Abstract
Background:
During recent years transmission of Dirofilaria immitis (dog heart worm) by Culex pipiens and West Nile virus have been reported from Iran. The present study was preformed for evaluating the susceptibility status of Cx. pipiens collected from capital city of Tehran, Iran.
Methods:
Four Insecticides including: DDT 4%, Lambdacyhalothrin 0.05%, Deltamethrin 0.05% and Cyfluthrin 0.15 % according to WHO standard methods were used for evaluating the susceptibility status of Cx. pipiens from Tehran moreover For comparison susceptibility status a Laboratory strain also was used. Bioassay data were analyzed using Probit program. The lethal time for 50% and 90% mortality (LT50 and LT90) values were calculated from regression line.
Results:
The susceptibility status of lab strain of Cx. pipiens revealed that it is susceptible to Lambdacyhalothrin, Deltamethrin, Cyfluthrin and resistant to DDT. Moreover cyfluthrin with LT50=36 seconds and DDT with LT50=3005 seconds had the least and most LT50s. Field population was resistance to all tested insecticides and DDT yielded no mortality.
Conclusion:
Highly resistance level against all WHO recommended imagicides were detected in field populations. We suggest more biochemical and molecular investigations to detect resistance mechanisms in the field population for further decision of vector control.
Keywords: Susceptibility status, Culex pipiens, Tehran
Introduction
Mosquitoes known as the main groups of arthropods in medical and public health due to their role in transmission of Malaria, filariasis, several types of encephalitis and also many arboviral diseases (Horsfall 1955, Service 2003, Mullen 2009). In the Culicidae Family, Culex genus and specifically Cx. pipiens complex members including: Cx. pipiens pipiens, Cx. quinquefasciatus, Cx. p. pallens, Cx. pipiens form molestus act as efficient vectors for Sindbis virus, West Nile virus, Equine encephalitis, St Louis, Oropouche, Rift Valley fever, moreover Cx. pipiens transmit Plasmodium relictum that causing bird malaria. Its distribution is wide so that this species approximately present in all continent of the world (Mitchell et al. 1980, Vinogradova 2000, Smith and Fonseca 2004, Savage et al. 2007, Mullen 2009, Strickman and Fonseca 2012). In Iran during recent years transmitting of Dirofilaria immitis (dog heart worm), West Nile and Sindbis viruses by Culex mosquitoes have been reported (Naficy and Saidi 1970, Azari-Hamidian et al. 2007, Azari-Hamidian et al. 2009). Culex Genus habituated capital city of Tehran in sewage system of the houses, where there are different insecticides which have been used for controlling of household and agricultural pests such as: permehrin, bioallethrin, dursban, pirimiphos-methyl, malathion, chlorpyrifos-methyl, allethrin, propoxur. I addition different reagents also exist in the sweage systems. we postulated that resistance to insecticides is as a result of continous exposure to Different group of insecticides which may indirectly cause selection pressure on the susceptibility of mosquitoes mainly breed in wastewater habitats (Horsfall 1955, Lotfi 1976, Golestani 1976, Lines 1988, Vatandoost et al. 2004, Calhoun et al. 2007). Here upon the evaluation of susceptibility level of mosquitos for monitoring of resistance to insecticides is necessary and for this approach in Iran in recent years the most studies about evaluating susceptibility level of mosquitos to common insecticides have been on Anopheles mosquitos (Enayati et al. 2003, Vatandoost and Borhani 2004, Vatandoost and Hanafi-Bojd 2005, Vatandoost et al. 2005, Hanafi-Bojd et al. 2006, Shahi et al. 2006, Abai et al. 2008, Hanafi-Bojd et al. 2010, Oshaghi et al. 2011, Hanafi-Bojd et al. 2012, Soltani et al. 2013) and there are just a limited study about susceptibility status of Culex genus in Iran for example in the performed studies in Caspian sea coast about susceptibility level of Cx. pipiens complex results indicated that this species is resistant to DDT and susceptible to Dieldrin (Lotfi et al. 1975). Nazari and Janbakhsh in 2000 reported that Cx. pipiens in the southern area of Tehran is resistance to DDT (Nazari and Janbakhsh 2000). In 2004 the susceptibility level of laboratory and field collected strains of Cx. Quinquefasciatusin a medically important member belong to Cx. pipiens complex to different insecticides evaluated, DDT resistant was observed in both laboratory and field collected strains (Vatandoost et al. 2004). According to the most performed study around the world it seems that this species approximately is resistant to many insecticides or have multiple insecticide resistances (Davidson 1964, Mukhopadhyay et al. 1993, Ben Cheikh et al. 1998, Bisset et al. 1999, Martinez-Torres et al. 1999, Corbel et al. 2007, Tantely et al. 2010, Toma et al. 2011, Jones et al. 2012, Pocquet et al. 2013). The present study was preformed for evaluating susceptibility status of Cx. pipiens of Tehran City. The result of this study can be useful for future chemical control programs in the study area.
