Abstract
Teratomas are primary germ-cell tumours in the mediastinum. Although they are generally slow-growing and asymptomatic, rapid growth causing life-threatening complications can occur. Sebaceous secretion, insulin production, chorionic gonadotropin secretion and pancreatic enzyme secretion are the presumptive causes of tumour progression. Only few cases of rapidly growing teratomas have been reported previously. Here, we present a case of a giant mature teratoma in the mediastinum that presented with rapid growth and compare the characteristics of this case with those of previous cases.
INTRODUCTION
Teratomas are common primary germ-cell tumours in the mediastinum. As they are usually slow-growing and asymptomatic, they are often discovered incidentally on chest X-rays obtained for unrelated reasons [1]. Rapid growth of teratomas occurs in rare cases, most likely due to secretion of ectopic hormones and digestive enzymes, and can cause life-threatening complications [2–4]. When rapid growth is accompanied by symptoms, physicians should consider immediate surgical resection owing to the possibility of tumour rupture or acute infection [5]. Here, we describe a giant mature teratoma, which grew rapidly and required resection.
CASE REPORT
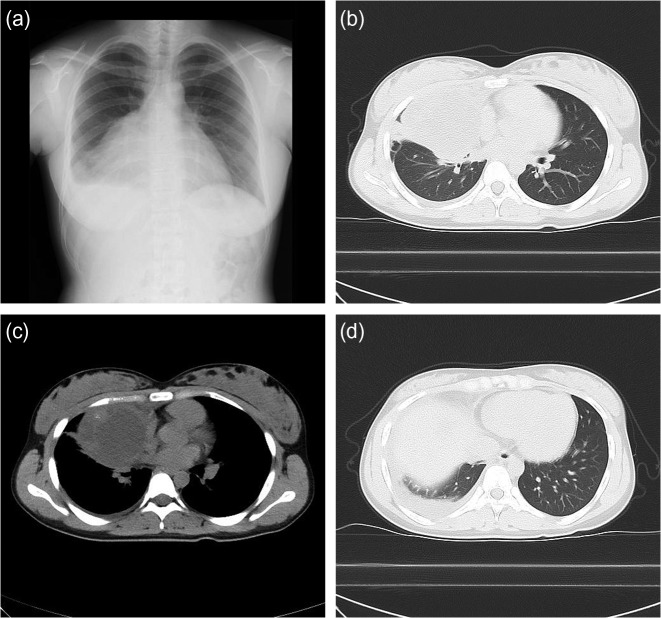
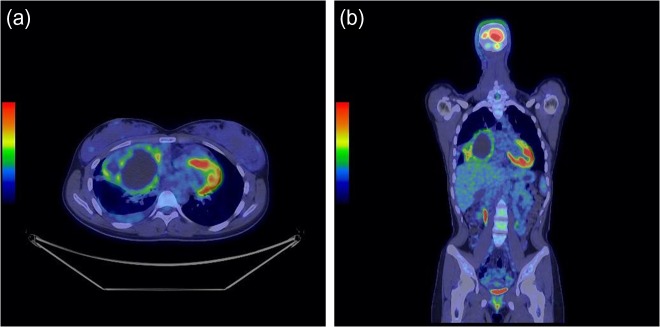
A 17-year-old female high-school student presented to our hospital owing to a dull feeling in the right thorax. She had no history of illness. A chest X-ray at the initial visit showed a large infiltration in the right lower thorax (Fig. 1a). Chest computed tomography (CT) revealed a large mass in the anterior mediastinal area with low-level pleural effusion (Fig. 1b–d), an internal fluid component and external parenchyma mixed with calcification. Serum tumour markers (carcinoembryonic antigen, cytokeratin 19 fragment, soluble interleukin-2 receptor, alpha-fetoprotein and human chorionic gonadotropin) were all negative. Positron emission tomography (PET)-CT (Fig. 2a and b) showed high uptake of fluorodeoxyglucose in the marginal area of the mass. A chest X-ray taken at a school physical examination 16 months earlier showed no obvious abnormal shadow (Fig. 3).
Figure 1:
Chest X-ray and CT at the initial visit. The chest X-ray showed a large infiltration in the right lower thorax (a). The CT scan showed a large mass with low-level pleural effusion, an internal fluid component and external parenchyma mixed with calcification in the anterior mediastinal area (b–d).
Figure 2:
PET-CT. A PET-CT scan revealed robust accumulation of fluorodeoxyglucose along with the entire circumference of the tumour (a and b).
