Abstract
Objective
To examine the relation between baseline measurements of thyroid function and response to selective serotonin reuptake inhibitors (SSRIs) and to consider the effect of these antidepressants on thyroid hormone levels.
Methods
Nineteen subjects with major depression, but without a history of thyroid treatment or lithium treatment, were treated openly with either sertraline or fluoxetine in a university- affiliated tertiary care hospital. Hamilton Depression Rating Scale (Ham-D) scores were measured before and after treatment. Clinical Global Impressions (CGI) scores were measured at study end. Thyroid data, consisting of values for thyroid-stimulating hormone (TSH), triiodothyronine (T3, measured by radioimmunoassay [RIA]), thyroxine (T4, measured by RIA) and free T4, were collected before and after treatment. Complete thyroid data were available for 17 subjects. Data were collected during 1997–1999.
Results
Baseline TSH correlated strongly with response to treatment as measured by change in Ham-D scores (r = 0.64, p = 0.003). Low TSH values correlated with greater improvement in depressive symptoms. Thyroid hormone levels decreased with treatment, but these decreases did not correlate with clinical improvement.
Conclusion
Baseline thyroid function, as measured by serum TSH, may predict a patient's response to antidepressant treatment with SSRIs. Optimal thyroid function, beyond simply being within the normal laboratory values, may be necessary for an optimal response to antidepressants.
Medical subject headings: depression, serotonin uptake inhibitors, thyroid hormones, thyrotropin, thyroxine, triiodothyronine.
Abstract
Objectif
Étudier le lien entre les mesures de base de la fonction thyroïdienne et la réponse aux inhibiteurs spécifiques du recaptage de la sérotonine (ISRS), ainsi que l'effet de ces antidépresseurs sur les concentrations d'hormone thyroïdienne.
Méthodes
On a traité ouvertement à la sertraline ou à la fluoxétine 19 sujets atteints de dépression grave, mais qui n'avaient pas d'antécédents de traitement thyroïdien ou de traitement au lithium, dans un hôpital de soins tertiaires affilié à une université. On a mesuré les scores selon l'échelle de dépression de Hamilton (HDRS) avant et après le traitement. On a mesuré les scores d'impression clinique globale à la fin de l'étude. On a recueilli, avant et après le traitement, des données sur la thyroïde, c.-à-d. des valeurs pour la thyréostimuline (TSH), la triiodothyronine (T3) (mesurée par dosage radio-immunologique [DRI]), la thyroxine (T4) (mesurée par DRI) et la T4 libre. On disposait de données complètes sur la thyroïde pour 17 sujets. Les données ont été recueillies pour la période de 1997 à 1999.
Résultats
On a établi un lien solide entre la TSH de référence et la réponse au traitement mesurée par le changement des scores de la HDRS (r = 0,64, p = 0,003). On a établi un lien entre de faibles valeurs de TSH et une plus grande amélioration des symptômes de dépression. Les concentrations d'hormone thyroïdienne ont diminué avec le traitement, mais il n'y avait pas de lien entre ces diminutions et l'amélioration clinique.
Conclusion
La fonction thyroïdienne de référence mesurée par la concentration sérique de TSH peut permettre de prédire la réponse d'un patient au traitement aux antidépresseurs, soit aux ISRS. Il se peut que la fonction thyroïdienne doive être optimale, outre se situer simplement dans la plage des valeurs normales de laboratoire, pour qu'il y ait réponse optimale aux antidépresseurs.
Introduction
There has long been an interest in the relation between thyroid function and the course of a depressive episode. As part of that interest, many studies have evaluated both the predictive value of baseline thyroid indices and subsequent response to antidepressant treatment, as well as the change in these indices with treatment.1,2,3,4,5 Up to 10% of individuals with depression may present with elevated levels of thyroid-stimulating hormone (TSH) and normal thyroxine (T4) and triiodothyronine (T3) levels (subclinical hypothyroidism).6,7 The clinical impact of an elevated TSH level is still unclear, but preliminary evidence suggests that it may predict a poor response to antidepressants.7
With antidepressant treatment, the most common change in thyroid hormones is a decrease in T4 and free T4 without a significant reduction in TSH.2,5 Of note, these changes are generally within the euthyroid range of values. Some studies have shown that responders to antidepressants show a greater decrease in T4 levels compared with nonresponders.8,9
In this study, we explored these 2 areas by examining, first, the relation between baseline thyroid hormones and the clinical antidepressant response to selective serotonin reuptake inhibitors (SSRIs) and, second, the change in thyroid hormone levels with SSRI treatment.
