Abstract
There is a need for better understanding of various characteristics in hyperacusis in the general population. The objectives of the present study were to investigate individuals in the general population with hyperacusis regarding demographics, lifestyle, perceived general health and hearing ability, hyperacusis-specific characteristics and behavior, and comorbidity. Using data from a large-scale population-based questionnaire study, we investigated individuals with physician-diagnosed (n=66) and self-reported (n=313) hyperacusis in comparison to individuals without hyperacusis (n=2995). High age, female sex, and high education were associated with hyperacusis, and that trying to avoid sound sources, being able to affect the sound environment, and having sough medical attention were common reactions and behaviors. Posttraumatic stress disorder, chronic fatigue syndrome, generalized anxiety disorder, depression, exhaustion, fibromyalgia, irritable bowel syndrome, migraine, hearing impairment, tinnitus, and back/joint/muscle disorders were comorbid with hyperacusis. The results provide ground for future study of these characteristic features being risk factors for development of hyperacusis and/or consequences of hyperacusis.
Keywords: Functional somatic syndrome, hyperacusis, noise sensitivity, prevalence, psychiatric disorder, sound intolerance
INTRODUCTION
Hyperacusis is a condition in which exposure to everyday sounds is perceived as more annoying or disturbing than normal, resulting in symptoms such as headache, fatigue, and concentration difficulties. Reactions are characteristically triggered by sounds in general, even at low intensities,[1] rather than to specific sounds as in misophonia.[2] However, misophonia as well as fear of sounds (phonophobia[3,4]) can occasionally appear together with hyperacusis[1,5,6] although the illnesses are not mutually inclusive. There are few population studies of hyperacusis, but prevalence rates of 8.6 and 15.2% have been reported from a Swedish[7] and Polish[8] study, respectively. However, although considering oneself to be sensitive to everyday sounds was asked in the Swedish study, no such information was reported from the Polish study. Data from specific, nonstratified population samples show a similar prevalence; a Norwegian study[9] investigating noise sensitivity, traffic noise, and self-reported health reported a noise sensitivity prevalence of 11.5%, whereas a Swedish study[10] focusing on adolescents (13–19 years) found a prevalence of 17.1%. This discrepancy in prevalence between studies may be referred to differences in question formulation regarding hyperacusis, as well as some studies being based on specific populations.
Regarding demographic data, Andersson et al.[7] reported prevalence rates that imply that increased age is associated with hyperacusis. Hyperacusis has also been found to be more common among men (61%),[8] whereas documentation appears to be lacking regarding marital status and education as well as lifestyle factors (eg, smoking habits and physical exercise) and perceived general health. As would be expected, not only markedly low uncomfortable loudness level but also higher sound detection thresholds[11,12] have been shown in hyperacusis. Less is known about how common it is to experience reduced hearing in hyperacusis.
Individuals with hyperacusis often report difficulties in everyday activities and try to adapt to situations that may trigger symptoms, for example, by wearing earplugs or avoiding social situations.[4,12,13,14] To what extent individuals with hyperacusis in the general population cope with their condition by seeking medical attention lacks documentation to the best of our knowledge.
It is common among those suffering from hyperacusis to also have other conditions of poor health. Regarding psychiatric disorders, 56% of patients referred to an ear, nose, and throat clinic with hyperacusis as primary diagnoses were found to meet criteria for at least one psychiatric disorder. More specifically, 47% met criteria for anxiety disorder, 8% for major depression, and 3% for posttraumatic stress disorder (PTSD).[15]
Tinnitus is particularly common in hyperacusis. Prevalence rates for tinnitus have been reported to range between 9 and 86%, with the lower rate for the general population as opposed to clinical populations.[7,16,17,18] Other common comorbid illness in hyperacusis are Bell's pares,[19] facial paralysis,[20] and Williams syndrome.[21,22]
Hyperacusis has also shown comorbidity with other medically unexplained symptoms, including fibromyalgia,[23,24,25] chronic fatigue syndrome (CFS),[24,26] as well as other environmental intolerances such as multiple chemical sensitivity, nonspecific building-related symptoms, and symptoms attributed to electromagnetic fields.[27,28,29,30]
Different sources thus suggest that hyperacusis is an affliction associated with several additional concerns for health and well-being. In this study, we aimed to make an encompassing overview of the characteristics of hyperacusis in the general population. We investigated two case groups − individuals who reported a physician-diagnosed hyperacusis and a self-reported hyperacusis regarding (1) demographics, lifestyle, perceived general health and hearing ability in comparison to individuals without hyperacusis, (2) hyperacusis-specific characteristics and behavior, and (3) comorbidity, in comparison with a control group without hyperacusis. These questions were addressed by means of data from a large-scale population-based questionnaire study, the Västerbotten Environmental Health Study.
