Abstract
Tourniquets are routinely and safely used in limb surgeries throughout the world. Tourniquet application alters normal physiology. Healthy patients tolerate these physiological changes well, but the physiological changes may not be well-tolerated by patients with poor cardiac function. This review discusses the physiological changes associated with tourniquet use, safe practice and provides the latest updates regarding tourniquet use. A systematic literature search of PubMed, MEDLINE, ScienceDirect, and Google Scholar was done. The search results were limited to the randomized controlled trials and systemic reviews. The papers are summarized in this review.
Key words: Complications, deflation, limb surgeries, tourniquet, tourniquet inflation
Introduction
Tourniquet use is a common practice in orthopedic and plastic surgeries. They are compressive devices that occlude blood flow to the limbs to create bloodless surgical field and decrease the perioperative blood loss. They are also used for intravenous regional anesthesia (Bier's block) to prevent the central spread of local anesthetics. Tourniquet usage is associated with several complications and over the years it has undergone various modifications to improve the safety.[1] Its use has been associated with several physiological alterations that can affect patient outcome following surgery. The operating team including the anesthetist should therefore have correct knowledge about its application. This review discusses the physiological changes associated with tourniquet use and safety practices, and provides the latest updates regarding tourniquet use.
History
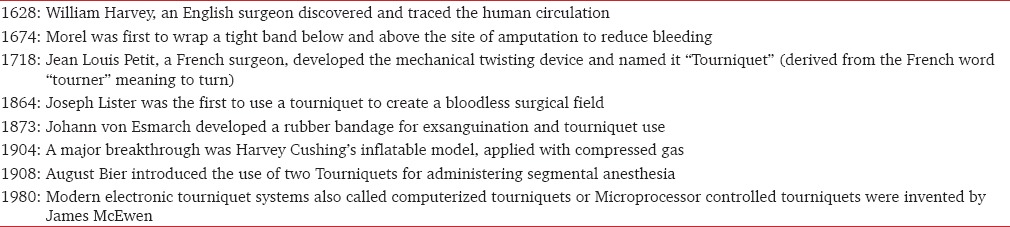
The tourniquet was first used in ancient times as a life-saving and limb saving devise during injuries. However, tourniquet has been defined as a limb-threatening device in some occasions when it is misused. The history of using tourniquets belonged to the middle ages when a tight band was first used on injured soldiers at the Battle of Flanders in 1674. The use of tight bands continued to develop through many stages until we reached the modern design of tourniquet [Table 1].[1,2]
Table 1.
Some stages of development of tourniquet
Definition of Tourniquets
A tourniquet is a constricting or compressing device used to control venous and arterial circulation to an extremity for a period of time.[3]
Types of tourniquets
Emergency tourniquets
A tightly tied band applied around a limb (upper or lower) to prevent severe blood loss from limb trauma during emergency. It should be used as a last resort to control bleeding. Emergency tourniquets are widely used by the military to save lives during combat.
Surgical tourniquets
Surgical tourniquets enable the surgeons to work in a bloodless operative field by preventing blood flow to a limb and allow surgical procedures to be performed with improved accuracy, safety, and speed. They have two basic designs – noninflatable and inflatable. Frequently the two types of tourniquets are used together in orthopedic and plastic surgery, such as in intravenous regional anesthesia (Bier block anesthesia).
Noninflatable (nonpneumatic) tourniquets
Noninflatable tourniquets are made of rubber or elastic cloth. Now-a-days, their surgical use alone is limited because they have been replaced by modern tourniquet systems.
Pneumatic tourniquet
Pneumatic tourniquets use compressed gas to inflate a bladder or cuff to occlude or restrict blood flow. A regulating device on the tourniquet machine can control the amount of cuff pressure exerted on the limb. The pressure is provided by an electrically driven pump or by a central compressed air supply.[3,4]
Components of pneumatic tourniquets
The five basic components are:
An inflatable cuff (bladder)
A compressed gas source
A pressure display
A pressure regulator
Connection tubing.