Materials and Methods
Study area
This study was conducted in Tehran city (35° 41′ 46″ N, 51° 25′ 23″ E), Tehran Province, Iran. Tehran is the capital of Iran and also is Iran's largest city (Fig. 1).
Fig. 1.

The map of Iran and location of Tehran city
Mosquito strains and adult susceptibility test
In this study four Insecticides including: DDT 4%, Lambdacyhalothrin 0.05%, Deltamethrin 0.05%, Cyfluthrin 0.15% were used for evaluating susceptibility status of Cx. pipiens. Moreover For comparison susceptibility status a Laboratory strain also was used. All tested species were reared in the insectary of School of Public Health, Tehran University of Medical Sciences under the standard condition.
Data analysis
Bioassay data were analyzed with Probit program (Finney 1971). For correction mortality, when control mortality is greater than 5% but less than 20%, then the observed mortality was corrected using Abbott's formula (Abbott 1965). By method of Finney the lethal Time for 50% and 90% mortality (LT50 and LT90) values and their 95% confidence interval and Probit regression line parameters were determined for both strains (Lab and field population). The regression line belong to each Insecticides after different exposure times were plotted using Microsoft Excel (ver. 2013).
Results
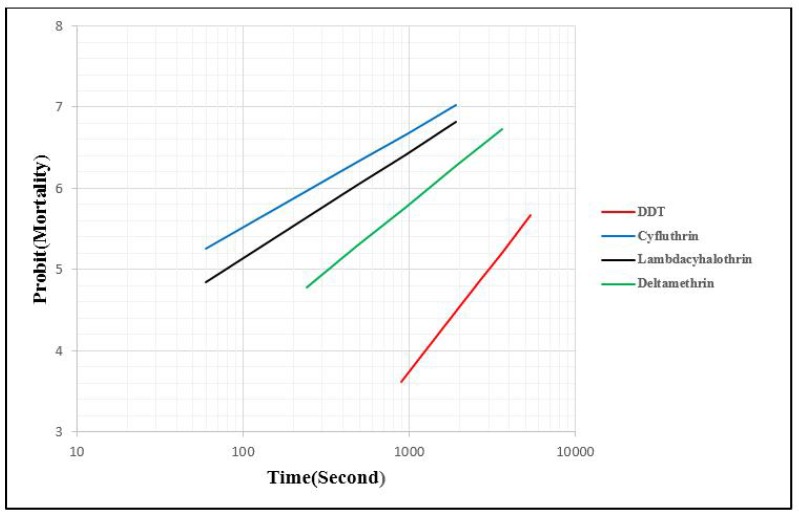
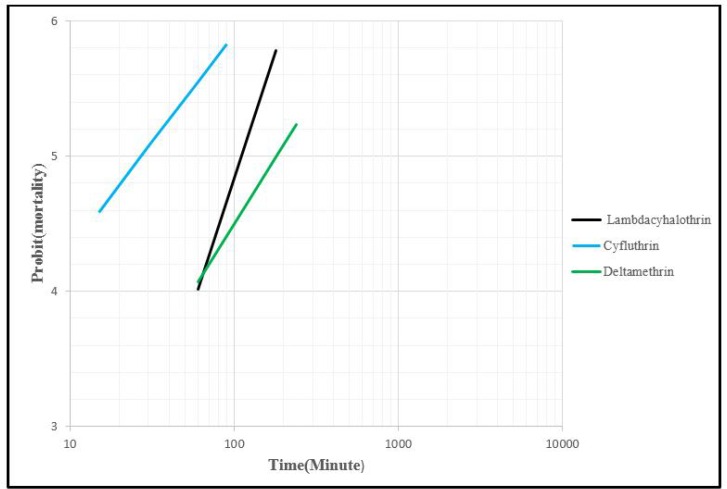
The result of susceptibility test for lab and filed strains of Cx. pipiens has been summarized in Table 1 and 2. Lab strain exhibited different LT50 valuses to different insecticides. Cyfluthrin with LT50= 36Sec, Lambdacyhalothrin (LT50=79), Deltamethrin (LT50 = 326) and DDT (LT50=3005) had the lowest to highest lethal time (Table 1 and 3). Although this result for field population indicated that DDT exhibited no mortality. Cyfluthrin with LT50=27minutes, Lambdacyhalothrin (LT50= 111 minutes) and Deltamethrin (LT50= 182 minutes) had lowest to highest LT50 (Table 2 and 3). The result also showed that among these insecticides, Lab strain is susceptible to