METHOD
Population and samples
The Västerbotten Environmental Health Study[30] is an ongoing research project that started in 2010. Its aim is to investigate factors relating to environmental health and environmental intolerances in Sweden, using a representative population sample. A random sample of 8520 individuals aged 18–79 years were drawn from the population of the Västerbotten county. Out of these, 40.0% (n=3406) agreed to participate. The sample was stratified for age and sex according to the following age strata: 18–29, 30–39, 40–49, 50–59, 60–69, and 70–79 years. The sample's age and sex distribution is given in Table 1.
Table 1.
Numbers of Respondents (and Percentage of Those Invited) Across Age and Sex Strata
| Age (years) | Women | Men |
|---|---|---|
| 18–29 | 307 (32.1) | 179 (17.3) |
| 30–39 | 266 (40.3) | 177 (24.7) |
| 40–49 | 288 (40.5) | 230 (31.0) |
| 50–59 | 367 (50.9) | 295 (39.5) |
| 60–69 | 405 (58.4) | 356 (50.7) |
| 70–79 | 265 (53.8) | 271 (63.9) |
| Total sample | 1898 (45.2) | 1508 (34.9) |
Among the 3406 respondents, 66 (1.9%) met the criterion for physician-diagnosed hyperacusis and 313 (9.2%) for self-reported hyperacusis. The group with physician-diagnosed hyperacusis responded affirmatively to the questions “Have you been diagnosed with sound intolerance by a physician?” and “Do you have a hard time tolerating everyday sounds that you believe most other people can tolerate?”, whereas the group with self-reported hyperacusis responded affirmatively only to the latter question. Thus, rather than being two distinct case groups, there is overlap between the two groups, and the physician-diagnosed group is likely to include more severe cases of hyperacusis. The physician-diagnosed group were found to have frequently more problems and for longer duration than the self-reported group; 48.5% reported daily, 34.8% reported once or a few times a week, and 15.2% reported once or a few times a month. Corresponding rates for the self-reported group were 34.2, 42.5, and 22%, respectively. The mean number of years experiencing hyperacusis was 13.54 (standard deviation, SD=8.52) for the physician-diagnosed group and 11.06 (SD=9.24) for the self-reported group.
Applying a cross-sectional design, the two case groups were compared with a reference group (n=2995), who reported having neither a physician-diagnosed nor self-reported sound intolerance.
Questionnaires
The 11-item Noise Sensitivity Scale (NSS)[31] was used that is a short-form version of the original 21-item NSS.[32] The NSS-11 quantifies degree of affective reactions to and behavioral disruptions by environmental sounds.[33] Cronbach's α for the present sample (n=3406) was 0.77. Mean (SD) score was 40.2 (6.89) in the group with physician-diagnosed hyperacusis, 36.9 (7.42) in the group with self-reported hyperacusis, and 26.1 (7.31) in the referent group. On the basis of normative data for the NSS-11,[33] the severity of hyperacusis corresponds, on average, to the 94.9th percentile of the general population in the group with physician-diagnosed hyperacusis, the 88.8th percentile in the group with self-reported hyperacusis, and the 44.5th percentile in the reference group.
The participants responded to questions about demographics, lifestyle, perceived general health and hearing ability (first research question), hyperacusis-specific characteristics and behavior (second question), and comorbidity (third question). The demographic and lifestyle questions related to age, sex, marital status/cohabitant, and present smoking. The questions regarding hyperacusis-related characteristics and behavior are given in Figure 1. The illnesses were back/joint muscle disorder, PTSD, generalized anxiety syndrome (GAD), tinnitus, hearing impairment, CFS, migraine, attention-deficit/hyperactivity disorder (ADHD), fibromyalgia, irritable bowel syndrome (IBS), panic disorder, depression, and exhaustion syndrome.