Inflatable Cuff
Pressure is exerted on the circumference of an extremity by means of compressed gas, which is introduced into a bladder within the tourniquet cuff. Different types of cuffs are available, and the appropriate choice is determined primarily by proper fit and surgical procedures. When selecting a cuff, the following criteria are considered:[4]
Cuff location
Single- versus dual-bladder design
Cuff shape
Cuff length
Cuff width
Disposable versus reusable cuffs
Specialty applications
Limb protection
The length and width of the tourniquet cuff should be individualized — considering the size and circumference of the patient's limb. The tourniquet cuff should overlap at least three inches but not more than 6 inches.[4] Too much overlap causes increased pressure and rolling or wrinkling of underlying soft tissue. Too small overlap compromises effective tourniquet inflation and can result in unexpected release or inadequate constriction.
The width of the cuff should be wider than half the limb's diameter. Wider cuffs minimize the risk of injury to underlying tissue by dispersing pressure over a greater surface area.[4] Wider cuffs have been found to consistently occlude blood flow at a lower pressure in adults and children.[4]
Tourniquets should be positioned on the limb at the point of the maximum circumference.[5,6] A soft padding should be placed around the limb before application of the tourniquet. It can help reduce wrinkling, pinching, and shearing of the soft tissues. The cuff tubing should be positioned on or near the lateral aspect of the extremity to avoid pressure on nerves and kinking of the tubing.
Tourniquet Cuff Pressure
The pressure to which a tourniquet cuff should be inflated depends on a number of variables: The patient's age, skin, blood pressure, shape and size of the extremity, and the dimensions of the cuff. The tourniquet pressure should be minimized in the effort to produce a bloodless surgical field. Lower pressures are thought to prevent injury of normal tissue. Despite many years of tourniquet use, the optimal inflation pressure to accomplish this objective is not yet established by a research study. Surgical texts recommend cuff pressures of 200–300 mmHg for adults. Various methods have been implemented in an effort to lower effective cuff pressure:[7,8,9,10,11,12,13]
Double tourniquet technique, to change the point of compression[7]
Controlled hypotension to bring down systolic blood pressure can also be used to decrease direct cuff pressure against the tissue[8]
Doppler technique and pulse oximetry to confirm the absence of the arterial pulse to determine the minimum inflation pressure[9]
Tourniquet inflation based on limb occlusion pressure (LOP)[10,11]
Cuff pressure synchronization with systolic blood pressure.[11,12,13]
Limb occlusion pressure
LOP can be defined as the minimum pressure required to stop the flow of arterial blood into the limb distal to the cuff. LOP is determined by gradually increasing tourniquet pressure until distal blood flow is interrupted. According to the guidelines from the Association of Perioperative Registered Nurses,[14] cuff inflation pressure should be adjusted by adding a safety margin to the LOP as follows:
Add 40 mmHg for LOP <130 mmHg
Add 60 mmHg for LOP between 131 and 190 mmHg
Add 80 mmHg for LOP >190 mmHg
For pediatric patients, adding 50 mmHg has been recommended.
The LOP should be measured during preoperative check-up or when the blood pressure is stabilized after induction of anesthesia. The risk of tourniquet related complications can be significantly reduced by measuring the LOP and selecting cuff inflation pressures accordingly.[15] Best practice recommends that optimal cuff pressure should be based on the patient's systolic blood pressure or LOP.[16]
Inflation of the tourniquet cuff should be under the direction of the surgeon and coordinated with the anesthetist because it facilitates patient management during the rapid physiologic changes caused before and after limb exsanguination and cuff inflation.
Exsanguination before inflation of the tourniquet improves the quality of the bloodless field and minimizes pain associated with tourniquet use. It is normally done by limb elevation or using an elastic wrap of the extremity. Elastic wraps should not be used if any of the following is present: Infection, malignant tumor, fractures, or thrombi in the extremity. Application of the wrap can force the thrombi, infection or malignant cells into the circulation. In these cases, exsanguination should be accomplished by extremity elevation alone. Exsanguination and the use of tourniquets are both controversial in patients with sickle cell disease.[17]
Pneumatic tourniquets should be inflated rapidly because rapid inflation occludes arteries and veins almost simultaneously preventing the filling of superficial veins before occlusion of arterial blood flow.
