Abstract
Systemic rheumatoid vasculitis (SRV) can develop in rheumatoid arthritis of long duration and high disease activity. It most commonly manifests as cutaneous vasculitis and mononeuritis multiplex. This can involve any organ of the body and carries very high mortality. We report a case of a young male who had rheumatoid arthritis for the past 15 years and became refractory to standard drugs and anti-TNF agents. He subsequently developed SRV, which started as mononeuritis multiplex. Disease progressed to result in gangrene of hands and feet despite receiving intravenous cyclophosphamide. Intravenous immunoglobulin and rituximab also could not provide any response. Prolonged ICU stay resulted in critical care neuromyopathy. Central nervous system vasculitis developed even after repeated infusions of intravenous immunoglobulins and at last he died of complications. In this case report, we have presented rare and chronic protracted presentation of rheumatoid vasculitis involving skin, nerves, brain and testis, which was refractory to the recommended therapies.
Keywords: malignant rheumatoid arthritis, rheumatoid arthritis, rheumatoid vasculitis, systemic rheumatoid vasculitis
Introduction
In rheumatoid arthritis (RA), 40% patients develop extra-articular manifestations (EAM). These include rheumatoid nodules, sicca syndrome, episcleritis, low bone mineral density, anaemia, pleuritis, interstitial lung disease, pulmonary nodules, Felty's syndrome, glomerulonephritis, pericarditis and atherosclerosis. Systemic rheumatoid vasculitis (SRV) is the most serious of all EAM and carries a 5-year mortality of ~40% [1]. Clinically, prevalence of SRV is 1–5% in cases of RA, whereas autopsy studies have reported it between 15% and 31% [2]. The most common manifestation of SRV is cutaneous vasculitis followed by progressive sensorimotor neuropathy and mononeuritis multiplex [3]. This case had severe SRV affecting skin, nerves, brain and testis. Our report illustrates the potentially devastating consequences of this rare manifestation of RA.
Case Report
A 48-year-old male was diagnosed as seropositive RA according to 1987 ACR criteria [4] 15 years ago and had been treated with conventional disease modifying anti-rheumatic drugs (DMARDs). He took methotrexate 15 mg once per week, hydroxychloroquine 200 mg daily and sulphasalazine 2000 mg daily for the initial 10 years of disease along with intermittent courses of steroids for disease flares. His disease became more active 5 years ago and tab leflunomide 20 mg daily was added to the treatment regimen. Nailfold vasculitis or subcutaneous nodules were absent. Compliance to the medications was good. Serum rheumatoid factor and anti-cyclic citrullinated peptide (anti-CCP) were positive in high titres. He did not have any other medical illness or comorbid condition. He was not on any medication other than DMARDs. He had no addiction to recreational drugs or alcohol, but used to smoke 2–3 cigarettes daily. Two years ago, his disease became refractory to DMARDs and 50 mg etanercept injection was started. Due to lack of efficacy, etanercept was discontinued after 3 months. Abatacept was started which provided inadequate and temporary effect and hence stopped after 6 months. He started developing severe neuropathic pain in both hands and feet and nerve conduction velocity (NCV) study showed mononeuritis multiplex. Sural nerve biopsy reported vasculitic neuropathy. SRV was considered and monthly intravenous cyclophosphamide (CYC) pulses of 1000 mg were administered for 6 months. There was a transient benefit lasting 6 months but again the neuropathic pain recurred. Pain was excruciating and did not control with any pain modulatory drug or conventional NSAIDS. For further management, he was referred to our rheumatology department.