Figure 1.
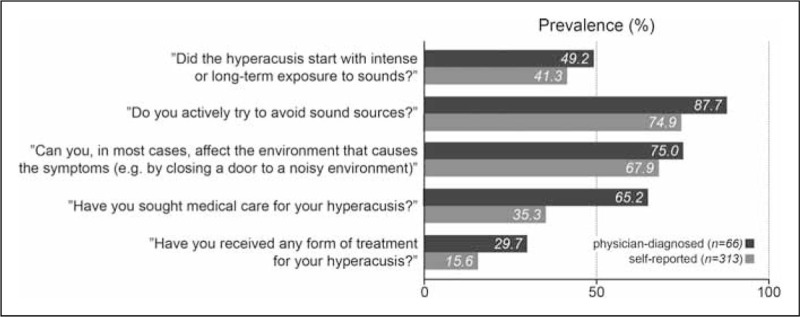
Hyperacusis-specific characteristics and behaviors among participants with physician-diagnosed hyperacusis and self-reported hyperacusis
Procedure
The questionnaire was sent to the participants with the instruction to return it via mail with prepaid postage. Those who did not respond to the first invitation received up to two reminders. All participants responded to the questionnaire during the period March to April 2010. The study was conducted in accordance with the Helsinki Declaration and approved by the Umeå Regional Ethics Board (Dnr 09-171M). All participants gave their informed consent to participate.
Statistical analysis
All analyses were performed using the Statistical Package for the Social Sciences (IBM SPSS Statistics for Windows, Version 21.0; Armonk, NY). The two case groups were compared with the referents on demographics, lifestyle, and perceived general health and hearing ability with independent t test and χ2 analysis. Logistic regression analyses were conducted to obtain crude and adjusted (for age, sex, and education that differed between the case groups and referents) odds ratios (ORs) for studying comorbidity in hyperacusis with the various diagnoses. The α level was set at 0.05.
RESULTS
Results for demographics, lifestyle, and perceived general health and hearing ability for both the case groups and referents are given in Table 2. Compared with the referents, the physician-diagnosed group was significantly older in age. The self-reported group was younger and had higher education. Both the case groups consisted of a larger proportion of women, reported poorer health, and more commonly perceived their hearing ability to be below normal.
Table 2.
Description of Case Groups and Referent Group with Respect to Demographics, Lifestyle, and Perceived General Health and Hearing Ability, and Comparisons Between Case Groups and Referents with t Test (Age) and χ2 Analysis
| Physician diagnosed (n=66) | Self reported (n=313) | Referents (n=2995) | |
|---|---|---|---|
| Age (years), mean (SD) | 57.8 (11.44)*** | 48.9 (15.45)* | 51.1 (16.94) |
| Women, n (%) | 44 (66.7)* | 220 (70.3)*** | 1619 (54.1) |
| Married/cohabitant, n (%) | 56 (84.8)ns | 222 (70.9)ns | 2213 (74.4) |
| No response | 0 | 3 (0.9) | 25 (0.8) |
| Education (highest level), n (%) | ns | ** | |
| Compulsory school | 19 (28.8) | 54 (17.4) | 711 (24) |
| Senior high school | 19 (28.8) | 98 (31.5) | 1016 (34.4) |
| College/University | 28 (42.4) | 159 (51.1) | 1230 (41.6) |
| No response | 2 (0.6) | 38 (1.3) | |
| Smoking, n (%) | 10 (15.2)ns | 27 (8.7)ns | 262 (8.8) |
| No response | 0 | 3 (0.9) | 21 (0.7) |
| Physical exercise, n (%) | ns | ns | |
| Once a month or less | 4 (6.1) | 31 (10) | 382 (12.9) |
| 2–4 times/month | 11 (16.7) | 71 (23) | 581 (19.6) |
| 2–3 times/week | 24 (36.4) | 114 (36.9) | 1132 (37.3) |
| More than 3 times/week | 27 (40.9) | 93 (30.1) | 862 (29.2) |
| No response | 4 (1.3) | 38 (1.3) | |
| Perceived general health, n (%) | *** | *** | |
| Excellent/Very good | 11 (16.7) | 89 (28.4) | 1245 (41.6) |
| Good | 22 (33.3) | 95 (30.4) | 1026 (34.3) |
| Somewhat good/Poor | 32 (48.5) | 127 (40.6) | 691 (23.1) |
| No response | 1 (1.5) | 2 (0.6) | 33 (1.1) |
| Perceived hearing ability, n (%) | *** | *** | |
| Normal | 19 (28.8) | 117 (37.5) | 1888 (63.6) |
| Above normal | 10 (15.2) | 52 (16.7) | 358 (12.1) |
| Below normal | 37 (56.1) | 143 (45.8) | 722 (24.3) |
| No response | 1 (0.3) | 27 (0.9) |
*P<0.05; **P<0.01; ***P<0.001; nsnonsignificant; SD: standard deviation.