Lambdacyhalothrin, deltamethrin, cyfluthrin and resistance to DDT according to WHO criteria that suggested (98–100% mortality indicates susceptibility, 90–97% mortality indicates resistance candidate (more investigation is needed or requires confirmation of resistance with other methods) and <90% mortality suggests resistance) (WHO 2013). And also cyfluthrin with LT50=45Sec and DDT with LT50=3005 were the most and least effect (Table 1,3 and Fig. 2,3).
Table 1.
Probit regression line parameters of lab strain of Culex pipiens exposed to different insecticides
| Insecticides | A | B ± SE | LT50, 95% C.I. (Second) | LT90, 95% C.I. (Second) | X2 (df) | P value |
|---|---|---|---|---|---|---|
| DDT 4% | −9.21 | 2.64± 0.31 | 2647 | 7061 | 3.56(3) | >0.05 |
| 3005 | 9156 | |||||
| 3455 | 13701 | |||||
| Lambdacyhalothrin 0.05% | −2.50 | 1.31±0.18 | 43 | 510 | 2.41(2) | >0.05 |
| 79 | 752 | |||||
| 120 | 1302 | |||||
| Deltamethrin 0.05% | −4.17 | 1.6± 0.16 | 255 | 1443 | 5.85 (4) | >0.05 |
| 326 | 1937 | |||||
| 406 | 2872 | |||||
| Cyfluthrin 0.15% | −1.84 | 1.17±0.18 | 14 | 308 | 3.60(4) | >0.05 |
| 36 | 448 | |||||
| 64 | 725 |
A= y-intercept, B= the slope of the line, SE= Standard error, CI= confidence interval, x2= heterogeneity about the regression line, df= degree of freedom, P> 0.05 = represent no heterogeneity in the population of tested mosquitos.
Table 2.
Probit regression line parameters of field population of Culex pipiens exposed to different insecticides
| Insecticides | A | B ± SE | LT50, 95% C.I. (Minute) | LT50, 95% C.I. (Minute) | X2 (df) | P value |
|---|---|---|---|---|---|---|
| Lambdacyhalothrin 0.05% | −7.58 | 3.71±0.36 | 99 | 214 | 5.34(2) | >0.05 |
| 111 | 245 | |||||
| 122 | 293 | |||||
| Deltamethrin 0.05% | −4.36 | 1.9± 0.35 | 152 | 511 | 0.37 (2) | >0.05 |
| 182 | 838 | |||||
| 234 | 2322 | |||||
| Cyfluthrin 0.15% | −2.29 | 1.59±0.23 | 21 | 117 | 3.47(2) | >0.05 |
| 27 | 172 | |||||
| 33 | 336 | |||||
| DDT 4%* | - | - | - | - | - | - |
No mortality after 24 hours exposure
Table 3.
