Abstract
Objectives
To assess the association between U.S. state medical marijuana laws (MML), the most liberal category of marijuana policies before legalization, their specific provisions, and adolescent past-30-day use and heavy marijuana use.
Methods
This quasi-experimental study used state Youth Risk Behavior Survey (YRBS) data collected during 1991–2011 from 45 states (N=715,014) to examine MML effects, taking advantage of heterogeneity across states in MML status and design. Multiple logistic regression modeling was used to adjust for state and year effects, and youth demographics.
Results
Unadjusted analyses found that MMLs were associated with higher rates of adolescent past-30-day marijuana use (odds ratio [OR]=1.08, 95% confidence interval, [(CI)=1.03,1.13]) and heavy marijuana use (OR=1.12, [CI=1.05,1.21]). However, analyses adjusting for state/year effects found a 7% lower odds of use (OR=0.99, [CI=0.98,0.999]) and no difference in heavy use. In the adjusted models, years since MML enactment (OR=0.93, [CI=0.86,0.99]) and MML inclusion of more liberalized provisions (OR=0.98, [CI=0.96,0.998]) were associated with slightly lowered odds of past-30-day marijuana use. Conversely, allowance for ≥2.5 usable marijuana ounces was associated with higher past-30-day marijuana use odds (OR=1.21, [CI=1.09,1.34]) and a voluntary vs. mandatory patient registration with higher odds of both past-30-day use (OR=1.41, [CI=1.28,1.56]) and heavy use (OR=1.23, [CI=1.08,1.40]).
Conclusions
MML enactment, years since enactment, and inclusion of more liberalized provisions were not associated with increased adolescent marijuana use in this dataset after adjusting for state and year effects; however, higher possession limits and a voluntary registration were. It is possible that state norms are the impetus for MML enactment.
Keywords: marijuana, medical marijuana, marijuana laws, youth, substance use, heavy marijuana use
1. INTRODUCTION
Since 1975, marijuana has been the most widely used illicit drug among adolescents in the United States (Johnston et al., 2015). Patterns and attitudes of substance use are often established in adolescence and marijuana use typically begins in the middle to late adolescence (Hall and Degenhardt, 2009). The Monitoring in the Future survey reports that daily marijuana use increased among 8th, 10th and 12th graders from 2007–2011 before declining with 21.2 % of 12th graders, 16.6% of 10th graders, and 6.5% of 8th graders reporting past 30-day marijuana use (Johnston et al., 2014). Keyes et al. (2016) reports that perceived harmfulness of marijuana is lower in states with MMLs. This is a grave public health concern since current research suggests that marijuana use may have both acute and long-term deleterious effects on the maturing adolescent brain (Camchong et al., 2016; Squeglia and Gray, 2016). Heavy marijuana use during adolescence could have more serious effects than use in adulthood (Jager and Ramsey, 2008) with studies of heavy adolescent marijuana users reporting learning and working memory impairments up to six weeks post cessation (Schweinsburg et al., 2008)
Marijuana cultivation and use were legal under federal and state laws throughout most of U.S. history; however, an increase in marijuana use coupled with political pressure in the early 1900s led twenty-nine states to pass laws prohibiting any sale or possession of marijuana. These state-level changes initiated federal-level prohibition marijuana policies, including the Marihuana Tax Act of 1937, making the nonmedical use of marijuana illegal (Pacula et al., 2002; Stack and Suddath, 2009) and effectively halted the medicinal use of marijuana (Belenko, 2000; Bilz, 1992; Pacula et al., 2002). The Federal Controlled Substance Act of 1970 replaced the Marihuana Tax Act, and additionally made it illegal under federal law for physicians to prescribe marijuana. Although, marijuana use, possession, cultivation, and physician prescribing has been illegal under federal law since the 1970, more recently states are challenging this prohibition.
As of September, 2016, twenty-five states and the District of Columbia have enacted varying laws that effectively allow patients to use marijuana for medicinal purposes. State medical marijuana laws (MMLs) have been fervently debated. The American College of Pediatricians state concern that marijuana legalization policies may increase adolescent marijuana exposure and use, additionally stating that there is no scientific evidence that the potential healthful effects of legalizing medical marijuana use outweigh its documented adverse effects (American College of Pediatricians, 2016). Volkow et al. (2016) state concern that the efforts to normalize marijuana are being driven without regard for scientific evidence, gaps in our knowledge and the possibility of unintended consequences. Given the accelerated pace at which states are enacting similar MMLs, it is critical to have a better understanding of how previous state-enacted MMLs and their varying provisions affect adolescent marijuana use.
MMLs are enacted at the state-level, leaving great variation amongst MMLs across states in regards to the years of enactment/implementation, included provisions, the varying degree of liberalization of these provisions (e.g., medical marijuana dispensaries, number of usable ounces allowed for possession, etc.), and the fidelity of implementation and enforcement, which may theoretically affect the perceived riskiness, access, cost, and quantity of marijuana within a state. Despite these increasing concerns, there is still limited empirical information available (Wall et al., 2016).
Current research examining the effects of MMLs on adolescents shows mixed results. A literature search identified ten studies that used large national datasets to assess adolescent marijuana use amidst medical marijuana policy reform, with two studies supporting the perspective that MMLs are associated with higher marijuana use rates (Stolzenberg et al., 2016; Wall et al., 2011) and the other eight supporting the perspective that MMLs do not significantly change marijuana use rates (Anderson et al., 2014; Choo et al., 2014; Harper et al., 2012; Hasin et al., 2015; Lynn-Landsman et al., 2013; Pacula et al., 2013; Wall et al., 2016; Wen et al., 2015).
However, the analyses of the two studies finding increases in adolescent marijuana use post-MML were contradicted by replication studies that adjusted for state fixed effects (Harper et al., 2012; Wall et al., 2016). Most previous studies tend to be limited by the inclusion of a small number of states/years, and treat MMLs as uniform across states, rather than a heterogeneous set of provisions; However, research has begun to assess the heterogeneity in state-level MMLs and provisions (Bestrashniy and Winters, 2015; Chapman et al, 2016). Moreover, few studies have examined how MMLs affect heavy marijuana use rates among adolescents. This study used 20 years of data collection in 45 states to examine the effects of MMLs, varying provisions and the degree of provision liberalization on adolescent past-30-day marijuana and heavy marijuana use.
