Abstract
Purpose
The aim of this work was to determine dose distributions for high-energy brachytherapy sources at spatial locations not included in the radial dose function gL(r) and 2D anisotropy function F(r,θ) table entries for radial distance r and polar angle θ. The objectives of this study are as follows: 1) to evaluate interpolation methods in order to accurately derive gL(r) and F(r,θ) from the reported data; 2) to determine the minimum number of entries in gL(r) and F(r,θ) that allow reproduction of dose distributions with sufficient accuracy.
Material and methods
Four high-energy photon-emitting brachytherapy sources were studied: 60Co model Co0.A86, 137Cs model CSM-3, 192Ir model Ir2.A85-2, and 169Yb hypothetical model. The mesh used for r was: 0.25, 0.5, 0.75, 1, 1.5, 2–8 (integer steps) and 10 cm. Four different angular steps were evaluated for F(r,θ): 1°, 2°, 5° and 10°. Linear-linear and logarithmic-linear interpolation was evaluated for gL(r). Linear-linear interpolation was used to obtain F(r,θ) with resolution of 0.05 cm and 1°. Results were compared with values obtained from the Monte Carlo (MC) calculations for the four sources with the same grid.
Results
Linear interpolation of g L(r) provided differences ≤ 0.5% compared to MC for all four sources. Bilinear interpolation of F(r,θ) using 1° and 2° angular steps resulted in agreement ≤ 0.5% with MC for 60Co, 192Ir, and 169Yb, while 137Cs agreement was ≤ 1.5% for θ < 15°.
Conclusions
The radial mesh studied was adequate for interpolating gL(r) for high-energy brachytherapy sources, and was similar to commonly found examples in the published literature. For F(r,θ) close to the source longitudinal-axis, polar angle step sizes of 1°-2° were sufficient to provide 2% accuracy for all sources.
Keywords: brachytherapy, dosimetry, TG-43, interpolation, radial dose function, 2D anisotropy function
Purpose
Treatment planning systems (TPS) used in brachytherapy, employ the American Association of Physicists in Medicine (AAPM) Task Group No. 43 Report (TG-43) formalism [1, 2] in which the radial dose function gL(r) and 2D anisotropy function F(r,θ) are introduced in the form of single and double entry tables, respectively, using a specific mesh for each parameter. Current TPS require dose calculation in a clinical implant using higher spatial resolution of radial distance r and polar angle θ than the entered parameter data, i.e., gL(r) and F(r,θ). Therefore, TPS must interpolate gL(r) and F(r,θ) values from data tables.
A review of the published data for various brachytherapy sources indicated that different authors used a variety of spatial and angular increments and ranges in their reporting. Therefore, a standardized methodology for interpolation from the published data may be required to determine the dose rate distributions at spatial locations not explicitly included in the published data. The AAPM TG-43U1 [2] report provided guidelines for interpolation from 2D and 1D dosimetry parameters for the case of low energy sources of 125I and 103Pd. The supplement to 2004 TG-43 report (i.e., TG-43U1S1) [3] included further clarification and modifications of the interpolation techniques in order to assemble these procedures as more accurate and user-friendly.
The TG-43U1 and TG-43U1S1 reports recommended log-linear interpolation for gL(r) and linear-linear interpolation for F(r,θ). An accuracy of ± 2% was required for establishing r and θ resolution, interpolation techniques and fitting procedures. The TG-43U1S1 indicated that these interpolation techniques may be extended to other brachytherapy sources in general. Polynomial fits are usually included, although tri-exponential fits and other fitting functions recently have been explored with very good agreement for all sources [4–9].
The TG-43 formalism has also been extended for high-energy sources of 60Co, 137Cs, 192Ir and 169Yb [10]. However, given the contradictory behaviour of gL(r) and F(r,θ) between low-energy and high-energy brachytherapy sources due to photon interactions, it is quite interesting to determine whether the TG-43U1 and TG-43U1S1 recommendations on interpolation and extrapolation for low-energy sources are applicable to high-energy sources [11, 12]. Therefore, the objectives of this study are: 1) to check what interpolation method allows accurate acquisition of gL(r) and F(r,θ) from the published data; 2) to determine the minimum number of entries in gL(r) and F(r,θ) that allow reproduction of dose distributions with sufficient accuracy.