Mortality rate and susceptibility status of Culex pipiens (Lab and field population) exposed to different insecticides at one hour exposure and 24 hours recovery period
| Insecticides | MR±EB* | Resistance status** | ||
|---|---|---|---|---|
| Lab strain | Field population | Lab strain | Field population | |
| Lambdacyhalothrin 0.05% | 100 | 20±2 | S | R |
| Deltamethrin 0.05% | 98±1 | 18±3 | S | R |
| Cyfluthrin 0.15% | 100 | 66±3 | S | R |
| DDT 4% | 55±3 | 0 | R | R |
Mortality Rate±Error Bar
R Resistance, S Susceptible
Fig. 2.
Regression lines for lab strain of Culex pipiens exposed to different insecticides
Fig. 3.
Regression lines for field population of Culex pipiens exposed to different insecticides
Discussion
In the present study four Insecticides including: DDT 4%, Lambdacyhalothrin 0.05%, Deltamethrin 0.05% and Cyfluthrin 0.15% were used for evaluatin the susceptibility status of Cx.pipiens According to WHO criteria lab starin was resistant to DDT and Filed strain exhibited resistant to all insecticides used. In the both strains a highly level of resistance to DDT were determined and also the LT50 for DDT >Deltamethrin > Lambdacyhalothrin >Cyfluthrin respectively. In the two previous studies conducted in Tehran, resistant to DDT have been reported in Cx. pipiens and Cx. quinquefasciatusin and these results was in parallel to our finding (Nazari and Janbakhsh 2000, Vatandoost et al. 2004). It seems that Cx. pipiens in the most part of the world has been resistant to DDT (Mukhopadhyay et al. 1993, Nazni et al. 2005, Corbel et al. 2007, Sarkar et al. 2009, Jones et al. 2012, Pocquet et al. 2013). In the study conducted by Nazni et al. (2005) mosquitoes from two field sites in Kuala Lumpur exhibited resistance to DDT with no mortality 24h after exposure, and this result was same to our result about field population (Nazni et al. 2005). In another study, high frequencies of resistance to DDT in Cx. quinquefasciatus from Benin have been reported and mortality rate ranged from 5 to 54% (Corbel et al. 2007). In northeastern India Cx. quinquefasciatus which caught from 7 different field sites of study area this species was resistance to DDT in all sites and its mortality rate varied from 11.9 to 50.0% (Sarkar et al. 2009). Result of susceptibility test in northwest and southeastern part of Iran indicated that this species is highly resistant to DDT (Ataie et al. 2015, Fathian et al. 2015). In the current study, Field population also was resistance to Lambdacyhalothrin, Deltamethrin and Cyfluthrin and in some same studies this result also reported, for example resistance to Lambdacyhalothrin and Cyfluthrin reported in the Southeastern part of Iran and resistance to Lambdacyhalothrin in Northwestern part of Iran (Ataie et al. 2015, Fathian et al. 2015). In Cx. quinquefasciatus from Wete on Pemba Island in Zanzibar resistance to Deltamethrin and Lambdacyhalothrin also have been reported (Jones et al. 2012). In Thailand, Cx. quinquefasciatus belong to The Baan Suan strain was highly resistant to Deltamethrin even its mortality was very lower than our results (Sathantriphop et al. 2006). Resistance to Deltamethrin also reported by Chen et al. (2010), so that all the six surveyed Cx. pipiens pallens populations strains were resistance to Deltamethrin and also their mortality Ranged from 20.2% to 78.6% (Chen et al. 2010). In some studies resistance to the others group of insecticides like organophosphates and Carbamate also have been reported (Bisset et al. 1999, Corbel et al. 2007, Tantely et al. 2010, Toma et al. 2011, Ataie et al. 2015 Fathian et al. 2015). for example in the both study that performed in Northwestern and Southern part of Iran, Cx. pipiens showed resistance to Propoxur (Ataie et al. 2015, Fathian et al. 2015). Tolerance to Deltamethrin (with mortality=86%) in Culex populations from Kilimani, Unguja Island in Zanzibar also reported by Jones et al. (2012). Although this populations was susceptible to Lambdacyhalothrin. Moreover in this study Culex from the nearby site of Tibirinzi in Pemba was relatively susceptible to Deltamethrin and also Lambdacyhalothrin (Jones et al. 2012). In the same previously study that performed by Vatandoost et al in 2004, field population of Cx. Quinquefasciatus which collected from Sewage System of Tehran after evaluating their susceptibly status to insecticides result showed that this species is susceptible to Cyfluthrin and also have tolerance to Lambdacyhalothrin and Deltamethrin. Routine use of pesticides in Household and agricultural pest control might have developed this Enhanced Tolerance to insecticide in the wastewater mosquito, Cx. Quinquefasciatus (Vatandoost et al. 2004).
