups in Table 3 and Figure 2. Coronal view from FES PET and FDG PET scans. Ordered-subset expectation maximization (OSEM) reconstruction was used for improved presentation, but not for quantitation. A. low FDG SULmax3. This 56-yo woman had 4 lesions in her breast and lymph nodes. Geometric mean FDG SULmax for the 3 hottest lesions was 1.5. (Geometric mean FES SULmean was 1.1.) She was on anastrozole for 5 months until progression. B. high FDG SULmax3 and low FES SULmean3. This 59-yo woman had 5 lesions in lymph nodes and spine. Geometric mean FDG SULmax for the 3 hottest lesions was 4.4. Geometric mean FES SULmean3 was 0.3. She was on tamoxifen for 3 months until progression. C. high FDG SULmax3 and high FES SULmean3. This 59-yo woman had lesions in the breast, chest wall, and hilar nodes, as well as multiple bony lesions. Geometric mean FDG SULmax for the 3 hottest lesions was 12.7. Geometric mean FES SULmean was 6.6. She was on exemestane for 9.5 months until progression.
Discussion
We analyzed imaging characteristics and tumor response in ER+ breast cancer patients undergoing endocrine therapy in a mixed first-line and salvage setting. We prespecified 4 potential imaging biomarker classifiers to predict response to endocrine therapy. The classifiers used information from FDG PET and/or FES PET, and included a qualitative FES PET measure. Although none of these classifiers predicted PFS or OS in multivariate models controlling for known risk factors, exploratory tree-based methods revealed a novel three-way classification using both FDG and FES PET results. In this heterogeneous and heterogeneously treated population, with varying disease stage and lines of prior therapy, about 13% (11/88) of patients displayed a phenotype (high average FDG SULmax3, low average FES SULmean3) that was unlikely to benefit from endocrine therapy. Our analysis suggested that FES and FDG PET imaging can help guide therapy selection, or therapy dosing (28), and assist clinicians who face an expanding array of therapeutic options. Sorting patients into 3 groups (indolent disease, aggressive but strongly ER avid, and aggressive and weakly ER avid) has relevance for clinicians and patients weighing toxicities, costs, and logistics of therapeutic options. For instance, an FES PET scan would not be necessary to predict outcome, if the FDG PET indicates indolent disease.
Our results suggest that for ER+ (primary) breast cancer, patients with indolent disease by FDG PET are potential candidates for endocrine therapy, as are patients with more aggressive disease but high ER activity as detected by FES PET. While the 3-way classifier is novel, our results are consistent with and complementary to prior studies predicting response to endocrine therapy. Average FES SUVmean of about 1.5 from a single-field-of-view dynamic scan, the same classifier used in earlier studies to predict clinical response (11), predicted superior PFS but only in patients with non-indolent (FDG SULmax3 ≥ 2.2) disease. A nearly identical cutpoint for FDG SULmax was selected to predict OS, even though none of the PFS events were deaths. FES cutpoints of 0.85 (SULmean3) and 1.5 (dynSUV) may seem too close to background activity to allow reproducible quantification, but background activity for FES is <1 due to intense uptake in the liver. Some expected predictors of response to endocrine therapy, such as primary tumor PgR expression, did not predict PFS or OS in this heterogeneous, moderately-sized cohort.
This study has several limitations. First, patient disease characteristics in this heterogeneous patient population arising form 4 different studies varied greatly beyond having had ER+ primary breast cancer. At the time, these patients were all candidates for endocrine therapy, but these studies predated modern molecularly targeted drugs. We did not take into account prior benefit from endocrine therapy, or indolent disease as suggested by late recurrence. There also may be period effects in supportive care, treatment options, and patient selection due to the 12-year range of recruitment. The use of older PET reconstruction methods was necessary for attempted validation of prior quantitative uptake measure cutpoints, but may limit the generalizability of our classification. Although the sample size is relatively large (and outcomes data relatively complete) for a study of novel biomarkers that cannot be assessed retrospectively, it is too small for rigorous internal validation of cutpoints, and external validation is required as well. Our analysis also does not consider tumor genomic profiles or account for acquired mutations in ER (29-31), as these assays were not performed routinely during that time. However, this study reflects key advantages of imaging. First, imaging assesses the entire burden of disease rather than a sample of tissue or plasma tumor DNA. Additionally, patients may refuse biopsy due to fears of pain or treatment delay, sampling may not be feasible, and tissue sampled from metastatic disease is not analyzable in many cases (32). An imaging biomarker trial applying FES PET and FDG PET prospectively in a multicenter study (NCT02398773) will further evaluate qualitative and quantitative PET parameters as predictors of endocrine therapy response.
