Abstract
Data addressing the use of respiratory support in acute coronary syndromes are lacking. To address this evidence gap, we characterized prognostic impact and trends in utilization of invasive mechanical ventilation (IMV) and non-invasive ventilation (NIV) in patients hospitalized with ST-segment elevation myocardial infarction (STEMI) from 2002 through 2013 using the National Inpatient Sample. Multivariable logistic regression was performed to identify patient, hospital, and clinical characteristics associated with requiring IMV or NIV within 24-hours of hospitalization. Multivariable Cox proportional hazards regression was used to quantify the magnitude of in-hospital mortality associated with IMV and NIV use. Between 2002 and 2013, we identified 1,867,114 STEMI patients. Age, sex, higher comorbidity burden and chronic pulmonary disease were significantly associated with need for respiratory support. The use of IMV and NIV increased at average annual rates of 6.6% and 14.3%, respectively (Ptrend < 0.001). Age- and sex-adjusted mortality rates are high but declined for STEMI patients requiring IMV (44.7% in 2002 to 37.6% in 2013, Ptrend = 0.002) and NIV (11.6% in 2002 to 6.8% in 2013, Ptrend < 0.001). Compared to STEMI patients with no ventilation need, a requirement for IMV or NIV was associated with increased adjusted in-hospital mortality (hazard ratio [HR]: 2.5; p < 0.001 and [HR]: 1.7; p < 0.001, respectively). In conclusion, approximately 1 in 23 patients hospitalized with STEMI will require respiratory support in the form of IMV or NIV. STEMI patients who require respiratory support have a high risk of death, though rates of in-hospital mortality have decreased over time.
Keywords: myocardial infarction, invasive mechanical ventilation, non-invasive ventilation, resource utilization, mortality, trend
Introduction
ST-segment elevation myocardial infarction (STEMI) complicated by respiratory failure is a common entity in clinical practice, however the incidence nationwide and the risk attributable to concomitant need for respiratory support in STEMI are not well established. Positive pressure ventilation can impact myocardial ischemia1, and small studies have suggested substantially worse outcomes among patients with myocardial infarction (MI) requiring ventilator support2–4. Defining the magnitude of this problem is also a prerequisite to further study of specific ventilation strategies in patients with myocardial infarction, which is an unmet need in critical care cardiology research5. Thus, our goal was to characterize the incidence and temporal trends of use of IMV and NIV in STEMI, to identify the magnitude of hazard for mortality associated with requiring IMV and NIV in STEMI, and to identify clinical characteristics suggesting increased likelihood of need for respiratory support in STEMI. To address these questions, we conducted an analysis in the National Inpatient Sample (NIS), a comprehensive national database of United States hospital admissions.
Methods
We abstracted data from the NIS database from 2002 to 2013. The NIS is the largest all-payer inpatient care database in the United States and contains discharge level data for approximately 8 million hospitalizations annually from 1000 U.S hospitals. Approval for the use of the NIS patient-level data was obtained from the Institutional Review Board of Johns Hopkins University and from the Healthcare Cost and Utilization Project.
All diagnoses and procedures in the NIS are coded with standard International Classification of Disease-Ninth Edition- Clinical Modification (ICD-9-CM) codes. The first diagnosis in the database is the principal diagnosis considered the primary reason for hospital admission. All hospitalizations with a principal diagnosis of STEMI (n=2,385,288) were identified using ICD-9-CM codes consistent with previously published literature6,7. Patients were excluded (n=469,347) from the study if they were <18 years of age, were missing data on survival outcome upon discharge or were transferred in from another acute care hospital (Supplementary eFigure 1). Patients with out-of-hospital cardiac arrest as the primary diagnosis (identified by a primary ICD-9 code 427.5 & 427.41) were excluded given that nearly all of these patients would be expected to have advanced airways placed pre-hospital or shortly after emergency department arrival. ICD-9-CM procedural codes 96.04 and 93.90 were then used to identify the implementation of invasive mechanical ventilation (IMV) and non-invasive ventilation (NIV) consistent with methodology previously published8,9. Time from admission to initiation of IMV or NIV was extracted and patients with time-to-ventilation beyond 24 hours were excluded (n=48,827) to ensure that the use of IMV and NIV was immediately proximal to and likely referable to presentation with STEMI. The final study population analyzed, therefore, included 7,030 patients with STEMI treated with NIV, 72,220 patients with STEMI treated with IMV and 1,787,864 patients with STEMI and no ventilation needs (Supplemental Figure 1).
The NIS provides 29 Elixhauser comorbidities for each hospital admission on the basis of standard ICD-9 CM codes. These were used to derive the prevalence of chronic pulmonary disease, chronic renal failure, congestive heart failure, diabetes mellitus, hypertension, obesity and peripheral vascular disease in our population. In addition, we used standard ICD-9-CM codes to identify the prevalence of coronary artery disease, dyslipidemia, smoking, prior myocardial infarction, prior percutaneous coronary intervention, prior coronary artery bypass graft surgery as well as occurrence of in-hospital cardiac arrest and cardiogenic shock. The burden of comorbidities was assessed using the Charlson Comorbidity Score which is based on 17 diagnosis categories with higher scores associated with higher in-hospital mortality10. Procedural ICD-9-CM codes were also used to capture treatment with intra-aortic balloon pump, percutaneous coronary intervention, coronary artery bypass graft surgery as well as thrombolysis during the current hospitalization. Our choice of ICD-9-CM codes is consistent with methodologies detailed elsewhere11,12 and a list of all used ICD-9-CM codes is shown in Supplementary eTable 1.
We evaluated the trends in mortality and use of ventilation strategies in patients hospitalized with ST-segment elevation myocardial infarction in the United States between 2002 and 2013. We divided our population into three groups: STEMI with IMV, STEMI with NIV and STEMI with no ventilation needs. In-hospital mortality and use of ventilation (either IMV or NIV) were primary end points in this study. Secondary end points of interest included total hospital charges, and total hospital costs and charges.