Frequencies of hyperacusis-specific characteristics and behavior are shown in Figure 1. In both the case groups, a majority reported actively trying to avoid sound sources, and mostly being able to affect the sound environment, whereas a majority in the physician-diagnosed group, but not the self-reported group, also reported having sough medical attention. Around half of the people in the case groups reported that the hyperacusis started after high-dose or long-term sound exposure, and less than a third reported that they had received treatment. For all five aspects, the proportions were larger in the physician-diagnosed group than in the self-reported group.
Percentage of the participants in each case group, who also had a certain diagnosis, is depicted in Figures 2 and 3. The figures also give ORs for comorbidity in hyperacusis with the diagnoses when unadjusted (crude) and adjusted for age, sex, and education. ADHD and panic disorder were excluded from the analyses for the physician-diagnosed group because of less than five of the cases reporting the two diagnoses. With the exception of migraine being adjusted in the physician-diagnosed group, the OR for all diagnoses, when both unadjusted and adjusted, were significantly higher than unity. In both the case groups, the ORs were particularly high for PTSD, CFS, and GAD, and the ORs were generally higher in the physician-diagnosed group than in the self-reported group.
Figure 2.
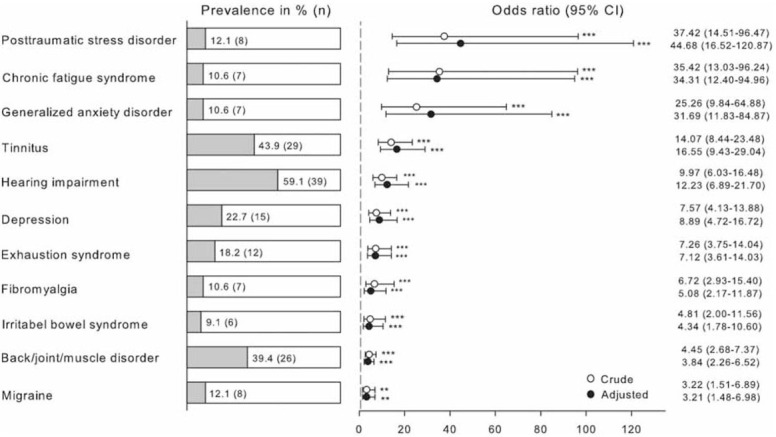
Percentage of participants with physician-diagnosed hyperacusis who reported a certain diagnosis as well as odds ratios (ORs), confidence intervals (CIs), and P values for comorbidity with a certain diagnosis when unadjusted (crude) and adjusted for age, sex, and education
Figure 3.