Inflation or occlusion time
Inflation time should be kept to a minimum to minimize risks to the patient. Safe tourniquet inflation time has not been accurately determined. The time varies with the patient's age, physical status, and the vascular supply to the extremity. No strict guidelines exit. A safe time limit of 1–3 h has been described. It has been recommended to assess the operative situation at 2 h and if the anticipated duration is >2.5 h then use a 10-min deflation interval at that point and at subsequent 1-h intervals.[18] In pediatric patients, inflation time of <75 min has been recommended for lower extremities.[19,20]
Cuff deflation
Tourniquet deflation causes release of anaerobic metabolites into the systemic circulation causing hypotension, metabolic acidosis, hyperkalemia, myoglobulinemia, myoglobinuria, and possible renal failure. It is also known as “myonephropathic metabolic syndrome,” and it depends on the size of the extremity, duration of tourniquet time, and overall physiologic status of the patient.[20]
Tourniquet related complications
Tourniquet related complications or side effects are either local or systemic.
Localized complications now follow.
Nerve injuries
Nerve injuries related to tourniquet application range from paresthesia to paralysis. Nerve tissues are less vulnerable to acute injury compared to skeletal muscle. The incidence is estimated to be 1:6200 for the upper limb and 1:3700 for the lower limb. The overall incidence of permanent injury is 0.032%.[21]
The nerve injury is maximum at the proximal and distal edges of the cuff where the shear stress is greatest. Nerve injuries are more common in the upper limb than lower limb. The most common upper limb nerve injury is that of radial nerve, followed by the ulnar and median nerves. The common peroneal nerve is the most commonly injured lower extremity nerve.
The pathophysiologic cause of nerve injury following tourniquet is thought to be a combination of compression and ischemia. It is thought compression plays a more important role. Compression of the nerve by the cuff causes intraneural microvascular abnormalities in the parts of the nerve adjacent to the cuff. Edema results and leads to compromised tissue nutrition and axonal degeneration. Nerve injuries are more common with the use of Esmarch bandage than with a pneumatic tourniquet. The Esmarch bandage can generate pressures as high as 1000 mmHg.[22] The prognosis of tourniquet induced nerve injuries is generally good-permanent deficits are rare, and most injuries will heal spontaneously within 6 months.[21,22]
Muscle injury
Muscle injury following the application of the tourniquet is due to the combined effect of ischemia and mechanical deformation of the tissue. The ischemia and compression lead to metabolic and microvascular changes. These changes become more profound as the duration of the tourniquet inflation increases. Intracellular concentrations of creatine phosphate, glycogen, oxygen, and ATP are exhausted by 3 h.[22,23]
Tourniquet induced ischemia and reperfusion generate hydrogen peroxide and cause increased xanthine oxidase activity in local and systemic blood which contributes to the injury of skeletal muscle, myocardium, kidneys, and lungs after ischemia and reperfusion.
Vascular injury
Direct vascular injury is an uncommon complication of tourniquet use. It occurs most commonly in children, obese, elderly, and patients with peripheral vascular disease.
Skin injury
Skin injuries are uncommon, but excessive tourniquet time or poorly placed tourniquets may result in cutaneous abrasions, blisters and even pressure necrosis. The highest risk of skin injury occurs in: Children, obese, elderly, and patients with peripheral vascular disease.
Systemic Effects
Cardiovascular effects
Cardiovascular changes occur during all phases of tourniquet application from exsanguination to deflation. Limb exsanguination and tourniquet inflation increase blood volume and systemic vascular resistance that ultimately cause a transient increase in central venous pressure. This fluid shift can augment central venous pressure and also blood volume by 15% that can be up to 800 ml following exsanguination of both legs.[2,24,25] Hemodynamic changes associated with tourniquet use are minimal in healthy patients, but patients with poor cardiac function may not tolerate these changes. Heart rate, systolic, and diastolic pressures may increase after 30–60 min of tourniquet inflation due to ischemia and tourniquet pain. These changes persist until tourniquet deflation and poorly respond to analgesic drugs or increasing the depth of anesthesia. Many interventions have been reported to reduce cardiovascular stress:[24,25,26,27,28,29,30,31,32] Ketamine, dexmedetomidine, magnesium sulfate, clonidine, and remifentanil infusion.
