Abstract
Introduction
The HEART Pathway is a diagnostic protocol designed to identify low-risk patients presenting to the Emergency Department (ED) with chest pain that are safe for early discharge. This protocol has been shown to significantly decrease healthcare resource utilization compared to usual care. However, the impact of the HEART Pathway on the cost of care has yet to be reported.
Methods and Results
We performed a cost analysis of patients enrolled in the HEART Pathway trial, which randomized participants to either usual care or the HEART Pathway protocol. For low-risk patients, the HEART Pathway recommended early discharge from the ED without further testing. We compared index visit cost, cost at 30 days, and cardiac-related healthcare cost at 30 days between the two treatment arms. Costs for each patient included facility and professional costs. Cost at 30 days included total inpatient and outpatient costs, including the index encounter, regardless of etiology. Cardiac-related healthcare cost at 30 days included the index encounter and costs adjudicated to be cardiac-related within that period.
270 of the 282 patients enrolled in the trial had cost data available for analysis. There was a significant reduction in cost for the HEART Pathway group at 30 days (median cost savings of $216 per individual), which was most evident in low-risk (TIMI score of 0–1) patients (median savings of $253 per patient) and driven primarily by lower cardiac diagnostic costs in the HEART Pathway group.
Conclusions
Utilizing the HEART Pathway as a decision aid for patients with undifferentiated chest pain resulted in significant cost savings.
Clinical Trial Registration
clinicaltrials.gov (clinical trial number, NCT01665521)
Keywords: cost-benefit analysis, coronary disease, diagnosis
Chest pain is one of the most common symptoms evaluated in the Emergency Department (ED). One of the primary diagnostic concerns during this evaluation is whether there is evidence of an acute coronary syndrome (ACS) as this diagnosis is a major cause of short- and long-term morbidity and mortality. The cost of chest pain evaluations has been estimated at $10 billion annually, yet only 10% of these patients are ultimately diagnosed with ACS or other acute diagnoses requiring urgent hospitalization, resulting in very inefficient healthcare resource utilization.1, 2
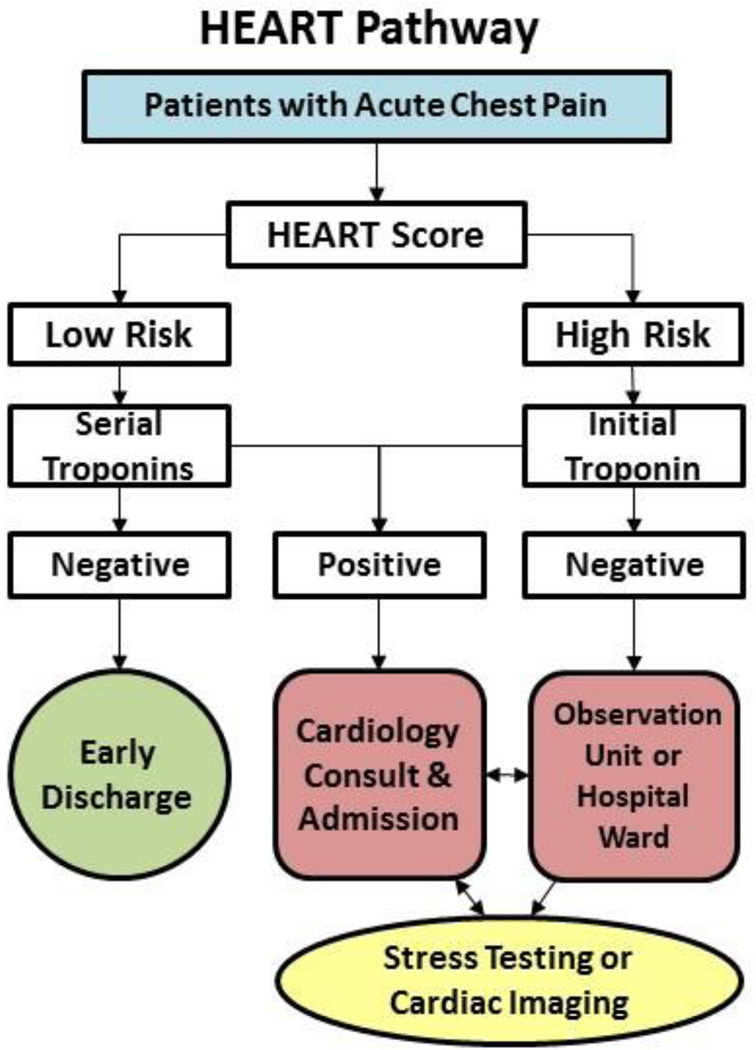
In an effort to improve the efficiency of evaluating this patient group, our group recently validated a risk stratification tool called the HEART Pathway, which utilizes the HEART score (History, ECG, Age, Risk factors, and initial Troponin) combined with a serial troponins at 0 and 3 hours after ED presentation.3 In a randomized trial, the HEART Pathway was shown to reliably categorize ED patients who presented with acute, undifferentiated chest pain as high-risk (≥1%) or low-risk (<1%) for major adverse cardiovascular events (MACE) at 30 days. Compared with usual care, use of the HEART Pathway significantly decreased objective cardiac testing at 30 days by 12.1% (68.8% versus 56.7%; p=0.04) and length of stay by 12 hours (9.9 versus 21.9 hours; p=0.01) and increased early discharges by 21.3% (39.7% versus 18.4%; p<0.01). None of the patients identified for early discharge had major adverse cardiac events within 30 days.3 However, the impact of the HEART Pathway on cost, compared to usual care, has yet to be reported. Based on our prior studies, we hypothesized that there will be cost savings in the HEART Pathway arm compared to the usual care arm of the HEART Pathway study, particularly among low-risk patients.