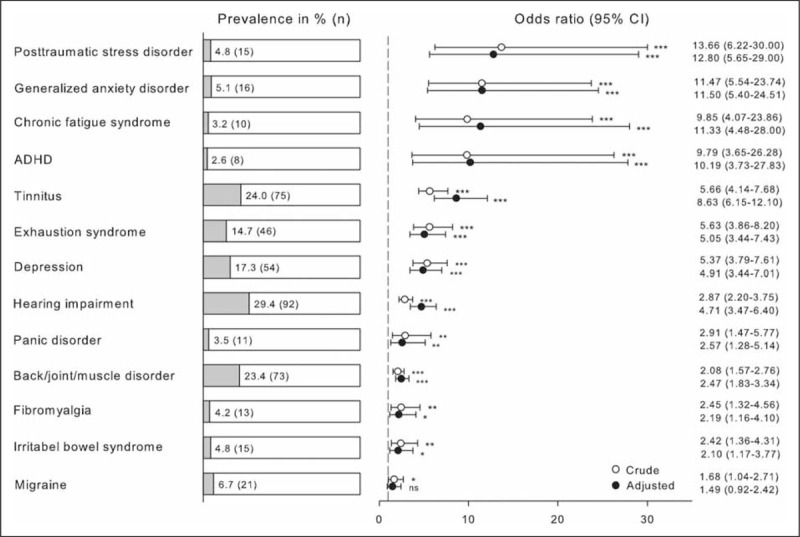
Percentage of participants with self-reported hyperacusis who reported a certain diagnosis as well as odds ratios (ORs), confidence intervals (CIs), and P values for comorbidity with a certain diagnosis when unadjusted (crude) and adjusted for age, sex, and education
DISCUSSION
Till date, only two population-based studies have been published.[7,8] In this study, we investigated hyperacusis with respect to demographics, lifestyle factors, perceived general health and hearing ability, as well as hyperacusis-specific characteristics and behavior and comorbidity. The results showed that the groups with hyperacusis (physician-diagnosed and self-reported), compared with the referents, were older and predominantly women, had higher education (self-reported group only), and had poorer perceived general health and hearing ability, but did not differ regarding being married/cohabitant, smoking habits, and physical exercise. Regarding hyperacusis-specific characteristics, a large majority of the case groups reported trying to avoid sound sources, and mostly being able to affect the sound environment, and a majority in the physician-diagnosed group, but not the self-reported group, also reported having sough medical attention. Close to half of the case groups reported that the hyperacusis started after high-dose or long-term sound exposure, and about a quarter that they had received treatment. Furthermore, all five aspects were somewhat more common in the physician-diagnosed group than in the self-reported group.
Concerning comorbidity, both the case groups showed higher risk than the referents of comorbidity with psychiatric diagnoses (PTSD, GAD, depression, and exhaustion syndrome), functional somatic syndromes (CFS, fibromyalgia, IBS, and migraine), and the conditions of tinnitus, hearing impairment, and back/joint/muscle disorder when both unadjusted and adjusted for age, sex, and education. ADHD and panic disorder were studied only in the self-reported group having higher than normal risk. However, caution should be taken regarding the exact size of the OR for PTSD, GAD, CFS, and ADHD because of large confidence intervals. It should also be noted that migraine did not reach statistical significance in the self-reported group when adjusted for age, sex, and education. Although the ORs were high for many of the diagnoses, in particular for PTSD, CFS and GAD, the prevalence rates in the hyperacusis groups were, in general, low, with the exceptions of tinnitus, hearing impairment, back/joint/muscle disorder, and depression.
Out of our total sample, 9.2% had self-reported hyperacusis and 1.9% reported having received a diagnosis from a physician. Using a similar criterion for self-reported hyperacusis, the present prevalence rate is similar to that of 8.6% reported by Andersson et al.[7] Similar to the study by Andersson et al.,[7] the results from the present study imply middle aged and elderly being a risk group for hyperacusis. In accordance with the past findings of higher sound detection thresholds in hyperacusis,[11,12] our results suggest that it is also common to experience reduced hearing. Although hyperacusis was found to be more common in men than in women in a Polish sample,[8] the opposite result was obtained from our Swedish sample. However, although not studying a population-based sample, Ellermeier et al.[34] reported a sound intolerant group being dominated by women. Further studies are needed to better understand the role of sex and gender in hyperacusis. This may also apply to the role of education as hyperacusis was found to be associated with high education in the self-reported but not in the physician-diagnosed group.
Similar to the previous studies,[7,12] our participants with hyperacusis tried to avoid sound, and also commonly reporting that they could affect the sound environment. Less than half of the respondents attributed their onset of hyperacusis to high or long-term sound exposure, something that is often cited as a cause for tinnitus[35,36] and may explain the comorbidity of the two conditions. It may seem counterintuitive that only two out of the three with physician-diagnosed hyperacusis had sought medical attention for this condition. However, it is possible, given the high risk of comorbidity with hearing impairment and tinnitus, that the patients have sought medical attention for other illnesses and were then diagnosed with hyperacusis. It is also worth noting that only one third had received treatment for their condition, motivating future research on why this proportion is low and on types of treatment being received.