2. METHODS
2.1 Data
Individual-level data (N=715,014) consisted of state Youth Risk Behavior Surveillance (YRBS) data collected in up to 45 states biennially from 1991 to 2011. The YRBS is a cross-sectional school-based survey of representative samples of 9th through 12th grade students conducted by the Centers for Disease Control and Prevention (CDC) and various state and local agencies. State samples were drawn using a two-stage cluster sampling design that first randomly selected schools to participate, and then classes within those schools (CDC, 2013). State data that were collected from a scientifically selected sample and a ≥60% response rate were weighted to yield estimates representative of all 9–12th grade students within the state (CDC, 2013). For this study, only state YRBS data that could be weighted were included. Of the 395 state-year YRBS datasets available between 1991 and 2011 across the 45 participating states, 123 were excluded because data did not meet criteria for weighting. The number of participating states in this sample ranged from six states in 1991, with the number of participating states increasing each year of data collection, to include forty-one states in 2011. Three key MML states: Oregon, California, and Washington did not have any weighted YRBS data available and were therefore not included in the analyses.
This study took advantage of the heterogeneity across states in MML year of enactment and included provisions. State-level data on MML provisions and year of enactment were collected and cross-checked using marijuana reform proponent websites, various state government websites, National Conference of State Legislatures, and the Office of National Drug Control Policy. Among the states that had YRBS data between 1991 and 2011, twelve states had enacted MMLs through 2011 (Table 1). Ten states enacted MMLs during study years and had both pre- and post-MML data. Two states (Colorado and Vermont) enacted MMLs during study years, but only had post-MML data.
Table 1.
Years of youth risk behavior survey (YRBS) data collection before and after medical marijuana law (MML) enactment.
| State | Year MML Enacted |
Years of Data Pre-MML |
Years of Data Post-MML |
|---|---|---|---|
| States that enacted MML between 1991–2011 (Study Years) | |||
| Alaska (AK) | 1998 | 1 | 4 |
| Arizona (AZ) | 2010 | 4 | 1 |
| Colorado (CO) | 2000 | 0 | 3 |
| Delaware (DE) | 2011 | 5 | 1 |
| Maine (ME) | 1999 | 2 | 6 |
| Michigan (MI) | 2008 | 6 | 2 |
| Montana (MT) | 2004 | 6 | 4 |
| Nevada (NV) | 2000 | 4 | 5 |
| New Jersey (NJ) | 2010 | 3 | 1 |
| New Mexico (NM) | 2007 | 2 | 3 |
| Rhode Island (RI) | 2006 | 4 | 3 |
| Vermont (VT) | 2004 | 0 | 1 |
| States in sample that enacted MML after 2011 (post-study years)a | |||
| Connecticut (CT) | 2012 | 5 | 0 |
| Illinois (IL) | 2013 | 5 | 0 |
| Massachusetts (MA) | 2012 | 10 | 0 |
| New Hampshire (NH) | 2013 | 7 | 0 |
| New York (NY) | 2014 | 7 | 0 |
| Maryland (MD) | 2014 | 4 | 0 |
| Pennsylvania (PA) | 2016 | 1 | 0 |
| Ohio (OH) | 2016 | 7 | 0 |
States enacted MML after study years. Data cannot infer any changes from policy enactment.
2.2 Variables
2.2.1 Dependent variables
Dependent variables included two dichotomous variables at the individual-level: (1) past-30-day marijuana use, coded ‘yes’ if an adolescent reported any marijuana use in the past 30-days, and (2) past-30-day heavy marijuana use, coded ‘yes’ if the adolescent reported using marijuana ≥20 times in the past 30 days.
2.2.2 Independent variables
Independent variables included both predictor and adjustment variables. Adjustment variables, included: year (11 dichotomous variables to indicate each biennial year of data collection, 1991–2011), state (45 dichotomous variables to indicate each state), and individual demographics: age, gender, White, Black, Hispanic, and other. MML predictor variables included both dichotomous and ordinal variables, further categorized under: medical marijuana laws (“general”), and five MML provision categories (“provisions”): dispensaries, home cultivation, caregivers, possession, and patient registration.
The general MML variables include: whether the state had legalized medical marijuana in the year data were collected (“MML” yes/no), years since MML enacted (“years since enacted”), and whether it’s been four or more years since MML was enacted (“≥4 years since enacted” yes/no). The MML provisions variables include: whether a state allowed MML dispensaries to operate (“dispensaries” yes/no), whether a state had active dispensaries in the year data were collected (“active dispensaries” yes/no), whether a state allowed for-profit dispensaries in addition to the more common, non-profit dispensaries (“for-profit dispensaries” yes/no), whether a state allowed home cultivation of medical marijuana (“home cultivation” yes/no), number of medical marijuana plants allowed for home cultivation growth (“number of plants”), whether a state allowed for the home cultivation of ten or more medical marijuana plants (“≥10 plants” yes/no), number of usable medical marijuana ounces allowed for possession (“usable ounces”), whether a state allowed possession of ≥ 2.5 usable ounces of medical marijuana (“≥ 2.5 usable ounces” yes/no), whether a state’s medical marijuana patient registration was voluntary (“registration voluntary” yes/no), the number of patients caregivers are allowed (“number of patients”), and whether states allowed caregivers to have five patients, the max amount (“5 patients” yes/no).
We also created a variable for whether a state allowed for MML individuals to possess, cultivate and provide medical marijuana to qualified patients (“caregivers” yes/no). All twelve MML states in this sample had this provision, making this variable perfectly collinear with the overall MML status variable. However, the twelve states did vary in the number of patients that caregivers were allowed, so this latter measure was usable in regressions.
