Abstract
Thyrotoxicosis is most commonly caused by Graves’ disease, toxic multinodular goitre, a functioning thyroid adenoma, or thyroiditis. Extrinsic infiltrative conditions affecting the thyroid gland are typically destructive, and associated with thyroid hypofunction. We describe the case of a 61-year-old woman who presented to our hospital with symptoms of thyrotoxicosis, neck swelling and thyroid function tests consistent with hyperthyroidism. An ultrasound revealed a multinodular goitre with retrosternal extension, but CT imaging suggested thyroid gland infiltration, with cervical lymphadenopathy. An excisional lymph node biopsy confirmed the diagnosis of diffuse large B cell lymphoma causing infiltrative thyrotoxicosis. Treatment with six cycles of Rituximab-CHOP lead to rapid normalization of symptoms, imaging, and thyroid function.
Keywords: infiltrative thyrotoxicosis, lymphoma, hyperthyroidism
Introduction
Hyperthyroidism affects 0.1–0.5% of the population, and is most commonly caused by Graves’ disease, toxic multinodular goitre, functioning thyroid adenoma or thyroiditis. Infiltrative thyroid diseases are rarely associated with thyrotoxicosis, and are more commonly associated with thyroid gland destruction and hypothyroidism. We describe a case of thyroid gland infiltration by diffuse large B cell lymphoma (DLBCL) leading to presentation at our hospital with neck swelling and thyrotoxicosis. To our knowledge, this is the first reported case of infiltrative thyrotoxicosis caused by DLBCL.
Case Report
A 61-year-old woman was referred to this hospital with a 3-month history of palpitations and breathlessness. One week prior to presentation, she noticed mild neck swelling. Her medical history included hypertension, and a partial right nephrectomy for a benign lesion. Physical examination revealed only mild generalized neck swelling. Measurement of her thyroid hormone levels revealed an elevated free T4 at 22.3 pmol/L, and a low thyroid stimulating hormone (TSH) level at 0.05 mU/L. Three months prior to this presentation, normal thyroid function tests were recorded.
An ultrasound of thyroid revealed a multinodular goitre with retrosternal extension, and possible cystic cervical lymphadenopathy. A CT scan confirmed diffuse enlargement of the thyroid gland with bilateral cervical lymphadenopathy causing tracheal deviation, concerning for a thyroid gland malignancy.
A week after the CT scan, she presented acutely with progressive neck swelling and palpitations. The thyroid function tests remained abnormal, with a free T4 of 23.2 pmol/L, and a TSH of < 0.01 mU/L. Anti-thyroid peroxidase antibodies were negative, suggesting that a diagnosis of thyroiditis was less likely. She was commenced on carbimazole and propranolol to treat thyrotoxicosis.
An excisional biopsy of a cervical lymph node was arranged, which confirmed the diagnosis of diffuse large B cell non-Hodgkin lymphoma (DLBCL). Staging investigations—including a PET–CT scan—revealed a final stage of IIIAE.
Our patient commenced treatment with Rituximab-CHOP chemotherapy. The neck swelling and thyrotoxic symptoms resolved completely prior to cycle 2, and the carbimazole was discontinued. Serial thyroid function tests demonstrated a return to normal thyroid hormone levels after cycle 2. A PET–CT scan carried out upon completion of chemotherapy showed the complete resolution of pre-treatment abnormalities (Fig. 1). She remains in remission.
Figure 1:
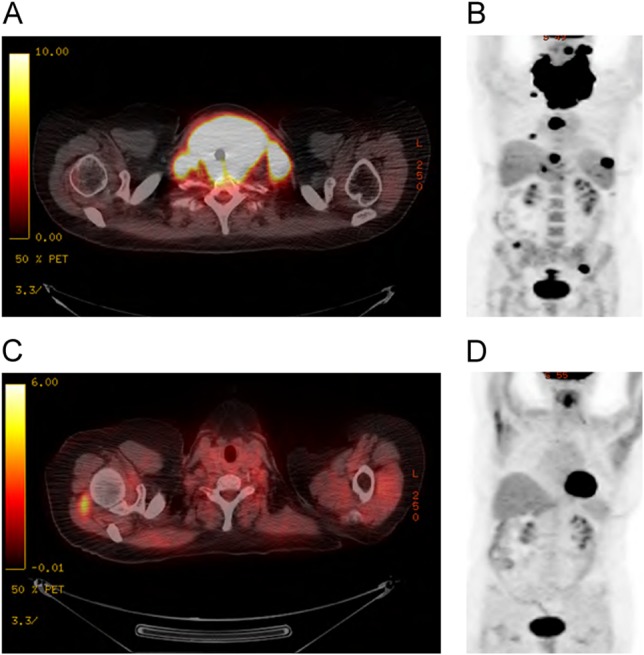
PET–CT imaging of DLBCL infiltration of the thyroid gland. PET–CT images before and after chemotherapy treatment. These demonstrate infiltration of the thyroid gland with cervical lymphadenopathy (A, B). Re-staging PET–CT images following six cycles of Rituximab-CHOP showing complete resolution of the abnormalities (C, D)
Discussion
Excluding thyroid cancer, we identified three infiltrative thyroid conditions in the literature related to this case: primary thyroid lymphoma (PTL), benign infiltration of the thyroid gland, and infiltration of the thyroid gland by metastatic cancer.