Conclusion
In the present study, in the population whitch collected from field highly resistance to all insecticides exhibited it might be due to pollution of wastewater with chemical substances Findings of this research could provide a clue for logical operations of future chemical control program. Next step of this research will focus on the biochemical and molecular investigation.
Acknowledgements
This article is a part of the first author's dissertation for fulfillment of a PhD degree in Medical Entomology and Vector Control from Department of Medical Entomology and Vector Control, School of Public Health, Tehran University of Medical Sciences, Tehran, Iran. This study was financially supported by the Deputy of Research, Tehran University of Medical Sciences. The authors declare that there is no conflict of interest.
References
- Abai MR, Mehravaran A, Vatandoost H, Oshaghi MA, Javadian E, Mashayekhi M, Mosleminia A, Piyazak N, Edallat H, Mohtarami F, Jabbari H, Rafi F. (2008) Comparative performance of imagicides on Anopheles stephensi, main malaria vector in a malarious area, southern Iran. J Vector Borne Dis. 45(4): 307–312. [PubMed] [Google Scholar]
- Abbott WS. (1965) A method of comparing the effectiveness of an insecticide. J Econ Entomol. 18: 265–267. [Google Scholar]
- Ataie A, Moosa-Kazemi SH, Vatandoost H, Yaghoobi-Ershadi MR, Bakhshi H, Anjomruz M. (2015) Assessing the Susceptibility Status of Mosquitoes (Diptera: Culicidae) in a Dirofilariasis Focus, Northwestern Iran. J Arthropod-Borne Dis. 9(1): 7–21. [PMC free article] [PubMed] [Google Scholar]
- Azari-Hamidian S, Yaghoobi-Ershadi MR, Javadian E, Abai MR, Mobedi I, Linton YM, Harbach RE. (2009) Distribution and ecology of mosquitoes in a focus of dirofilariasis in northwestern Iran, with the first finding of filarial larvae in naturally infected local mosquitoes. Med Vet Entomol. 23(2): 111–121. [DOI] [PubMed] [Google Scholar]
- Azari-Hamidian S, Yaghoobi-Ershadi MR, Javadian E, Mobedi I, Abai MR. (2007) Review of dirofilariasis in Iran. J Med Fac Guilan Univ Med Sci. 15(60: 102–113 (In Persian). [Google Scholar]
- Ben Cheikh H, Ben Ali-Haouas Z, Marquine M, Pasteur N. (1998) Resistance to organophosphorus and pyrethroid insecticides in Cx. pipiens (Diptera: Culicidae) from Tunisia. J Med Entomol. 35: 251–260. [DOI] [PubMed] [Google Scholar]
- Bisset JA, Rodriguez MM, Diaz C, Alain Soca L. (1999) Characterization of resistance to organophosphate insecticides, carbamates, and pyrethroids in Culex quinquefasciaus from the State of Miranda, Venzuela. Rev Cubana Med Trop. 51(2): 89–94. [PubMed] [Google Scholar]
- Bisset J, Rodríguez M, Díaz C, Ortiz E, Marquetti M, Hemingway J. (1990) The mechanisms of organophosphate and carbamate resistance in Culex quinquefasciatus (Diptera: Culicidae) from Cuba. Bull Entomol Res. 80(3): 245–250. [Google Scholar]
- Calhoun LM, Avery M, Jones L, Gunarto K, King R, Roberts J, Burkot TR. (2007) Combined sewage overflows (CSO) are major urban breeding sites for Culex quinquefasciatus in Atlanta, Georgia. Am J Trop Med Hyg. 77: 478–484. [PubMed] [Google Scholar]