Sensitivity analyses were run to construct the dichotomous variables to further assess “more liberalized” vs. “less liberalized” provisions (e.g., ≥ 2.5 usable ounces). To further assess the degree of liberalization and effects of specific provisions groupings, we created two ordinal index variables. One was a provision index score [scored “1” if a MML had caregivers and/or home cultivation, and scored 2–5 depending on the number of more liberalized provisions in addition to allowance for home cultivation and/or caregivers, including: (a) dispensaries for profit OR dispensaries active in 2011, (b) ≥10 plants, (c) ≥2.5 usable ounces, (d) 5 patients, and (e) registration voluntary]. The other index variable was a dispensary index [scored “1” if a state had MML, but dispensaries were not allowed, scored “2” if dispensaries were allowed, and scored “3” if dispensaries were allowed and were additionally active in 2011 and/or for-profit dispensaries permitted].
Table 2 lists the provisions and index scores for each state that legalized medical marijuana during the study period, along with the number/percent of individual-level data observations accounted for by each state.
Table 2.
Specific law provisions and degree of provision liberalization for states with a medical marijuana law (MML).
| State | MML Provision Categories | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Dispensaries | Home cultivation | Possession | Caregivers+ | Patient Registry |
Index Scores | |||||
| Any allowed | Active by 2011 |
For-profit allowed |
Any allowed |
≥10 plants |
≥2.5 usable ounces |
5 patients allowed |
Voluntary | Prov.1 | Disp.2 | |
| AK | Yes | 1 | 1 | |||||||
| AZ | Yes | Yes | Yes | Yes | Yes | 4 | 1 | |||
| CO* | Yes | Yes | Yes | Yes | Yes | 4 | 3 | |||
| DE | Yes | Yes | Yes | Yes | 3 | 2 | ||||
| ME | Yes | Yes | Yes | Yes | Yes | Yes | 5 | 3 | ||
| MI | Yes | Yes | Yes | Yes | 4 | 1 | ||||
| MT | Yes | 1 | 1 | |||||||
| NV | Yes | Yes | Yes | 2 | 3 | |||||
| NJ | Yes | Yes | 2 | 3 | ||||||
| NM | Yes | Yes | Yes | Yes | Yes | 4 | 3 | |||
| RI | Yes | Yes | Yes | Yes | Yes | 4 | 2 | |||
| VT* | Yes | Yes | 1 | 2 | ||||||
| Total | 9 (75,913) | 2 (29,455) | 4 (28,619) | 10 (98,168) | 4 (32,583) | 6 (57,167) | 6 (50,777) | 1 (28,149) | 12 (102,124) | |
| Percentage of adolescents living in state with this MML provision out of all states with a MML (N=102,124) | ||||||||||
| % | 74.33 | 28.84 | 28.02 | 96.13 | 31.91 | 55.98 | 49.72 | 27.56 | 100 | |
| Percentage of adolescents living in state with this MML provision out of all observations (N=735,352) | ||||||||||
| % | 10.32 | 4 | 3.89 | 13.35 | 4.43 | 7.77 | 6.91 | 3.83 | 13.89 | |
Caregivers: All 12 MML states in this study allow for caregivers
States in which this study only has post-MML enactment YRBS data
Prov.: Provision Index Score
Disp.: Dispensary Index Score
2.3 Data Analysis
State-level MML policy data and individual-level YRBS data were merged using Stata MP 13. Because our dependent variables were dichotomous, we used logistic regression analyses yielding odds ratios (OR) and their two-sided 95% confidence intervals (CI), to examine the association between the MML variables and adolescent marijuana use variables.
We initially conducted unadjusted logistic regression analysis to examine the association between each MML variable and adolescent past 30-day marijuana and heavy marijuana use without any adjustment variables, “Unadjusted” columns in Table 3. A separate multiple fixed effects logistic regression model was estimated for each MML variable and each adjustment variable separately to assess differential effects of each adjustment variable, data not shown. Lastly, a final separate fixed effects multiple logistic regression model was estimated for each predictor variable with all adjustment variables (year, state, and individual demographics: age, gender, White Black, Hispanic, and other race/ethnicity), retaining the same adjustment variables across all models, “Adjusted” columns in Table 3. Since states that adopted MMLs may have differed systematically from those that did not, “state” was an important adjustment variable in these analyses.
Table 3.
Unadjusted and adjusted odds ratios for adolescent past-30-day marijuana use and past-30-day heavy marijuana use by state medical marijuana law (MML) status/ provisions, 1991–2011 (N=715,014).
| Any Marijuana Use | Heavy Marijuana Use ≥20a | |||
|---|---|---|---|---|
| MML/Provision Status at the time of data year |
bUnadjusted OR (95%CI) |
cAdjusted OR (95%CI) |
bUnadjusted OR (95%CI) |
cAdjusted OR (95%CI) |
| Medical Marijuana Law - General | ||||
| Any MML | 1.08*** | 0.93* | 1.12*** | 1.00 |
| 12 states (n=102,124) | (1.03–1.13) | (0.86–0.99) | (1.05–1.21) | (0.89–1.13) |
| Years since enacted | 1.01* | 0.99* | 1.01* | 0.99 |
| Range (0–11) | (1.00–1.02) | (0.98–0.999) | (1.00– 1.02) | (0.98– 1.01) |