Methods
This study was a pre-planned secondary analysis of patients enrolled in the HEART Pathway trial, a randomized controlled single-center clinical trial funded by the American Heart Association (AHA). The trial enrolled patients with symptoms suggestive of ACS from the ED (of institution name withheld for review) from 09/2012 through 02/2014. All 282 enrolled participants provided witnessed written informed consent and were randomized to either usual care or the HEART Pathway (1:1 randomization). Eligibility criteria included the provider ordering an ECG and troponin with the primary purpose of evaluating potential ACS in patients ≥21 years old. Patients were determined ineligible for the following reasons: new ST-segment elevation ≥1 mm (STEMI), hypotension, life expectancy <1 year, the presence of a non-cardiac medical, surgical, or psychiatric illness determined by the provider to require admission, previous enrollment, non-English speaking, and incapacity or unwillingness to consent.
In the usual care arm, care delivery was at the discretion of the provider and not determined by trial protocol; providers were encouraged to follow standards of care per the ACCF/AHA guidelines.4, 5 For those participants randomized to the HEART Pathway arm, they were risk stratified by attending ED providers using the HEART score and serial troponin measures at 0 and 3 hours after ED presentation. The HEART score consists of 5 components: (History, ECG, Age, Risk factors, and initial Troponin). To calculate a HEART score, first each component is assessed (on a scale of 0–2), and then component scores are summed to produce the final score (Table 1). A HEART score of 0–3 is consistent with a low-risk assessment for MACE within 30 days, whereas a score of ≥4 is consistent with a high-risk assessment.6–9 On the basis of the HEART score and serial troponin results, the attending physicians received care recommendations according to the HEART pathway (Figure 1). For patients with low-risk HEART scores (HEART score of 0–3) and negative troponin results, the HEART pathway recommended discharge from the ED without further testing (biomarkers, stress testing, coronary angiography, etc); these patients were encouraged to follow up with their primary care provider. In patients with a high-risk HEART score (HEART score of ≥4) or any troponin measure above the 99th percentile threshold (regardless of HEART score), the HEART Pathway recommended further evaluation in the hospital or observation unit per ACCF/AHA guidelines.4, 5 Follow-up was performed at 30 days for all patients via chart review and telephone interviews. The institutional review committee at (Institution name withheld for review) approved this study and subjects gave informed consent to participate in this study prior to recruitment. Further details regarding the trial have been previously published.3
Table 1.