Regarding comorbidity, we found that hyperacusis co-occurred with several diagnoses, similar to other studies including psychiatric diagnoses,[15,37,38,39] functional somatic syndromes,[14,23,24,25,26] hearing impairment,[40] and tinnitus.[7,16,17,18]
With a 9.2% prevalence of self-reported hyperacusis found in our sample, it can be estimated that about 700,000 of the adult Swedish population might suffer from hyperacusis, warranting additional research and healthcare resources. Our study was conducted on a statically representative sample of the general population, but it bears to have in mind that the reply rate was only 40%, with the largest nonreply among young ages. As the purpose of the study was to investigate environmental health issues, those with these issues might have been more motivated to reply. Being a questionnaire-based survey, we did not have data on hearing threshold or loudness discomfort levels, but future studies may investigate the relation between such measures and experience of hearing.
Despite limitations of the study, the results suggest that high age, female sex, and possibly high education are associated with hyperacusis. Trying to avoid sound sources, and being able to affect the sound environment, and to some extent also having sough medical attention are common reactions and behaviors. Finally, various psychiatric conditions and functional somatic syndromes as well as hearing impairment, tinnitus, and back/joint/muscle disorders show comorbidity with hyperacusis, and more so when diagnosed for hyperacusis than when only reporting more sound intolerance than normal. The academic field of hyperacusis has rapidly expanded in the past 2 decades,[41] and given that about one in 10 individuals in our study experience problems with everyday sounds, more research is warranted to further increase our understanding of hyperacusis in the general public. Caution should be taken because of the cross-sectional nature of the data, but, nevertheless, the presented results provide ground for future study of these characteristic features being risk factors for development of hyperacusis and/or consequences of hyperacusis.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgements
The authors are thankful to Eva Palmquist for valuable help with the database.
REFERENCES
- 1.Baguley DM. Hyperacusis. J R Soc Med. 2003;96:582–5. doi: 10.1258/jrsm.96.12.582. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Schwartz P, Leyendecker J, Conlon M. Hyperacusis and misophonia: The lesser-known siblings of tinnitus. Minn Med. 2011;94:42–3. [PubMed] [Google Scholar]
- 3.Phillips DP, Carr MM. Disturbances of loudness perception. J Am Acad Audiol. 1998;9:371–9. [PubMed] [Google Scholar]
- 4.Tyler RS, Pienkowski M, Roncancio ER, Jun HJ, Brozoski T, Dauman N, et al. A review of hyperacusis and future directions: part I. Definitions and manifestations. Am J Audiol. 2014;23:402–19. doi: 10.1044/2014_AJA-14-0010. [DOI] [PubMed] [Google Scholar]
- 5.Jastreboff P, Jastreboff M. Aminoff MJ, Boller F, Swaab DF, editors. Decreased sound tolerance: hyperacusis, misophonia, diplacousis, and polyacousis. [Internet] Handbook of clinical neurology – The Human Auditory System Fundamental Organization and Clinical Disorders. 2015:357–87. doi: 10.1016/B978-0-444-62630-1.00021-4. [DOI] [PubMed] [Google Scholar]
- 6.Schröder A, Vulink N, Denys D. Misophonia: Diagnostic criteria for a new psychiatric disorder. PLoS One. 2013;8:e54706. doi: 10.1371/journal.pone.0054706. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Andersson G, Lindvall N, Hursti T, Carlbring P. Hypersensitivity to sound (hyperacusis): A prevalence study conducted via the Internet and post. Int J Audiol. 2002;41:545–54. doi: 10.3109/14992020209056075. [DOI] [PubMed] [Google Scholar]