| ≥4 years since enacted | 1.14*** | 0.98 | 1.19*** | 0.98 |
| 6 states (n=58,107) | (1.06– 1.22) | (0.90–1.07) | (1.08– 1.30) | (0.88– 1.09) |
| Medical Marijuana Law - Provisions | ||||
| Dispensary-related variables | ||||
| Any dispensaries allowed | 1.13 *** | 0.94 | 1.18*** | 1.03 |
| 9 states (n=75,913) | (1.07– 1.19) | (0.87– 1.03) | (1.09– 1.28) | (0.89– 1.19) |
| Any active dispensaries by 2011 | 1.16 ** | 0.90 | 1.26*** | 1.02 |
| 2 states (n=29,455) | (1.05– 1.29) | (0.78– 1.04) | (1.11– 1.45) | (0.84– 1.24) |
| Any for-profit dispensaries allowed | 1.10** | 0.94 | 1.15** | 1.07 |
| 4 states (n=28,619) | (1.03– 1.17) | (0.83– 1.06) | (1.04– 1.28) | (0.88– 1.30) |
| MML Dispensary Index Scored | 1.03** | 0.97 | 1.04* | 1.01 |
| Range (0–3) | (1.01– 1.06) | (0.94– 1.00) | (1.01– 1.08) | (0.95– 1.06) |
| MML Dispensary Index Score category (separate model for each individual score) | ||||
| MML Dispensary Index Score 1 | 0.99 | 0.92 | 1.03 | 0.99 |
| 4 states (n=28,245) | (0 .92– 1.06) | (0.82– 1.02) | (0.92– 1.16) | (0.84– 1.17) |
| MML Dispensary Index Score 2 | 1.37*** | 1.01 | 1.23*** | 0.86 |
| 3 states (n=18,127) | (1.28– 1.47) | (0.91– 1.12) | (1.09– 1.39) | (0.74– 1.01) |
| MML Dispensary Index Score 3 | 1.10* | 0.94 | 1.13* | 1.04 |
| 5 states (n=28,191) | (1.02– 1.19) | (0.84– 1.05) | (1.02– 1.27) | (0.87– 1.25) |
| Home Cultivation and Allowed Plant Limit | ||||
| Home cultivation allowed | 1.08** | 0.92 | 1.14*** | 0.97 |
| 10 states (n=98,168) | (1.03– 1.13) | (0.85– 1.00) | (1.06– 1.22) | (0.86– 1.11) |
| Number of plants limit | 1.01 | 1.04 | 1.01** | 1.02 |
| Range (0–16) | (1.01– 1.01) | (1.02– 1.06) | (1.00– 1.01) | (1.00– 1.05) |
| ≥10 plants allowed | 1.07 | 0.92 | 1.14* | 0.98 |
| 4 states (n=32,583) | (0.99– 1.14) | (0.82– 1.03) | (1.02–1.26) | (.83– 1.14) |
| Allowed Possession Amounts | ||||
| Number usable ounces limit | 1.05*** | 1.21*** | 1.04*** | 1.18 |
| Range (0–10) | (1.04– 1.05) | (1.09– 1.34) | (1.03– 1.04) | (0.99– 1.40) |
| ≥2.5 usable ounces limit | 1.08** | 0.92 | 1.15*** | 0.97 |
| 6 states (n=57,167) | (1.03– 1.14) | (0.84– 1.01) | (1.06– 1.25) | (0.85– 1.11) |
| Patient Registry Requirement | ||||
| Registration Voluntary | 1.27*** | 1.41*** | 1.31*** | 1.23** |
| 1 State (n=28,149) | (1.17– 1.37) | (1.28– 1.56) | (1.20– 1.43) | (1.08– 1.40) |
| Caregivers (All MML states allow caregivers to supply patients with medical marijuana) | ||||
| Number of patients limit per caregiver | 1.02** | 0.98 | 1.03*** | 1.00 |
| Range (0–5) | (1.01– 1.03) | (0 .97– 1.00) | (1.01– 1.05) | (0.97– 1.02) |
| 5 patients per caregiver allowed | 1.07* | 0.91 | 1.14** | 0.97 |
| 6 states (n=50,777) | (1.01– 1.15) | (0.82– 1.01) | (1.04– 1.26) | (0 .83– 1.13) |
| MML Provision Index Variables | ||||
| Provision Index Scoree | 1.02*** | 0.98* | 1.04*** | 1.00 |
| Range (0–5) | (1.01– 1.04) | (0.96– 0.998) | (1.02– 1.06) | (0.96– 1.03) |
| Provision Index Score (separate model for each individual score) | ||||
| Provision Index Score 1 | 1.10*** | 1.04 | 1.06 | 1.07 |
| 3 states (n=27,260) | (1.04– 1.16) | (0.94– 1.14) | (0.98– 1.16) | (0.93– 1.23) |
| Provision Index Score 2 | 0.98 | 0.92 | 0.95 | 1.07 |
| 2 states (n=10,527) | (0.89– 1.08) | (0.79– 1.07) | (0.82– 1.09) | (0.84– 1.36) |
| Provision Index Score 3 | 1.47*** | 1.03 | 1.33* | 0.86 |
| 1 state (n=2,299) | (1.26– 1.72) | (0.88– 1.19) | (1.04– 1.69) | (0.67–1.11) |
| Provision Index Score 4 | 1.09* | 0.92 | 1.16** | 0.97 |
| 5 states (n= 34,477) | (1.01– 1.17) | (0.83– 1.02) | (1.04– 1.29) | (0.84– 1.13) |
| Provision Index Score 5 | 1.17*** | 0.90 | 1.28*** | 1.02 |
| 1 state (n=24,923) | (1.07– 1.28) | (0.78– 1.03) | (1.15– 1.42) | (0.84– 1.25) |
Each row shows the unadjusted and adjusted model results for each independent variable with the two dependent variables in the columns. Stata 13 MP “svyset” survey data settings were used to assign YRBS design variables: [sampling units: 'psu' and strata 'stratum'] as provided by all state YRBS datasets to account for their sampling procedures.
Each cell shows the result of a separate logistic regression analysis. Control groups included: (1) all states without MMLs in any of the years of data collection (Medical Marijuana Law – General analyses) and (2) states without MMLs in any of the years of data collection combined with states with MMLs that did not have the specific provision assessed in each model (Medical Marijuana Law – Provisions analyses).
MML does not include policies permitting high concentration Cannabidiol products for medicinal purposes.
Estimates are weighted using YRBS weights [*p ≤.05, **p≤.01, ***p≤.001].
Heavy marijuana use coded “1” if adolescent reported use 20≤ times in past-30-days
Unadjusted, bivariate models.
Adjusted for: year fixed effects, state fixed effects, and individual demographics: age, gender, White, Black, Hispanic, and other.