The HEART Score
| Component | Description | Point Value |
|---|---|---|
| History | Highly Suspicious | 2 |
| Moderately Suspicious | 1 | |
| Slightly Suspicious | 0 | |
| ECG | Significant ST-depression | 2 |
| Non-specific | 1 | |
| Abnormalities | ||
| Normal | 0 | |
| Age | ≥ 65 | 2 |
| 45–64 | 1 | |
| < 45 | 0 | |
| Risk Factors | ≥3 Risk Factors | 2 |
| 1–2 Risk Factors | 1 | |
| No Risk Factors | 0 | |
| Troponin | > 3X Normal Limit | 2 |
| 1–3X Normal Limit | 1 | |
| < Normal Limit | 0 | |
| Total | ||
Figure 1.
For this study, we performed a cost analyses of patients enrolled in the HEART Pathway trial, including pre-specified comparisons between the usual care and HEART Pathway arms, high- and low-risk patients as determined by the HEART Score in the HEART Pathway arm, and of high- and low-risk patients by TIMI (“Thrombolysis In Myocardial Infarction”) criteria between the usual care and HEART Pathway arms. We compared index visit cost, cost at 30 days (including the index visit cost), and cardiac-related healthcare cost at 30 days (including index visit cost) between the two treatment arms. Index cost for each patient was based on total facility and professional costs for the index encounter. Cost at 30 days included all inpatient and outpatient facility and professional costs for 30 days after the index encounter, including the index encounter cost, and included all costs (cardiac and non-cardiac-related) during that period. Cardiac-related healthcare cost at 30 days included the index cost plus any cardiac-related office visits, admissions, or cardiac testing within the follow-up period. Costs were deemed cardiac-related if they pertained to cardiac-related office, ED, or hospital visits and/or included objective cardiac testing based on blinded review and adjudication by Drs. Mahler and Hiestand.
We then broke the 30-day total costs down into individual components based on the specific aims of the parent trial, including: cardiac and non-cardiac diagnostic testing cost, emergency department cost, inpatient cost for the index visit (excluding emergency department cost), and outpatient cost. Cardiac diagnostics included stress testing modalities, echocardiography, CT angiography, or invasive coronary angiography.
Cost was measured directly, calculated as the sum of hospital and provider cost and measured from the health system perspective, including cost associated with care at the enrolling hospital system and those outside the enrolling system, if applicable. For hospital or clinic cost, itemized patient charges were converted to cost, with 2012 departmental-specific cost:charge ratios used to file cost reports with the Centers for Medicare & Medicaid Services annually. Provider cost was determined by using current procedural terminology codes from each charged service, converting to physician work relative value units with the Centers for Medicare & Medicaid Services physician fee schedule and subsequently converting to dollars with the Medicare conversion factor. For all payers, itemized hospital charges from each participant were converted to cost. This method has been previously reported by our group.10
All discrete variables were compared using chi-square rank-based group means score statistics and all continuous variables were compared using Spearman’s rank correlations for the comparison of the two treatment arms’ baseline characteristics. Cost data differences were evaluated using Mann-U-Whitney tests. Medians, 25th and 75th percentiles, means, and 95% confidence intervals were calculated for the observed cost data. We reported median (IQR) and mean (SD) differences in cost rounded to the nearest dollar, though focus on the median values for the Results section given the skewed, non-parametric distribution of the data, as shown by the interquartile ranges and means. Statistical analysis was performed using SAS 9.4 (Cary, NC).