Figure 3:
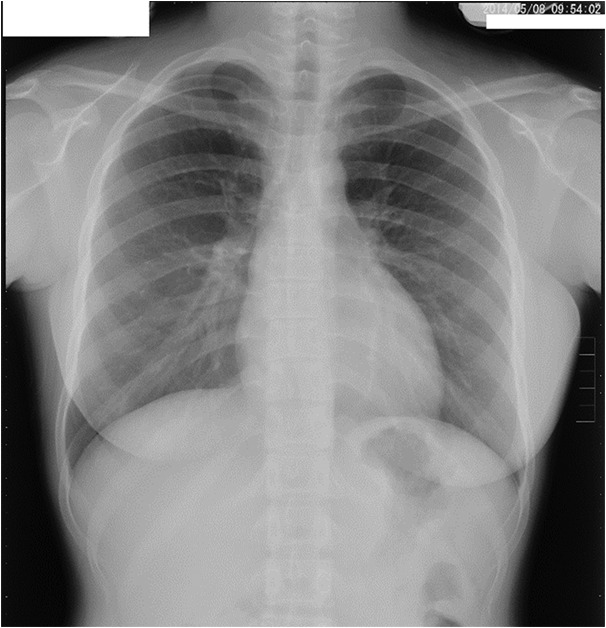
Chest X-ray 16 months before the initial visit. A chest X-ray from a school physical examination 16 months before the initial visit showed no obvious abnormal shadow.
A germ-cell tumour was suspected, and further pathological examinations were required. A week after the initial visit, we performed a CT-guided biopsy to determine whether the tumour was malignant or benign. The biopsy specimens showed no evidence of malignancy, but did not allow a detailed pathological diagnosis. Calcification, pleural effusion and the heterogeneous density of the tumour, along with the results of the CT-guided biopsy, strongly suggested rupture of the mature teratoma.
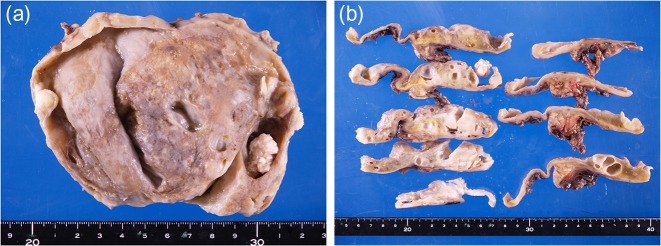
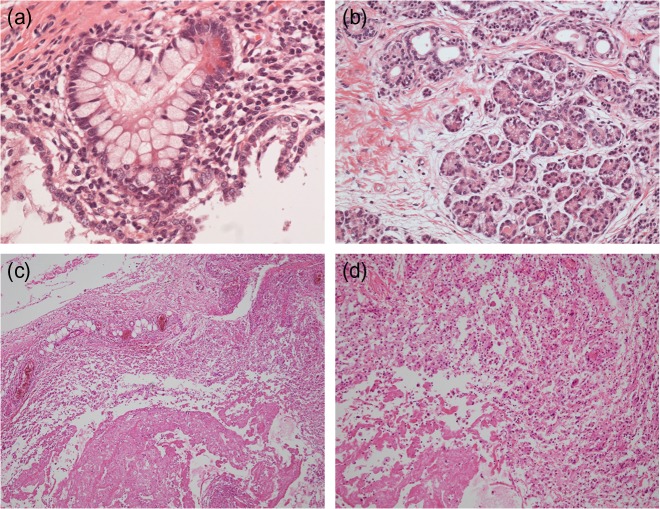
A week later, the patient was referred to a thoracic surgeon, and tumorectomy with median sternotomy was performed. The resected tumour had a multiloculated cyst-like structure with wall thickening (Fig. 4a and b). There was no evidence of tumour rupture. The pleural effusion contained mostly serous exudative fluid but no blood. Microscopically, the tumour consisted of ciliated columnar epithelium and mature squamous epithelium with sweat glands and sebaceous glands. Mucous-secreting glands and pancreatic tissue were also detected (Fig. 5a and b). These findings confirmed the diagnosis of a mature teratoma. The patient's post-surgical condition was good, and she was discharged from the hospital 1 week after surgery. A chest X-ray showed no mass in the mediastinum at a follow-up visit 1 month after surgery.
Figure 4:
Macroscopic findings of the resected tumour. The resected tumour had an uneven scarred surface with mild elastic sensing (a). The yellow areas represent mature fat. The divided surface of the tumour showed multilocular solid growth and wall thickening (b).
Figure 5:
Microscopic findings of the resected tumour. Histopathological analysis revealed a mixture of mucous-secreting glands (a) and pancreatic tissue (b). Haematoxylin and eosin stain, ×400. Inflammatory changes with lymphocytic infiltration were also detected (c and d). Haematoxylin and eosin stain, (c) ×100 and (d) ×200.