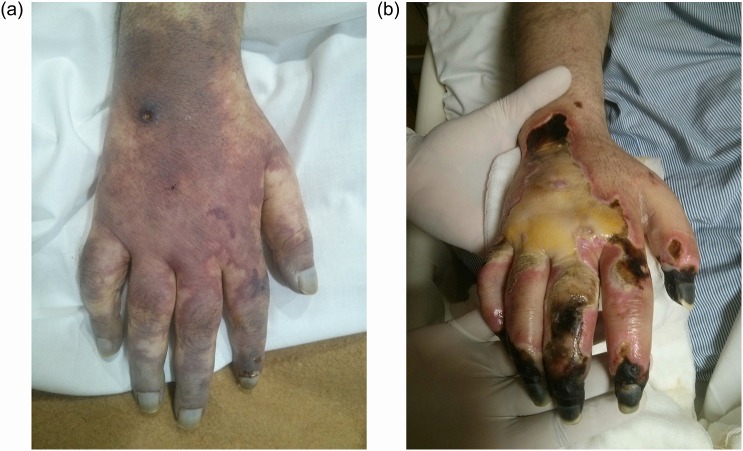
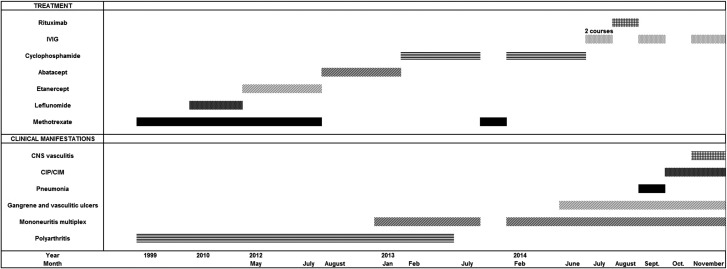
On presentation at our centre, he had mild deformity of metacarpophalangeal joints of both hands without clinical synovitis. There were no subcutaneous rheumatoid nodules. Dysaesthesia was present over dorsum of both feet without muscular weakness. Lungs were not involved clinically. He was taking oral steroids, methotrexate, pregabalin and nortriptyline. Relevant investigations showed haemoglobin 11.2 gm/dl, total leucocyte counts 26 400, serum albumin 2.1 g/dl, erythrocyte sedimentation rate (ESR) 60 mm and C-reactive protein (CRP) 127 mg/l. Titre of rheumatoid factor in serum was 5700 units/ml and titre of anti-CCP was more than 500 units/ml. Blood sugar, creatine phosphokinase (CPK) and vitamin B12 were in normal range. Hepatitis B surface antigen, cryoglobulins, anti-nuclear antibodies (ANA) and anti-neutrophil cytoplasmic antibodies (ANCA) were negative. Serum total testosterone level was very low (110 ng/dl). Diagnosis of SRV was confirmed employing the Scott and Bacon criteria [5]. In view of history of good response to CYC, a second course of monthly intravenous CYC 1000 mg was started. He continued to have episodes of severe neuropathic pain in hands, which was refractory to drugs like tramadol, pregabalin, nortryptiline, ketamine infusions and acupuncture. He was also suffering from major depression and his only complaint was severe pain in limbs. Functional component was suspected to be dominating over actual disease due to lack of objective findings. Multiple sessions of psychotherapy and antidepressants were administered but in vain. After 5 months of CYC infusions, he developed foot drop and repeat NCV study confirmed the progression of mononeuritis multiplex. Gangrene of tip of toes and vasculitic ulcers over legs developed, which progressed rapidly. In view of severe disease, CYC was abandoned and intravenous immunoglobulin (IVIG) in full dose was given. After 1 month, gangrene of toes and legs extended further with involvement of both hands (Figs 1 and 2). As a next therapeutic option, an infusion of rituximab 1000 mg was administered. After a week, he developed severe pneumonia and was admitted in ICU. There he had a prolonged stay and became ventilator dependent due to critical illness polyneuromyopathy. Interestingly, due to quadriplegia his serum creatinine remained around 0.2 mg/dl despite a body weight of 120 kg. He developed multiple episodes of status epilepticus and was refractory to several anti-epileptics. During seizures, only facial muscles were contracting; all other muscles of the body remained flaccid and inactive. CT brain showed right thalamic haemorrhage with multiple cerebral and cerebellar infarcts due to cerebral vasculitis. For this, fourth course of IVIG was administered as he had received rituximab recently and no other immunosuppressant was favoured in the critically ill patient due to risk of severe immunosuppression, risk of severe infection and long latent period of most immunosuppressive medications. Figure 3 charts the clinical course of the patient. Unfortunately, in spite of IVIG he did not regain consciousness and finally succumbed to his illness after 68 days of stay in ICU.
Figure 1:
(a) Gangrene of dorsum of hand. (b) Gangrene seen in (a) progressing despite CYC pulses.
Figure 2:

Gangrene of foot.
Figure 3:
Clinical course of the patient with SRV. CIP/CIM, critical illness polyneuropathy and myopathy.