Methods
All subjects in the current study were recruited from a larger study of the dosing and efficacy of fluoxetine versus sertraline in the treatment of major depression.10 Subjects who agreed to have their peripheral thyroid hormones assayed before and after treatment with the SSRI gave written informed consent and were included in the current study. Nineteen subjects form the sample described in this report. Inclusion criteria were a current diagnosis of major depressive episode, as defined in the Diagnostic and Statistical Manual of Mental Disorders, fourth edition,11 and age between 18 and 60 years. The diagnosis was made by a structured interview with trained raters. Exclusion criteria were as follows: 1) a history of substance abuse within the last 30 days; 2) current or recent treatment with an antidepressant; 3) history of previous manias or hypomanias; 4) previous failure of treatment with fluoxetine or sertraline; and 5) a history of thyroid disease or current treatment with thyroid hormones. No patient was treated with lithium before study entry.
At study entry, baseline clinical assessments included the 21-item Hamilton Depression Rating Scale (Ham-D)12 and the Clinical Global Impressions (CGI) Severity of Illness and Global Improvement scales.13 Subjects were then treated with sertraline, 50 mg daily (n = 8), sertraline, 100 mg daily (n = 4), or fluoxetine, 20 mg daily (n = 7), with medication and dose assigned alternately, that is, patient 1 received sertraline, 50 mg, patient 2, sertraline, 100 mg, and patient 3, fluoxetine, but openly. At 6 weeks, subjects with a Ham-D score above 7 and a CGI Global Improvement score above 1 (less than “marked improvement”) had their daily doses increased to sertraline, 100 mg daily, sertraline, 200 mg daily, or fluoxetine, 40 mg daily, respectively. Total treatment time was 10 weeks. Although subjects were assessed every 2 weeks for 10 weeks, in this report, only the final CGI scores (both severity and improvement subscales) and Ham-D will be considered. Ham-D scores were assessed by research assistants and physicians who all had previous rating training.
At baseline, thyroid indices were measured using standard venipuncture techniques: TSH was assessed using solid-phase immunoradiometric assay, T4 by radioimmunoassay (RIA), T3 by RIA and free T4 by rabbit anti-T4 antibody (Diagnostic Products Kit). For all assays, the intra-assay and interassay variation were less than 10%. Thyroid tests were batch run. At the end of the study, the same thyroid indices were measured again. Two subjects did not complete the post- treatment thyroid measurements. Our sample, therefore, includes 19 subjects at baseline (12 on sertraline and 7 on fluoxetine) and post-treatment clinical evaluation, of whom 17 underwent thyroid evaluations both before and after treatment.
Hormone levels were screened for distributional properties and determined to be appropriate for parametric analysis. Paired t tests were used to evaluate changes in levels of TSH, T4, T3 and free T4 before and after treatment for the 17 patients with values from both time points. Response to treatment was measured by the change in Ham-D scores from before and after treatment, with positive values reflecting improvement in Ham-D symptoms. A stepwise regression analysis was used to predict improvement in Ham-D scores, with baseline values for TSH, T4, T3 and free T4 as the independent variables (n = 19).
Results
The 19 subjects were 10 women and 9 men, with a mean age of 37.6 (standard deviation [SD] 9, range 27–58) years. Four subjects had a high school education or less, 10 were college graduates and 5 had graduate school experience. The mean Ham-D score was 20.7 (SD 1, range 14–31). After treatment, the mean Ham-D score was 7.8 (SD 1.4, range 0–18). Thyroid values at baseline and after treatment for the 17 subjects with complete data are shown in Table 1. There was a slight increase in TSH and a decrease in T4, T3 and free T4 after treatment. These differences were statistically significant for T4 and T3, but not for free T4 or TSH. Changes in Ham-D scores did not correlate significantly with changes in thyroid hormone values.
