Abstract
Osteoporosis and osteoporotic fractures are strongly associated with mortality and morbidity, both in developing and developed countries. Menopause accelerates bone loss due to estrogen deficiency and age-related linear bone loss. We investigated plasminogen activator inhibitor-1 (PAI-1) gene polymorphisms in postmenopausal women with osteoporotic vertebral compression fractures (OVCFs). In this case-control study, 355 postmenopausal women were genotyped for the presence of PAI-1 gene polymorphisms −844A > G, −675 4G > 5G, 43G > A, 9785A > G, and 11053T > G. Genetic polymorphisms of PAI-1 were analyzed by the polymerization chain reaction restriction fragment length polymorphism assay, and their association with disease status and folate and homocysteine levels was determined in 158 OVCF patients and 197 control subjects. The PAI-1 −675 5G5G (adjusted odds ratio (AOR), 3.302; p = 0.017) and 43GA + AA (AOR, 2.087; p = 0.042) genotype frequencies showed significant association with the increased prevalence of OVCFs in postmenopausal women. In addition, we performed gene–environment interaction studies and demonstrated an association between PAI-1 gene polymorphisms and OVCF prevalence. Our novel finding is the identification of several PAI-1 genetic variants that increase susceptibility to OVCF. Our findings suggest that polymorphisms in PAI-1 may contribute to OVCF, and that they can be developed as biomarkers for evaluating OVCF risk.
Keywords: polymorphism, osteoporotic vertebral compression fractures, PAI-1, plasminogen activator inhibitor-1, osteoporosis
1. Introduction
Osteoporosis is a common metabolic bone disorder characterized by reduced bone mass, increased skeletal fragility, microarchitectural deterioration, and an increase in bone fractures [1]. Osteoporosis leads to decreased skeletal strength and increased fracture susceptibility. Osteoporotic fractures are a leading cause of disability and, subsequently, death in postmenopausal women [1,2]. The occurrence of osteoporotic fractures is closely associated with mortality worldwide [3,4]. Approximately 30% of women and 12% of men will be affected by osteoporosis in their lifetime; therefore, osteoporosis imposes a major economic burden on society. In particular, osteoporosis and osteoporotic fractures occur frequently in postmenopausal women due to decreased estrogen levels [5,6]. Estrogen deficiency associated with menopause, combined with age-related linear bone loss, leads to accelerated bone loss [7]. Bone mineral density (BMD) is a quantitative trait (g/cm2), with a normal distribution based on age and sex [8], and is thought to be controlled genetically in 50%–90% of cases [9,10,11,12]. A previous study has shown that several gene polymorphisms can affect BMD levels [6,12,13,14,15,16].
The plasminogen activator inhibitor-1 (PAI-1) gene has several alternative names; the Human Gene Nomenclature Committee (HGNC) provides SERPINE1 as the name that is used officially. The PAI-1 gene encodes a member of the serine protease inhibitor superfamily (located on chr.7q21.3). The PAI-1 protein inhibits plasminogen activators , including tissue plasminogen activator (tPA) and urokinase-type plasminogen activator (uPA), that touch off a fibrinolysis pathway by conversion from plasminogen to plasmin [17]. Following the formation of a fibrin clot, the fibrinolytic system is activated through regulation by PAI-1. The fibrinolytic system provides vessel elasticity by eliminating thrombosis, dismantling the extracellular matrix, and causing tissue remodeling, cell adhesion, and cell migration [18,19]. Daci et al. [20] previously reported that PAI-1 deficiency partially protects against bone loss in estrogen-deficient mice. Another study reported prevention of bone loss in diabetes in PAI-1-deficient mice [21,22]. A recent study has shown that plasminogen is involved in bone recovery in mice [22], suggesting that fibrinolysis in tissue might be a crucial factor in bone fracture recovery [23].
Many previous studies have investigated functional PAI-1 in osteoporosis patients [20,21,23]. However, none have reported on the association between PAI-1 polymorphisms and osteoporotic vertebral compression fractures (OVCFs) in postmenopausal women. Therefore, the purpose of this study was to investigate whether these polymorphisms of PAI-1 (−844A > G, −675 4G > 5G, 43G > A, 9785A > G, and 11053T > G) correlate with OVCF susceptibility in postmenopausal women.
2. Results
Demographic characteristics and clinical profiles of osteoporosis patients (with/without osteoporotic vertebral compression fracture, OVCF) and controls are summarized in Table 1 and Table S1.
Table 1.
Baseline characteristics between controls and osteoporosis patients.
| Characteristic | Controls (n = 197) | Osteoporosis (n = 158) | p | OVCF (n = 87) | p | Non-OVCF (n = 71) | p |
|---|---|---|---|---|---|---|---|
| Age (years, mean ± SD) | 66.11 ± 8.93 | 70.50 ± 8.24 | <0.0001 | 70.23 ± 9.44 | 0.001 | 70.83 ± 6.53 | <0.0001 |
| Hypertension (%) | 92 (46.7) | 57 (36.1) | 0.196 | 37 (42.5) | 0.760 | 20 (28.2) | 0.087 |
| SBP (mmHg, mean ± SD) | 134.98 ± 18.13 | 128.42 ± 15.27 | 0.0005 | 129.99 ± 16.51 | 0.041 | 126.66 ± 13.65 | 0.001 |
| DBP (mmHg, mean ± SD) | 80.69 ± 12.22 | 76.13 ± 10.44 | 0.0003 | 77.63 ± 10.57 | 0.049 | 74.45 ± 10.10 | 0.0001 |
| Diabetes mellitus (%) | 25 (12.7) | 28 (17.7) | 0.324 | 11 (12.6) | 0.992 | 17 (23.9) | 0.062 |
| FBS (mg/dL, mean ± SD) | 110.46 ± 33.98 | 125.80 ± 44.48 | <0.0001 | 135.89 ± 53.96 | <0.0001 | 114.30 ± 26.15 | 0.025 |
| Hcy (μmol/L, mean ± SD) | 9.38 ± 2.89 | 9.81 ± 4.06 | 0.056 | 10.01 ± 3.85 | 0.022 | 9.57 ± 4.31 | 0.316 |
| Folate (ng/mL, mean ± SD) | 9.67 ± 9.25 | 8.12 ± 4.78 | 0.054 | 6.54 ± 4.03 | 0.003 | 10.19 ± 4.91 | 0.027 |
| BMI (kg/m2, mean ± SD) | 24.51 ± 3.30 | 23.88 ± 4.04 | 0.169 | 23.87 ± 5.02 | 0.286 | 23.89 ± 2.75 | 0.180 |
| HDL-cholesterol (mg/dL, mean ± SD) | 47.83 ± 12.05 | 44.60 ± 14.24 | 0.201 | 44.39 ± 15.95 | 0.249 | 44.83 ± 12.24 | 0.250 |
| LDL-cholesterol (mg/dL, mean ± SD) | 131.09 ± 44.47 | 106.74 ± 39.49 | 0.001 | 117.87 ± 42.82 | 0.161 | 95.02 ± 32.02 | <0.0001 |
| TG (mg/dL, mean ± SD) | 150.29 ± 88.98 | 140.66 ± 80.11 | 0.324 | 147.62 ± 74.17 | 0.824 | 132.23 ± 86.68 | 0.176 |
| Vitamin B12 (pg/mL, mean ± SD) | 788.25 ± 821.74 | 710.69 ± 591.37 | 0.015 | 973.11 ± 1024.37 | 0.361 | 639.46 ± 384.93 | 0.006 |
| 25-(OH) Vitamin D (ng/mL, mean ± SD) | - | 24.02 ± 21.50 | - | 41.97 ± 34.20 | - | 18.57 ± 11.62 | - |
| Osteocalcin (ng/mL, mean ± SD) | - | 7.83 ± 6.39 | - | 7.83 ± 6.39 | - | - | - |
| DPD (nMDP/mMcre, mean ± SD) | - | 8.41 ± 5.55 | - | 8.41 ± 5.55 | - | - | - |
| BMD (g/cm2, mean ± SD) | - | −3.06 ± 0.97 | - | −2.98 ± 1.26 | - | −3.06 ± 0.97 | - |
Abbreviations: OVCF, osteoporotic vertebral compression fracture; SBP, systolic blood pressure; DBP, diastolic blood pressure; FBS, fasting blood sugar; Hcy, homocysteine; BMI, body mass index; HDL, high density lipoprotein; LDL, low density lipoprotein; TG, triglyceride; DPD, deoxypyridinoline; BMD, bone mineral density.