- 8.Fabijanska A, Rogowski M, Bartnik G, Skarzyński H. Epidemiology of tinnitus and hyperacusis in Poland. Proc 6th Int Tinnitus Semin. 1999:569–72. [Google Scholar]
- 9.Fyhri A, Klaeboe R. Road traffic noise, sensitivity, annoyance and self-reported health: A structural equation model exercise. Environ Int. 2009;35:91–7. doi: 10.1016/j.envint.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 10.Olsen Widén SE, Erlandsson SI. The influence of socio-economic status on adolescent attitude to social noise and hearing protection. Noise Health. 2004;7:59–70. [PubMed] [Google Scholar]
- 11.Anari M, Axelsson A, Eliasson A. Hypersensitivity to sound. Scand J Audiol. 1999;28:219–30. doi: 10.1080/010503999424653. [DOI] [PubMed] [Google Scholar]
- 12.Blaesing L, Kroener-Herwig B. Self-reported and behavioral sound avoidance in tinnitus and hyperacusis subjects, and association with anxiety ratings. Int J Audiol. 2012;51:611–7. doi: 10.3109/14992027.2012.664290. [DOI] [PubMed] [Google Scholar]
- 13.Jüris L, Andersson G, Larsen HC, Ekselius L. Cognitive behaviour therapy for hyperacusis: A randomized controlled trial. Behav Res Ther. 2014;54:30–7. doi: 10.1016/j.brat.2014.01.001. [DOI] [PubMed] [Google Scholar]
- 14.Pienkowski M, Tyler RS, Roncancio R, Jun HJ, Brozoski T, Dauman N, et al. A review of hyperacusis and future directions: part II. Measurement, mechanisms, and treatment. Am J Audiol. 2015;23:420–36. doi: 10.1044/2014_AJA-13-0037. [DOI] [PubMed] [Google Scholar]
- 15.Jüris L, Andersson G, Larsen HC, Ekselius L. Psychiatric comorbidity and personality traits in patients with hyperacusis. Int J Audiol. 2013;52:230–5. doi: 10.3109/14992027.2012.743043. [DOI] [PubMed] [Google Scholar]
- 16.Anari M, Axelsson A, Eliasson A, Magnusson L. Hypersensitivity to sound: Questionnaire data, audiometry and classification. Scand Audiol. 2009;28:219–30. doi: 10.1080/010503999424653. [DOI] [PubMed] [Google Scholar]
- 17.Andersson G, Vretblad P, Larsen HC, Lyttkens L. Longitudinal follow-up of tinnitus complaints. Arch Otorhinolaryngol Head Neck Surg. 2001;127:175–9. doi: 10.1001/archotol.127.2.175. [DOI] [PubMed] [Google Scholar]
- 18.Jastreboff PJ, Jastreboff MM. Tinnitus retraining therapy (TRT) as a method for treatment of tinnitus and hyperacusis patients. J Am Acad Audiol. 2000;11:162–77. [PubMed] [Google Scholar]
- 19.Adour KK, Wingerd J. Idiopathic facial paralysis (Bell's palsy): Factors affecting severity and outcome in 446 patients. Neurology. 1974;24:1112–6. doi: 10.1212/wnl.24.12.1112. [DOI] [PubMed] [Google Scholar]
- 20.Majid A, Noor R, Bashir M. Incidence of hyperacusis in pediatrics facial paralysis. J Riphah Coll Rehabil Sci. 2013;1:36–9. [Google Scholar]
- 21.Nigam A, Samuel PR. Hyperacusis and Williams syndrome. J Laryngol Otol. 1994;108:494–6. doi: 10.1017/s0022215100127203. [DOI] [PubMed] [Google Scholar]
- 22.Gothelf D, Farber N, Raveh E, Apter A, Attias J. Hyperacusis in Williams syndrome: Characteristics and associated neuroaudiologic abnormalities. Neurology. 2006;66:390–5. doi: 10.1212/01.wnl.0000196643.35395.5f. [DOI] [PubMed] [Google Scholar]
- 23.McDermid AJ, Rollman GB, McCain GA. Generalized hypervigilance in fibromyalgia: Evidence of perceptual amplification. Pain. 1996;66:133–44. doi: 10.1016/0304-3959(96)03059-x. [DOI] [PubMed] [Google Scholar]
- 24.Jason LA, Taylor RR, Kennedy CL. Chronic fatigue syndrome, fibromyalgia, and multiple chemical sensitivities in a community-based sample of persons with chronic fatigue syndrome-like symptoms. Psychosom Med. 2000;62:655–63. doi: 10.1097/00006842-200009000-00009. [DOI] [PubMed] [Google Scholar]