Tourniquet deflation is a critical stage because it causes sudden drop in central venous pressure and mean arterial pressures. Cardiac arrests have been reported following cuff deflation.[24,25,26,27] These hemodynamic changes are due to the combination of a shift in blood volume back into the limb and washout of metabolites from the ischemic limb into the systemic circulation. Hemodynamic changes are more marked with the simultaneous use of tourniquets on both lower limbs.
Respiratory effects
Respiratory changes are rare and mainly seen during the deflation of the tourniquet. It is associated with transient increase in end-tidal carbon dioxide (EtCO2) tension due to efflux of hypercapnic venous blood and metabolites into the systemic circulation.[24,25] The increase in EtCO2 is related to the duration of ischemia. EtCO2 increase is also greater with the lower limb tourniquet and in men than in women, because of a man's greater muscle bulk. The EtCO2 peaks at 1–3 min, returning to baseline at 10–13 min in a spontaneously breathing patient but takes longer in mechanically ventilated patients unless the minute volume is increased.[25,26,27]
Cerebral circulatory effects
Cerebral circulatory changes are secondary to increase in EtCO2 after tourniquet deflation that increases the cerebral blood flow in 2 min and returns to baseline within 10 min. Patients with reduced intracranial compliance may be at higher risk for adverse effects related to the increase in cerebral blood flow. Maintaining normocapnia can prevent this increase in cerebral blood flow during deflation.[33,34,35]
Hematological effects
Tourniquet use induces changes in both coagulability and fibrinolysis. Tourniquet inflation during surgery is associated with a hypercoagulable state that is due to increased platelet aggregation and stimulation of coagulation factors caused by tissue damage and catecholamines released in response to pain from surgery and the tourniquet application.[36,37,38,39]
There is a brief period of increased fibrinolytic activity due to the release of tissue plasminogen activator, activating the anti-thrombin III and thrombomodulin — protein C anticoagulant system after the deflation of the tourniquet. This acts as one of the contributors in posttourniquet bleeding. The increase in fibrinolysis is maximal at 15 min and returns to preoperative levels within 30 min of tourniquet release.[39,40]
Tourniquet use in hematological disorders such as sickle cell disorder is controversial.[17] In sickle cell disease, sickling is precipitated by circulatory stasis, acidosis, and hypoxemia, all of which happen during the use of a tourniquet. Available evidence suggests that with proper necessary precautions, tourniquets may be used with no relative harmful effects in most patients with sickle cell disease.[41]
Metabolic Changes
Limb occlusion causes metabolic changes in the ischemic limb that include: Increased lactic acid, PaCO2 and potassium levels, and decreased levels of PaO2, and pH. Toxic metabolites produce pathophysiological changes when released into the general circulation.[10,22,23,24] The degree of these changes correlates with the duration of ischemia. All of these changes are fully reversed within 30 min of tourniquet deflation. Metabolic changes are more pronounced when bilateral tourniquets are used.