Discussion
Rheumatoid vasculitis typically occurs in patients who are male, smoker, have erosions, subcutaneous nodules and have long-standing course of more than 10 years duration [6]. Elevated ESR, CRP, anaemia, high levels of immune complexes, high-titre RF, hypocomplementemia, circulating cryoglobulins, elevated alkaline phosphatase and leucocytosis are associated with it [7]. Most of the predisposing factors were present in this patient. There has been a significant decrease in the incidence of SRV in the last few decades because of the availability of better treatment strategies like treat to target approach and use of methotrexate as a first-line agent. Use of biological drugs in severe and refractory disease resulted in more effective disease control [8]. Our patient had refractory SRV, which continued to progress despite treatment with biological drugs, CYC and IVIG. Studies showed that the morbidity and mortality of SRV remains high and has not improved since last decade, despite the use of CYC [8].
The most common manifestation of SRV is cutaneous vasculitis followed by neurologic involvement. Arthritis remained inactive in this patient. This is consistent with the reports in the literature that synovitis is usually quiescent when SRV presents. Cerebral vasculitis is a serious and rare complication of RA. It can manifest as ischaemic stroke, haemorrhages, headache, seizures, cranial nerve palsies, pachymeningitis and encephalopathy [9]. This patient had severe CNS involvement in the form of haemorrhage, infarct, encephalopathy and seizures. This manifestation was progressive despite CYC, rituximab and IVIG, which is the treatment of choice in severe or refractory disease [10]. However, our patient did not benefit from any treatment.
SRV is defined using the Scott and Bacon criterion, i.e. the presence of one of the following features in a patient with RA: mononeuritis multiplex, peripheral gangrene, acute necrotizing arteritis or deep cutaneous ulcers. Other causes of such lesions must be excluded [5].
It may be confused with polyarteritis nodosa (PAN) due to similar clinical features, and therefore it is sometimes called secondary PAN. Pathologically both PAN and SRV are similar in that both involve small and medium-sized arteries by immune complex deposition. Although fever, weight loss, mononeuritis multiplex, CNS involvement, orchitis and peripheral gangrene are common manifestations of both the diseases, lack of hypertension, rising serum creatinine, abdominal catastrophes like haemorrhage, pancreatitis and perforation differs it from PAN. Moreover, arteriography in PAN shows typical aneurysms in medium-sized arteries, whereas SRV has high-titre RF and anti-CCP antibodies in serum. Vasculitis is never the initial presenting manifestation when it occurs in RA and is thus readily diagnosed by features of the parent illness.
Anti-TNF therapy has been implicated in the causation of SRV and there are >200 cases of suspected anti-TNF-induced vasculitis reported in the literature [11]. Prolonged treatment with anti-TNF therapy can lead to the development of autoantibodies mainly ANA, anti–double-stranded DNA, ANCA and anticardiolipin antibodies in up to 10% of patients. This can lead to development of lupus, cutaneous leukocytoclastic vasculitis, interstitial lung disease and ANCA-associated vasculitis. Drug-induced vasculitis is suspected as the cause of vasculitis when vasculitis is temporally related to the use of the offending drug, vasculitis regresses on withdrawing the drug, serum ANCA become positive, primary disease remain quiescent and other causes of vasculitis are excluded. Our patient did not have any of the association and vasculitis progressed even after etanercept being discontinued a long ago. Serum ANCA also remained negative. Therefore, anti-TNF therapy was unlikely to be the factor causing SRV in this case.
Serum creatinine is derived from muscle mass and undergoes renal excretion at a constant rate. Its level is affected by renal function and low level is found in females, muscle wasting or paralysis, diet low in proteins and hyperthyroidism [12]. Our patient had a fall in serum creatinine from baseline value of 0.8 mg/dl to 0.2 mg/dl due to prolonged immobilization.
CIP/CIM is a frequent complication of critical illness affecting the motor and sensory nerves, neuromuscular junctions and muscles. This disorder can cause severe muscular weakness and prolongs weaning, compromises rehabilitation, increases hospital stay and increases mortality rates. Serum CPK remains and electromyography (EMG)/NCV tests are helpful in detecting this condition though muscle biopsy remains the gold standard. About 70% of patients with systemic inflammatory response syndrome, 100% of patients with multiple organ failure and 49–77% of patients staying in the ICU for at least 7 days develop CIP/CIM [13]. In the situation of repeated sepsis, severe rheumatoid vasculitis and prolonged stay in ICU, this patient developed severe CIP/CIM.