In conclusion, our data suggest that the combination of FDG PET and FES PET will be useful in discriminating between patients with disease that is indolent or amenable to endocrine therapy, and patients whose disease is more aggressive and is unlikely to respond to endocrine therapy. Further confirmation with a prospective study design and modern options for endocrine and molecularly targeted treatment is needed to test the ability of combined FDG and FES PET to guide therapy selection for patients with ER+ metastatic breast cancer.
Supplementary Material
Translational Relevance.
Currently, a wide range of therapy regimens are available for treatment of estrogen receptor positive (ER+) metastatic breast cancer, including endocrine therapy, cytotoxic chemotherapy, and molecularly targeted therapy. However, no guidelines are established for sequencing or combining these therapies. 18F-fluorodeoxyglucose (FDG) PET and 18F-fluoroestradiol (FES) positron emission tomography (PET) may help guide the timing of endocrine therapy and selection of other targeted and/or cytotoxic chemotherapy. FDG PET is widely used to measure tumor glycolytic activity. FES PET measures regional estrogen binding and is not yet available clinically. Unlike tissue sampling, these imaging assays may evaluate the entire burden of metastatic disease. By identifying indolent tumors and tumors likely to respond to endocrine therapy, FDG PET and FES PET may be developed as predictive biomarkers to inform decisions about when to prescribe toxic and/or costly therapies as part of the often lengthy sequence of treatments for ER+ metastatic breast cancer.
Acknowledgments
We gratefully acknowledge financial support from a Fred Hutchinson Cancer Research Center Breast Cancer Research Program Pilot grant (Safeway), NCI Phase I and II Cancer Imaging Program (Contract #N01-CM-37008, Protocol 8052), Komen SAC140060, and NIH grants CA42045, CA148131, and DOD W81XWH-04-01-0675. This project used the UPCI Biostatistics Shared Resource Facility that is supported in part by award P30CA047904. We also thank Thomas Lawton, Kim Allison, Mark Muzi, Paul Kinahan, the study participants, the referring physicians, and the nuclear medicine team in the University of Washington Radiology Department.
Footnotes
Conflicts of Interest: None.
Presented in part at the Society of Nuclear Medicine and Molecular Imaging Annual Meeting, Vancouver, BC, June 8-12, 2013.
References
- 1.Kwast AB, Voogd AC, Menke-Pluijmers MB, Linn SC, Sonke GS, Kiemeney LA, et al. Prognostic factors for survival in metastatic breast cancer by hormone receptor status. Breast Cancer Res Treat. 2014;145(2):503–511. doi: 10.1007/s10549-014-2964-0. [DOI] [PubMed] [Google Scholar]
- 2.Baselga J, Campone M, Piccart M, Burris HA, 3rd, Rugo HS, Sahmoud T, et al. Everolimus in postmenopausal hormone-receptor-positive advanced breast cancer. N Engl J Med. 2012;366(6):520–529. doi: 10.1056/NEJMoa1109653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Turner NC, Ro J, Andre F, Loi S, Verma S, Iwata H, et al. Palbociclib in Hormone-Receptor-Positive Advanced Breast Cancer. N Engl J Med. 2015;373(3):209–219. doi: 10.1056/NEJMoa1505270. [DOI] [PubMed] [Google Scholar]
- 4.Johnston SR. BOLERO-2 - will this change practice in advanced breast cancer? Breast Cancer Res. 2012;14(3):311. doi: 10.1186/bcr3126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Early Breast Cancer Trialists’ Collaborative G. Davies C, Godwin J, Gray R, Clarke M, Cutter D, et al. Relevance of breast cancer hormone receptors and other factors to the efficacy of adjuvant tamoxifen: patient-level meta-analysis of randomised trials. Lancet. 2011;378(9793):771–784. doi: 10.1016/S0140-6736(11)60993-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mintun MA, Welch MJ, Siegel BA, Mathias CJ, Brodack JW, McGuire AH, et al. Breast cancer: PET imaging of estrogen receptors. Radiology. 1988;169(1):45–48. doi: 10.1148/radiology.169.1.3262228. [DOI] [PubMed] [Google Scholar]