Dispensary Index Score range 0–3: Analyzed as an ordinal variable, and as separate dichotomous variables (one for each individual score 1–3). Categories: 0=States with no MMLs; 1=State has MML, but dispensaries not allowed, 2=Dispensaries allowed, 3=Dispensaries allowed and either active in 2011 and/or for-profit dispensaries allowed
Provision Index Score range 0–5: Analyzed as an ordinal variable, and as separate dichotomous variables, one for each individual score 1–5; [0=States with no MMLs; 1=Home cultivation and/or caregivers allowed; 2–5=Enumeration of state MMLs inclusion of more liberalized provisions in addition to home cultivation and caregivers: (a) Dispensaries for profit OR dispensaries active in 2011, (b) Home cultivation ≥10 plants allowed, (c) Possession: ≥2.5usable ounces allowed, (d) Caregivers allowed 5 patients, and (e) Patient registry voluntary].
In all models assessing “general” MML variables, the control group included all states without MMLs and states that eventually enacted an MML after 2011 but had not yet enacted an MML in any of the years of data collection. In all models assessing “provisions” MML variables, the control group additionally included states with MMLs that did not have the provision assessed in the specific model.
3. RESULTS
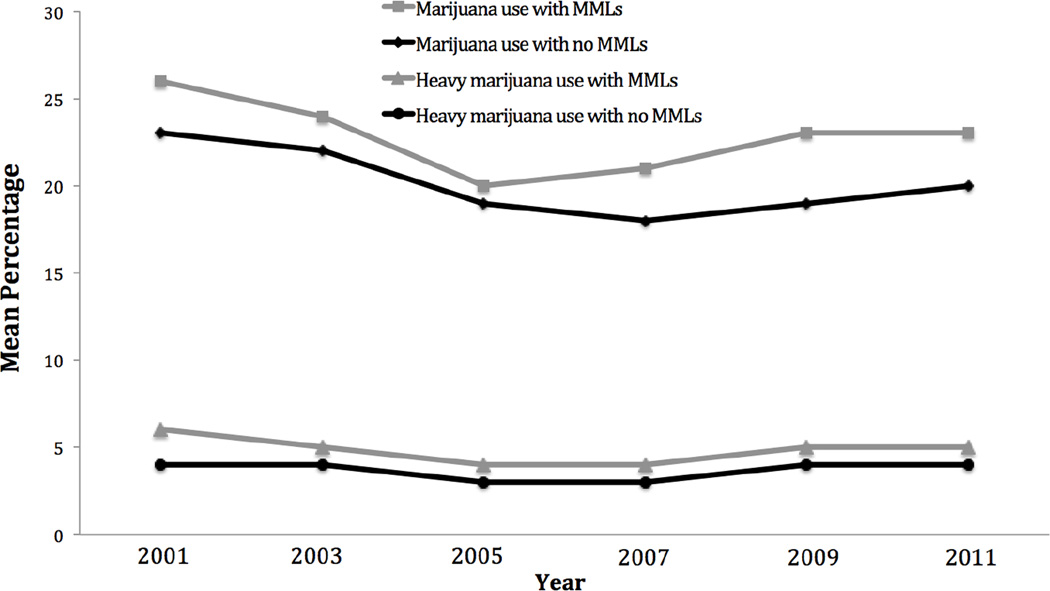
The overall prevalence of adolescent past-30-day marijuana use across all study years was 22.7% among adolescents residing in MML states compared to 19.8% in non-MML states (unadjusted OR 1.08, [95% CI= 1.03, 1.13]). Past-30-day heavy marijuana use rates were 7.0% vs. 5.6%, respectively (unadjusted OR 1.12, [95% CI=1.05, 1.21]). Figure 1 presents the unadjusted mean values for past-30-day use and heavy use of marijuana in states with and without MMLs from 2001–2011. Table 3 presents unadjusted and adjusted odds ratios and 95% confidence intervals for past-30-day use and heavy use of marijuana for all analyses. After adjustment for state, year, and adolescent demographics, there was a small but significant decreased odds of any marijuana use (OR 0.93, [95% CI= 0.86, 0.99]), and no difference in odds of heavy marijuana use (OR 1.00, [95% CI= 0.89, 1.13]), for adolescents living in MML states vs. non-MML states. It was inclusion of the state fixed effects that resulted in the changes in direction and significance of the MML effect seen between the unadjusted and adjusted models.
Figure 1.
Trends in unadjusted prevalence rates of adolescent past-30-day marijuana and heavy marijuana use by state medical marijuana law (MML) status, 2001–2011.
With regard to the effects of MML provisions assessed, the number of usable ounces allowed for possession and having a voluntary patient registration were the only two MML provision variables that showed positive and significant associations in the adjusted models. The odds of reporting past-30-day marijuana use were higher (adjusted OR 1.21, [95% CI= 1.09, 1.34]) for adolescents residing in MML states that allowed more ounces of usable medical marijuana possession vs. states that did not have MML or had MML with lower possession limits. The odds of reporting past-30-day marijuana use (adjusted OR 1.41, [95% CI= 1.28, 1.56]) and heavy marijuana use (adjusted OR 1.23, [95% CI= 1.08, 1.40]) were higher for adolescents residing in MML states where the MML patient registration was voluntary vs. states that did not have MML or had a mandatory registration. Conversely, years since MML was enacted showed a negative and significant association for adolescent report of past-30-day marijuana use (adjusted OR 0.99, [95% CI= 0.98, 0.999]).
The ten other provision variables assessed did not show significance in the adjusted models. Eight showed positive and significant unadjusted associations with adolescent past-30-day marijuana and heavy marijuana use, and two others showed positive and significant associations for past-30-day heavy marijuana use, with effects disappearing in adjusted models.
In regards to the index variables, having a higher score on the provision index variable (indicating more liberalized provisions) showed lowered odds of past-30-day marijuana use (adjusted OR 0.98, [95% CI= 0.96, 0.998]). The dispensary index as a continuous variable as well as all individual scores assessed as dichotomous variables on the provisions index did not show significance in any of the adjusted models.
4. DISCUSSION
This study utilizing repeated, cross-sectional YRBS data collected from 45 states between 1991 to 2011 found that adolescents living in states with legalized medical marijuana tended to have higher past-30-day marijuana use and heavy marijuana use (≥20 times in past 30 days) rates compared to those living in non-MML states. However, we found no evidence during this study period of an increase in adolescent past-30-day marijuana use or heavy marijuana use after enactment of a MML. Interestingly, enactment of an MML appeared to be associated with a slightly lower odds of adolescent marijuana use in this dataset, after adjustment for state and year effects. Our results suggest that the state in which adolescents lived is likely the more powerful predictor of their marijuana use than passage of a MML.
