Short abstract
Obesity seems to be perpetuated by a series of vicious cycles, which, in combination with increasingly obesogenic environments, accelerate weight gain and represent a major challenge for weight management
The chronic positive energy balance that leads to obesity is apparently relatively small.1 It is therefore paradoxical that obesity is so persistent and difficult to treat, because, in Western countries at least, the basic causes of obesity are readily apparent to everyone (eating too much and exercising too little). Obesity is associated with a substantial loss of quality of life and with social stigmatisation; awareness of the health consequences of obesity has never been greater. Even the body's physiological systems try to prevent weight gain by minimising the impact of energy imbalance on weight change.2
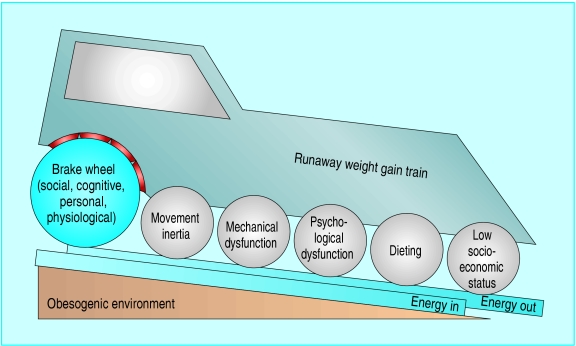
To help explain this apparent paradox, we propose that numerous vicious cycles are acting as “accelerators” that maintain and even increase overweight. We liken the situation to a “runaway weight gain train” (figure), which already has high momentum from the downhill slope of obesogenic (obesity promoting) environments but is getting faster as the vicious cycles start acting as accelerators. The brakes, which, on the face of it, should be strong enough to slow down the train, turn out to be weak by comparison.
Figure 1.
The runaway weight gain train
The downhill slope of obesogenic environments
The obesogenic environments of the modern world have been well described.3,4 They make the unhealthy choices the easy, default choices, resulting in a high intake of energy dense foods and beverages and in reduced physical activity. Examples include the heavy promotion of fast food outlets, energy dense snacks, and high sugar drinks to children; the low cost and large serving sizes of such foods; and the transport systems and urban design that inhibit active transport and active recreation.
In our runaway train model (figure), the twin tracks of “energy in” and “energy out” are on the downhill slope of the obesogenic environments, indicating that the default direction is downhill towards positive energy balance. Levelling out the obesogenic slope is fundamental to slowing down the momentum of the obesity epidemic. However, in some areas, such as “retro fitting” walking, cycling and public transport into a car oriented built environment, this will require a massive engineering effort and is likely to take a very long time.5
Ineffective brakes
Several “brakes” are acting against increasing weight gain. Possibly the strongest in Western societies is the social discrimination of being overweight or obese.6 Unlike other conditions related to a combination of inappropriate diet, lack of exercise, and genetic background—for example, hypertension and dyslipidaemia—obesity is visible to others and carries the social stigmata of sloth and gluttony. Interestingly, the rise of support groups for big people, the sanctions against discrimination on the basis of size, and the rise of the average body size into the overweight range may reduce the pressure on this brake.
A further brake is the personal physical discomfort associated with obesity, which reduces quality of life substantially.7 Knowledge about the fundamental causes of weight gain (eating too much and exercising too little) is common, but this cognitive brake is often ineffectual. Some authors argue for a greater application of cognitive efforts to control weight gain,5 but knowledge alone seems to be a weak predictor of human behaviour, and educational strategies, at least at the population level, seem to have little effect on preventing weight gain.8
Even physiology attempts to slow weight gain. The metabolic profile of an obese person is one of physiological brakes being fully applied to prevent further weight gain. These include reductions in appetite, increased fat oxidation, increased energy expenditure, insulin resistance, increased activity of the sympathetic nervous system, increased leptin concentrations, and so on.2,9,10 In response to weight loss, these physiological mechanisms are reversed (and more vigorous—for obvious survival reasons),9,10 so their role seems to be to dampen the impact of energy imbalances on subsequent weight change.
While all these brakes seem to be substantive, they are clearly not strong enough to halt the increasing momentum of the weight gain train. This argues for the existence of a powerful set of accelerating forces in addition to the downhill obesogenic slope.