Table 1
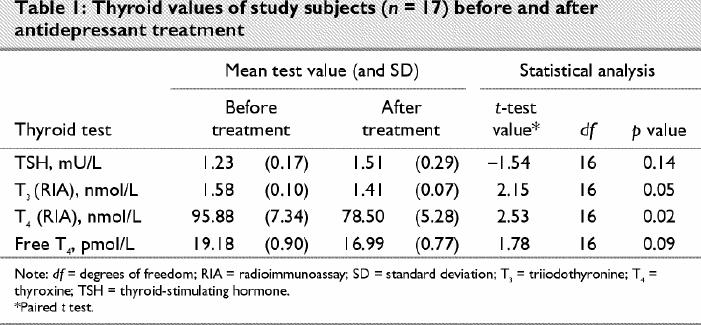
The patients' condition improved by an average of 12.9 points on the Ham-D scale (range –1 to 31) after treatment. The degree of improvement was related significantly to baseline TSH levels (r = 0.64, p = 0.003), with low baseline TSH predicting a greater decline in Ham-D scores (Fig. 1). This relation held even after controlling for initial Ham-D scores. However, this relation was not seen when dividing the sample into subjects with remitting depression (Ham-D score < 8) versus subjects with nonremitting depression (Ham-D score > 8) (t17 = –1.06, p = 0.31). None of the other baseline thyroid indices added significantly to the prediction of response to treatment when correlations and t tests for subjects with remitting depression versus those with nonremitting depression were examined.
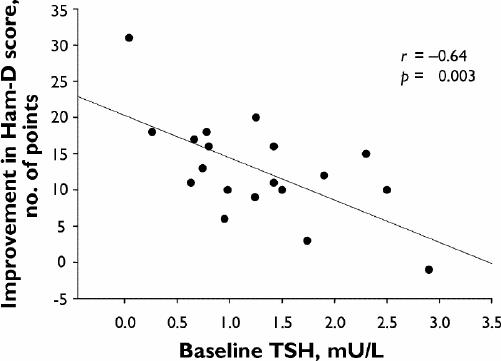
Fig. 1: Correlation of improvement in Hamilton Depression Rating Scale (Ham-D) scores with low baseline thyroid-stimulating hormone (TSH) values.
Discussion
The results of this study suggest that a more active hypothalamic–pituitary–thyroid system, as measured by a lower serum TSH value, is associated with a better response to SSRI antidepressants. The relation was not seen, however, when the sample was split into subjects with remitting depression versus subjects with nonremitting depression.
The small number of subjects studied is a major limitation of the study and suggests the need for caution in the interpretation of our results. Insufficient statistical power because of the small number of subjects might explain some of the negative results seen. Another limitation of the study is the use of 2 SSRIs that, although similar, may have had different effects on and relations to thyroid measures. A third study limitation is the lack of placebo controls, which may have contributed to inflated response rates.
The association between a lower baseline TSH and greater improvement in depressive symptoms is compatible with a small, but consistent, literature that suggests a relation between thyroid indices and clinical response. In the most recent study, Cole et al14 found that a lower baseline free T4 index and a higher TSH value were significantly associated with a poorer response to treatment of bipolar depression. No other variables, whether demographic, clinical or treatment with lithium, explained this association. Similarly, Sane et al15 found a higher free T4 index was associated with a shorter length of stay in hospital (as a measure of response to antidepressant treatment) in men who had been admitted to hospital with major depression.
Furthermore, in this study, changes in peripheral thyroid hormone levels decreased with antidepressant treatment. The reduction in peripheral thyroid indices after antidepressant treatment is also consistent with most, but not all, previous studies.1,5 As noted here, the lack of statistical significance for the changes in free T4 may reflect the small sample in our study.
Few studies have evaluated the association between SSRI treatment for depression and changes in thyroid indices. Shelton et al16 found no significant changes in TSH or total T4 with fluoxetine treatment but found an association between the decline in T3 levels and response to fluoxetine. König et al17 found an 11% decrease in thyroxine levels with paroxetine treatment. As in other studies, we found that changes in TSH values after antidepressant treatment were less consistent than those of T3 and T4.
In summary, the results of our study suggest that more active thyroid function, even within the normal range as measured by TSH values, may predict the response to therapy with SSRIs.
Acknowledgments
This study was supported in part by a grant from Eli Lilly and Company.
Footnotes
Presented at the 153rd annual meeting of the American Psychiatric Association in Chicago on May 13–18, 2000.