2.1. Genotype Frequencies of the PAI-1 Polymorphisms
Genotype and allele frequencies of the PAI-1 polymorphisms −844A > G, −675 4G > 5G, 43G > A, 9785A > G, and 11053T > G are listed for osteoporosis patients (with/without OVCF) and control in Table 2. Table 2 shows association between osteoporosis and PAI-1 polymorphisms including −675 4G > 5G (4G4G vs. 5G5G: adjusted odds ratio (AOR) 3.302, 95% confidence interval (CI) 1.224–7.512, p = 0.017; 4G4G vs. 4G5G + 5G5G: AOR 1.727, 95% CI 1.102–2.706, p = 0.017; and 4G4G + 4G5G vs. 5G5G: AOR 2.510, 95% CI 1.056–5.968, p = 0.037), and +43G > A (GG vs. GA + AA: AOR 2.087, 95% CI 1.027–4.241, p = 0.042). In addition, it shows a significant correlation between OVCF risk and PAI-1 polymorphisms, −844G > A (GG vs. GA: AOR 2.244, 95% CI 1.164–4.326, p = 0.015; GG vs. GA + AA: AOR 1.918, 95% CI 1.016–3.621, p = 0.044), −675 4G > 5G (4G4G vs. 5G5G: AOR 4.646, 95% CI 1.625–13.286, p = 0.004; 4G4G vs. 4G5G + 5G5G: AOR 1.969, 95% CI 1.130–3.430, p = 0.017; 4G4G + 4G5G vs. 5G5G: AOR 3.378, 95% CI 1.301–8.769, p = 0.012), and +43 G > A (GG vs. GA: AOR 2.421, 95% CI 1.057–5.546, p = 0.017; GG vs. GA + AA: AOR 2.292, 95% CI 1.009–5.206, p = 0.048). Furthermore, we analyzed the association between OVCF patients and non-OVCF patients (Table S2).
Table 2.
Comparison of genotype frequencies and adjusted odds ratio (AOR) values of plasminogen activator inhibitor-1 (PAI-1) gene polymorphisms between the osteoporosis and control subjects.
| Genotypes | Controls (n = 197) | Osteoporosis (n = 158) | AOR (95% CI) * | p | Non-OVCF (n = 71) | AOR (95% CI) * | p | OVCF (n = 87) | AOR (95% CI) * | p |
|---|---|---|---|---|---|---|---|---|---|---|
| PAI-1 −844 | - | - | - | - | - | - | - | - | - | - |
| GG | 70 (35.5) | 40 (25.3) | 1.000 (reference) | - | 22 (31.0) | 1.000 (reference) | - | 18 (20.7) | 1.000 (reference) | - |
| GA | 91 (46.2) | 89 (56.3) | 1.584 (0.951–2.640) | 0.077 | 33 (46.5) | 1.168 (0.604–2.256) | 0.645 | 56 (64.4) | 2.244 (1.164–4.326) | 0.016 |
| AA | 36 (18.3) | 29 (18.4) | 1.263 (0.647–2.467) | 0.494 | 16 (22.5) | 1.460 (0.641–3.327) | 0.368 | 13 (14.9) | 1.052 (0.415–2.664) | 0.915 |
| Dominant (GG vs. GA + AA) | - | - | 1.496 (0.919–2.435) | 0.105 | - | 1.252 (0.677–2.318) | 0.474 | - | 1.918 (1.016–3.621) | 0.044 |
| Recessive (GG + GA vs. AA) | - | - | 0.949 (0.528–1.705) | 0.860 | - | 1.342 (0.657–2.740) | 0.420 | - | 0.620 (0.278–1.385) | 0.244 |
| HWE-P | 0.502 | 0.097 | - | - | - | - | - | - | - | - |
| PAI-1 −675 4G5G | - | - | - | - | - | - | - | - | - | - |
| 4G4G | 113 (57.4) | 69 (43.7) | 1.000 (reference) | 33 (46.5) | 1.000 (reference) | - | 36 (41.4) | 1.000 (reference) | - | |
| 4G5G | 75 (38.1) | 70 (44.3) | 1.550 (0.967–2.485) | 0.069 | 32 (45.1) | 1.316 (0.716–2.419) | 0.376 | 38 (43.7) | 1.653 (0.921–2.968) | 0.092 |
| 5G5G | 9 (4.6) | 19 (12.0) | 3.032 (1.224–7.512) | 0.017 | 6 (8.5) | 1.769 (0.552–5.665) | 0.337 | 13 (14.9) | 4.646 (1.625–13.29) | 0.004 |
| Dominant (4G4G vs. 4G5G + 5G5G) | - | - | 1.727 (1.102–2.706) | 0.017 | - | 1.366 (0.764–2.441) | 0.293 | - | 1.969 (1.130–3.430) | 0.017 |
| Recessive (4G4G + 4G5G vs. 5G5G) | - | - | 2.510 (1.056–5.968) | 0.037 | - | 1.584 (0.516–4.864) | 0.422 | - | 3.378 (1.301–8.769) | 0.012 |
| HWE-P | 0.435 | 0.847 | - | - | - | - | - | - | - | - |
| PAI-1 +43 | - | - | - | - | - | - | - | - | - | - |
| GG | 180 (91.4) | 132 (83.5) | 1.000 (reference) | - | 61 (85.9) | 1.000 (reference) | - | 71 (81.6) | 1.000 (reference) | - |
| GA | 16 (8.1) | 24 (15.2) | 2.006 (0.963–4.175) | 0.063 | 8 (11.3) | 1.598 (0.596–4.284) | 0.352 | 16 (18.4) | 2.421 (1.057–5.546) | 0.037 |