Material and methods
Four high-energy photon-emitting brachytherapy sources were studied in the present work: (1) 60Co source from BEBIG (model Co0.A86) [13]; (2) 137Cs source from BEBIG (model CSM-3) [14]; (3) 192Ir source from BEBIG (model Ir2.A85-2) [15]; and (4) a hypothetical 169Yb source having the same design as 192Ir Flexisource from Isodose Control [16], but with central core composed of 169Yb. These sources represents the typical high-energy sources in shape and material composition. All four sources had active lengths L = 0.35 cm with the exception of 137Cs source that had an equivalent active length (number of seeds times separation between sources) of L = 1.8 cm [17].
For these sources, we used the Monte Carlo (MC) raw data, (r,θ), in a mesh of 0.5 mm from 0 to 10 cm in θ = 1° steps obtained in previous publications [13–15], and performed equivalent simulations for 169Yb theoretical source. The gL(r) and F(r,θ) brachytherapy dosimetry parameters were derived using this dense mesh. Detailed description of the MC study of 60Co, 137Cs and 192Ir sources can be found in respective publications. The study for 169Yb source has been performed with the same methodology as for the other. A summary of methodology employed is presented below:
Geant4 toolkit was used [18].
Cross-section libraries based on EPDL97 [19].
Radiation spectra was adopted from the National Nuclear Data Center (NNDC) [20].
Water- and air-kerma per photon history were scored using linear track-length estimator of energy deposition.
Each source was placed at the centre of a spherical water phantom with radius R = 40 cm, except for 60Co where the radius used was 50 cm. Kerma estimation in water used spherical voxels that were arranged every 0.05 cm in 1° steps.
Source materials considered were assumed from the corresponding publication of each source.
Water and air composition and conditions were recommended by the TG-43U1.
Photons were generated uniformly and distributed within the active source core.
The quantity of simulated photon histories was sufficient enough to assure good statistical uncertainties (see each publication for additional details).
Published gL(r) and F(r,θ) tables for high-energy sources used a radial mesh for r that typically includes a combination of 0.25, 0.5, 0.75, 1, 1.5, 2-8 (integer steps) and 10 cm. Some authors may add supplementary data points for r < 10 cm [21, 22] or at larger distances such as r = 12 cm or r = 15 cm [13–16]. In case of F(r,θ), the typical spatial resolution for θ is 0°-5° (in 1° steps), 5°-10° (in 2° steps), 10°-30° (in 5° steps), 30°-90° (in 10° steps) with the same possibility of supplementary angles. In some studies of high-energy sources, lower angular resolutions were used such as 10° near the source longitudinal-axis [21, 22]. For the four sources examined, the published gL(r) and F(r,θ) tables used the typical mesh as previously indicated. The TG-43U1 and TG-43U1S1 interpolation recommendations were examined in this context. Furthermore, linear-linear interpolation of gL(r) was examined. Results were compared with the values obtained from the MC calculations for the aforementioned sources with the same grid.