- 7.Peterson LM, Mankoff DA, Lawton T, Yagle K, Schubert EK, Stekhova S, et al. Quantitative imaging of estrogen receptor expression in breast cancer with PET and 18F-fluoroestradiol. J Nucl Med. 2008;49(3):367–374. doi: 10.2967/jnumed.107.047506. [DOI] [PubMed] [Google Scholar]
- 8.Gemignani ML, Patil S, Seshan VE, Sampson M, Humm JL, Lewis JS, et al. Feasibility and predictability of perioperative PET and estrogen receptor ligand in patients with invasive breast cancer. J Nucl Med. 2013;54(10):1697–1702. doi: 10.2967/jnumed.112.113373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mortimer JE, Dehdashti F, Siegel BA, Katzenellenbogen JA, Fracasso P, Welch MJ. Positron emission tomography with 2-[18F]Fluoro-2-deoxy-D-glucose and 16alpha-[18F]fluoro-17beta-estradiol in breast cancer: correlation with estrogen receptor status and response to systemic therapy. Clin Cancer Res. 1996;2(6):933–939. [PubMed] [Google Scholar]
- 10.Mortimer JE, Dehdashti F, Siegel BA, Trinkaus K, Katzenellenbogen JA, Welch MJ. Metabolic flare: indicator of hormone responsiveness in advanced breast cancer. J Clin Oncol. 2001;19(11):2797–2803. doi: 10.1200/JCO.2001.19.11.2797. [DOI] [PubMed] [Google Scholar]
- 11.Linden HM, Stekhova SA, Link JM, Gralow JR, Livingston RB, Ellis GK, et al. Quantitative fluoroestradiol positron emission tomography imaging predicts response to endocrine treatment in breast cancer. J Clin Oncol. 2006;24(18):2793–2799. doi: 10.1200/JCO.2005.04.3810. [DOI] [PubMed] [Google Scholar]
- 12.Ulaner GA, Eaton A, Morris PG, Lilienstein J, Jhaveri K, Patil S, et al. Prognostic value of quantitative fluorodeoxyglucose measurements in newly diagnosed metastatic breast cancer. Cancer Med. 2013;2(5):725–733. doi: 10.1002/cam4.119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Daube-Witherspoon ME, Karp JS, Casey ME, DiFilippo FP, Hines H, Muehllehner G, et al. PET performance measurements using the NEMA NU 2-2001 standard. J Nucl Med. 2002;43(10):1398–1409. [PubMed] [Google Scholar]
- 14.Hamacher K, Coenen HH, Stocklin G. Efficient stereospecific synthesis of no-carrier-added 2-[18F]-fluoro-2-deoxy-D-glucose using aminopolyether supported nucleophilic substitution. J Nucl Med. 1986;27(2):235–238. [PubMed] [Google Scholar]
- 15.Peterson LM, Kurland BF, Link JM, Schubert EK, Stekhova S, Linden HM, et al. Factors influencing the uptake of 18F-fluoroestradiol in patients with estrogen receptor positive breast cancer. Nucl Med Biol. 2011;38(7):969–978. doi: 10.1016/j.nucmedbio.2011.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Peterson LM, Kurland BF, Schubert EK, Link JM, Gadi VK, Specht JM, et al. A phase 2 study of 16alpha-[18F]-fluoro-17beta-estradiol positron emission tomography (FES-PET) as a marker of hormone sensitivity in metastatic breast cancer (MBC) Mol Imaging Biol. 2014;16(3):431–440. doi: 10.1007/s11307-013-0699-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hallynck TH, Soep HH, Thomis JA, Boelaert J, Daneels R, Dettli L. Should clearance be normalised to body surface or to lean body mass? British Journal of Clinical Pharmacology. 1981;11:523–526. doi: 10.1111/j.1365-2125.1981.tb01163.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kurland BF, Peterson LM, Lee JH, Linden HM, Schubert EK, Dunnwald LK, et al. Between-Patient and Within-Patient (Site-to-Site) Variability in Estrogen Receptor Binding, Measured In Vivo by 18F-Fluoroestradiol PET. J Nucl Med. 2011;52(10):1541–1549. doi: 10.2967/jnumed.111.091439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dehdashti F, Mortimer JE, Trinkaus K, Naughton MJ, Ellis M, Katzenellenbogen JA, et al. PET-based estradiol challenge as a predictive biomarker of response to endocrine therapy in women with estrogen-receptor-positive breast cancer. Breast Cancer Res Treat. 