To our knowledge, this is one of the only studies to date that assessed the effects of specific MML provisions separately, the varying degree of liberalization of MML provisions, or examined the effect of MMLs on heavy marijuana use among adolescents.
Only two provisions showed positive and significant relationships with marijuana use in the adjusted models. These were: higher limits on the usable ounces allowed for medical marijuana possession, and voluntary patient registration. Higher usable marijuana possession limits were positive and significant for past-30-day marijuana use, and voluntary patient registration was positive and significant for past-30-day marijuana use and past-30-day heavy marijuana use. Similar to the findings for overall MML status, we found that while all the other MML provisions examined were positively associated with adolescent marijuana use in the unadjusted analyses, none showed significance after adjusting for state and year effects.
It is important to note that although a voluntary patient registry showed a positive and significant association in our analyses, only one state in the sample had this provision. Of the twenty-five current states with MMLs, only three states have a voluntary patient registration (Maine, California, and Washington), while the remaining twenty-two states have a mandatory patient registration. More research is needed to understand the effects of this provision.
These results are consistent with the most recent literature that also examined MMLs using large national datasets and found no increase in adolescent marijuana use rates with MML passage (Anderson et al., 2014; Choo et al., 2014; Harper et al., 2012; Hasin et al., 2015; Lynne-Landsman et al., 2013; Pacula et al., 2013; Wall et al., 2016; Wen et al., 2015). Our finding that adolescent marijuana use rates were higher in MML states in unadjusted analysis is similar to that of two studies that did not control for state and year effects and reported increased rates of adolescent marijuana use in MML states (Wall et al., 2011). On the other hand, other studies that controlled for state and year effects also showed no effect of MML passage on adolescent marijuana use rates. The most comprehensive study thus far used survey data from another large school-based surveillance system (Monitoring the Future) and found that marijuana use was more prevalent in states that passed MMLs, but the risk of marijuana use did not differ significantly after the MMLs were enacted (Hasin et al., 2015). Combined, these studies suggest that the states that passed MMLs had unobserved characteristics that are predictive of higher marijuana use among adolescents, even without an MML. For example, states with more accepting social norms surrounding marijuana use may both have higher use rates and be more likely to enact an MML.
Five studies published between 2012 and 2014 also used YRBS samples to examine the relationship between adolescent marijuana use and MMLs. They too report no difference in marijuana use after MML enactment. However, there are key differences among these studies and the current study. Two studies combined data from the national YRBS sample and state-specific samples for years 1993–2011 to include sub-samples from the national samples to cover 49 states, but were only able to access state samples from 35 states (Anderson et al., 2014, 2012). Another study only included 8 states that had pre-and-post MML enactment using state YRBS samples (Anderson et al., 2014). The third study also used YRBS state samples and compared pre to post MML data from four states with MML enactment from 2003–2009 (Montana, Rhode Island, Michigan, and Delaware; Lynn-Landsman et al., 2013). Because of access limitations, the fourth study was only able to use aggregated state-level YRBS data rather than individual level data, which would have allowed for the control of individual characteristics (Pacula et al., 2013). The fifth study used state-level YRBS data from ten states and paired five states with MMLs to five states in geographic proximity without MMLs. Three of the five comparison states without MMLs at the time of analyses later adopted similar laws (Choo et al., 2014). Our sample includes: (1) individual-level data from 45 states and (2) spans an extended period of time (1991–2011).
A strength of this study is the treatment of MMLs as heterogeneous policies with varying provisions and degree of liberalization within provisions across MMLs. Two recent studies also created MML provision indices (Bestrashniy and Winters, 2015; Chapman et al, 2016). Chapman et al. created indices on three analytical domains: initiation, quantity, and distribution and Bestrashniy and Winters on: permissiveness of cultivation, permissiveness of possession, and overall restrictiveness. Our first index focused exclusively on the dispensary provision, whereas the second overall liberality index was more similar to these previous studies, which calculated a score 0–5 based on the enumeration of the specific provision categories assessed. This research is in its nascent stage and it is imperative that future research continues to assess the heterogeneity of MMLs and differences within provisions in regards to adolescent use, access, price, and social acceptability.
This study had a number of potential limitations. This study relied on YRBS data, which are derived from adolescent samples limited to those in school, and the majority in public high schools. Thus, while weighting was applied to yield more population-representative samples, results may not be generalizable to adolescents not attending public schools. In addition, data relied on self-report, which may be subject to recall error and social desirability bias. The YRBS samples are cross-sectional, and changes in the composition of the study population over time could have contributed to the trends in marijuana use over time. The analysis attempted to address this potential confounding by adjusting for student demographic characteristics. Additionally, YRBS data weighting procedures are intended to yield representative samples that could be compared across years.
There were also gaps in available data across states and years. The YRBS did not have weighted state-level data for California, Oregon, and Washington and only had post-enactment data for Colorado and Vermont, five important MML states with relatively early MML enactment. Preliminary sensitivity analyses on states with post-enactment data only (Colorado and Vermont) showed that their inclusion did not significantly change results; thus, they were kept in the final analyses. Additionally, eight states in the control group enacted MMLs after our study period (Connecticut and Massachusetts in 2012; Illinois and New Hampshire in 2013; New York and Maryland in 2014; and Pennsylvania and Ohio in 2016). These states may have had marijuana use rates and social norms surrounding marijuana that are closer to those of states that had already enacted MML during study years, resulting in their eventually legalizing medical marijuana. This would be consistent with what the current literature has shown: states that enacted MMLs already had higher rates of marijuana use before MML enactment (Hasin et al., 2015). Additionally, this study is not able to examine the pre-post effects of state MMLs enacted before 2001, which include California that passed its MML in 1996, and Washington and Oregon, which passed their MMLs in 1998. Earlier MML adopter states and MML provisions may differ systematically from the later MML adopter states and MMLs assessed in this study; thus, these results are not generalizable to all states with MMLs, especially states that enacted MMLs previous to 1998.