Temperature Changes
Tourniquet inflation and deflation cause alteration of body temperature. Core body temperature gradually increases following tourniquet application as the available surface area for heat loss decreases resulting in less heat transfer from the central to the peripheral compartment. Deflation leads to a transient fall in core temperature due to the redistribution of body heat and hypothermic blood from the ischemic limb. Maintenance of core body normothermia during surgery reduces this decline in temperature.[42,43]
Tourniquet Pain
Tourniquet pain is described as a poorly localized, dull, tight, aching sensation at the site of tourniquet application. During general anesthesia, it manifests as an increase in heart rate and mean arterial pressure. It is more common under general anesthesia (53–67%) and occurs most often during lower-limb surgeries. The exact etiology is unclear, but it is thought to be due to a cutaneous neural mechanism.[44] The pain is thought to be mediated by the unmyelinated, slow conducting C fibers that are usually inhibited by the A-delta fibers. The A-delta fibers are blocked by mechanical compression after about 30 min, while the C fibers continue to function. Tourniquet compression leads to release of prostaglandins by the injured cells. These prostaglandins increase pain perception by sensitizing and exciting pain receptors. Also, limb ischemia causes central sensitization via NMDA receptor activation due to repeated nociceptive afferent input from the affected limb.[45,46]
Tourniquet pain has important impacts on anesthesia. Many techniques[27] like application of EMLA cream, infiltration with local anesthetics, use of wider cuff with lower inflation pressure, addition of opioids, clonidine, epinephrine along with local anesthetics in spinal block have been tried in order to decrease the incidence or severity of this pain but none has attained complete success in pain relief. Intravenous drugs,[24,25,27,28,29,30,31,32,47] ketamine, dexmedetomidine, magnesium sulfate, clonidine remifentanil infusions have also been studied, and the only thing that works reliably is tourniquet deflation.
Pharmacological Effects
Tourniquet inflation isolates the limb from the rest of the body and can alter the volume of distribution of some medications resulting in alteration of the pharmacokinetics of anesthetic drugs. The clinical significance of such variation in drug pharmacokinetics has not been studied but is thought to be limited.
The time interval between antibiotic administration and tourniquet inflation is important for antibiotic prophylaxis during surgery, but there are no specific guidelines. Orthopedic surgery guidelines suggests that the antibiotic must be completely infused prior to the inflation of the tourniquet.[48] The clinical evidence has suggested that prophylactic antibiotics need to be given at least 5–10 min before tourniquet inflation to allow good tissue penetration.[48,49,50]
Contraindications
There are no absolute contraindications to tourniquet application, but adequate care should be taken in the following group of patients:
Severe peripheral vascular disease
Sickle cell disease
Severe crush injury
Diabetic neuropathic patients
Patients with history of deep vein thrombosis and pulmonary embolism
Conclusion
Arterial tourniquets are widely used in surgery, and can have significant systemic as well as local effects on the body. It is therefore important for us to be aware of the physiological effects of tourniquets and there implications in anesthesia as they may affect any system in the body. Complications are rare, but if they occur, can be devastating.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Murphy CG, Winter DC, Bouchier-Hayes DJ. Tourniquet injuries: Pathogenesis and modalities for attenuation. Acta Orthop Belg. 2005;71:635–45. [PubMed] [Google Scholar]