- Chen L, Zhong D, Zhang D, Shi L, Zhou G, Gong M, Zhou H, Sun Y, Ma L, He J, Hong S, Zhou D, Xiong C, Chen C, Zou P, Zhu C, Yan G. (2010) Molecular ecology of pyrethroid knockdown resistance in Culex pipiens pallens mosquitoes. PloS one. 5(7): e11681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Corbel V, N'Guessan R, Brengues C, Chandre F, Djogbenou L, Martin T, Akogbéto M, Hougard JM, Rowland M. (2007) Multiple insecticide resistance mechanisms in Anopheles gambiae and Culex quinquefasciatus from Benin, West Africa. Acta Trop. 101: 207–216. [DOI] [PubMed] [Google Scholar]
- Davidson G. (1964) DDT resistance and dieldrin resistance in Cx. pipiens fatigans. Ann Trop Med Parasitol. 58: 180–188. [DOI] [PubMed] [Google Scholar]
- Enayati AA, Vatandoost H, Ladonni H, Townson H, Hemingway J. (2003) Molecular evidence for a kdr-like pyrethroid resistance mechanism in the malaria vector mosquito Anopheles stephensi. Med Vet Entomol. 17(2):138–144. [DOI] [PubMed] [Google Scholar]
- Fathian M, Vatandoost H, Moosa-Kazemi SH, Raeisi A. (2015) Susceptibility of Culicidae Mosquitoes to Some Insecticides Recommended by WHO in a Malaria Endemic Area of Southeastern Iran. J Arthropod-Borne Dis. 9(1): 22–34. [PMC free article] [PubMed] [Google Scholar]
- Finney DJ. (1971) Probit analysis, III edn Cambridge University Press, Cambridge. [Google Scholar]
- Golestani J. (1967) The methods of the mosquito Culex control in Tehran City. J General Med Tehran Univ Med School. 6: 376–379. (In Persian). [Google Scholar]
- Hanafi-Bojd AA, Vatandoost H, Jafari R. (2006) Susceptibility status of Anopheles dthali and An. fluviatilis to commonly used larvicides in an endemic focus of malaria, southern Iran. J Vector Borne Dis. 43(1): 34–38. [PubMed] [Google Scholar]
- Hanafi-Bojd AA, Vatandoost H, Oshaghi MA, Haghdoost AA, Shahi M, Sedaghat MM, Yeryan M, Pakari A. (2012) Entomological and epidemiological attributes for malaria transmission and implementation of vector control in southern Iran. Acta Trop. 121: 85–92. [DOI] [PubMed] [Google Scholar]
- Hanafi-Bojd AA, Vatandoost H, Philip E, Stepanova E, AI Abdi A, Safari R, Mohseni GH, Bruhi MI, Peter A, Abdulrazag SH, Mangal G. (2010) Malaria situationanalysis and stratification in Bandar Abbas County, Southern Iran, 2004– 2008. Iran J Arthropod-Borne Dis. 4: 31–41. [PMC free article] [PubMed] [Google Scholar]
- Horsfall WR. (1955) Mosquitoes: Their Bionomics and Relation to Disease. Hafner publishing, New York, pp.723. [Google Scholar]
- Jones CM, Machin C, Mohammed K, Majambere S, Ali AS, Khatib BO, Kelly-Hope LA. (2012) Insecticide resistance in Culex quinquefasciatus from Zanzibar: implications for vector control programmes. Parasit Vectors. 5: 78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lines JD. (1988) Do agricultural insecticides select for insecticide resistance in mosquitoes: A look at the evidence Parasitol Today. 4: S17–S20. [DOI] [PubMed] [Google Scholar]
- Lotfi MD. (1976) Key to Culicinae of Iran, genus Culex and their biology (Diptera: Culicidae). Iranian J Publ Health. 5: 71–84. [Google Scholar]