Finally, the MML variables constructed were based on year of enactment, not full implementation, in order to have sufficient years of available data for analysis. Many MMLs were enacted but not fully implemented by 2011 (e.g., Colorado had legalized medical marijuana in 2001 but did not have active dispensaries until 2010); thus, the effects of MMLs on adolescent marijuana use may be lagged and this study may not have had sufficient years of data to detect an effect. Moreover, only two states had data post-implementation of active medical marijuana dispensaries during the study period (2011 data from Colorado and Maine), making it difficult to assess the effect of such dispensaries in this study. Adding in more years of YRBS data will allow future studies to better examine the effects of this provision. It will be important to assess the degree of liberalization among varying MML dispensary provisions, including the number of dispensaries allowed to operate per geographic area and proximity to schools.
Using data through 2011, this study found little evidence for an increase in past-30-day marijuana use, or past-30-day heavy marijuana use, among adolescents in response to state-enacted MMLs, regardless of most provisions, consistent with findings from other recent studies. However, this study found positive and significant associations between: (1) MMLs allowing for higher limits on the number of usable ounces of medical marijuana possession and past-30-day marijuana use and (2) voluntary patient registration and past-30-day marijuana use and past-30-day heavy marijuana use. The heterogeneity of MML provisions combined with amendments to policies over time create additional complexities in our understanding of how these provisions affect marijuana use as well as necessitate the need for continued surveillance. Additional research is needed to assess: (1) the effects of these MMLs as they evolve and as more states enact and implement similar MMLs, including provisions that could theoretically increase access to diverted marijuana within the state, (2) differential effects by adolescent age (e.g., do the effects of MMLs differ for younger vs. older adolescents), and (3) how MMLs affect other substance use behaviors (e.g., tobacco, alcohol, and prescription drug use).
Highlights.
Crude current marijuana and heavy marijuana use rates higher in medical marijuana law (MML) states.
Decreased odds of current marijuana use with MMLs with state fixed effects.
Decreased odds of current marijuana use with years since MML enactment.
Increased odds of current marijuana use with higher possession limits.
Increased odds of current marijuana use with a voluntary patient registration.
Acknowledgments
The lead author would like to acknowledge: Peter Kreiner, PhD, Rosalie Pacula, PhD for their advisement at varying points during this study.
Role of funding source
This research was supported by Grant 5F31DA036923-02 from the National Institute on Drug Abuse (PI: Johnson) and partially supported by Grant T32AA007567 from the National Institute on Alcohol Abuse and Alcoholism (PI: Constance Horgan; Sharon Reif). This article is the sole responsibility of the authors and does not reflect the views of either the National Institute on Drug Abuse (NIDA) or the National Institute on Alcohol Abuse and Alcoholism (NIAAA).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributors
All of the authors contributed to the study conception and design, interpretation of findings, and manuscript preparation and revision. Julie K. Johnson originated the study, conducted the statistical analyses and drafted the manuscript. Sion Harris advised on the conception and design, statistical analysis, interpretation of findings and reviewed drafts of the manuscript. Dominic Hodgkin advised on the statistical analysis, interpretation of findings and reviewed drafts of the manuscript.
Financial disclosure
No financial disclosure to report.
Submission declaration and verification
This manuscript has not been published in any other journal or place, is not under consideration for publication in any other journal, and will not be sent out to any journal while under consideration for publication with Drug and Alcohol Dependence.
Human Participant Protection statement
This was a secondary analysis of existing, public use, state-level data from 45 states participating in the Youth Risk Behavior Survey (YRBS) and complies with the HIPAA Privacy Rule.
Conflict of interest statement
No conflicts of interest to report.
REFERENCES
- American College of Pediatricians. Marijuana Use: Detrimental to Youth. [accessed 09.14.16];2016 https://www.acpeds.org/marijuana-use-detrimental-to-youth. [Google Scholar]
- Anderson MD, Hansen B, Rees DI. NBER Working Paper Series. Cambridge, MA 02138: 1050 Massachusetts Avenue; 2014. Anderson Medical Marijuana Laws And Teen Marijuana Use; pp. 1–17. http://econpapers.repec.org/paper/nbrnberwo/20332.htm. [Google Scholar]
- Anderson MD, Hansen B, Reese DI. Discussion Paper Series No. 6592. Germany: Institute for the Study of Labor; 2012. [accessed 09.24.16]. Medical Marijauna Laws and Teen Marijuana Use. http://ftp.iza.org/dp6592.pdf. [Google Scholar]
- Belenko SR. Westport, CT: Greenwood Press; 2000. Drugs And Drug Policy In America: A Documentary History. https://www.ncjrs.gov/App/Publications/abstract.aspx?ID=185050. [Google Scholar]
- Bestrashniy J, Winters KC. Variability in medical marijuana laws in the United States. Psychol. Addict. Behav. 2015;29:639–642. doi: 10.1037/adb0000111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bilz GA. The medical use of marijuana: the politics of medicine. Hamline J. Public Law Policy. 1992;117:130. http://heinonline.org/HOL/LandingPage?handle=hein.journals/hplp13&div=10&id=&page=. [Google Scholar]
- Camchong J, Lim K, Kumra S. Adverse effects of cannabis on adolescent brain development: a longitudinal study. Cereb. Cortex. 2016 doi: 10.1093/cercor/bhw015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC. Methodology of the youth risk behavior surveillance system. In: Moolenaar RL, Casey CG, Rutledge TF, editors. Atlanta, GA: MMWR CDC; 2013. pp. 1–25. http://www.cdc.gov/mmwr/pdf/rr/rr6201.pdf. [Google Scholar]