Results
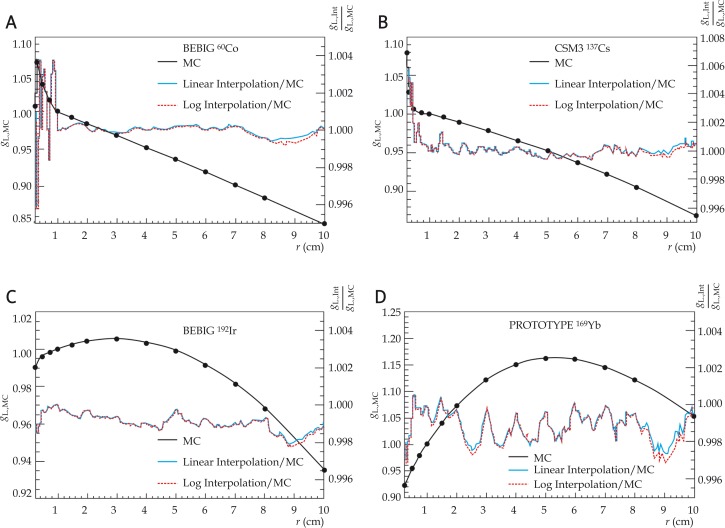
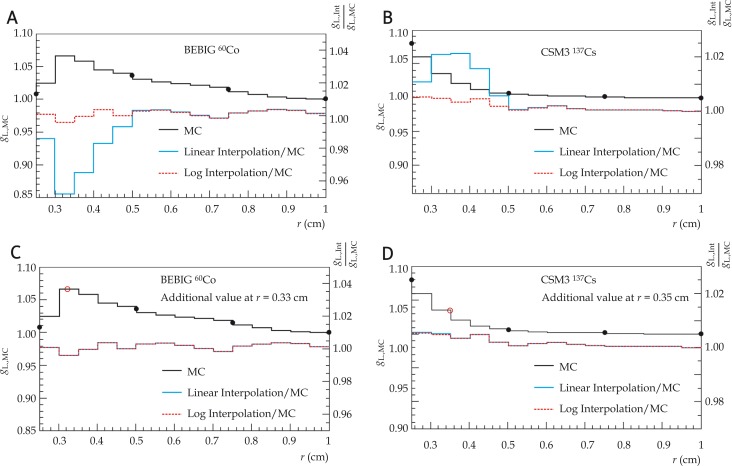
Results for linear-linear interpolation and logarithmic-linear interpolation did not differ significantly for gL(r) as shown in Fig. 1. For 192Ir and 162Yb sources, interpolation differences were ≤ 0.5% compared with MC results over the entire radial range 0.25 ≤ r ≤ 10 cm. For 60Co and 137Cs sources, differences between MC and interpolation results were > 2% for 0.25 < r < 0.5 cm and ≤ 0.5% elsewhere. Dissimilarities between MC and interpolation results reduced to ≤ 0.5% upon addition of gL(r = 0.33 cm) and gL(r = 0.35 cm) for 60Co and 137Cs, respectively, to account for gL(r) maximum in the case of 60Co, and the high gL(r) gradient in the case of 137Cs (Fig. 2). Due to small (< 0.5%) rounding errors in the published data, the gL,Int.(r)/gL,MC(r) ratio is not equal to unity at radii corresponding to the tabulated data points. There were no substantial differences between the linear-linear and log-linear interpolations for the four sources examined.
Fig. 1.
Radial dose function gL(r) for the four sources studied (left scale) and ratio of interpolated gL(r) to MC raw data (right scale). Full black lines represent MC results in a mesh of 0.5 mm from 0 to 10 cm. Closed circles represent the same MC results but for the radial mesh typically used in published tables. The mesh points used for interpolation are shown as closed circles
Fig. 2.
Radial dose fuction gL(r) for the two sources studied in the radial range up to 1 cm (left) and with two additional points (right)
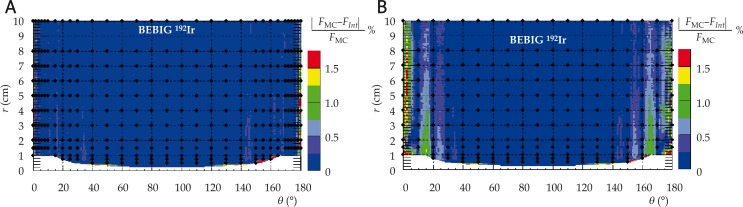
The results for F(r,θ) are shown in Table 1, with graphical representation for 192Ir source shown in Fig. 3. For the four sources and four approximations in case of F(r,θ), differences with MC were ≤ 0.5% in the radial range up to 10 cm when using 1° and 2° polar angle steps, with the exception of 137Cs where differences were ≤ 1.5% for θ < 15°. With 5° polar angle steps, differences for 60Co, 137Cs, 192Ir, and 169Yb sources were ≤ 0.5%, ≤ 1.5% for θ < 15°, ≤ 0.5%, and ≤ 2% for θ < 5°, respectively. With 10° polar angle steps, dissimilarities for 60Co, 137Cs, 192Ir, and 169Yb sources were ≤ 1.5% for θ < 5°, ≤ 2% for θ < 10°, ≤ 1.5% for θ < 25°, ≤ 2% for θ < 10°.
Table 1.
Differences of linear-linear interpolated F(r,θ) values compared to MC results
| θ step | 60Co | 137Cs | 192Ir | 169Yb |
|---|---|---|---|---|
| 1°-2° | ≤ 0.5% | ≤ 1.5% (θ < 15°) ≤ 0.5% (θ > 15°) |
≤ 0.5% | ≤ 0.5% |
| 5° | ≤ 0.5% | ≤1.5% (θ < 15°) ≤ 0.5% (θ > 15°) |
≤ 0.5% | ≤ 2 % (θ < 5°) ≤ 0.5% (θ > 5°) |
| 10° | ≤ 1.5% (θ < 5°) ≤ 0.5% (θ> 5°) |
≤ 2% (θ< 10°) ≤ 0.5% (θ > 10°) |
≤ 1.5% (θ < 25°) ≤ 0.5% (θ > 25°) |
≤ 2% (θ < 10°) ≤ 0.5% (θ > 10°) |
Fig. 3.