Vicious cycles as accelerators
A vicious cycle is a positive feedback loop in which the problem (in this case, weight gain) becomes self perpetuating. In almost all physiological systems, cycles are based on negative feedback relations, so the interaction of multiple systems ensures a dynamic stability. Positive feedback cycles, on the other hand, are destabilising and potentially accelerating, because an initial increase in one factor leads to changes in the system that feed back and further exaggerate the initial increase. Several vicious cycles, outlined in the table and explained below, seem to be operating in obesity, creating a potent driving force for perpetuation and even acceleration.
Table 1.
Vicious cycles that potentially contribute as accelerators of weight gain
|
Vicious cycle connections
|
|||
|---|---|---|---|
| Cycles | Obesity may lead to | Which may promote further weight gain by | Potential “cycle breakers” |
| Movement intertia | |||
| Increased effort of physical activity | Reducing levels of physical activity in:
|
Using motivational techniques
|
|
| Incidental activity
|
Setting small, achievable goals
|
||
| Active transport
|
Emphasis on nutrition goals
|
||
| Active recreation | Using weight supportive activities | ||
| Mechanical dysfunction | |||
| A variety of mechanical problems such as arthritis or arthralgia, sleep apnoea, respiratory dysfunction, incontinence | Reducing physical activity because of:
|
Specific treatment for the conditions (analgesics, continuous positive airways pressure, surgery)
|
|
| Pain, restricted movements
|
|
||
| Lethargy, daytime somnolence
|
|
||
| Shortness of breath
|
Motivational techniques
|
||
| Stress or exercise incontinence | More tailored prescription for physical activity | ||
| Psychological dysfunction | |||
| Increased psychological problems such as depression, anxiety, and feelings of low self esteem and guilt | Binge eating, comfort eating
|
Psychological and behavioural therapy as a central management strategy
|
|
| Excess alcohol intake
|
Careful management of medications
|
||
| Lethargy, sense of helplessness, reduced motivation
|
|
||
| Medications that exacerbate weight gain | |||
| Dieting | |||
| Starting a restrictive, rule-bound weight loss diet which perpetuates concepts of “forbidden” foods or “free” foods and is unsustainable | Vigorous metabolic response against rapid weight loss | Tighter regulations against claims and testimonials in weight loss diets and remedies | |
|
|
Added sense of personal failure and diet failure (`nothing works for me') when diet becomes unsustainable
|
Education about crash diets
|
|
| Reduced expectations of likely sustainable weight losses | |||
| Low socioeconomic status | |||
| Reduced opportunities for jobs, education, marriage, and social inclusion | Living in poor neighbourhoods which are obesogenic | Healthier environments for poor neighbourhoods | |
| Reduced capacity to pay for some healthy food or active recreation options | Reduced inequity in access to healthier choices | ||
| Higher levels of chronic stress | Reduced discrimination against obese people | ||
| Higher priority on immediate life issues than longer term health outcomes | |||
Movement inertia cycle
A heavy body weight is a disincentive for movement and physical activity, creating “movement inertia.” Although obese people expend more energy in performing a given level of physical activity than lighter people, they tend to do fewer of those energy demanding activities.11 These reductions in levels of physical activity are most apparent in people who are substantially overweight.12 Reducing levels of physical activity obviously then promotes further weight gain. The potential “cycle breakers” (analogous to a clutch in the train model) could be the use of motivational techniques, weight supportive exercise (such as pool based activities), and focusing on reducing energy intake in the first instance.
Mechanical dysfunction cycle
A related vicious cycle is one due to the mechanical problems associated with increased body weight. These include arthritis, arthralgia, low back pain, chest wall and diaphragm restriction, incontinence, obstructive sleep apnoea, oedema, and cellulitis.13-15 These may result in pain and difficulty walking and moving, shortness of breath (often diagnosed as asthma), exercise and stress incontinence, daytime somnolence, fatigue, and so on, which further limit physical activity and increase weight gain. Some specific treatments for the mechanical dysfunction itself to break the cycle may be available, such as continuous positive airways pressure for obstructive sleep apnoea and anti-inflammatory drugs and surgery for orthopaedic problems.