- 2.Deloughry JL, Griffiths R. Arterial tourniquets. Contin Educ Anaesth Crit Care Pain. 2009;9:56–60. [Google Scholar]
- 3.McEwen JA. Tourniquet use. [Last accessed on 2014 Jun-Jul]. Available from: http://www.tourniquets.org/lop.php .
- 4.Recommended Practices for the Use of the Pneumatic Tourniquet in the Perioperative Practice Setting. AORN Guidelines on Use of Pneumatic Tourniquets. 2009:373–85. [Google Scholar]
- 5.Maury AC, Roy WS. A prospective, randomized, controlled trial of forearm versus upper arm tourniquet tolerance. J Hand Surg Br. 2002;27:359–60. doi: 10.1054/jhsb.2002.0787. [DOI] [PubMed] [Google Scholar]
- 6.Odinsson A, Finsen V. The position of the tourniquet on the upper limb. J Bone Joint Surg Br. 2002;84:202–4. doi: 10.1302/0301-620x.84b2.12777. [DOI] [PubMed] [Google Scholar]
- 7.Tuncali B, Karci A, Bacakoglu AK, Tuncali BE, Ekin A. Controlled hypotension and minimal inflation pressure: A new approach for pneumatic tourniquet application in upper limb surgery. Anesth Analg. 2003;97:1529–32. doi: 10.1213/01.ANE.0000081660.97731.91. [DOI] [PubMed] [Google Scholar]
- 8.Dreyfuss UY, Smith RJ. Sensory changes with prolonged double-cuff tourniquet time in hand surgery. J Hand Surg Am. 1988;13:736–40. doi: 10.1016/s0363-5023(88)80137-0. [DOI] [PubMed] [Google Scholar]
- 9.Noordin S, McEwen JA, Kragh JF, Jr, Eisen A, Masri BA. Surgical tourniquets in orthopaedics. J Bone Joint Surg Am. 2009;91:2958–67. doi: 10.2106/JBJS.I.00634. [DOI] [PubMed] [Google Scholar]
- 10.Oragui E, Parsons A, White T, Longo UG, Khan WS. Tourniquet use in upper limb surgery. Hand. 2011;6:165–73. doi: 10.1007/s11552-010-9312-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sato J, Ishii Y, Noguchi H, Takeda M. Safety and efficacy of a new tourniquet system. BMC Surg. 2012;12:17. doi: 10.1186/1471-2482-12-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ishii Y, Noguchi H, Matsuda Y, Takeda M, Higashihara T. A new tourniquet system that determines pressures in synchrony with systolic blood pressure. Arch Orthop Trauma Surg. 2008;128:297–300. doi: 10.1007/s00402-007-0446-0. [DOI] [PubMed] [Google Scholar]
- 13.Tuncali B, Karci A, Tuncali BE, Mavioglu O, Ozkan M, Bacakoglu AK, et al. A new method for estimating arterial occlusion pressure in optimizing pneumatic tourniquet inflation pressure. Anesth Analg. 2006;102:1752–7. doi: 10.1213/01.ane.0000209018.00998.24. [DOI] [PubMed] [Google Scholar]
- 14.Perioperative Standards and Recommended Practices. Denver, CO: AORN, Inc; 2013. Recommended practices for care of patients undergoing pneumatic tourniquet-assisted procedures; pp. e25–e50. [Google Scholar]
- 15.Guay J. Adverse events associated with intravenous regional anesthesia (Bier block): A systematic review of complications. J Clin Anesth. 2009;21:585–94. doi: 10.1016/j.jclinane.2009.01.015. [DOI] [PubMed] [Google Scholar]
- 16.Hicks RW, Denholm B. Implementing AORN recommended practices for care of patients undergoing pneumatic tourniquet-assisted procedures. AORN J. 2013;98:383–93. doi: 10.1016/j.aorn.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 17.Wilson M, Forsyth P, Whiteside J. Haemoglobinopathy and sickle cell disease. Contin Educ Anaesth Crit Care Pain Oxford J. 2010;10:24–8. [Google Scholar]
- 18.Fitzgibbons PG, Digiovanni C, Hares S, Akelman E. Safe tourniquet use: A review of the evidence. J Am Acad Orthop Surg. 2012;20:310–9. doi: 10.5435/JAAOS-20-05-310. [DOI] [PubMed] [Google Scholar]
- 19.Standards, Guidelines, and Position Statements for Perioperative Registered Nursing Practice ORNAC Safety/Risk Prevention and Management. 2011 Mar [Google Scholar]