Statistical comparisons were performed using Stata/MP version 13.0 (StataCorp Inc, College Station, TX). The NIS database provides “trend weights” to facilitate analysis of trends across multiple years and to obtain national estimates. Patient- and hospital- level characteristics and outcomes of interest were compared between the three groups (STEMI with IMV, STEMI with NIV and STEMI with no ventilation needs) using the Pearson χ2 test for categorical variables and linear regression (1-way ANOVA) for continuous variables. To determine the predictors of need for IMV, we constructed survey-weighted logistic regression models with IMV as the dependent variable while accounting for clustering within hospitals. A similar model was used to determine predictors of need for NIV. Multivariate logistic regression models were fitted adjusting for factors of a priori interest including age, sex, race, Charlson comorbidity index, chronic pulmonary disease, smoking, obesity, weekend versus weekday admission, in-hospital cardiac arrest, development of cardiogenic shock and admission to a teaching vs. non-teaching hospital.
Annual rates of IMV and NIV were calculated per 1000 STEMI patients between 2002 and 2013. Logistic regression models for IMV and NIV were fitted with year as an independent continuous variable (2002-2013) to obtain odds ratios per year-unit increase and corresponding Ptrend. Linear regression models were similarly fitted to examine temporal trends in mean total hospital charges and costs between 2002 and 2013. To assess whether in-hospital mortality had improved over time, multivariable regression models adjusting for age and sex were constructed according to mode of ventilation. These models accounted for clustering of patients within hospitals. Because in-hospital mortality exceeded 10%, we used Zou’s method to directly estimate rate ratios instead of odds ratios by specifying a Poisson distribution and including a robust variance estimate in our models13. Our independent variable, calendar year, was included as a categorical variable, with 2002 as the reference year. Predictive margins were then used to obtain yearly risk-adjusted mortality rates for the study period. These rates represent the estimated in-hospital mortality for each year if the patient age/sex distribution were identical to that in the reference year. We also evaluated calendar year as a continuous variable to obtain adjusted rate ratio for year-to-year mortality trends (Ptrend). We analyzed the association between ventilation strategies and in-hospital mortality using Cox proportional hazards models censoring at end of follow up (hospital discharge or 30-days of hospital stay), whichever came first. Survival curves for the three groups were plotted by the Kaplan–Meier method, and the log‐rank test was used to test group differences in mortality. Cox proportional hazards modeling was used to calculate univariate and multivariate hazard ratios and the associated 95% CIs and P values. The proportional hazards assumption was met in all cases.
Data were complete for all covariates except race (21.9% missing), teaching status (0.4% missing), and sex (<0.1% missing). The report of the “other” race category in NIS varies between participating states; thus the “other” race (2.5%) category was considered as missing. We made the assumption that data were missing at random (MAR) and performed multivariate imputation by chained equations (MICE) methods estimated from sequential multivariable models with fully conditional specifications. Overall, 25 imputed data sets were constructed using information from all covariates used in regression models as well as other covariates in the database without missing information. Results with and without imputation were not meaningfully different. Thus, the former are reported.
Results
Of 1,867,114 STEMI patients included from 2002 to 2013, 72,220 were treated with IMV (3.9%) and 7,030 were treated with NIV (0.4%). Compared to STEMI patients requiring no respiratory support, patients who required IMV or NIV were older and more likely to be females (Table 1). Patients requiring respiratory support with IMV or NIV were also more likely to have chronic lung disease, chronic kidney disease and diabetes with a resultant higher Charlson comorbidity index but less likely to smoke or have previously diagnosed coronary artery disease and dyslipidemia (Table 1). Smokers were younger than non-smokers and had correspondingly lower co-morbidity index as shown in supplemental eTable 2.
Table 1.
Demographics and Outcomes of Patients with ST-Elevation Myocardial Infarction, NIS 2002–2013
| Characteristics | ST Elevation Myocardial Infarction: | p Value | |||
|---|---|---|---|---|---|
| without IMV or NIV (n = 1,787,864) |
with NIV (n = 7,030) |
with IMV (n = 72,220) |
|||
| NIV vs. neither | IMV vs. neither | ||||