Psychological dysfunction cycle
For some obese individuals, body dissatisfaction, the physical discomfort of obesity, and social stigmatisation may trigger or exacerbate depression, anxiety, and feelings of low self esteem and guilt. Some of the consequences of these psychological problems may increase energy intake (such as binge or comfort eating, excess alcohol intake) or reduce physical activity (such as lethargy and lack of motivation).16 In addition, some medications that might be used to manage the psychological condition may promote weight gain (for example, psychotropic drugs). Appropriate management of the psychological condition and the medication may be needed to help break the effects of this vicious cycle.
Dieting cycle
New diets (and recycled old diets) are constantly coming in and going out of fashion. They often have specific “magic” weight loss ingredients or a set of restrictive rules with “free” and “forbidden'” foods. Some of the diets are very hypocaloric and result in marked weight loss, and most are unsustainable. The metabolic response to a large weight loss is vigorous, and the subsequent weight that is regained is disproportionately higher in fat.17 In addition, the sense of failure (personal failure and “diet” failure) may contribute to the depression and psychological problems described in the previous cycle. For some people with so called food cravings or addictions, self deprivation of particular favourite foods, such as chocolate, may lead to a heightened desire for those foods18 and contribute to the failure of the diet.
Low socioeconomic status cycle
In developed countries, socioeconomic status is strongly associated with obesity, especially among women, with a higher prevalence of obesity in groups with a lower socioeconomic status.3 This relation seems to be bidirectional. Obesity leads to reduced opportunities for jobs, education, marriage, and social inclusion,19 and these may be more potent in women than in men. A lower income reduces the range of healthy choices, such as fresh fruit and vegetables, and expensive active recreational pursuits. Neighbourhoods with a low socioeconomic status are usually more obesogenic than neighbourhoods with a high status.20 A low income is also associated with higher levels of chronic stress, which may lead to comfort eating, excessive consumption of alcohol, and even the chronic activation of the hypothalamic-pituitary-adrenal axis,21 resulting ultimately in increased obesity and hence perpetuating the cycle. Improving equity of access to healthy choices and reducing the obesogenicity of poor neighbourhoods are important strategies to break this cycle.
Conclusion
The combination of the described vicious cycles acting as accelerator wheels, a set of ineffective brakes, and increasingly obesogenic environments represents a major challenge for weight management. We have identified several vicious cycles that may be operating in obesity and acknowledge that there may even be more. Defining these potential vicious cycles is vital for several reasons. Firstly, they help explain the apparent paradox of continuing (and often increasing) obesity in the face of brakes such as strong social stigmatisation and knowledge of causes and solutions. Secondly, they may contribute to the increasing right skewness of the frequency distribution of body mass index as the population gains weight over time. In other words, the lean people gain a little weight but the already overweight and obese gain a lot of weight, creating an exaggerated interaction between individual and environment. Thirdly, they underline the variety and strength of the factors that people with established obesity have to struggle against in their attempts to lose weight. Fourthly, they point to opportunities for specific measures that can be taken at an individual or societal level that might help to diminish the driving forces that are promoting weight gain. Fifthly, they point to the need for more research into the nature of these vicious cycles and the effectiveness of strategies to break them. Lastly, all this makes it imperative to focus on prevention, especially in children. This is one train ride they won't want to take.
Summary points
Obesity seems to be perpetuated by a series of vicious cycles
Obesity may result in movement inertia, mechanical dysfunction, psychological dysfunction, cyclical dieting, and socioeconomic disadvantage, all of which may promote further weight gain
The “obesogenic” environment is also driving the obesity epidemic, whereas the “brakes” against weight gain (social, personal, cognitive, physiological) are weak by comparison
Management of obesity should include the identification of active vicious cycles and implementation of strategies to break the cycle
The authors each have more than 15 years' experience in research and action on obesity at metabolic, clinical, and population levels. BS's obesity research includes metabolic studies at the National Institutes of Health, Phoenix, Arizona; clinical and public health interventions at the University of Auckland; and whole of community obesity prevention at Deakin University. He is a member of the Prevention Group of the International Obesity TaskForce. GE was the founder of GutBusters, a waist loss programme for men which treated thousands of overweight Australian men between 1991 and 2002. He was the lead author of the Australian Physical Activity Guidelines and the National Health and Medical Council's National Clinical Guidelines for Weight Control and Obesity Management.
Contributors: Both authors contributed to defining the concepts included in the paper and both were involved in writing and editing. BS is guarantor.
Competing interests: None declared.