Comparison between interpolated (Fint) and MC (FMC) 2D anisotropy function results for the BEBIG 192Ir source for two different angular resolutions: a) 2° increments and b) 10° increments. The mesh points (closed circles) used for interpolation are shown. The region inside the source capsule is shown in white near r = 0 and is not clinically relevant
Discussion
If dosimetric information is required (i.e., desire to evaluate organ-at-risk dose) for r > 10 cm, physicists should refer to the original MC publications. However, radiation scatter conditions and the water equivalence of tissues may need to be considered for accurate dose estimation [23].
In contrast with dosimetry parameter interpolation for low-energy brachytherapy sources, extrapolation to r ≤ rrmin for high-energy sources is complicated by the lack of electronic equilibrium and the assumption that collisional kerma is equal to absorbed dose over the entire radial range. Significant issues that are generally not included in most publications on high-energy brachytherapy source dosimetry are the presence of electronic disequilibrium near the source and the contributions from emitted electrons [24]. Consequently, no extrapolation method can predict the behaviour of data without obtaining the physical basis in order to understanding the effect.
Conclusions
In contrast to the established standards (TG-43U1S1) for low-energy sources which recommends log-linear interpolation for gL(r), linear-linear or log-linear interpolation methods, produced nearly the same results for high-energy sources. For gL(r) and for sources analysed in this study, the typical mesh used in the literature was adequate for linear-linear or log-linear interpolations of 192Ir and 169Yb sources. For 60Co and 137Cs, the mesh was also adequate for gL(r), however an additional gL(r) point for 0.25 < r < 0.5 cm was included to keep minimize interpolation errors to < 0.5%. For F(r,θ) close to longitudinal axis source (i.e., θ < 15°), 1°-2° polar angle steps were adequate for all 4 sources examined.
Acknowledgments
This study was supported in part by the Generalitat Valenciana (Project GVEMP06/015), Ministerio de Educación y Ciencia (Spain) Projects No. FIS2004-05713, DPI2004-04268-C02-01 and FPA2003-07581-C02-01, and by FEDER. M.C. Pujades-Claumarchirant was supported by Fundación FIVO (Valencia, Spain).
References
- 1.Nath R, Anderson LL, Luxton G, et al. Dosimetry of interstitial brachytherapy sources: Recommendations of the AAPM Radiation Therapy Committee Task Group No. 43. Med Phys. 1995;22:209–234. doi: 10.1118/1.597458. [DOI] [PubMed] [Google Scholar]
- 2.Rivard MJ, Coursey BM, DeWerd LA, et al. Update of AAPM Task Group No. 43 Report: A revised AAPM protocol for brachytherapy dose calculation. Med Phys. 2004;31:633–674. doi: 10.1118/1.1646040. [DOI] [PubMed] [Google Scholar]
- 3.Rivard MJ, Butler WM, DeWerd LA, et al. Supplement to the 2004 update of the AAPM Task Group No. 43 Report. Med Phys. 2007;34:2187–2205. doi: 10.1118/1.2736790. [DOI] [PubMed] [Google Scholar]
- 4.Wu X, Brezovich IA, Fiveash JB. Bi- and tri-exponential fitting to TG-43 radial dose functions of brachytherapy sources based on a genetic algorithm. Brachytherapy. 2009;8:361–366. doi: 10.1016/j.brachy.2008.11.005. [DOI] [PubMed] [Google Scholar]
- 5.Taylor RPE, Rogers DWO. More accurate fitting of 125I and 103Pd radial dose functions. Med Phys. 2008;35:4242–4250. doi: 10.1118/1.2964097. [DOI] [PubMed] [Google Scholar]
- 6.Furhang EE, Wallace RE. Fitting and benchmarking of dosimetry data for new brachytherapy sources. Med Phys. 2000;27:2302–2306. doi: 10.1118/1.1308278. [DOI] [PubMed] [Google Scholar]
- 7.Fung AY. Comment on ‘‘Functional fitting of interstitial brachytherapy dosimetry data recommended by the AAPM Radiation Therapy Committee Task Group 43’’[Med Phys 1999; 26: 153-160] and ‘‘Fitting and benchmarking of dosimetry data for new brachytherapy sources’’[Med Phys 2000; 27: 2302-2306] Med Phys. 2007;28:400. doi: 10.1118/1.1350680. [DOI] [PubMed] [Google Scholar]