| AA | 1 (0.5) | 2 (1.3) | 3.188 (0.270–37.664) | 0.358 | 2 (2.8) | 7.504 (0.561–100.480) | 0.128 | 0 (0.0) | N/A | 0.998 |
| Dominant (GG vs. GA + AA) | - | - | 2.087 (1.027–4.241) | 0.042 | - | 1.941 (0.775–4.860) | 0.157 | - | 2.292 (1.009–5.206) | 0.048 |
| Recessive (GG + GA vs. AA) | - | - | 2.972 (0.251–35.212) | 0.388 | - | 7.202 (0.531–97.693) | 0.138 | - | N/A | 0.998 |
| HWE-P | 0.336 | 0.454 | - | - | - | - | - | - | - | - |
| PAI-1 +9785 | - | - | - | - | - | - | - | - | - | - |
| GG | 182 (92.4) | 148 (93.7) | 1.000 (reference) | - | 68 (95.8) | 1.000 (reference) | - | 80 (92.0) | 1.000 (reference) | - |
| GA | 14 (7.1) | 10 (6.3) | 1.072 (0.437–2.633) | 0.879 | 3 (4.2) | 0.946 (0.252–3.549) | 0.934 | 7 (8.0) | 1.324 (0.477–3.669) | 0.590 |
| AA | 1 (0.5) | 0 (0.0) | N/A | 0.995 | 0 (0.0) | N/A | 0.998 | 0 (0.0) | N/A | 0.998 |
| Dominant (GG vs. GA + AA) | - | - | 1.005 (0.414–2.440) | 0.991 | - | 0.898 (0.241–3.344) | 0.872 | - | 1.227 (0.447–3.365) | 0.691 |
| Recessive (GG + GA vs. AA) | - | - | N/A | 0.995 | - | N/A | 0.998 | - | N/A | 0.998 |
| HWE-P | 0.217 | 0.681 | - | - | - | - | - | - | - | - |
| PAI-1 +11053 | - | - | - | - | - | - | - | - | - | - |
| TT | 54 (27.4) | 33 (20.9) | 1.000 (reference) | 15 (21.1) | 1.000 (reference) | - | 18 (20.7) | 1.000 (reference) | - | |
| TG | 101 (51.3) | 85 (53.8) | 1.347 (0.768–2.362) | 0.298 | 36 (50.7) | 1.036 (0.493–2.176) | 0.926 | 49 (56.3) | 1.647 (0.814–3.334) | 0.166 |
| GG | 42 (21.3) | 40 (25.3) | 1.655 (0.858–3.190) | 0.133 | 20 (28.2) | 1.920 (0.825–4.470) | 0.130 | 20 (23.0) | 1.521 (0.664–3.483) | 0.322 |
| Dominant (TT vs. TG + GG) | - | - | 1.429 (0.842–2.428) | 0.186 | - | 1.253 (0.632–2.483) | 0.518 | - | 1.593 (0.814–3.116) | 0.174 |
| Recessive (TT + TG vs. GG) | - | - | 1.285 (0.762–2.165) | 0.347 | - | 1.499 (0.773–2.907) | 0.231 | - | 1.108 (0.581–2.114) | 0.755 |
| HWE-P | 0.682 | 0.326 | - | - | - | - | - | - | - | - |
* The adjusted odds ratio on the basis of risk factors, such as age, hypertension, diabetes mellitus. HWE-P: Hardy–Weinberg equilibrium p-value. N/A, not applicable.
2.2. Haplotype Analysis
The linkage disequilibrium of the PAI-1 polymorphisms at loci −844/−675/43/9785/11053 in patients with OVCF and those in the control group is shown in Figure S1. There was strong linkage disequilibrium between loci −844 and −675 (D’ = 0.838, LOD = 8.42, r2 = 0.153), −844 and +43 (D’ = 0.764, LOD = 1.2, r2 = 0.02) in the control group, whereas OVCF patients showed strong linkage disequilibrium between loci +43 and +11053 (D’ = 1.000, LOD = 4.51, r2 = 0.106), +43 and +9785 (D’ = 0.831, LOD = 0.06, r2 = 0.002). Haplotype analysis of five, four, three, and two loci is presented in Table 3 and Tables S3–S5. Five-polymorphism allelic combination analysis resulted in meaningful combination models: G-4G-G-G-G (odds ratio (OR), 2.231; 95% CI, 1.189–4.187; p = 0.015), G-4G-A-G-T (OR, 62.33; 95% CI, 3.547–1095; p < 0.0001), G-4G-A-G-G (OR, 8.000; 95% CI, 1.996–32.06; p = 0.002), G-5G-G-G-T (OR, 2.565; 95% CI, 1.483–4.434; p = 0.001), G-5G-G-G-G (OR, 5.571; 95% CI, 2.039–15.22; p = 0.001), G-5G-A-G-T (OR, 5.455; 95% CI, 2.353–12.64; p < 0.0001), A-4G-G-G-G (OR, 2.195; 95% CI, 1.346–3.580; p = 0.002), A-4G-G-A-G (OR, 32.65; 95% CI, 1.754–607.7; p = 0.001), A-4G-A-G-G (OR, 45.00; 95% CI, 5.706–354.9; p < 0.0001), A-5G-G-G-T (OR, 38.590; 95% CI, 2.112–705.1; p = 0.0004), and A-5G-A-G-T (OR, 56.40; 95% CI, 3.188–997.7; p < 0.0001) (Table 3). In Table 3, we found difference between non-OVCF and OVCF risk in haplotype analysis. Haplotype analyses of four-, three-, and two-polymorphism allelic combinations demonstrated many statistically significant results, which are listed in Tables S3–S5.
Table 3.