| Age (years) | 64 ± 0.1 | 73 ± 0.4 | 68 ± 0.1 | <0.001 | <0.001 |
| Women | 604,820 (34%) | 3,527 (50%) | 28,777 (40%) | <0.001 | <0.001 |
| White | 1,461,618 (82%) | 5,671 (81%) | 55,159 (76%) | <0.001 | <0.001 |
| Black | 140,681 (8%) | 497 (7%) | 6,671 (9%) | ||
| Hispanic | 137,792 (8%) | 630 (9%) | 7,343 (10%) | ||
| Asian/Pacific Islander | 39,818 (2%) | 217 (3%) | 2,778 (4%) | ||
| Native American | 7,955 (0.4%) | 15 (0.2%) | 269 (0.4%) | ||
| Admission on weekend | 489,979 (27%) | 1,906 (27%) | 21,240 (29%) | 0.8 | <0.001 |
| Chronic pulmonary disease | 266,047 (15%) | 2,504 (36%) | 15,375 (21%) | <0.001 | <0.001 |
| Chronic renal failure | 117,597 (7%) | 1,574 (22%) | 9,696 (13%) | <0.001 | <0.001 |
| Chronic heart failure | 15,068 (1%) | 43 (1%) | 2,047 (3%) | 0.3 | <0.001 |
| Coronary artery disease | 1,355,231 (76%) | 4,516 (64%) | 44,719 (62%) | <0.001 | <0.001 |
| Diabetes mellitus (Uncomplicated) | 403,269 (23%) | 2,273 (32%) | 18,958 (26%) | <0.001 | <0.001 |
| Diabetes mellitus (Complicated) | 51,816 (3%) | 557 (8%) | 3,270 (5%) | <0.001 | <0.001 |
| Dyslipidemia | 905,506 (51%) | 2,955 (42%) | 22,546 (31%) | <0.001 | <0.001 |
| Hypertension | 1,010,537 (57%) | 4,519 (64%) | 37,671 (52%) | <0.001 | <0.001 |
| Obesity (coded in NIS) | 166,983 (9%) | 1,062 (15%) | 6,577 (9%) | <0.001 | 0.4 |
| Peripheral vascular disease | 119,725 (7%) | 757 (11%) | 6,800 (9%) | <0.001 | <0.001 |
| Previous myocardial infarction | 128,071 (7%) | 721 (10%) | 4,695 (6.5%) | <0.001 | 0.005 |
| Previous coronary intervention | 149,118 (8%) | 591 (8%) | 5,032 (7%) | 0.9 | <0.001 |
| Previous coronary bypass grafting | 62,958 (4%) | 304 (4%) | 2,944 (4.1%) | 0.1 | 0.001 |
| Smoker | 672,111 (38%) | 1,998 (28%) | 18,308 (25%) | <0.001 | <0.001 |
| Charlson comorbidity index | <0.001 | <0.001 | |||
| 1 | 856,130 (48%) | 723 (10%) | 19,475 (27%) | ||
| 2 | 546,155 (31%) | 1,942 (28%) | 24,184 (33%) | ||
| ≥3 | 385,579 (22%) | 4,366 (62%) | 28,561 (40%) | ||
| Teaching hospital | 791,483 (44%) | 3,096 (44%) | 31,388 (43%) | 0.9 | 0.4 |
| Outcomes | |||||
| Acute renal failure | 111,471 (6%) | 1,636 (23%) | 19,873 (28%) | <0.001 | <0.001 |
| Cardiogenic shock | 106,545 (6%) | 1,249 (18%) | 33,191 (46%) | <0.001 | <0.001 |
| Delirium | 14,338 (1%) | 211 (3%) | 1,960 (3%) | <0.001 | <0.001 |
| In-hospital arrest | 17,865 (1%) | 133 (2%) | 17,429 (24%) | 0.001 | <0.001 |
| In-hospital mortality | 92,381 (5%) | 1,269 (18%) | 33,394 (46%) | <0.001 | <0.001 |
| Hospital length of stay (days) | 4.4 ± 0.1 | 5.9 ± 0.1 | 7.2 ± 0.1 | <0.001 | <0.001 |
| Total hospital charges (US$) | $67,739 ± $824 | $73,978 ± $2,561 | $123,925 ± $2,332 | 0.009 | <0.001 |
| Total hospital costs (US$) | $21,355 ± $168 | $22,130 ± $595 | $35,961 ± $518 | 0.2 | <0.001 |
| Intra-aortic balloon pump | 132,397 (7%) | 696 (10%) | 22,183 (31%) | 0.001 | <0.001 |
| Angiography and Revascularization | |||||
| Coronary angiography | 1,357,992 (76%) | 3,163 (45%) | 43,849 (61%) | <0.001 | <0.001 |
| Percutaneous coronary intervention | 1,134,721 (63%) | 2,324 (33%) | 35,928 (50%) | <0.001 | <0.001 |
| Thrombolysis | 81,435 (5%) | 261 (4%) | 3,270 (5%) | 0.1 | 0.9 |
| Coronary bypass grafting | 131,826 (7%) | 318 (5%) | 3,824 (5%) | <0.001 | <0.001 |
Values are mean ± SE, or n (%)
Abbreviations: IMV, invasive mechanical ventilation; NIS, national inpatient sample; NIV, non-invasive mechanical ventilation; SE, standard error of the mean; STEMI, ST-elevation myocardial infarction.
Moving from no respiratory support to NIV to IMV, there were stepwise increases in rates of cardiogenic shock, in-hospital arrest, in-hospital mortality, hospital length of stay and hospital costs and charges (Table 1). Patients requiring IMV and NIV had higher rates of anterior and anterolateral infarction and lower rates of inferior infarction compared to patients requiring neither modality (eTable 3). Patients requiring IMV and NIV both had increased rates of additional organ failure- delirium (brain failure) and renal failure- compared to those requiring neither modality. Compared to STEMI patients requiring no respiratory support, patients with STEMI requiring IMV or NIV had significantly lower use of coronary angiography, PCI and CABG.
The association between selected factors and need for IMV or NIV for the entire study population is shown in Table 2. Older age, female sex, increasing co-morbidity index, chronic lung disease, weekend admission, presence of cardiogenic shock, and in-hospital arrest were all independently associated with requiring IMV. Similarly, age, female sex, increasing co-morbidity index, chronic lung disease, and presence of cardiogenic shock were associated with requiring NIV. Smoking was associated with a lower likelihood of requiring IMV and obesity was associated with a higher likelihood of requiring NIV.
Table 2.