- Lotfi MD., Manouchehri AV, Yazdanpanah H. (1975) Resistance of Cx. pipiens pipiens to DDT in Northern Iran, 1973. Bull Soc Pathol Exot Filiales. 68(1): 91. [PubMed] [Google Scholar]
- Martinez-Torres D, Chevillon C, Brun-Barale A, Berge JB, Pasteur N, Pauron D. (1999) Voltage-dependent Na+ channels in pyrethroid-resistant Cx. pipiens L mosquitoes. Pestic Sci. 55: 1012–1020. [Google Scholar]
- Mitchell CJ, Francy DB, Monath TP. (1980) Arthropod vectors. In: Monath TP, Reeves WC, editors. St. Louis Encephalitis. Washington: American Public Health Association; 313–379. [Google Scholar]
- Mukhopadhyay AK, Sinha SN, Yadav RL, Narasimham MV. (1993) Susceptibility status of Culex quinquefasciatus in Patna to insecticides. Indian J Public Health. 37(2): 57–60. [PubMed] [Google Scholar]
- Mullen GR, Durden L. (2009) Medical and Veterinary Entomology, Mosquitoes (Culicidae) Woodbridge A. Foster and Edward D Walter. Vol. 2 Elsevier, Burlington, pp. 207–260. [Google Scholar]
- Naficy K, Saidi S. (1970) Serological survey on viral antibodies in Iran. Trop Geogr Med. 22: 183–188. [PubMed] [Google Scholar]
- Nazari M, Janbakhsh B. (2000) a survey of the susceptibility level of Culex theileri and Cx. pipiens to DDT, Dieldrin, Propoxur and Malathion in the southern area of Tehran. J Uromia Univ Med Sci. 11(1): 13–19. [Google Scholar]
- Nazni WA, Lee HL, Azahari AH. (2005) Adult and larval insecticide susceptibility status of Culex quinquefasciatus (Say) mosquitoes in Kuala Lumpur, Malaysia. Trop Biomed. 22: 63–68. [PubMed] [Google Scholar]
- Oshaghi MA, Vatandoost H, Gorouhi A, Abai MR, Madjidpour A, Arshi S, Mehravaran A. (2011) Anopheline species composition in borderline of Iran, Azerbaijan. Acta trop. 119(1): 44–49. [DOI] [PubMed] [Google Scholar]
- Pocquet N, Milesi P, Makoundou P, Unal S, Zumbo B, Atyame C, Darriet F, Dehecq J, Thiria J, Bheecarry A, Iyaloo D, Weill M, Chandre F, Labbé P. (2013) Multiple Insecticide Resistances in the Disease Vector Culex quinquefasciatus from Western Indian Ocean. PLoS One. 8(10): e77855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sarkar M, Bhattacharyya I, Borkotoki A, Goswami D, Rabha B, Baruah I, Srivastava RB. (2009) Insecticide resistance and detoxifying enzyme activity in the principal bancroftian filariasis vector, Culex quinquefasciatus, in northeastern India. Med vet entomol. 23(2): 122–131. [DOI] [PubMed] [Google Scholar]
- Sathantriphop S, Paeporn P, Supaphathom K. (2006) Detection of insecticides resistance status in Culex quinquefasciatus and Aedes aegypti to four major groups of insecticides. Trop Biomed. 23: 97–101. [PubMed] [Google Scholar]
- Savage HM, Aggarwal D, Apperson CS, Katholi CR, Gordon E, Hassan HK, Unnasch TR. (2007) Host choice and West Nile virus infection rates in blood-fed mosquitoes, including members of the Cx. pipiens complex, from Memphis and Shelby County, Tennessee, 2002–2003. Vector Borne Zoonotic Dis. 7: 365–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Service MW. (2003) Medical Entomology for Students. Vol. 3 United Kingdom: Cambridge. University Press, Cambridge. [Google Scholar]