Malignant rheumatoid vasculitis is a serious and rare complication of RA, which can involve different organs causing ischaemia and infarction in various organs. It is common in long-standing and deforming RA. This patient developed SRV that progressed from mononeuritis multiplex to severe cerebral vasculitis in a 2-year duration. His disease was refractory to IVIG and biological treatment resulting in fatal outcome.
Ethical Approval
Ethical approval from institutional ethical committee has been taken before submitting this article.
Consent
Consent from the parents of the deceased patient has been taken for this case report.
Guarantor
Ashok Kumar as corresponding author agrees to be guarantor for the accuracy of final manuscript and submission of this article.
CONFLICT OF INTEREST STATEMENT
None declared.
References
- 1.Turesson C, O'Fallon WM, Crowson CS, Gabriel SE, Matteson EL. Occurrence of extraarticular disease manifestations is associated with excess mortality in a community based cohort of patients with rheumatoid arthritis. J Rheumatol 2002;29:62–7. [PubMed] [Google Scholar]
- 2.Genta MS, Genta RM, Gabay C. Systemic rheumatoid vasculitis: a review. Semin Arthritis Rheum 2006;36:88–98. [DOI] [PubMed] [Google Scholar]
- 3.Puéchal X, Said G, Hilliquin P, Coste J, Job-Deslandre C, Lacroix C, et al. Peripheral neuropathy with necrotizing vasculitis in rheumatoid arthritis. A clinicopathologic and prognostic study of thirty-two patients. Arthritis Rheum 1995;38:1618–29. [DOI] [PubMed] [Google Scholar]
- 4.Arnett FC, Edworthy SM, Bloch DA, McShane DJ, Fries JF, Cooper NS, et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum 1988;31:315–24. [DOI] [PubMed] [Google Scholar]
- 5.Scott DGI, Bacon PA. Intravenous cyclophosphamide plus methylprednisolone in the treatment of systemic rheumatoid vasculitis. Am J Med 1984;76:377–84. [DOI] [PubMed] [Google Scholar]
- 6.Voskuyl AE, Zwinderman AH, Westedt ML, Vandenbroucke JP, Breedveld FC, Hazes JM. Factors associated with the development of vasculitis in rheumatoid arthritis: results of a case-control study. Ann Rheum Dis 1996;55:190–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Turesson C, Jacobsson LT. Epidemiology of extra-articular manifestations in rheumatoid arthritis. Scand J Rheumatol 2004;33:65–72. [DOI] [PubMed] [Google Scholar]
- 8.Ntatsaki E, Mooney J, Scott DG, Watts RA. Systemic rheumatoid vasculitis in the era of modern immunosuppressive therapy. Rheumatology (Oxford) 2014;53:145–52. [DOI] [PubMed] [Google Scholar]
- 9.Zolcinski M, Bazan-Socha S, Zwolinska G, Musial J. Central nervous system involvement as a major manifestation of rheumatoid arthritis. Rheumatol Int 2008;28:281–3. [DOI] [PubMed] [Google Scholar]
- 10.Schwab I, Nimmerjahn F. Intravenous immunoglobulin therapy: how does IgG modulate the immune system. Nat Rev Immunol 2013;13:176–89. [DOI] [PubMed] [Google Scholar]
- 11.Ramos-Casals M, Brito-Zeron P, Muñoz S, Soria N, Galiana D, Bertolaccini L, et al. Autoimmune diseases induced by TNF-targeted therapies: analysis of 233 cases. Medicine (Baltimore) 2007;86:242–51. [DOI] [PubMed] [Google Scholar]
- 12.Hagemann P, Kahn SN. Significance of low concentrations of creatinine in serum from hospital patients. Clin Chem 1988;34:2311–2. [PubMed] [Google Scholar]
- 13.Hermans G, De Jonghe B, Bruyninckx F, Van den Berghe G. Clinical review: critical illness polyneuropathy and myopathy. Crit Care 2008;12:238. [DOI] [PMC free article] [PubMed] [Google Scholar]