Association Between Select Factors and Type of Ventilation For the Entire Study Period, NIS 2002–2013
| Factor | Odds Ratio (95% CI) | |||
|---|---|---|---|---|
| Invasive Mechanical Ventilation on Day 1 | Non-Invasive Ventilation on Day 1 | |||
| Unadjusted | Adjusted* | Unadjusted | Adjusted* | |
| Age (every 10yrs >18) | 1.18 (1.17–1.20) | 1.04 (1.02–1.06) | 1.56 (1.49–1.62) | 1.40 (1.33–1.47) |
| Women | 1.29 (1.25–1.34) | 1.08 (1.04–1.12) | 1.95 (1.75–2.17) | 1.23 (1.11–1.37) |
| White | Reference | Reference | Reference | Reference |
| Black | 1.26 (1.17–1.35) | 1.32 (1.22–1.43) | 0.90 (0.72–1.12) | 0.94 (0.75–1.17) |
| Hispanic | 1.41 (1.31–1.52) | 1.36 (1.25–1.48) | 1.16 (0.95–1.42) | 1.29 (1.05–1.58) |
| Asian/Pacific Islander | 1.84 (1.65–2.07) | 1.50 (1.32–1.71) | 1.36 (0.97–1.92) | 1.43 (1.01–2.01) |
| Native American | 0.90 (0.65–1.23) | 0.86 (0.59–1.25) | 0.48 (0.13–1.76) | 0.52 (0.14–1.9) |
| Charlson comorbidity index | ||||
| 1 | Reference | Reference | Reference | Reference |
| 2 | 1.94 (1.86–2.03) | 1.52 (1.45–1.60) | 4.13 (3.42–4.97) | 3.01 (2.48–3.65) |
| ≥3 | 3.22 (3.08–3.37) | 2.17 (2.05–2.29) | 12.77 (10.70–15.25) | 7.27 (5.97–8.85) |
| Chronic pulmonary disease | 1.54 (1.47–1.61) | 1.11 (1.05–1.17) | 3.10 (2.79–3.46) | 1.42 (1.26–1.60) |
| Smoker | 0.56 (0.54–0.59) | 0.74 (0.70–0.78) | 0.67 (0.59–0.76) | 1.07 (0.94–1.22) |
| Obesity | 0.97 (0.91–1.03) | 1.04 (0.97–1.11) | 1.73 (1.49–2.01) | 2.10 (1.81–2.44) |
| Weekend versus weekday | 1.10 (0.06–1.14) | 1.11 (1.07–1.16) | 0.98 (0.87–1.10) | 1.01 (0.90–1.13) |
| Teaching versus non-teaching | 0.97 (0.89–1.05) | 0.94 (0.87–1.03) | 0.99 (0.85–1.16) | 1.10 (0.94–1.29) |
| In-hospital arrest | 31.4 (29.6–33.3) | 20.4 (18.9–22.0) | 1.0 (0.67–1.49) | 0.64 (0.43–0.96) |
| Cardiogenic Shock | 13.3 (12.7–13.9) | 9.2 (8.8–9.7) | 2.66 (2.32–3.04) | 1.96 (1.70–2.26) |
Adjusted for age, gender, race, Charlson comorbidity index, chronic pulmonary disease, smoking, obesity, weekend vs. weekday admission, in-hospital cardiac arrest, cardiogenic shock, and teaching status of hospital.
Abbreviations: NIS, national inpatient sample
As shown in Figure 1, use of IMV increased at an average annual rate of 6.6%; use of NIV increased at an average annual rate of 14.3% (Ptrend < 0.001). During the same period, age-and sex-adjusted mortality decreased in both groups (Figure 2). The Kaplan-Meier survival curves associated with in-hospital mortality are displayed in Figure 3 for STEMI patients requiring IMV or NIV as well as for those with no requirement for respiratory support.
Figure 1. Trends of Ventilation Strategies.
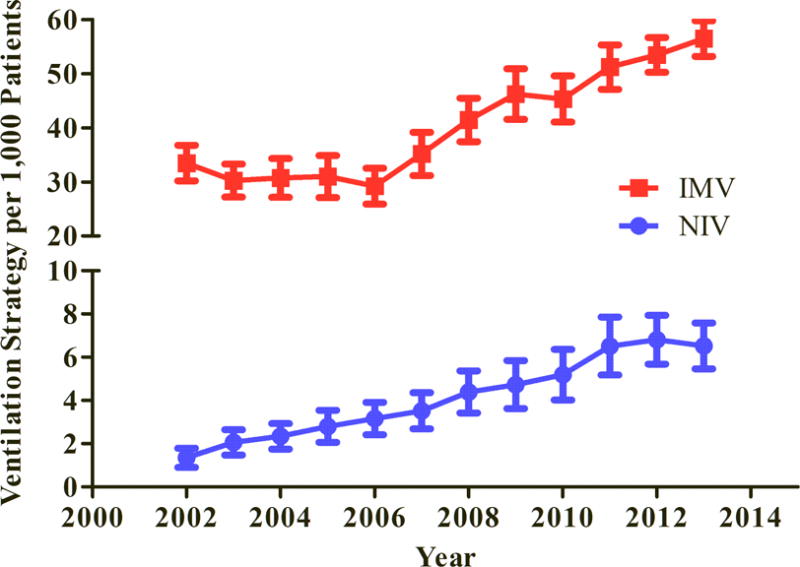
Rates of IMV and NIV use in STEMI during the study period (P < 0.001 for trend for both IMV and NIV). STEMI = ST-segment elevation myocardial Infarction; IMV = invasive mechanical ventilation; NIV = non-invasive mechanical ventilation.
Figure 2. Mortality Trends.
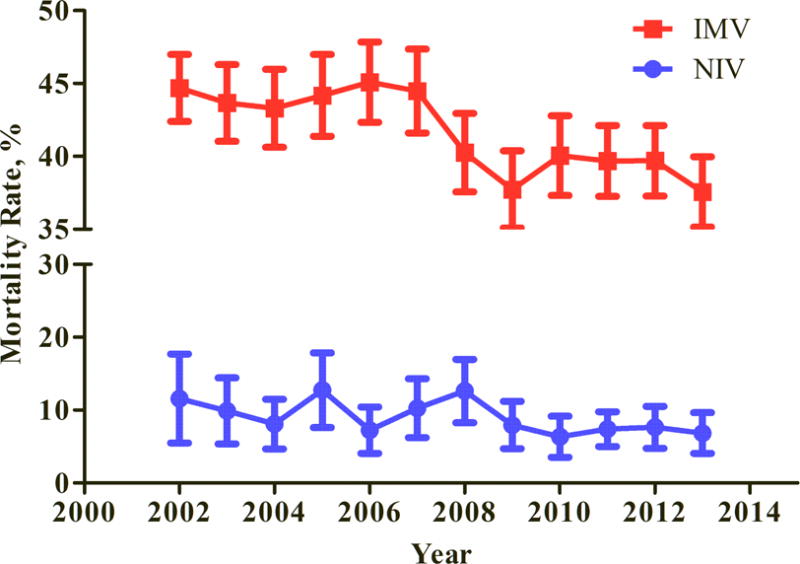
Rates are adjusted for age and sex in patients with STEMI treated with both NIV and IMV (P < 0.001 for trend for both). STEMI = ST-segment elevation myocardial Infarction; IMV = invasive mechanical ventilation; NIV = non-invasive mechanical ventilation.