- 20.Sharma JP, Salhotra R. Tourniquets in orthopedic surgery. Indian J Orthop. 2012;46:377–83. doi: 10.4103/0019-5413.98824. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mingo-Robinet J, Castañeda-Cabrero C, Alvarez V, León Alonso-Cortés JM, Monge-Casares E. Tourniquet-related iatrogenic femoral nerve palsy after knee surgery: Case report and review of the literature. Case Rep Orthop. 2013;2013:368290. doi: 10.1155/2013/368290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Van der Spuy LA. Complications of the arterial tourniquet. South Afr J Anaesth Analg. 2012;18:14–8. [Google Scholar]
- 23.Shadgan B, Reid WD, Harris RL, Jafari S, Powers SK, O'Brien PJ. Hemodynamic and oxidative mechanisms of tourniquet-induced muscle injury: Near-infrared spectroscopy for the orthopedics setting. J Biomed Opt. 2012;17:081408–1. doi: 10.1117/1.JBO.17.8.081408. [DOI] [PubMed] [Google Scholar]
- 24.Estebe JP, Davies JM, Richebe P. The pneumatic tourniquet: Mechanical, ischaemia-reperfusion and systemic effects. Eur J Anaesthesiol. 2011;28:404–11. doi: 10.1097/EJA.0b013e328346d5a9. [DOI] [PubMed] [Google Scholar]
- 25.Zaman SM, Islam MM, Chowdhury KK, Rickta D, Ireen ST, Choudhury MR, et al. Haemodynamic and end tidal CO2 changes state after inflation and deflation of pneumatic tourniquet on extremities. Mymensingh Med J. 2010;19:524–8. [PubMed] [Google Scholar]
- 26.Feng L, Zhang XG, Yang QG, Wang G. Effects of tourniquet on cardiac function in total knee arthroplasty with trans-esophageal echocardiography. Zhonghua Yi Xue Za Zhi. 2013;93:3755–7. [PubMed] [Google Scholar]
- 27.Saied A, Ayatollahi Mousavi A, Arabnejad F, Ahmadzadeh Heshmati A. Tourniquet in surgery of the limbs: A review of history, types and complications. Iran Red Crescent Med J. 2015;17:e9588. doi: 10.5812/ircmj.9588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Allee J, Muzaffar AR, Tobias JD. Dexmedetomidine controls the hemodynamic manifestations of tourniquet pain. Am J Ther. 2011;18:e35–9. doi: 10.1097/MJT.0b013e3181c35088. [DOI] [PubMed] [Google Scholar]
- 29.Lee DH, Jee DL, Kim SY, Kim JM, Lee HM. Magnesium sulphate attenuates tourniquet-induced hypertension and spinal c-fos mRNA expression: A comparison with ketamine. J Int Med Res. 2006;34:573–84. doi: 10.1177/147323000603400602. [DOI] [PubMed] [Google Scholar]
- 30.Honarmand A, Safavi MR. Preoperative oral dextromethorphan vs. clonidine to prevent tourniquet-induced cardiovascular responses in orthopaedic patients under general anaesthesia. Eur J Anaesthesiol. 2007;24:511–5. doi: 10.1017/S0265021506002055. [DOI] [PubMed] [Google Scholar]
- 31.Jung JY, Han JH, Yi JW, Kang JM. Remifentanil prevents tourniquet-induced arterial pressure increase in elderly orthopedic patients under sevoflurane/N2O general anesthesia. Int J Med Sci. 2012;9:311–5. doi: 10.7150/ijms.4369. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Shinoda T, Murakami W, Takamichi Y, Iizuka H, Tanaka M, Kuwasako Y. Effect of remifentanil infusion rate on stress response in orthopedic surgery using a tourniquet application. BMC Anesthesiol. 2013;13:14. doi: 10.1186/1471-2253-13-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Panerai RB, Saeed NP, Robinson TG. Cerebrovascular effects of the thigh cuff maneuver. Am J Physiol Heart Circ Physiol. 2015;308:H688–96. doi: 10.1152/ajpheart.00887.2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Hinohara H, Kadoi Y, Ide M, Kuroda M, Saito S, Mizutani A. Differential effects of hyperventilation on cerebral blood flow velocity after tourniquet deflation during sevoflurane, isoflurane, or propofol anesthesia. J Anesth. 2010;24:587–93. doi: 10.1007/s00540-010-0965-7. [DOI] [PubMed] [Google Scholar]