PTL is a well-recognized diagnosis. A population based study of 1,408 cases showed that DLBCL accounted for two thirds of all PTL cases, and follicular lymphoma was found in approximately one third. The effect of PTL on thyroid function was not documented [1]. A second case series of PTL including 119 patients showed that 41% had biochemical evidence of hypothyroidism, with no reported cases of hyperthyroidism [2]. In our case, the imaging and histology excluded the diagnosis of PTL.
Benign infiltrative thyrotoxicosis is also described. Kimura et al. reported 30 cases of amyloid goitre, or secondary amyloidosis affecting the thyroid gland. Six individuals were hypothyroid, while one individual was found to be hyperthyroid [3]. Cases of thyroid gland infiltration by sarcoidosis have been reported since the 1960s, and are typically associated with hyperthyroidism [4].
Infiltration of the thyroid gland by metastatic cancer most commonly involves renal cell cancer, lung cancer and head/neck cancer. While infiltrative thyroid diseases are primarily associated with thyroid gland hypofunction, we have identified two previous reported cases of malignant infiltrative thyrotoxicosis associated with lung adenocarcinoma [5] and pancreatic adenocarcinoma [6]. Together with our report, these cases highlight the fact that infiltrative thyrotoxicosis should be considered a potential, though rare, differential diagnosis in the setting of hyperthyroidism and thyroid gland enlargement, and emphasize the importance of tissue biopsy in such cases.
Conflict of Interest statement
No conflicts of interest.
Funding
This work (publication costs) was supported by the Department of Medical Oncology, University Hospital Limerick.
Ethical Approval
No ethical approval was required for this case report.
Consent
Written informed consent was obtained from the patient for publication.
Guarantor
Rajnish K. Gupta.
References
- 1.Graff-Baker A, Roman SA, Thomas DC, Udelsman R, Sosa JA. Prognosis of primary thyroid lymphoma: demographic, clinical, and pathologic predictors of survival in 1,408 cases. Surgery 2009;146:1105–15. [DOI] [PubMed] [Google Scholar]
- 2.Matsuzuka F, Miyauchi A, Katayama S, Narabayashi I, Ikeda H, Kuma K, et al. . Clinical aspects of primary thyroid lymphoma: diagnosis and treatment based on our experience of 119 cases. Thyroid 1993;3:93–9. [DOI] [PubMed] [Google Scholar]
- 3.Kimura H, Yamashita S, Ashizawa K, Yokoyama N, Nagataki S. Thyroid dysfunction in patients with amyloid goitre. Clin Endocrinol (Oxf) 1997;46:769–74. [DOI] [PubMed] [Google Scholar]
- 4.Papi G, Briganti F, Artioli F, Cavazza A, Carapezzi C, Roggeri A, et al. . Sarcoidosis of the thyroid gland associated with hyperthyroidism: review of the literature and report of two peculiar cases. J Endocrinol Invest 2006;29:834–9. [DOI] [PubMed] [Google Scholar]
- 5.Miyakawa M, Sato K, Hasegawa M, Nagai A, Sawada T, Tsushima T, et al. . Severe thyrotoxicosis induced by thyroid metastasis of lung adenocarcinoma: a case report and review of the literature. Thyroid 2001;11:883–8. [DOI] [PubMed] [Google Scholar]
- 6.Eriksson M, Ajmani SK, Mallette LE. Hyperthyroidism from thyroid metastasis of pancreatic adenocarcinoma. JAMA 1977;238:1276–8. [PubMed] [Google Scholar]