Figure 3. Kaplan-Meier Survival Curves.
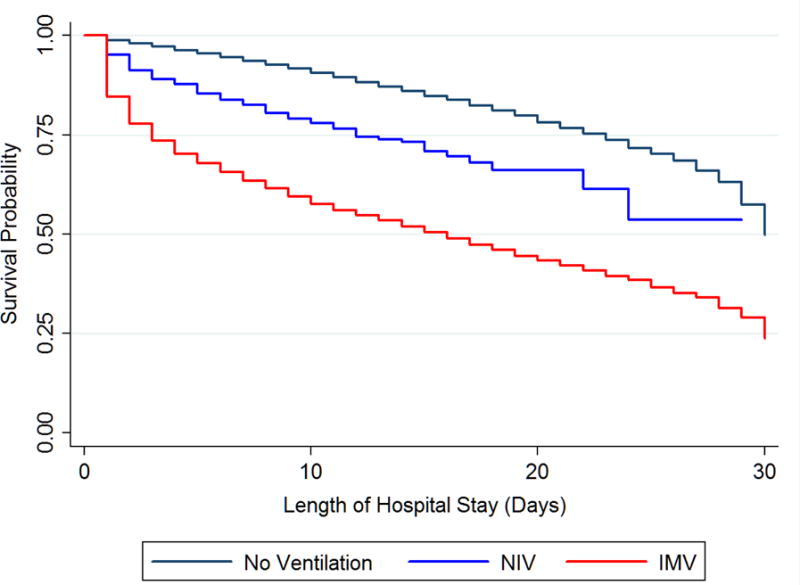
Kaplan-Meier curves for 30-day in-hospital mortality for patients with STEMI receiving IMV, NIV, or neither modality (P < 0.001 by log-rank). STEMI = ST-segment elevation myocardial Infarction; IMV = invasive mechanical ventilation; NIV = non-invasive mechanical ventilation.
Figure 4 displays hazard ratios for clinical factors predicting mortality in the overall cohort. In panel A, which displays hazard ratios from univariate models, the need for IMV in STEMI was associated with a 5.47 fold increased hazard for death, which was second only to in-hospital cardiac arrest in magnitude. The need for NIV was associated with a 2.88 fold increased hazard for death. Both these associations persisted when adjusting for multiple clinical and hospital factors (Figure 4 panel B). Relative use of IMV and NIV across hospital size and geographic region is displayed in supplemental eFigures 2 and 3.
Figure 4. Cox Proportional Hazards Regression Analysis.
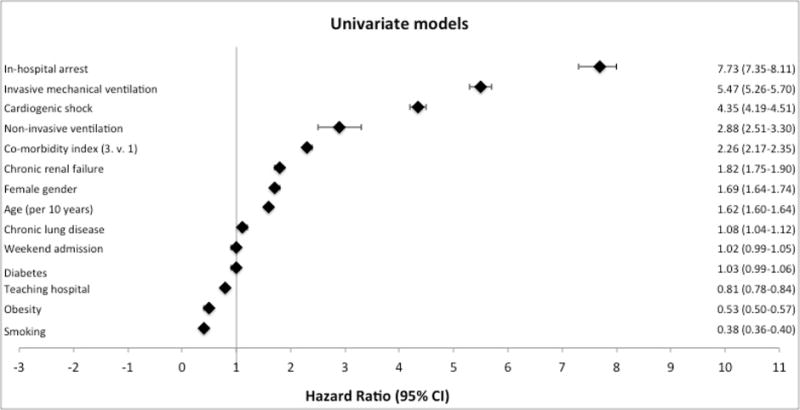
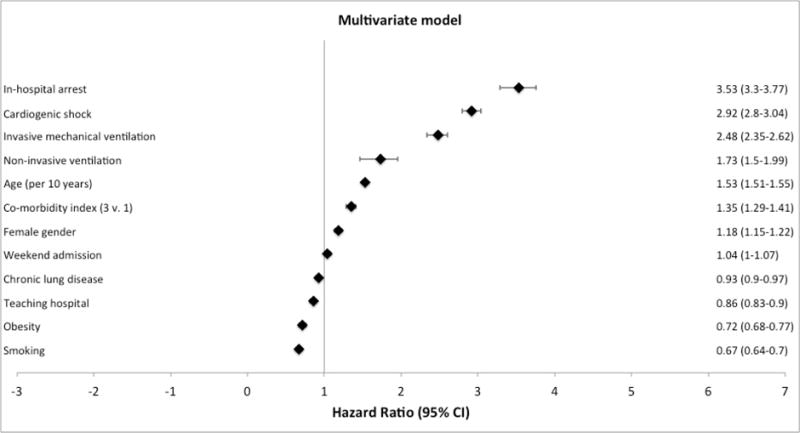
Panel A displays hazard ratios from univariate cox models with a primary outcome of in-hospital mortality. Panel B displays the hazard ratios from a multivariate cox model incorporating the covariates displayed, with a primary outcome of in-hospital mortality.
Both cost of hospitalization and hospital charges for STEMI patients requiring IMV and NIV increased over the study period (Figure 5).
Figure 5. Trends of Hospital Costs and Charges.