Comparison of genotype frequencies of PAI-1 gene haplotype between the osteoporosis, non-OVCF, OVCF patients and control subjects.
| Haplotype | Overall (n = 355) | Control (n = 197) | Case (n = 158) | OR (95% CI) | p a | Non-OVCF (n = 71) | OR (95% CI) | p a | OVCF (n = 87) | OR (95% CI) | p a |
|---|---|---|---|---|---|---|---|---|---|---|---|
| PAI-1 −844/−675/+43/+9785/+11053 | - | - | - | - | - | - | - | - | - | ||
| G-4G-G-G-T | 0.179 | 0.237 | 0.098 | 1.000 (reference) | - | 0.107 | 1.000 (reference) | - | 0.133 | 1.000 (reference) | - |
| G-4G-G-G-G | 0.092 | 0.099 | 0.092 | 2.231 (1.189–4.187) | 0.015 | 0.127 | 2.862 (1.311–6.247) | 0.013 | 0.099 | 1.763 (0.849–3.658) | 0.177 |
| G-4G-G-A-T | 0.008 | 0.019 | 0.000 | 0.198 (0.011–3.567) | 0.197 | 0.000 | 0.402 (0.022–7.408) | 0.592 | 0.002 | 0.265 (0.015–4.816) | 0.346 |
| G-4G-G-A-G | 0.006 | 0.007 | 0.000 | 0.424 (0.023–8.443) | 1.000 | 0.000 | 0.862 (0.042–17.52) | 1.000 | 0.015 | 4.043 (0.765–21.36) | 0.110 |
| G-4G-A-G-T | 0.007 | 0.000 | 0.032 | 62.33 (3.547–109.5) | <0.0001 | 0.008 | 18.10 (0.704–465.0) | 0.147 | 0.012 | 19.89 (0.923–428.8) | 0.044 |
| G-4G-A-G-G | 0.021 | 0.007 | 0.025 | 8.000 (1.996–32.06) | 0.002 | 0.000 | 0.862 (0.042–17.52) | 1.000 | 0.000 | 0.568 (0.028–11.40) | 1.000 |
| G-4G-A-A-T | 0.004 | 0.000 | 0.004 | 8.905 (0.353–224.4) | 0.256 | 0.000 | N/A | - | 0.006 | 11.94 (0.471–302.7) | 0.205 |
| G-5G-G-G-T | 0.157 | 0.158 | 0.168 | 2.565 (1.483–4.434) | 0.001 | 0.173 | 2.500 (1.221–5.118) | 0.013 | 0.140 | 1.565 (0.812–3.017) | 0.184 |
| G-5G-G-G-G | 0.029 | 0.018 | 0.043 | 5.571 (2.039–15.22) | 0.001 | 0.047 | 6.200 (1.903–20.20) | 0.004 | 0.058 | 5.776 (1.984–16.82) | 0.001 |
| G-5G-G-A-T | 0.009 | 0.006 | 0.000 | 0.594 (0.028–12.71) | 1.000 | 0.013 | 6.200 (0.810–47.44) | 0.109 | 0.004 | 2.022 (0.176–23.29) | 0.495 |
| G-5G-G-A-G | 0.002 | 0.003 | 0.000 | 0.989 (0.039–24.93) | 1.000 | 0.001 | 2.011 (0.078–51.66) | 1.000 | 0.001 | 1.326 (0.052–33.63) | 1.000 |
| G-5G-A-G-T | 0.042 | 0.027 | 0.062 | 5.455 (2.353–12.64) | <0.0001 | 0.067 | 5.636 (2.042–15.56) | 0.001 | 0.061 | 4.043 (1.560–10.48) | 0.006 |
| G-5G-A-G-G | 0.007 | 0.003 | 0.007 | 6.000 (0.526–68.51) | 0.165 | 0.001 | 2.011 (0.078–51.66) | 1.000 | 0.001 | 1.326 (0.052–33.63) | 1.000 |
| G-5G-A-A-T | 0.000 | 0.003 | 0.000 | 0.989 (0.039–24.93) | 1.000 | 0.001 | 2.011 (0.078–51.66) | 1.000 | 0.001 | 1.326 (0.052–33.63) | 1.000 |
| A-4G-G-G-T | 0.062 | 0.076 | 0.056 | 1.800 (0.883–3.668) | 0.132 | 0.079 | 2.273 (0.943–5.483) | 0.089 | 0.028 | 0.674 (0.236–1.928) | 0.621 |
| A-4G-G-G-G | 0.310 | 0.311 | 0.283 | 2.195 (1.346–3.580) | 0.002 | 0.361 | 2.571 (1.361–4.855) | 0.004 | 0.329 | 1.874 (1.077–3.261) | 0.032 |
| A-4G-G-A-T | 0.006 | 0.003 | 0.005 | 6.000 (0.526–68.51) | 0.165 | 0.008 | 6.200 (0.368–104.6) | 0.271 | 0.010 | 8.087 (0.702–93.16) | 0.111 |
| A-4G-A-G-T | 0.009 | 0.003 | 0.000 | 0.989 (0.039–24.93) | 1.000 | 0.001 | 2.011 (0.078–51.66) | 1.000 | 0.001 | 1.326 (0.052–33.63) | 1.000 |
| A-4G-A-G-G | 0.014 | 0.003 | 0.046 | 45.00 (5.706–354.9) | <0.0001 | 0.001 | 2.011 (0.078–51.66) | 1.000 | 0.001 | 1.326 (0.052–33.63) | 1.000 |
| A-5G-G-G-T | 0.011 | 0.000 | 0.020 | 38.59 (2.112–705.1) | 0.0004 | 0.000 | N/A | - | 0.076 | 107.4 (6.156–1875) | <0.0001 |
| A-5G-G-G-G | 0.011 | 0.018 | 0.006 | 0.857 (0.169–4.347) | 1.000 | 0.000 | 0.402 (0.022–7.408) | 0.592 | 0.011 | 1.155 (0.225–5.937) | 1.000 |
| A-5G-A-G-T | 0.013 | 0.000 | 0.029 | 56.40 (3.188–997.7) | <0.0001 | 0.010 | 18.100 (0.704–465.0) | 0.147 | 0.013 | 19.89 (0.923–428.8) | 0.044 |
a Fisher’s exact test. N/A, not applicable.