- Chapman SA, Spetz J, Lin J, Chan K, Schmidt LA. Capturing heterogeneity in medical marijuana policies: a taxonomy of regulatory regimes across the United States. Subst. Use Misuse. 2016;51:1174–1184. doi: 10.3109/10826084.2016.1160932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Choo EK, Benz M, Zaller N, Warren O, Rising K, Carlin JB, Degenhardt L. The impact of state medical marijuana legislation on adolescent marijuana use. J. Adolesc. Health. 2014;55:160–166. doi: 10.1016/j.jadohealth.2014.02.018. http://dx.doi.org/10.1016/j.jadohealth.2014.02.018. [DOI] [PubMed] [Google Scholar]
- Hall W, Degenhardt L. Adverse health effects of non-medical cannabis use. Lancet. 2009;374:1383–1391. doi: 10.1016/S0140-6736(09)61037-0. http://dx.doi.org/10.1016/S0140-6736(09)61037-0. [DOI] [PubMed] [Google Scholar]
- Harper S, Strumpf Erin C, Kaufman Jay S. Do medical marijuana laws increase marijuana use? Replication study and extension. Ann. Epidemiol. 2012;22:207–212. doi: 10.1016/j.annepidem.2011.12.002. http://dx.doi.org/10.1016/j.annepidem.2011.12.002. [DOI] [PubMed] [Google Scholar]
- Hasin DS, Wall M, Keyes KM, Cerdá M, Schulenberg J, O’Malley PM, Galea S, Pacula R, Feng T. Medical marijuana laws and adolescent marijuana use in the USA from 1991 to 2014: results from annual, repeated cross-sectional surveys. Lancet Psychiatry. 2015;601–608 doi: 10.1016/S2215-0366(15)00217-5. http://dx.doi.org/10.1016/S2215-0366(15)00217-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jager G, Ramsey N. Long-term consequences of adolescent cannabis exposure on the development of cognition, brain structure and function: an overview of animal and human research. Curr. Drug Abuse Rev. 2008;1:114–123. doi: 10.2174/1874473710801020114. http://www.eurekaselect.com/92609/article. [DOI] [PubMed] [Google Scholar]
- Johnston LD, O'Malley PM, Miech RA, Bachman JG, Schulenberg JE. Monitoring The Future: National Survey Results On Drug Use 1975–2014. Ann Arbor: The University of Michigan Institute for Social Research; 2014. pp. 1–98. http://www.monitoringthefuture.org/pubs/monographs/mtf-overview2014.pdf. [Google Scholar]
- Johnston LD, O'Malley PM, Miech RA, Bachman JG, Schulenberg JE. Monitoring The Future: National Survey Results on Drug Use 1975–2015. Ann Arbor: The University of Michigan Institute for Social Research; 2015. 2015 Overview: Key Findings on Adolescent Drug Use. http://www.monitoringthefuture.org/pubs/monographs/mtfoverview2015.pdf. [Google Scholar]
- Keyes KM, Wall M, Cerdá M, Schulenberg J, O'Malley PM, Galea S, Feng T, Hasin DS. How does state marijuana policy affect US youth? Medical marijuana laws, marijuana use and perceived harmfulness: 1991–2014. Addiction. 2016 doi: 10.1111/add.13523. 10.1111/add.13523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynne-Landsman SD, Livingston MD, Wagenaar AC. Effects of state medical marijuana laws on adolescent marijuana use. Am. J. Public Health. 2013;103:1500–1506. doi: 10.2105/AJPH.2012.301117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacula R, Powell D, Heaton P, Sevigny E. NBER Working Paper Series. Cambridge, MA: National Bureau of Economic Research; 2013. Assessing The Effects of Medical Marijuana Laws on Marijuana and Alcohol Use: The Devil Is In The Details; pp. 1–42. http://www.nber.org/papers/w19302. [Google Scholar]
- Pacula RL, Chriqui JF, Reichmann DA, Terry-McElrat YM. State medical marijuana laws: understanding the laws and their limitations. J. Public Health Policy. 2002;23:413–439. http://link.springer.com/article/10.2307/3343240. [PubMed] [Google Scholar]
- Schweinsburg AD, Brown SA, Tapert SF. The influence of marijuana use on neurocognitive functioning in adolescents. Curr. Drug Abuse Rev. 2008;1:99–111. doi: 10.2174/1874473710801010099. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC2825218/ [DOI] [PMC free article] [PubMed] [Google Scholar]
- Squeglia LM, Gray KM. Alcohol and drug use and the developing brain. Curr. Psychiatry Rep. 2016;18 doi: 10.1007/s11920-016-0689-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stack P, Suddath C. A brief history of medical marijuana. [accessed 09.24.16];TIME. 2009 http://content.time.com/time/health/article/0,8599,1931247,00.html. [Google Scholar]
- Stolzenberg L, D’Alessio SJ, Dariano D. The effect of medical cannabis laws on juvenile cannabis use. Int. J. Drug Policy doi. 2016;27:82–88. doi: 10.1016/j.drugpo.2015.05.018. 10.1016/j.drugpo.2015.05.018. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Swanson JM, Evins E, DeLisi LE, Meier MH, Gonzalez R, Bloomfield M, Curran V, Baler R. Effects of cannabis use on human behavior, including cognition, motivation, and psychosis: a review. JAMA Psychiatry. 2016;73:292–297. doi: 10.1001/jamapsychiatry.2015.3278. [DOI] [PubMed] [Google Scholar]
- Wall MM, Mauro C, Hasin DH, Keyes KM, Cerda M, Martins SS, Feng T. Prevalence of marijuana use does not differentially increase among youth after states pass medical marijuana laws: commentary on and reanalysis of US National Survey on Drug Use in Households data 2002–2011. Int. J. Drug Policy. 2016;29:9–13. doi: 10.1016/j.drugpo.2016.01.015. http://dx.doi.org/10.1016/j.drugpo.2016.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wall MM, Poh E, Cerdá M, Keyes KM, Galea S, Hasin DS. Adolescent marijuana use from 2002 to 2008: higher in states with medical marijuana laws, cause still unclear. Ann. Epidemiol. 2011;21:714–716. doi: 10.1016/j.annepidem.2011.06.001. http://dx.doi.org/10.1016/j.annepidem.2011.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen H, Hockenberry JM, Cummings JR. The effect of medical marijuana laws on adolescent and adult use of marijuana, alcohol, and other substances. J. Health Econ. 2015;42:64–80. doi: 10.1016/j.jhealeco.2015.03.007. http://dx.doi.org/10.1016/j.jhealeco.2015.03.007. [DOI] [PubMed] [Google Scholar]