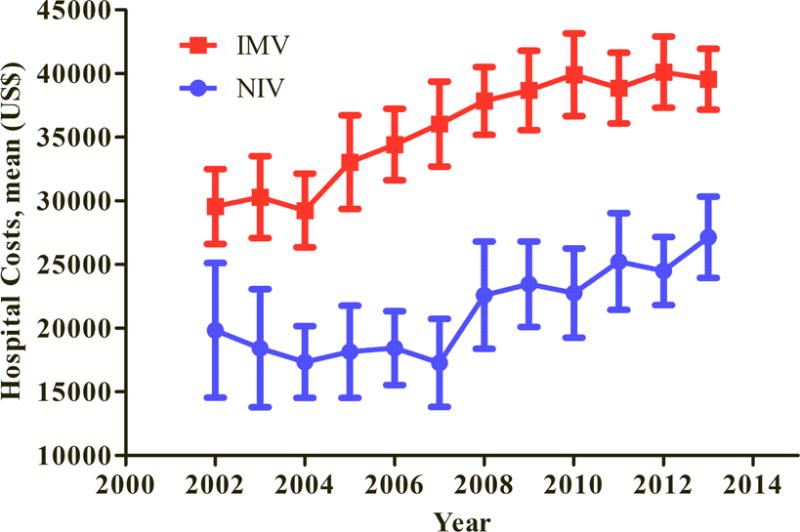
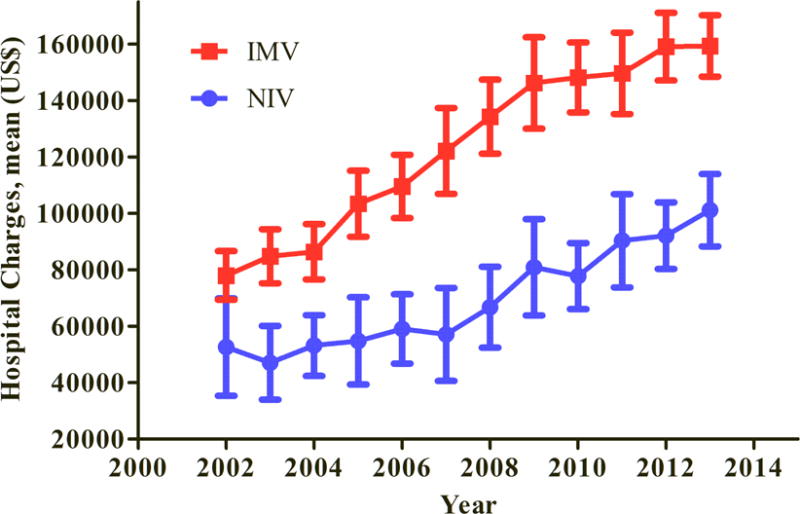
Panel A displays the hospital costs and panel B hospital charges for patients with STEMI treated with IMV and NIV over time. (P < 0.001 for all trends). STEMI = ST-segment elevation myocardial Infarction; IMV = invasive mechanical ventilation; NIV = non-invasive mechanical ventilation.
Discussion
We demonstrate that approximately 1 in 23 patients with STEMI will require respiratory support with either invasive mechanical ventilation or non-invasive ventilation and the use of both IMV and NIV in STEMI is increasing over time. Patient demographics, chronic comorbidity, and acute illness predict the need for respiratory support, and the use of IMV and NIV is associated with substantially increased mortality and rising costs of care.
To our knowledge, our study represents the first nationwide assessment of the incidence and trends in use of mechanical and non-invasive ventilation in the setting of STEMI. Although we demonstrate that mortality is improving over time, mortality rates remain substantial. Of STEMI patients treated with IMV, 46% died, and a 2.5 fold increased risk of death persisted even after adjusting for presence of cardiogenic shock and in-hospital arrest. Prior small studies are consistent with our findings. A multi-center study of 457 intubated patients with acute MI reported 48% in-hospital mortality3. One single-center study of 157 intubated patients with acute MI reported 52% 28-day mortality4, and a second single center study of intubated STEMI patients reported short-term mortality of 44%14. Of note, our findings of decreased likelihood of mortality associated with obesity and smoking are consistent with some other studies of the “obesity paradox”15 and “smoker’s paradox”16, felt to represent asymmetry of baseline risk factors rather than protective effect. This paradox has been observed in other studies of STEMI in the NIS17. Our finding that weekend admission was associated with increased rates of respiratory failure may be related to the fact that multiple studies and a systematic review have suggested that STEMI patients admitted during weekends and off-hours have worse outcomes related in part to delays in presentation and longer door-to-reperfusion times18.
The excess mortality associated with IMV and NIV is likely multifactorial and incorporates the high percentage of these patients with cardiogenic shock and in-hospital arrest19,20. After adjustment for these factors, the hazard ratio for death for STEMI patients requiring IMV in our study was 2.5, which is comparable to the magnitude of risk of a Killip 2, 3, or 4 myocardial infarction21,22. The need for respiratory support with IMV or NIV in STEMI may thus be an integrative risk marker that incorporates infarct size, chronic co-morbidities, and respiratory and hemodynamic status. In our study, patients requiring NIV and IMV also received fewer revascularization procedures including both PCI and CABG- it is possible that these patients would have been transferred to other centers, felt ineligible due to severity of illness, or died prior to revascularization. The lower rate of revascularization would also contribute to the excess mortality observed, and presentation with respiratory failure has been shown to be associated with increased delay to PCI23. Health systems should identify and minimize delays in reperfusion for acute MI patients with respiratory failure.
Mechanical ventilation itself could also impact the excess mortality we observe. Barotrauma, atelectrauma, volutrauma and biotrauma are all adverse effects of mechanical ventilation24. Whereas high quality evidence exists to guide prescription of safe ventilation settings in patients with25 and without26 ARDS, there is a dearth of evidence as to the optimal ventilator settings in acute ischemic heart disease. Positive intrathoracic pressure can impact cardiac hemodynamics27 and reduction in ventilator support can precipitate worsening cardiac ischemia1. Thus, there is a large evidence gap in how best to ventilate the patient with acute ischemic heart disease who requires positive pressure ventilation. There is little-to-no high quality data to guide selection of the optimal mode of respiratory support in acute ischemic heart disease.