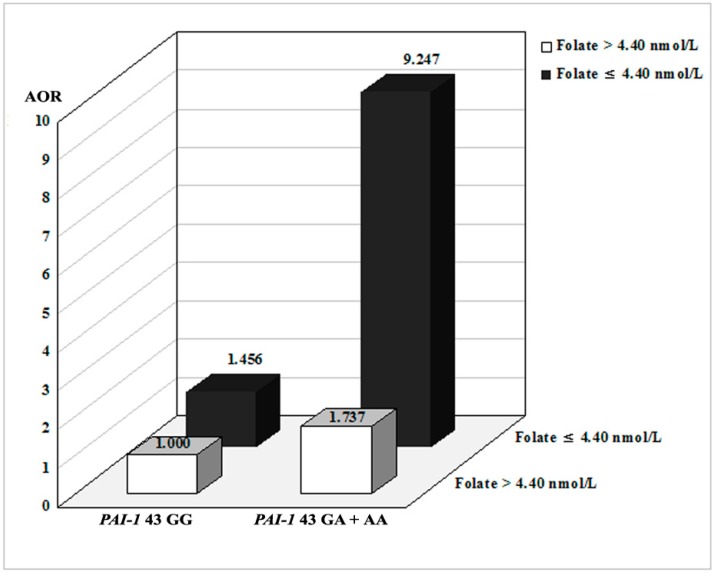
2.3. Combined Effects between PAI-1 Polymorphisms and Environmental Factors
To determine additional clinical significance, we performed stratified (Table S6) and gene–environment interaction (Table S7) analyses according to hypertension, diabetes mellitus, 25-hydroxyl vitamin D (25-OH vit. D), vitamin B12, folate, and plasma total homocysteine (tHcy). We divided subjects into two groups representing the upper and lower 15% cutoff values for plasma tHcy and folate levels (folate: 4.40 ng/mL, tHcy: 12.41 µmol/L). We performed stratified analyses comparing clinical factors and polymorphisms (Table S6). Clinical risk factors strongly correlated with PAI-1 −844 G > A, and −675 4G > 5G polymorphisms. In gene–environment interaction studies (Table S7), the PAI-1 −675 polymorphism, coupled with low plasma folate levels or high homocysteine levels, was associated with an increased odds ratio when comparing osteoporosis patients with control subjects. In addition, when comparing the association of PAI-1 +43 and plasma folate levels with osteoporosis (Figure 1), the PAI-1 +43 GA + AA genotype combined with low plasma folate levels produced a significant result (GG vs. GA + AA: AOR, 9.247; 95% CI, 1.049–81.51). In addition, we evaluated the effects of PAI-1 genotypes on bone mineral density (BMD), plasma vitamin B12, 25-OH vit. D concentrations, and bone metabolism markers (osteocalcin and deoxypyridinoline) in Table S8. PAI-1 −844G > A was significantly associated with BMD. Reduced osteocalcin and deoxypyridinoline were influenced by PAI-1 −844GA + AA and 11053TG + GG genotypes, respectively (Figure S2).
Figure 1.
Osteoporosis risk stratified by interaction between PAI-1 +43G > A and plasma folate levels. Combinations of the PAI-1 +43 genotype and plasma folate level subgroups. We divided subjects into two groups representing the lower 15% cutoff values for plasma folate levels: >4.40 ng/mL and ≤4.40 ng/mL.
3. Discussion
Osteoporosis and low BMD commonly occur in postmenopausal women and lead to increased susceptibility to fractures. BMD, along with other factors, is known to contribute to skeletal health [24]. In particular, the role of genetic factors, including gene polymorphisms, takes center stage in pathogenic studies [8,25,26]. Recent studies investigated synergic effects between gene polymorphisms and OVCF risk factors [27,28,29].
PAI-1 is a downregulator of the fibrinolysis gene and the key factor for plasminogen ratios [23,30]. Rundle et al. [31] showed that PAI-1 deficiency results in an increase in not only callus size but also callus cartilage regeneration in PAI-1 knockout (KO) mice recovering from fractures. In addition, fracture callus development was promoted in PAI-1 KO mice in comparison to control mice. These results showed strengthened tissue fibrinolysis in PAI-1 deficiency, which may enhance fracture recovery by facilitating extracellular matrix regeneration [23,31]. This is consistent with our current finding that an abnormal plasminogen level adversely affects bone recovery and regeneration. Furthermore, fibrinolysis in tissue can be a crucial factor in both acute inflammation and fracture restoration [23,32].
A previous study [33] described the 10 most well-known polymorphisms of PAI-1, as follows: rs2227631 G > A, rs6092 G > A, rs2227708 C > T, rs2227662 C > T, rs2227666 G > A, rs2227667 A > G, rs2227672 G > T, rs2227683 A > G, rs2227694 G > A, and rs7242 T > G. The rs1799889 (PAI-1 −675 4G > 5G) polymorphism is widely genotyped in PAI-1 genetic studies. The five polymorphisms selected for our study affect transcription and are expected to regulate PAI-1 levels. Therefore, we hypothesized that regulation of PAI-1 activity by PAI-1 polymorphisms results in an abnormality in the bone repair system or bone loss mechanism. Furthermore, postmenopausal women have an increased risk for OVCF because of sex hormone dysregulation. We have identified an association between PAI-1 polymorphisms and OVCF prevalence. Based on statistical analyses, this result demonstrates a significant correlation between PAI-1 −844A > G, −675 4G > 5G, and 43G > A, and OVCF risk. However, another study reported the lack of any association between the rs1799889 (PAI-1 −675 4G > 5G) polymorphism and osteoporosis in Turkish postmenopausal women [34]. Interestingly, this finding conflicts with the results of our research; the discrepancy could be due to differences in the ethnic group or sample size used. On the other hand, the Turkish postmenopausal women exhibited only osteoporosis [35], whereas our study participants exhibited symptoms of greater severity, such as compound fracture due to osteoporosis; this could also be the reason for the discrepancy between the results of the two studies. There are several limitations to our study. First, serum PAI-1 concentrations were not examined in our study population. Previous studies have evaluated the contribution of each PAI-1 polymorphism to serum PAI-1 expression [35,36,37]. Second, functional studies for PAI-1 SNP were not performed to elucidate OVCF-related pathogenesis. Although several studies have reported an association between PAI-1 polymorphisms and bone repair, few have evaluated the pathogenesis by which PAI-1 polymorphisms affect osteoporosis in postmenopausal women. This study cannot, therefore, propose a detailed pathogenesis by which PAI-1 polymorphism affects vertebral artery and tissue. Finally, PAI-1 expression depends on the PAI-1 single nucleotide polymorphism (SNP) genotypes in the local tissue; therefore, PAI-1 expression in vertebral tissue is more important than that in serum.