DISCUSSION
Teratoma is the third-most common mediastinal tumour. Most teratomas are mature teratomas, which typically occur in female patients in their 20s and 30s [6]. In more than 50% of cases, mature teratomas have no symptoms at initial diagnosis and are detected by chance [1]. When symptoms arise in patients with teratomas, rapid progression of the tumour should be suspected. Haemorrhage, infection and rupture are the major causes of progression [5]; additional causes include sebaceous secretion, insulin production, chorionic gonadotropin secretion and pancreatic enzyme secretion, whereas malignant transformation is very rare [7]. After rupture, the density of the teratoma is less likely to homogeneous than before; rather, each part of the tumour is heterogeneous [5].
Although many cases of mature teratoma of the mediastinum have been reported, only three described a rapidly growing mature teratoma (Table 1) [2–4]. In these reports, the patients with such tumours were all less than 30 years of age and were equally men and women. The growth rate of teratomas caused by hormone or enzyme secretion was determined monthly, whereas that of teratomas caused by bleeding was determined daily. Rupture or bleeding is likely to be the more life-threatening condition. We first suspected that the rapid growth of the tumour in the present case was due to rupture and bleeding; however, after surgical resection, there was no evidence of rupture. Therefore, the mechanism underlying the rapid growth of this tumour is unknown. Because we found inflammatory changes with lymphocyte infiltration in some area of resected tissue (Fig. 5c and d), exudative fluid in the right thorax and pancreatic tissue in the tumour, we speculate that pancreatic enzymes might partially affect inflammation in the tumour, resulting in its enlargement, as observed in a previous report [4].
Table 1:
Previous reports of patients with rapid growing mature teratoma
| Author | Patient age (years)/sex | Duration of progression | Symptom | Pathogenesis (presumption) | Reference |
|---|---|---|---|---|---|
| Hussain | 27/male | 5 days | Chest pain | Haemorrhage | [2] |
| Uyama | 12/female | 14 months | Chest pain | Oestrogen hormone | [3] |
| Omachi | 23/male | 4 months | Dyspnoea | Pancreatic enzyme | [4] |
| Present case | 17/female | 16 months | Chest discomfort | Pancreatic enzyme | – |
In summary, we presented a case of a rapid growing mature teratoma. Any mature teratoma in young patient has a potential risk of rapid progression on a monthly basis. We think it is an optimal time to surgical treatment for teratomas when they are detected.
ACKNOWLEDGEMENTS
We thank to Drs Osamu Kanai, Misato Okamura and Koichi Nakatani (Division of Respiratory Medicine, National Hospital Organization Kyoto Medical Center) for their helpful suggestions on patient management.
CONFLICT OF INTEREST STATEMENT
None declared.
EHICAL APPROVALT
Our institution does not require ethical approval for case reports. This submission was approved by the patient and her relatives.
CONSENT
We obtained written consent from the patient as well as from one of her parents because she was underage.
GUARANTOR
K.F. is the guarantor of this work.
REFERENCES
- 1.Lewis BD, Hurt RD, Payne WS, Farrow GM, Knapp RH, Muhm JR. Benign teratomas of the mediastinum. J Thorac Cardiovasc Surg 1983;86:727–31. [PubMed] [Google Scholar]
- 2.Hussain SA, Shenaq S, Mendoza L, Sundermeyer J, Chakarvarty S. Mediastinal teratoma presenting as a rapidly enlarging paracardial mass. Int Surg 1983;68:179–80. [PubMed] [Google Scholar]
- 3.Uyama T, Monden Y, Harada K, Kimura S, Morimoto T, Miura K, et al. Rapidly growing mature teratoma of the mediastinum: do sex hormones affect growth of the tumor. J Surg Oncol 1988;38:285–9. [DOI] [PubMed] [Google Scholar]
- 4.Omachi N, Kawaguchi T, Shimizu S, Okuma T, Kitaichi M, Atagi S, et al. Life-threatening and rapidly growing teratoma in the anterior mediastinum. Intern Med 2015;54:2487–9. [DOI] [PubMed] [Google Scholar]
- 5.Choi SJ, Lee JS, Song KS, Lim TH. Mediastinal teratoma: CT differentiation of ruptured and unruptured tumors. AJR Am J Roentgenol 1998;171:591–4. [DOI] [PubMed] [Google Scholar]
- 6.Travis WD, Brambilla E, Konrad Muller-Hermelink H, Harris Curtis C. Pathology and Genetics of Tumours of the Lung, Pleura, Thymus and Heart. Lyon: International Agency for Research on Cancer, 2004. [Google Scholar]
- 7.Harms D, Zahn S, Göbel U, Schneider DT. Pathology and molecular biology of teratomas in childhood and adolescence. Klin Padiatr 2006;218:296–302. [DOI] [PubMed] [Google Scholar]