There are limitations to our study including retrospective study design; thus, we demonstrate associations and can only speculate as to causal relationships between clinical factors, the use of IMV and NIV, and outcome. The NIS is an administrative database; therefore inaccuracies in coding of procedures or diagnoses are an inherent limitation. Given the administrative nature of the database, it is also not possible to ascertain granular differences in medical therapy between groups- such as antiplatelet therapy, for example- which is an important area for future research. We included only patients presenting de novo to the hospital, excluding patients who were admitted as inter-hospital transfers. Characterizing the population of patients with STEMI and respiratory failure who are treated with a transfer strategy is an important area for future study. Overall, our findings imply that studies to optimize systems-related issues including CCU staffing, and to identify the optimal mode of respiratory support and the safest ventilator settings for patients with acute ischemic heart disease are needed.
Supplementary Material
Acknowledgments
Dr. Metkus received prior salary support from NIH-NHLBI grant number T32-HL007227-40 and performs consulting unrelated to this subject matter for BestDoctors Inc and Oakstone/EBIX. Dr. Metkus received royalties for a textbook publication for McGraw-Hill publishing, unrelated to this subject matter.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Authors have no conflicts of interest germane to this paper.
References
- 1.Rasanen J, Nikki P, Heikkila J. Acute myocardial infarction complicated by respiratory failure. The effects of mechanical ventilation. Chest. 1984;85:21–28. doi: 10.1378/chest.85.1.21. [DOI] [PubMed] [Google Scholar]
- 2.Eran O, Novack V, Gilutz H, Zahger D. Comparison of thrombolysis in myocardial infarction, Global Registry of Acute Coronary Events, and Acute Physiology and Chronic Health Evaluation II risk scores in patients with acute myocardial infarction who require mechanical ventilation for more than 24 hours. The American journal of cardiology. 2011;107:343–346. doi: 10.1016/j.amjcard.2010.09.024. [DOI] [PubMed] [Google Scholar]
- 3.Kouraki K, Schneider S, Uebis R, Tebbe U, Klein HH, Janssens U, Zahn R, Senges J, Zeymer U. Characteristics and clinical outcome of 458 patients with acute myocardial infarction requiring mechanical ventilation. Results of the BEAT registry of the ALKK-study group. Clinical research in cardiology. 2011;100:235–239. doi: 10.1007/s00392-010-0235-6. [DOI] [PubMed] [Google Scholar]
- 4.Lesage A, Ramakers M, Daubin C, Verrier V, Beynier D, Charbonneau P, du Cheyron D. Complicated acute myocardial infarction requiring mechanical ventilation in the intensive care unit: prognostic factors of clinical outcome in a series of 157 patients. Critical care medicine. 2004;32:100–105. doi: 10.1097/01.CCM.0000098605.58349.76. [DOI] [PubMed] [Google Scholar]
- 5.van Diepen S, Granger CB, Jacka M, Gilchrist IC, Morrow DA, Katz JN. The unmet need for addressing cardiac issues in intensive care research. Critical care medicine. 2015;43:128–134. doi: 10.1097/CCM.0000000000000609. [DOI] [PubMed] [Google Scholar]
- 6.Joynt KE, Blumenthal DM, Orav EJ, Resnic FS, Jha AK. Association of public reporting for percutaneous coronary intervention with utilization and outcomes among Medicare beneficiaries with acute myocardial infarction. Jama. 2012;308:1460–1468. doi: 10.1001/jama.2012.12922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Yeh RW, Sidney S, Chandra M, Sorel M, Selby JV, Go AS. Population trends in the incidence and outcomes of acute myocardial infarction. The New England journal of medicine. 2010;362:2155–2165. doi: 10.1056/NEJMoa0908610. [DOI] [PubMed] [Google Scholar]
- 8.Chandra D, Stamm JA, Taylor B, Ramos RM, Satterwhite L, Krishnan JA, Mannino D, Sciurba FC, Holguin F. Outcomes of noninvasive ventilation for acute exacerbations of chronic obstructive pulmonary disease in the United States, 1998–2008. American journal of respiratory and critical care medicine. 2012;185:152–159. doi: 10.1164/rccm.201106-1094OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Mehta AB, Syeda SN, Wiener RS, Walkey AJ. Epidemiological trends in invasive mechanical ventilation in the United States: A population-based study. Journal of critical care. 2015;30:1217–1221. doi: 10.1016/j.jcrc.2015.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, Saunders LD, Beck CA, Feasby TE, Ghali WA. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Medical care. 2005;43:1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83. [DOI] [PubMed] [Google Scholar]
- 11.Khera S, Kolte D, Aronow WS, Palaniswamy C, Subramanian KS, Hashim T, Mujib M, Jain D, Paudel R, Ahmed A, Frishman WH, Bhatt DL, Panza JA, Fonarow GC. Non-ST-elevation myocardial infarction in the United States: contemporary trends in incidence, utilization of the early invasive strategy, and in-hospital outcomes. Journal of the American Heart Association. 2014;3 doi: 10.1161/JAHA.114.000995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kolte D, Khera S, Aronow WS, Palaniswamy C, Mujib M, Ahn C, Iwai S, Jain D, Sule S, Ahmed A, Cooper HA, Frishman WH, Bhatt DL, Panza JA, Fonarow GC. Regional variation in the incidence and outcomes of in-hospital cardiac arrest in the United States. Circulation. 2015;131:1415–1425. doi: 10.1161/CIRCULATIONAHA.114.014542. [DOI] [PubMed] [Google Scholar]