4. Materials and Methods
4.1. Study Population
This was a case-control study, in which the case group consisted of 158 osteoporotic postmenopausal women (mean age ± SD, 69.50 ± 8.24 years; age range, 56–81 years), defined as having a T-score of −2.5 or lower and/or at least one non-traumatic fracture of the spine. Women were recruited from the Neurosurgery and Orthopedic Surgery Departments at CHA Bundang Medical Center, CHA University of South Korea between March 2005 and December 2008. The control group consisted of 197 postmenopausal women (mean age ± SD, 66.57 ± 8.05 years; age range, 50–85 years) without disease and not taking any medications known to influence bone mass or bone turnover. BMD at the lumbar spine was measured using a dual-energy X-ray (Hologic Discovery W, Waltham, MA, USA). An OVCF was defined as a ≥15% reduction in the anterior, posterior, or central height of the vertebra [38]. All examinations were performed by a trained neurosurgeon and orthopedic surgeon according to previously described methods [39]. All subjects provided their informed consent for inclusion before they participated in the study. The study was conducted in accordance with the Declaration of Helsinki, and the protocol was approved by the Ethics Committee of the Institutional Review Board of CHA Bundang Medical Center on 20 January 2014 (reference No. BD2015-043). We provided each participant with a full explanation of participation in this study and obtained confirmed written consent from all study participants. Bone mineral density (BMD) of the lumbar spine (L2–L4), femur neck (FN), Ward’s triangle, and trochanter (Tro) were measured using dual-energy X-ray absorptiometry (Norland Medical Systems, White Plains, NY, USA). Osteoporosis was defined according to the 1994 classification of the World Health Organization (WHO) [40].
4.2. Genotyping
We performed DNA extraction from peripheral blood with an anticoagulant tube using the G-DEX™ II kit (Intron Biotechnology, Seongnam, Korea). The PAI-1 polymorphisms were amplified by polymerase chain reaction and digested with a restriction enzyme to identify them via restriction fragment length polymorphism (RFLP; Table S9) [41]. We selected 30% of the PCR product at random and checked the RFLP results for concordance with DNA sequencing results. The concordance of the quality control samples was 100%.
4.3. Bone Measurements
The diagnosis of osteoporosis was based on WHO criteria (dual energy X-ray absorptiometry (DXA) hip or lumbar T-score <−2.5 standard deviations), and an OVCF was diagnosed when a progressive or newly generated compression fracture was identified after low-energy trauma. The BMD T-score was measured in g/cm2 using Hologic densitometers (Hologic Inc., Waltham, MA, USA) [39]. The control group had a BMD T-score greater than −1.0 and had no spine or hip fractures based on the results of simple radiography. The BMD T-score analysis in this study was conducted with reference to the WHO report [40].
4.4. Measurement of Vitamin B12, Plasma Total Homocysteine (tHcy), and Folate Levels
We collected plasma samples to measure vitamin B12, tHcy, and folate levels within 48 h of osteoporosis detection. Twelve hours after the patient’s previous meal, we collected whole blood in a tube containing anticoagulant. We centrifuged the tube for 15 min at 1000× g to separate the plasma and stored it at −80 °C. Plasma vitamin B12 concentrations were measured using the BioRad Quantaphase II radioassay (Hercules, CA, USA). We measured plasma tHcy concentration using a fluorescent polarizing immunoassay with the IMx system (Abbott Laboratories, Chicago, IL, USA) and the plasma folate concentration with a radio assay kit (ACS 180; Bayer, Tarrytown, NY, USA).
4.5. Statistical Analysis
The genotype and allele combination frequency differences between case and control subjects were analyses by logistic regression and Fisher’s exact test. The adjusted odds ratio (AORs) and confidence intervals (CIs) were used as a measure of the association between genotype frequencies and osteoporosis. All of the alleles were in Hardy–Weinberg equilibrium (p > 0.05). The genotypes with osteoporosis and OVCF occurrence was calculated with AORs and 95% CIs from logistic regression adjusted for age, hypertension, and diabetes mellitus. The linkage disequilibrium (LD) with blocking calculation with HaploView software and haplotype analysis for the models chosen by multifactor dimensionality reduction (MDR) methods were checked with the HAPSTAT program version 3.0 (www.bios.unc.edu/~lin/hapstat). The correlations of genotypes with BMD, as well as plasma folate, vitamin B12, 25-hydroxyl vitamin D, osteocalcin and deoxypyridinoline levels, were evaluated by Kruskal–Wallis test and Mann–Whitney test. Statistical analyses were performed by GraphPad Prism 4.0 (GraphPad Software Inc., San Diego, CA, USA), MedCalc software version 16.8.4 (MedCalc Ltd., Ostend, Belgium), HaploView 4.1 (Broad Inc., Cambridge, MA, USA), and HAPSTAT 3.0 (Univ. of North Carolina, Chapel Hill, NC, USA).
5. Conclusions
In summary, we found an association between PAI-1 polymorphisms and osteoporosis risk in postmenopausal women. Furthermore, PAI-1 polymorphisms were shown to strongly association with OVCF occurrence. Interestingly, our results suggest differences between non-OVCF and OVCF patients in this association with PAI-1 polymorphisms. In particular, the PAI-1 −844G > A, −675 4G > 5G, +43G > A polymorphisms were associated with increased susceptibility for OVCF rather than non-OVCF and osteoporosis. Therefore, we expect a potentially higher fracture risk in postmenopausal women who are osteoporosis patients with these PAI-1 polymorphisms. Our findings present the first report on the association between PAI-1 polymorphisms and OVCF. In conclusion, this study suggests that PAI-1 polymorphisms (−844G > A, −675 4G > 5G, +43G > A) may contribute to OVCF and could be used as genetic biomarkers for OVCF risk.
Acknowledgments
This work was supported by National Research Foundation of Korea Grants funded by the Korean Government (NRF-2015R1D1A1A09057432, NRF-2014R1A2A2A01003994 and NRF-2014R1A1A2059118) and by the Korea Health Technology R&D Project through the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (grant number: HI15C1972010015).
Supplementary Materials
Supplementary materials can be found at www.mdpi.com/1422-0067/17/12/2062/s1.
Author Contributions
Nam Keun Kim designed and directed the whole project. Yeon Ho Lee, Tae Keun Ahn, Jae Joon Lim, Young Sun Chung, Woo Sik Lee, In Bo Han collected the blood samples from osteoporosis patients and control subjects. Jung Oh Kim and Soo Hong Han performed the experiments, collected the results, and analyzed the data. Woo Sik Lee, In Bo Han, Dong Eun Shin and Soo Hong Han discussed and interpreted the data and results. Jung Oh Kim wrote the first draft of the manuscript. All authors contributed to and have approved the final manuscript.
Conflicts of Interest
All authors declare no conflicts of interest.