- 8.Lliso F, Perez-Calatayud J, Carmona V, et al. Fitted dosimetric parameters of high dose-rate 192Ir sources according to the AAPM TG43 formalism. Med Phys. 2001;28:654–660. doi: 10.1118/1.1359438. [DOI] [PubMed] [Google Scholar]
- 9.Lliso F, Perez-Calatayud J, Carmona V, et al. Technical note: Fitted dosimetric parameters of high dose-rate 192Ir sources according to the AAPM TG43 formalism. Med Phys. 2003;30:651–654. doi: 10.1118/1.1561621. [DOI] [PubMed] [Google Scholar]
- 10.Li Z, Das R K, DeWerd L A, et al. Dosimetric prerequisites for routine clinical use of photon emitting brachytherapy sources with average energy higher than 50 keV. Med Phys. 2007;34:37–40. doi: 10.1118/1.2388155. [DOI] [PubMed] [Google Scholar]
- 11.Sakelliou L, Sakellariou K, Sarigiannis K, et al. Dose rate distributions around 60Co, 137Cs, 198Au, 192Ir, 241Am, 125I (models 6702 and 6711) brachytherapy sources and the nuclide 99Tcm. Phys Med Biol. 1992;37:1859–1872. doi: 10.1088/0031-9155/37/10/004. [DOI] [PubMed] [Google Scholar]
- 12.Mainegra E, Capote R, López E. Radial dose functions for 103Pd, 125I, 192Ir and 169Yb brachytherapy sources: an EGS4 Monte Carlo study. Phys Med Biol. 2000;45:703–717. doi: 10.1088/0031-9155/45/3/309. [DOI] [PubMed] [Google Scholar]
- 13.Granero D, Perez-Calatayud J, Ballester F. Technical note: Dosimetric study of a new Co-60 source used in brachytherapy. Med Phys. 2007;34:3485–3488. doi: 10.1118/1.2759602. [DOI] [PubMed] [Google Scholar]
- 14.Perez-Calatayud J, Granero D, Casal E, et al. Monte Carlo and experimental derivation of TG-43 dosimetric parameters for CSM-type Cs-137 sources. Med Phys. 2005:28–36. doi: 10.1118/1.1834835. [DOI] [PubMed] [Google Scholar]
- 15.Granero D, Perez-Calatayud J, Ballester F. Monte Carlo study of the dose rate distributions for the Ir2.A85-2 and Ir2.A85-1 Ir-192 afterloading sources. Med Phys. 2008;35:1280–1287. doi: 10.1118/1.2868766. [DOI] [PubMed] [Google Scholar]
- 16.Granero D, Perez-Calatayud J, Casal E, et al. A dosimetric study on the Ir-192 HDR Flexisource. Med Phys. 2006;33:4578–4582. doi: 10.1118/1.2388154. [DOI] [PubMed] [Google Scholar]
- 17.Williamson JF. Monte Carlo and analytic calculation of absorbed dose near 137Cs intracavitary sources. Int J Radiat Oncol Biol Phys. 1988;15:227–237. doi: 10.1016/0360-3016(88)90372-0. [DOI] [PubMed] [Google Scholar]
- 18.Agostinelli S, Allison J, Amako K, et al. GEANT4 – a Simulation Toolkit. Nuc Ins Meth. 2003;A506:250–303. See also http://geant4.web.cern.ch/geant4 last accessed 14 February 2010. [Google Scholar]
- 19.Cullen DE, Hubbell JH, Kissel L. EPDL97: The Evaluated Photon Data Library, ’97 Version. Lawrence Livermore National Laboratory report UCRL-50400 1997. 6 Revision 5. [Google Scholar]
- 20.NUDAT 2.5, National Nuclear Data Center, Brookhaven National Laboratory. http://www.nndc.bnl.gov/nudat2/ last accessed 14 February 2010.
- 21.Medich DC, Munro JJ. Monte Carlo characterization of the M-19 high dose rate Iridium-192 brachytherapy source. Med Phys. 2007;34:1999–2006. doi: 10.1118/1.2733809. [DOI] [PubMed] [Google Scholar]
- 22.Medich DC, Tries MA, Munro JJ. Monte Carlo characterization of an Ytterbium-169 high dose rate brachytherapy source with analysis of statical uncertainty. Med Phys. 2006;33:163–172. doi: 10.1118/1.2147767. [DOI] [PubMed] [Google Scholar]
- 23.Rivard MJ, Venselaar JLM, Beaulieu L. The evolution of brachytherapy treatment planning systems. Med Phys. 2009;36:2136–2153. doi: 10.1118/1.3125136. [DOI] [PubMed] [Google Scholar]
- 24.Ballester F, Granero D, Perez-Calatayud J, et al. Evaluation of high-energy brachytherapy source electronic disequilibrium and dose from emitted electrons. Med Phys. 2009;36:4250–4256. doi: 10.1118/1.3194754. [DOI] [PubMed] [Google Scholar]