- 35.Zaman SM, Islam MM, Chowdhury KK, Rickta D, Ireen ST, Choudhury MR, et al. Haemodynamic and end tidal CO2 changes state after inflation and deflation of pneumatic tourniquet on extremities. Mymensingh Med J. 2010;19:524–8. [PubMed] [Google Scholar]
- 36.Kageyama K, Nakajima Y, Shibasaki M, Hashimoto S, Mizobe T. Increased platelet, leukocyte, and endothelial cell activity are associated with increased coagulability in patients after total knee arthroplasty. J Thromb Haemost. 2007;5:738–45. doi: 10.1111/j.1538-7836.2007.02443.x. [DOI] [PubMed] [Google Scholar]
- 37.Reikerås O, Clementsen T. Time course of thrombosis and fibrinolysis in total knee arthroplasty with tourniquet application. Local versus systemic activations. J Thromb Thrombolysis. 2009;28:425–8. doi: 10.1007/s11239-008-0299-6. [DOI] [PubMed] [Google Scholar]
- 38.Watanabe H, Kikkawa I, Madoiwa S, Sekiya H, Hayasaka S, Sakata Y. Changes in blood coagulation-fibrinolysis markers by pneumatic tourniquet during total knee joint arthroplasty with venous thromboembolism. J Arthroplasty. 2014;29:569–73. doi: 10.1016/j.arth.2013.08.011. [DOI] [PubMed] [Google Scholar]
- 39.Zhang W, Li N, Chen S, Tan Y, Al-Aidaros M, Chen L. The effects of a tourniquet used in total knee arthroplasty: A meta-analysis. J Orthop Surg Res. 2014;9:13. doi: 10.1186/1749-799X-9-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Abbas K, Raza H, Umer M, Hafeez K. Effect of early release of tourniquet in total knee arthroplasty. J Coll Physicians Surg Pak. 2013;23:562–5. [PubMed] [Google Scholar]
- 41.Fisher B, Roberts CS. Tourniquet use and sickle cell hemoglobinopathy: How should we proceed? South Med J. 2010;103:1156–60. doi: 10.1097/SMJ.0b013e3181efaf3b. [DOI] [PubMed] [Google Scholar]
- 42.Chon JY, Lee JY. The effects of surgery type and duration of tourniquet inflation on body temperature. J Int Med Res. 2012;40:358–65. doi: 10.1177/147323001204000137. [DOI] [PubMed] [Google Scholar]
- 43.Kim YS, Jeon YS, Lee JA, Park WK, Koh HS, Joo JD, et al. Intra-operative warming with a forced-air warmer in preventing hypothermia after tourniquet deflation in elderly patients. J Int Med Res. 2009;37:1457–64. doi: 10.1177/147323000903700521. [DOI] [PubMed] [Google Scholar]
- 44.Crews JC, Cahall MA. An investigation of the neurophysiologic mechanisms of tourniquet-related pain: Changes in spontaneous activity and receptive field size in spinal dorsal horn neurons. Reg Anesth Pain Med. 1999;24:102–9. doi: 10.1016/s1098-7339(99)90069-x. [DOI] [PubMed] [Google Scholar]
- 45.MacIver MB, Tanelian DL. Activation of C fibers by metabolic perturbations associated with tourniquet ischemia. Anesthesiology. 1992;76:617–23. doi: 10.1097/00000542-199204000-00020. [DOI] [PubMed] [Google Scholar]
- 46.Chabel C, Russell LC, Lee R. Tourniquet-induced limb ischemia: A neurophysiologic animal model. Anesthesiology. 1990;72:1038–44. doi: 10.1097/00000542-199006000-00014. [DOI] [PubMed] [Google Scholar]
- 47.Park JW, Jung YH, Baek CW, Kang H, Cha SM. Effects of low dose ketamine on tourniquet-induced haemodynamic responses during general anaesthesia. J Int Med Res. 2007;35:600–8. doi: 10.1177/147323000703500504. [DOI] [PubMed] [Google Scholar]
- 48.Bratzler DW, Dellinger EP, Olsen KM, Perl TM, Auwaerter PG, Bolon MK, et al. Clinical practice guidelines for antimicrobial prophylaxis in surgery. Am J Health Syst Pharm. 2013;70:195–283. doi: 10.2146/ajhp120568. [DOI] [PubMed] [Google Scholar]
- 49.Denholm B. Administering prophylactic antibiotics during tourniquet-assisted procedures. AORN J. 2013;98:653–62. doi: 10.1016/j.aorn.2013.08.004. [DOI] [PubMed] [Google Scholar]
- 50.Tomita M, Motokawa S. Effects of air tourniquet on the antibiotics concentration, in bone marrow, injected just before the start of operation. Mod Rheumatol. 2007;17:409–12. doi: 10.1007/s10165-007-0609-4. [DOI] [PubMed] [Google Scholar]