References
- 1.Center J.R., Nguyen T.V., Schneider D., Sambrook P.N., Eisman J.A. Mortality after all major types of osteoporotic fracture in men and women: An observational study. Lancet. 1999;353:878–882. doi: 10.1016/S0140-6736(98)09075-8. [DOI] [PubMed] [Google Scholar]
- 2.Anne K., Lucile A.-C., Tamsen B., Steven N.B., Scott D.B., Kay D., David R.G., Lou G., Steven R.G., Keith H., et al. Osteoporosis prevention, diagnosis, and therapy. JAMA. 2001;285:785–795. doi: 10.1001/jama.285.6.785. [DOI] [PubMed] [Google Scholar]
- 3.Dawson-Hughes B., National Osteoporosis Foundation Guide Committee A revised clinician’s guide to the prevention and treatment of osteoporosis. J. Clin. Endocrinol. Metab. 2008;93:2463–2465. doi: 10.1210/jc.2008-0926. [DOI] [PubMed] [Google Scholar]
- 4.Costa N., Paramanathan S., Mac Donald D., Wierzbicki A.S., Hampson G. Factors regulating circulating vascular endothelial growth factor (VEGF): Association with bone mineral density (BMD) in post-menopausal osteoporosis. Cytokine. 2009;46:376–381. doi: 10.1016/j.cyto.2009.03.012. [DOI] [PubMed] [Google Scholar]
- 5.Francesco M., Jean Y.R., Maria L.B. Genetics of menopause-associated diseases. Maturitas. 2001;40:103–116. doi: 10.1016/s0378-5122(01)00283-3. [DOI] [PubMed] [Google Scholar]
- 6.Pouilles J.M., Tremollieres F., Bonneu M., Ribot C. Influence of early age at menopause on vertebral bone mass. J. Bone Miner. Res. 1994;9:311–315. doi: 10.1002/jbmr.5650090304. [DOI] [PubMed] [Google Scholar]
- 7.Urano T., Inoue S. Genetics of osteoporosis. Biochem. Biophys. Res. Commun. 2014;452:287–293. doi: 10.1016/j.bbrc.2014.07.141. [DOI] [PubMed] [Google Scholar]
- 8.Flicker L., Hopper J.L., Rodgers L., Kaymakci B., Green R.M., Wark J.D. Bone density determinants in elderly women: A twin study. J. Bone Miner. Res. 1995;10:1607–1613. doi: 10.1002/jbmr.5650101102. [DOI] [PubMed] [Google Scholar]
- 9.Smith D.M., Nance W.E., Kang K.W., Christian J.C., Johnston C.C., Jr. Genetic factors in determining bone mass. J. Clin. Investig. 1973;52:2800–2808. doi: 10.1172/JCI107476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Young D., Hopper J.L., Nowson C.A., Green R.M., Sherwin A.J., Kaymakci B., Smid M., Guest C.S., Larkins R.G., Wark J.D. Determinants of bone mass in 10- to 26-year-old females: A twin study. J. Bone Miner. Res. 1995;10:558–567. doi: 10.1002/jbmr.5650100408. [DOI] [PubMed] [Google Scholar]
- 11.Nelson D.A., Kleerekoper M. The search for the osteoporosis gene. J. Clin. Endocrinol. Metab. 1997;82:989–990. doi: 10.1210/jc.82.4.989. [DOI] [PubMed] [Google Scholar]
- 12.Vidal C., Brincat M., Anastasi A.X. TNFRSF11B gene variants and bone mineral density in postmenopausal women in Malta. Maturitas. 2006;53:386–395. doi: 10.1016/j.maturitas.2005.11.003. [DOI] [PubMed] [Google Scholar]
- 13.Firat S.C., Cetin Z., Samanci N., Aydin F., Balci N., Gungor F., Firat M.Z., Luleci G., Karauzum S.B. Evaluation of eNOS gene polymorphisms in relation to BMD in postmenopausal women. Maturitas. 2009;63:352–356. doi: 10.1016/j.maturitas.2009.05.004. [DOI] [PubMed] [Google Scholar]
- 14.Singh M., Singh P., Singh S., Juneja P.K., Kaur T. A susceptible haplotype within APOE gene influences BMD and intensifies the osteoporosis risk in postmenopausal women of Northwest India. Maturitas. 2010;67:239–244. doi: 10.1016/j.maturitas.2010.06.017. [DOI] [PubMed] [Google Scholar]
- 15.Mencej-Bedrač S., Preželj J., Marc J. TNFRSF11B gene polymorphisms 1181G > C and 245T > G as well as haplotype CT influence bone mineral density in postmenopausal women. Maturitas. 2011;69:263–267. doi: 10.1016/j.maturitas.2011.02.010. [DOI] [PubMed] [Google Scholar]
- 16.Marshall A.L., Thomas J.K., Uri S. Williams Hematology. 8th ed. McGraw-Hill Education; Columbus, OH, USA: 2010. pp. 2742–2743. [Google Scholar]
- 17.Dellas C., Loskutoff D.J. Historical analysis of PAI-1 from its discovery to its potential role in cell motility and disease. Thromb. Haemost. 2005;93:631–640. doi: 10.1160/TH05-01-0033. [DOI] [PubMed] [Google Scholar]
- 18.Lijnen H.R. Pleiotropic functions of plasminogen activator inhibitor-1. J. Thromb. Haemost. 2005;3:35–45. doi: 10.1111/j.1538-7836.2004.00827.x. [DOI] [PubMed] [Google Scholar]
- 19.Daci E., Verstuyf A., Moermans K., Bouillon R., Carmeliet G. Mice lacking the plasminogen activator inhibitor 1 are protected from trabecular bone loss induced by estrogen deficiency. J. Bone Miner. Res. 2000;15:1510–1516. doi: 10.1359/jbmr.2000.15.8.1510. [DOI] [PubMed] [Google Scholar]
- 20.Tamura Y., Kawao N., Okada K., Yano M., Okumoto K., Matsuo O., Kaji H. Plasminogen activator inhibitor-1 is involved in streptozotocin-induced bone loss in female mice. Diabetes. 2013;62:3170–3179. doi: 10.2337/db12-1552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mao L., Kawao N., Tamura Y., Okumoto K., Okada K., Yano M., Matsuo O., Kaji H. Plasminogen activator inhibitor-1 is involved in impaired bone repair associated with diabetes in female mice. PLoS ONE. 2014;9:e92686. doi: 10.1371/journal.pone.0092686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kawao N., Tamura Y., Okumoto K., Yano M., Okada K., Matsuo O., Kaji H. Plasminogen plays a crucial role in bone repair. J. Bone Miner. Res. 2013;28:1561–1574. doi: 10.1002/jbmr.1921. [DOI] [PubMed] [Google Scholar]