- 25.Geisser ME, Glass JM, Rajcevska LD, Clauw DJ, Williams DA, Kileny PR, et al. A psychophysical study of auditory and pressure sensitivity in patients with fibromyalgia and healthy controls. J Pain. 2008;9:417–22. doi: 10.1016/j.jpain.2007.12.006. [DOI] [PubMed] [Google Scholar]
- 26.Wessely S, Nimnuan C, Sharpe M. Functional somatic syndromes: One or many? Lancet (London, England) 1999;354:936–9. doi: 10.1016/S0140-6736(98)08320-2. [DOI] [PubMed] [Google Scholar]
- 27.Bell IR, Hardin EE, Baldwin CM, Schwartz GE. Increased limbic system symptomatology and sensitizability of young adults with chemical and noise sensitivities. Environ Res. 1995;70:84–97. doi: 10.1006/enrs.1995.1052. [DOI] [PubMed] [Google Scholar]
- 28.Bell IR, Schwartz GE, Baldwin CM, Hardin EE. Neural sensitization and physiological markers in multiple chemical sensitivity. Regul Toxicol Pharmacol. 1996;24:S39–47. doi: 10.1006/rtph.1996.0075. [DOI] [PubMed] [Google Scholar]
- 29.Nordin S, Ljungberg JK, Claeson A, Neely G. Stress and odor sensitivity in persons with noise sensitivity. Noise Health. 2013;15:173–7. doi: 10.4103/1463-1741.112366. [DOI] [PubMed] [Google Scholar]
- 30.Palmquist E, Claeson A-S, Neely G, Stenberg B, Nordin S. Overlap in prevalence between various types of environmental intolerance. Int J Hyg Environ Health. 2014;217:427–34. doi: 10.1016/j.ijheh.2013.08.005. [DOI] [PubMed] [Google Scholar]
- 31.Nordin S, Palmquist E, Claeson A-S. Metric properties and normative data for brief noise and electromagnetic field sensitivity scales. Scand J Public Health. 2013;41:293–301. doi: 10.1177/1403494813475532. [DOI] [PubMed] [Google Scholar]
- 32.Weinstein ND. Individual differences in reactions to noise: A longitudinal study in a college dormitory. J Appl Psychol. 1978;63:458–66. [PubMed] [Google Scholar]
- 33.Nordin S, Palmquist E, Claeson AS. The environmental symptom-attribution scale: Metric properties andnormative data. J Environ Psychol. 2013;36:9–17. [Google Scholar]
- 34.Ellermeier W, Eigenstetter M, Zimmer K. Psychoacoustic correlates of individual noise sensitivity. J Acoust Soc Am. 2001;109:1464–73. doi: 10.1121/1.1350402. [DOI] [PubMed] [Google Scholar]
- 35.Axelsson A, Prasher D. Tinnitus induced by occupational and leisure noise. Noise Health. 2000;2:47–54. [PubMed] [Google Scholar]
- 36.Axelsson A, Sandh A. Tinnitus in noise-induced hearing loss. Br J Audiol. 1985;19:271–6. doi: 10.3109/03005368509078983. [DOI] [PubMed] [Google Scholar]
- 37.Fagelson M. Military trauma and its influence on loudness perception. ENT Audiol News. 2013;21:80–1. [Google Scholar]
- 38.Wallén MB, Hasson D, Theorell T, Canlon B. The correlation between the hyperacusis questionnaire and uncomfortable loudness levels is dependent on emotional exhaustion. Int J Audiol. 2012;51:722–9. doi: 10.3109/14992027.2012.695874. [DOI] [PubMed] [Google Scholar]
- 39.Westcott M. Case study: Management of hyperacusis associated with post-traumatic stress disorder. In: Patuzzi R, editor. Proceedings of the Seventh International Tinnitus Seminar 2002. Perth, Australia: University of Western Australia; 2002. pp. 280–5. [Google Scholar]
- 40.Martines F, Bentivegna D, Martines E, Sciacca V, Martinciglio G. Assessing audiological, pathophysiological and psychological variables in tinnitus patients with or without hearing loss. Eur Arch Oto-Rhino-Laryngology. 2010;267:1685–93. doi: 10.1007/s00405-010-1302-3. [DOI] [PubMed] [Google Scholar]
- 41.Moller AR, Salvi R, De Ridder D, Kleinjung T, Vanneste S. Pathology of tinnitus and hyperacusis: Clinical implications. Biomed Res Int 2015. 2015:1–2. doi: 10.1155/2015/608437. [DOI] [PMC free article] [PubMed] [Google Scholar]