Competing interests: None declared for Dr. Frye, Ms. Huynh, Dr. Fairbanks and Dr. Korenman. Dr. Gitlin is in the speaker's bureau for Eli Lilly and Pfizer. Dr. Altshuler has been a consultant for, has received honoraria from and sits on the advisory boards of Abbott, Bristol-Myers Squibb, Eli Lilly, Forest Laboratories and Janssen. She has received grant/research support from Abbott, Eli Lilly and Forest Laboratories and is in the speaker's bureau of Abbott. Dr. Suri has received an honorarium for a speaking engagement with Pfizer. Dr. Bauer has received travel assistance from Eli Lilly and GlaxoSmithKline.
Correspondence to: Dr. Michael Gitlin, 300 UCLA Medical Plaza, Ste. 2200, Los Angeles, CA 90095; fax 310 206-4310; mgitlin@mednet.ucla.edu
Submitted Mar. 6, 2003; Revised Aug. 26, 2003; Accepted Sept. 22, 2003
References
- 1.O'Connor D, Gwirtsman H, Loosen PT. Thyroid function in psychiatric disorders. In: Wolkowitz OM, Rothschild TJ, editors. Psychoneuroendocrinology: the scientific basis of clinical practice. Washington: American Psychiatric Press; 2003.
- 2.Joffe RT, Sokolov STH. Thyroid hormones, the brain, and affective disorders. Crit Rev Neurobiol 1994;8(1/2):45-63. [PubMed]
- 3.Sauvage MF, Marquet P, Rousseau A, Raby C, Buxeraud J, Lachâtre G. Relationship between psychiatric drugs and thyroid function: a review. Toxicol Appl Pharmacol 1998;149:127-35. [DOI] [PubMed]
- 4.Jackson I. The thyroid axis and depression. Thyroid 1998;8:951-6. [DOI] [PubMed]
- 5.Baumgartner A. Thyroxine and the treatment of affective disorders: an overview of the results of basic and clinical research. Int J Neuropsychopharmacol 2000;3:149-65. [DOI] [PubMed]
- 6.Gold MS, Pottash AC, Mueller EAN, Extein I. Grades of thyroid failure in 100 depressed and anergic inpatients. Am J Psychiatry 1981;138:253-5. [DOI] [PubMed]
- 7.Joffe RT, Levitt AJ. Major depression and subclinical (Grade 2) hypothyroidism. Psychoneuroendocrinology 1992;17:215-21. [DOI] [PubMed]
- 8.Baumgartner A, Gräf KJ, Kürten I, Meinhold H. The hypothalamic-pituitary-thyroid axis in psychiatric patients and healthy subjects: parts 1-4. Psychiatry Res 1988;24:271-332. [DOI] [PubMed]
- 9.Joffe RT, Singer W. The effects of tricyclic antidepressants on basal thyroid hormone levels in depressed patients. Pharmacopsychiatry 1990;23:67-9. [DOI] [PubMed]
- 10.Suri RA, Altshuler LA, Rasgon NL, Calcago JL, Frye MA, Gitlin MJ, et al. Efficacy and response time to sertraline vs. fluoxetine in the treatment of unipolar major depressive disorder. J Clin Psychiatry 2000;61:942-6. [DOI] [PubMed]
- 11.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington: The Association; 1994.
- 12.Hamilton M. Development of a rating scale for primary depressive illness. Br J Soc Clin Psychol 1967;6:278-96. [DOI] [PubMed]
- 13.Guy W, editor. ECDEU assessment manual for psychopharmacology. Washington: US Department of Health, Education and Welfare; 1976. p. 218-22. Publication ADM 76-338.
- 14.Cole DP, Thase ME, Mallinger AG, Soares JC, Luther JF, Kupfer DJ, et al. Slower treatment response in bipolar depression predicted by lower pretreatment thyroid function. Am J Psychiatry 2002;159:116-21. [DOI] [PubMed]
- 15.Sane NS, Frye MA, Kiriakos LR, Cossolino A, Altshuler LL, Mehra V, et al. Serum-free T4 and shorter hospital length of stay in depressed male patients [presentation]. American Psychiatric Association annual meeting; 2001 May 5–10; New Orleans (LA).
- 16.Shelton C, Winn S, Ekhatore N, Loosen P. The effects of antidepressants on the thyroid axis in depression. Biol Psychiatry 1993;33(2):120-6. [DOI] [PubMed]
- 17.König F, Hauger B, von Hippel C, Wolfersdorf M, Kaschka WP. Effect of paroxetine on thyroid hormone levels in severely depressed patients. Pharmacopsychiatry 2000;42:135-8. [DOI] [PubMed]