References
- 1.Hill JO, Wyatt HR, Reed GW, Peters JC. Obesity and the environment: where do we go from here? Science 2003;299: 853-5. [DOI] [PubMed] [Google Scholar]
- 2.Ravussin E, Swinburn BA. Metabolic predictors of obesity: cross-sectional versus longitudinal data. Int J Obes Relat Metab Disord 1993;17(suppl 3): S28-31; discussion S41-2. [PubMed] [Google Scholar]
- 3.Swinburn B, Egger G. Preventive strategies against weight gain and obesity. Obes Rev 2002;3: 289-301. [DOI] [PubMed] [Google Scholar]
- 4.French SA, Story M, Jeffery RW. Environmental influences on eating and physical activity. Annu Rev Public Health 2001;22: 309-35. [DOI] [PubMed] [Google Scholar]
- 5.Peters JC, Wyatt HR, Donahoo WT, Hill JO. From instinct to intellect: the challenge of maintaining healthy weight in the modern world. Obes Rev 2002;3: 69-74. [DOI] [PubMed] [Google Scholar]
- 6.Puhl R, Brownell KD. Bias, Discrimination, and obesity. Obes Res 2001;9: 788-805. [DOI] [PubMed] [Google Scholar]
- 7.Han TS, Tijhuis MA, Lean ME, Seidell JC. Quality of life in relation to overweight and body fat distribution. Am J Public Health 1998;88: 1814-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jeffery RW, French SA. Preventing weight gain in adults: the pound of prevention study. Am J Public Health 1999;89: 747-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Leibel RL, Rosenbaum M, Hirsch J. Changes in energy expenditure resulting from altered body weight. N Engl J Med 1995;332: 621-8. [DOI] [PubMed] [Google Scholar]
- 10.Blundell JE, Gillett A. Control of food intake in the obese. Obes Res 2001;9(suppl 4): 263S-270S. [DOI] [PubMed] [Google Scholar]
- 11.Ferraro R, Boyce VL, Swinburn B, De Gregorio M, Ravussin E. Energy cost of physical activity on a metabolic ward in relationship to obesity. Am J Clin Nutr 1991;53: 1368-71. [DOI] [PubMed] [Google Scholar]
- 12.Prentice AM, Black AE, Coward WA, Cole TJ. Energy expenditure in overweight and obese adults in affluent societies: an analysis of 319 doubly-labelled water measurements. Eur J Clin Nutr 1996;50: 93-7. [PubMed] [Google Scholar]
- 13.World Health Organization. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. Geneva: World Health Organization, 2000. (WHO Technical Report Series 894.) [PubMed]
- 14.Visscher TL, Seidell JC. The public health impact of obesity. Annu Rev Public Health 2001;22: 355-75. [DOI] [PubMed] [Google Scholar]
- 15.Mommsen S, Foldspang A. Body mass index and adult female urinary incontinence. World J Urol 1994;12: 319-22. [DOI] [PubMed] [Google Scholar]
- 16.Wardle J. Aetiology of obesity VII: psychological factors. In: Force BNFT, ed. Obesity. Oxford: Blackwell Science, 1999: 83-91.
- 17.Dulloo AG, Jacquet J, Girardier L. Poststarvation hyperphagia and body fat overshooting in humans: a role for feedback signals from lean and fat tissues. Am J Clin Nutr 1997;65: 717-23. [DOI] [PubMed] [Google Scholar]
- 18.Rogers P, Smit H. Food craving and food `addiction': A critical review of the evidence from a biopsychosocial perspective. Pharmacol Biochem Behav 2000;66(1): 3-14. [DOI] [PubMed] [Google Scholar]
- 19.Stunkard AJ. Socioeconomic status and obesity. In: Cadwick DJ, Cardew G, eds. The origins and consequences of obesity. Chichester: Wiley, 1996: 174-93.
- 20.Reidpath D, Burns C, Garrard J, Mahoney M, Townsend M. An ecological study of the relationship between social and environmental determinants of obesity. Health Place 2002;8: 141-5. [DOI] [PubMed] [Google Scholar]
- 21.Bjorntorp P, Rosmond R. Neuroendocrine abnormalities in visceral obesity. Int J Obes Relat Metab Disord 2000;24(suppl 2): S80-5. [DOI] [PubMed] [Google Scholar]