- 23.Voormolen M.H., van Rooij W.J., van der Graaf Y., Lohle P.N., Lampmann L.E., Juttmann J.R., Sluzewski M. Bone marrow edema in osteoporotic vertebral compression fractures after percutaneous vertebroplasty and relation with clinical outcome. AJNR Am. J. Neuroradiol. 2006;27:983–988. [PMC free article] [PubMed] [Google Scholar]
- 24.Zofkova I. Role of genetics in prediction of osteoporosis risk. Vnitr. Lek. 2011;57:78–84. [PubMed] [Google Scholar]
- 25.Mosaad Y.M., Hammad E.M., Fawzy Z., Abdal Aal I.A., Youssef H.M., ElSaid T.O., Monir R., El-Deek B.S. Vitamin D receptor gene polymorphism as possible risk factor in rheumatoid arthritis and rheumatoid related osteoporosis. Hum. Immunol. 2014;75:452–461. doi: 10.1016/j.humimm.2014.02.009. [DOI] [PubMed] [Google Scholar]
- 26.Chung Y.S., Jeon Y.J., Shin D.E., Min K.T., Shin Y.S., Won K.S., Koh Y.C., Hong S.H., Kim N.K. Methylenetetrahydrofolate reductase (MTHFR) and thymidylate synthase (TS) polymorphisms with osteoporotic vertebral compression fracture (OVCF) in postmenopausal Korean women. Genes Genom. 2012;34:257–263. doi: 10.1007/s13258-011-0202-2. [DOI] [Google Scholar]
- 27.Jin H.S., Kim B.Y., Kim J., Hong K.W., Jung S.Y., Lee Y.S., Huh D., Oh B., Chung Y.S., Jeong S.Y. Association between the SPRY1 gene polymorphism and obesity-related traits and osteoporosis in Korean women. Mol. Genet. Metab. 2013;108:95–101. doi: 10.1016/j.ymgme.2012.10.017. [DOI] [PubMed] [Google Scholar]
- 28.Lei S.F., Papasian C.J., Deng H.W. Polymorphisms in predicted miRNA binding sites and osteoporosis. J. Bone Miner. Res. 2011;26:72–78. doi: 10.1002/jbmr.186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Romer J., Lund L.R., Eriksen J., Ralfkiaer E., Zeheb R., Gelehrter T.D., Danø K., Kristensen P. Differential expression of urokinase-type plasminogen activator and its type-1 inhibitor during healing of mouse skin wounds. J. Investig. Dermatol. 1991;97:803–811. doi: 10.1111/1523-1747.ep12486833. [DOI] [PubMed] [Google Scholar]
- 30.Rundle C.H., Wang X., Wergedal J.E., Mohan S., Lau K.H. Fracture healing in mice deficient in plasminogen activator inhibitor-1. Calcif. Tissue Int. 2008;83:276–284. doi: 10.1007/s00223-008-9169-7. [DOI] [PubMed] [Google Scholar]
- 31.Daci E., Everts V., Torrekens S., van Herck E., Tigchelaar-Gutterr W., Bouillon R., Carmeliet G. Increased bone formation in mice lacking plasminogen activators. J. Bone Miner. Res. 2003;18:1167–1176. doi: 10.1359/jbmr.2003.18.7.1167. [DOI] [PubMed] [Google Scholar]
- 32.Morange P.E., Saut N., Alessi M.C., Yudkin J.S., Margaglione M., di Minno G., Hamsten A., Humphries S.E., Tregouet D.A., Juhan-Vague I. Association of plasminogen activator inhibitor (PAI)-1 (SERPINE1) SNPs with myocardial infarction, plasma PAI-1, and metabolic parameters: The HIFMECH study. Arterioscler. Thromb. Vasc. Biol. 2007;27:2250–2257. doi: 10.1161/ATVBAHA.107.149468. [DOI] [PubMed] [Google Scholar]
- 33.Ozgen M., Cosan D.T., Doganer F., Soyocak A., Armagan O., Gunes H.V., Degirmenci I., Ozkara G.O., Mutlu F.S. Relationship between plasminogen activator inhibitor type-1 (PAI-1) gene polymorphisms and osteoporosis in Turkish women. Clinics. 2012;67:1299–1302. doi: 10.6061/clinics/2012(11)13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Muñoz-Valle J.F., Ruiz-Quezada S.L., Oregón-Romero E., Navarro-Hernández R.E., Castañeda-Saucedo E., De la Cruz-Mosso U., Illades-Aguiar B., Leyva-Vázquez M.A., Castro-Alarcón N., Parra-Rojas I. PAI-1 mRNA expression and plasma level in rheumatoid arthritis: Relationship with 4G/5G PAI-1 polymorphism. Rheumatol. Int. 2012;32:3951–3956. doi: 10.1007/s00296-011-2279-y. [DOI] [PubMed] [Google Scholar]
- 35.Lima L.M., Carvalho M.D., Fonseca Neto C.P., Garcia J.C., Sousa M.O. PAI-1 4G/5G polymorphism and plasma levels association in patients with coronary artery disease. Arq. Bras. Cardiol. 2011;97:462. doi: 10.1590/S0066-782X2011005000110. [DOI] [PubMed] [Google Scholar]
- 36.Choi J.W., Lee J.H., Park H.S., Kim Y.S. PAI-1 expression and its regulation by promoter 4G/5G polymorphism in clear cell renal cell carcinoma. J. Clin. Pathol. 2011;64:893–897. doi: 10.1136/jclinpath-2011-200182. [DOI] [PubMed] [Google Scholar]
- 37.Liguori R., Quaranta S., di Fiore R., Elce A., Castaldo G., Amato F. A novel polymorphism in the PAI-1 gene promoter enhances gene expression. A novel pro-thrombotic risk factor? Thromb. Res. 2014;134:1229–1233. doi: 10.1016/j.thromres.2014.09.021. [DOI] [PubMed] [Google Scholar]
- 38.Villadsen M.M., Bunger M.H., Carstens M., Stenkjaer L., Langdahl B.L. Methylenetetrahydrofolate reductase (MTHFR) C677T polymorphism is associated with osteoporotic vertebral fractures, but is a weak predictor of BMD. Osteoporos. Int. 2005;16:411–416. doi: 10.1007/s00198-004-1704-4. [DOI] [PubMed] [Google Scholar]
- 39.Gjesdal C.G., Vollset S.E., Ueland P.M., Refsum H., Drevon C.A., Gjessing H.K., Tell G.S. Plasma total homocysteine level and bone mineral density: The Hordaland Homocysteine Study. Arch. Intern. Med. 2006;166:88–94. doi: 10.1001/archinte.166.1.88. [DOI] [PubMed] [Google Scholar]
- 40.WHO Europe: A declaration on the promotion of patients’ rights in Europe. Eur. J. Health Law. 1994;1:279–291. [Google Scholar]
- 41.Jeon Y.J., Kim Y.R., Lee B.E., Choi Y.S., Kim J.H., Shin J.E., Rah H., Cha S.H., Lee W.S., Kim N.K. Genetic association of five plasminogen activator inhibitor-1 (PAI-1) polymorphisms and idiopathic recurrent pregnancy loss in Korean women. Thromb. Haemost. 2013;110:742–750. doi: 10.1160/TH13-03-0242. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.