2009;113(3):509–517. doi: 10.1007/s10549-008-9953-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.van Kruchten M, Glaudemans AW, de Vries EF, Beets-Tan RG, Schroder CP, Dierckx RA, et al. PET imaging of estrogen receptors as a diagnostic tool for breast cancer patients presenting with a clinical dilemma. J Nucl Med. 2012;53(2):182–190. doi: 10.2967/jnumed.111.092734. [DOI] [PubMed] [Google Scholar]
- 21.Thie JA, Hubner KF, Smith GT. The diagnostic utility of the lognormal behavior of PET standardized uptake values in tumors. J Nucl Med. 2000;41(10):1664–1672. [PubMed] [Google Scholar]
- 22.Mankoff DA, Dehdashti F. Imaging tumor phenotype: 1 plus 1 is more than 2. J Nucl Med. 2009;50(10):1567–1569. doi: 10.2967/jnumed.108.061044. [DOI] [PubMed] [Google Scholar]
- 23.Hillman SL, An MW, O’Connell MJ, Goldberg RM, Schaefer P, Buckner JC, et al. Evaluation of the optimal number of lesions needed for tumor evaluation using the Response Evaluation Criteria in Solid Tumors: A North Central Cancer Treatment Group investigation. J Clin Oncol. 2009;27(19):3205–3210. doi: 10.1200/JCO.2008.18.3269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Clark GM, Hilsenbeck SG, Ravdin PM, De Laurentiis M, Osborne CK. Prognostic factors: rationale and methods of analysis and integration. Breast Cancer Res Treat. 1994;32(1):105–112. doi: 10.1007/BF00666211. [DOI] [PubMed] [Google Scholar]
- 25.LeBlanc M, Crowley J. Relative risk trees for censored survival data. Biometrics. 1992;48(2):411–425. [PubMed] [Google Scholar]
- 26.Everitt B, Hothorn T. A handbook of statistical analyses using R. CRC Press; Boca Raton: 2006. [Google Scholar]
- 27.Hankinson SE, Manson JE, Spiegelman D, Willett WC, Longcope C, Speizer FE. Reproducibility of plasma hormone levels in postmenopausal women over a 2-3-year period. Cancer Epidemiol Biomarkers Prev. 1995;4(6):649–654. [PubMed] [Google Scholar]
- 28.Heidari P, Deng F, Esfahani SA, Leece AK, Shoup TM, Vasdev N, et al. Pharmacodynamic imaging guides dosing of a selective estrogen receptor degrader. Clin Cancer Res. 2015;21(6):1340–1347. doi: 10.1158/1078-0432.CCR-14-1178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Schiavon G, Hrebien S, Garcia-Murillas I, Cutts RJ, Pearson A, Tarazona N, et al. Analysis of ESR1 mutation in circulating tumor DNA demonstrates evolution during therapy for metastatic breast cancer. Sci Transl Med. 2015;7(313):313ra182. doi: 10.1126/scitranslmed.aac7551. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang P, Bahreini A, Gyanchandani R, Lucas PC, Hartmaier RJ, Watters RJ, et al. Sensitive Detection of Mono- and Polyclonal ESR1 Mutations in Primary Tumors, Metastatic Lesions, and Cell-Free DNA of Breast Cancer Patients. Clin Cancer Res. 2016;22(5):1130–1137. doi: 10.1158/1078-0432.CCR-15-1534. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Leyland-Jones B, Gray KP, Abramovitz M, Bouzyk M, Young B, Long B, et al. ESR1 and ESR2 polymorphisms in the BIG 1-98 trial comparing adjuvant letrozole versus tamoxifen or their sequence for early breast cancer. Breast Cancer Res Treat. 2015;154(3):543–555. doi: 10.1007/s10549-015-3634-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Amir E, Miller N, Geddie W, Freedman O, Kassam F, Simmons C, et al. Prospective study evaluating the impact of tissue confirmation of metastatic disease in patients with breast cancer. J Clin Oncol. 2012;30(6):587–592. doi: 10.1200/JCO.2010.33.5232. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.