- 13.Zou G. A modified poisson regression approach to prospective studies with binary data. American journal of epidemiology. 2004;159:702–706. doi: 10.1093/aje/kwh090. [DOI] [PubMed] [Google Scholar]
- 14.Lazzeri C, Valente S, Chiostri M, Attana P, Mattesini A, Gensini GF. Mechanical ventilation in the early phase of ST elevation myocardial infarction treated with mechanical revascularization. Cardiology journal. 2013;20:612–617. doi: 10.5603/CJ.2013.0161. [DOI] [PubMed] [Google Scholar]
- 15.Mehta RH, Califf RM, Garg J, White HD, Van de Werf F, Armstrong PW, Pieper KS, Topol EJ, Granger CB. The impact of anthropomorphic indices on clinical outcomes in patients with acute ST-elevation myocardial infarction. European heart journal. 2007;28:415–424. doi: 10.1093/eurheartj/ehl329. [DOI] [PubMed] [Google Scholar]
- 16.Reinstadler SJ, Eitel C, Fuernau G, de Waha S, Desch S, Mende M, Metzler B, Schuler G, Thiele H, Eitel I. Association of smoking with myocardial injury and clinical outcome in patients undergoing mechanical reperfusion for ST-elevation myocardial infarction. European heart journal cardiovascular Imaging. 2016 doi: 10.1093/ehjci/jew030. [DOI] [PubMed] [Google Scholar]
- 17.Gupta T, Kolte D, Khera S, Harikrishnan P, Mujib M, Aronow WS, Jain D, Ahmed A, Cooper HA, Frishman WH, Bhatt DL, Fonarow GC, Panza JA. Smoker’s Paradox in Patients With ST-Segment Elevation Myocardial Infarction Undergoing Primary Percutaneous Coronary Intervention. Journal of the American Heart Association. 2016;5 doi: 10.1161/JAHA.116.003370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sorita A, Ahmed A, Starr SR, Thompson KM, Reed DA, Prokop L, Shah ND, Murad MH, Ting HH. Off-hour presentation and outcomes in patients with acute myocardial infarction: systematic review and meta-analysis. Bmj. 2014;348:f7393. doi: 10.1136/bmj.f7393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kolte D, Khera S, Aronow WS, Mujib M, Palaniswamy C, Sule S, Jain D, Gotsis W, Ahmed A, Frishman WH, Fonarow GC. Trends in incidence, management, and outcomes of cardiogenic shock complicating ST-elevation myocardial infarction in the United States. Journal of the American Heart Association. 2014;3:e000590. doi: 10.1161/JAHA.113.000590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kontos MC, Scirica BM, Chen AY, Thomas L, Anderson ML, Diercks DB, Jollis JG, Roe MT, Ncdr Cardiac arrest and clinical characteristics, treatments and outcomes among patients hospitalized with ST-elevation myocardial infarction in contemporary practice: A report from the National Cardiovascular Data Registry. American heart journal. 2015;169:515–522 e511. doi: 10.1016/j.ahj.2015.01.010. [DOI] [PubMed] [Google Scholar]
- 21.Tsai TH, Chua S, Hussein H, Leu S, Wu CJ, Hang CL, Fang HY, Chung SY, Fu M, Chen HC, Chang LT, Yeh KH, Yip HK. Outcomes of patients with Killip class III acute myocardial infarction after primary percutaneous coronary intervention. Critical care medicine. 2011;39:436–442. doi: 10.1097/CCM.0b013e318206ccc3. [DOI] [PubMed] [Google Scholar]
- 22.De Luca G, Gibson CM, Huber K, Zeymer U, Dudek D, Cutlip D, Bellandi F, Noc M, Emre A, Zorman S, Gabriel HM, Maioli M, Rakowski T, Gyongyosi M, Van’t Hof AW, Cooperation E. Association between advanced Killip class at presentation and impaired myocardial perfusion among patients with ST-segment elevation myocardial infarction treated with primary angioplasty and adjunctive glycoprotein IIb-IIIa inhibitors. American heart journal. 2009;158:416–421. doi: 10.1016/j.ahj.2009.06.029. [DOI] [PubMed] [Google Scholar]
- 23.Blankenship JC, Skelding KA, Scott TD, Berger PB, Parise H, Brodie BR, Witzenbichler B, Gaugliumi G, Peruga JZ, Lansky AJ, Mehran R, Stone GW. Predictors of reperfusion delay in patients with acute myocardial infarction undergoing primary percutaneous coronary intervention from the HORIZONS-AMI trial. The American journal of cardiology. 2010;106:1527–1533. doi: 10.1016/j.amjcard.2010.07.033. [DOI] [PubMed] [Google Scholar]
- 24.Slutsky AS, Ranieri VM. Ventilator-induced lung injury. The New England journal of medicine. 2013;369:2126–2136. doi: 10.1056/NEJMra1208707. [DOI] [PubMed] [Google Scholar]
- 25.Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. The Acute Respiratory Distress Syndrome Network. The New England journal of medicine. 2000;342:1301–1308. doi: 10.1056/NEJM200005043421801. [DOI] [PubMed] [Google Scholar]
- 26.Serpa Neto A, Simonis FD, Barbas CS, Biehl M, Determann RM, Elmer J, Friedman G, Gajic O, Goldstein JN, Horn J, Juffermans NP, Linko R, de Oliveira RP, Sundar S, Talmor D, Wolthuis EK, de Abreu MG, Pelosi P, Schultz MJ. Association between tidal volume size, duration of ventilation, and sedation needs in patients without acute respiratory distress syndrome: an individual patient data meta-analysis. Intensive care medicine. 2014;40:950–957. doi: 10.1007/s00134-014-3318-4. [DOI] [PubMed] [Google Scholar]
- 27.Fessler HE. Heart-lung interactions: applications in the critically ill. The European respiratory journal. 1997;10:226–237. doi: 10.1183/09031936.97.10010226. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