- Shahi M, Vatandoost H, Abaei MR, Hanafi-Bojd AA. (2006) Susceptibility of Anopheles fluviatilis James to different insecticides in Bandar Abbas township, 2003. Hormozgan Med J. 10(4): 321–328. [Google Scholar]
- Smith JL, Fonseca DM. (2004) Rapid assays for identification of members of the Culex (Culex) pipiens complex, their hybrids, and other sibling species (Diptera: Culicidae). Am J Trop Med Hyg. 70: 339–345. [PubMed] [Google Scholar]
- Soltani A, Vatandoost H, Oshaghi MA, Enayati AA, Raeisi A, Eshraghian MR, Rafi F. (2013) Baseline Susceptibility of Different Geographical Strains of Anopheles stephensi (Diptera: Culicidae) to Temephos in Malarious Areas of Irana J Arthropod-Borne Dis. 7(1): 56–65. [PMC free article] [PubMed] [Google Scholar]
- Strickman D, Fonseca DM. (2012) Autogeny in Cx. pipiens complex mosquitoes from the San Francisco bay area. Am J Trop Med Hyg. 87(4): 719–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tantely ML, Tortosa P, Alout H, Berticat C, Berthomieu A, Rutee A, Weill M. (2010) Insecticide resistance in Cx. pipiens quinquefasciatus and Aedes albopictus mosquitoes from La Reunion Island. Insect Biochem Mol Biol. 40: 317–324. [DOI] [PubMed] [Google Scholar]
- Toma L, Menegon M, Romi R, De Matthaeis E, Montanari M, Severini C. (2011) Status of insecticide resistance in Culex pipiens field populations from northeastern areas of Italy before the withdrawal of OP compounds. Pest Manag Sci. 67(1): 100–106. [DOI] [PubMed] [Google Scholar]
- Vatandoost H, Borhani N. (2004) Susceptibility level and irritability of synthetic pyrethroids against main malaria vectors in the endemic areas of Iran. Acta Med Iran. 42: 247–255. [Google Scholar]
- Vatandoost H, Hanafi-Bojd AA. (2005) Current Resistant Status of Anopheles stephensi Liston to Different Larvicides in Hormozgan Province, Southeastern Iran, 2004. Pak J Biol Sci. 8: 1568–1570. [Google Scholar]
- Vatandoost H, Mashayekhi M, Abaie MR, Aflatoonian MR, Hanafi-Bojd AA, Sharifi I. (2005) Monitoring of insecticides resistance in main malaria vectors in a malarious area of Kahnooj district, Kerman Province, southeastern Iran. J Vector Borne Dis. 42(3): 100–108. [PubMed] [Google Scholar]
- Vatandoost H, Ezeddinloo L, Mahvi AH, Abai MR, Kia EB, Mobedi I. (2004) Enhanced tolerance of house mosquito to different insecticides due to agricultural and household pesticides in sewage system of Tehran, Iran. Iranian J Environ Health Sci Eng. 1(1): 42–45. [Google Scholar]
- Vinogradova EB. (2000) Cx. pipiens pipiens Mosquitoes: Taxonomy, Distribution Ecology, Physiology, Genetics and Control. Pensoft Publisher, Sofia. [Google Scholar]
- WHO (1981) Instruction for determining the susceptibility or resistance of adult mosquitoes to organochlorine, organ-phosphate and carbamate insecticides. Diagnostic test. WHO/VBC.81.806.
- WHO (2013) Test procedures for insecticide resistance monitoring in malaria vector mosquitoes. World Health Organization, Geneva, Switzerland. [Google Scholar]