Results
Cost data was available for 270 of the 282 enrolled patients in the trial; the first 12 patients were enrolled before the most recent electronic medical record at the enrolling institution had been implemented and had unreliable cost data for analysis. 30-day follow-up data was available for 100% (270/270) of this group. Baseline characteristics for patients included in this study for both treatment arms are shown in Table 2. Costs for the index visit and at 30-day follow-up for the two treatment arms are shown in Table 3. The HEART Pathway arm had a statistically significant lower cost (median cost of $1,307) per individual compared to the usual care arm (median cost of $1,523). Table 4 shows the cost difference between the high and low-risk HEART Pathway patients in the HEART Pathway arm, illustrating the significantly increased cost for high-risk (median cost of $2,349) compared to low-risk patients (median cost of $746). We also evaluated the cost between low-risk (TIMI 0/1) patients in both arms in Table 5. This table illustrates that use of the HEART Pathway leads to a significant reduction in total cost at 30 days compared to usual care in the low-risk group (median cost of $974 and $1,227, respectively).
Table 2.
Study Patient Baseline Characteristics
| Patient Characteristics | HEART Pathway Arm n= 134 |
Usual Care Arm n= 136 |
p value | ||
|---|---|---|---|---|---|
| Number | Percent | Number | Percent | ||
| Age (mean years old, +/−SD) | 53.4 +/− 12.1 | 53.0 +/− 12.2 | 0.77 | ||
| Gender | >0.99 | ||||
| Male | 57 | 42.7 | 57 | 41.9 | |
| Female | 77 | 57.5 | 79 | 58.1 | |
| Race | 0.92 | ||||
| Caucasian | 85 | 63.4 | 90 | 66.2 | |
| African American | 46 | 34.3 | 44 | 32.4 | |
| Asian | 1 | 0.8 | 0 | 0 | |
| Native American | 1 | 0.8 | 1 | 0.7 | |
| Other | 1 | 0.8 | 1 | 0.7 | |
| Ethnicity | 0.37 | ||||
| Hispanic | 1 | 0.8 | 4 | 2.9 | |
| Non-Hispanic | 133 | 99.2 | 132 | 97.1 | |
| CAD Risk Factors | |||||
| Current/Recent Smoking (last year) | 40 | 29.8 | 34 | 25 | 0.41 |
| Recent Cocaine (last 90 days) | 3 | 2.2 | 3 | 2.2 | >0.99 |
| Hypertension | 72 | 53.7 | 77 | 56.6 | 0.71 |
| Dyslipidemia | 59 | 44 | 58 | 42.7 | 0.90 |
| Diabetes | 29 | 21.6 | 25 | 18.4 | 0.54 |
| Family History of Premature Coronary Disease | 42 | 31.6 | 57 | 42.2 | 0.08 |
| BMI >30 mg/m2 | 68 | 50.8 | 76 | 55.9 | 0.46 |
| Known Coronary Disease (>50% stenosis) | 26 | 19.4 | 28 | 20.6 | 0.88 |
| Prior MI | 20 | 14.9 | 23 | 16.9 | 0.74 |
| Prior PCI | 12 | 9 | 18 | 13.2 | 0.33 |
| Prior CABG | 7 | 5.2 | 3 | 2.2 | 0.22 |
| Previous Stroke | 3 | 2.2 | 7 | 5.2 | 0.33 |
| Peripheral Vascular Disease | 4 | 3 | 3 | 2.2 | 0.72 |
| Insurance Status | 0.88 | ||||
| Insured | 102 | 76.1 | 101 | 74.3 | |
| Private | 70 | 52.2 | 65 | 47.8 | |
| Medicare | 19 | 14.2 | 20 | 14.7 | |
| Medicaid | 13 | 9.7 | 16 | 11.8 | |
| Uninsured | 32 | 23.9 | 35 | 25.7 | |
| TIMI | 0.63 | ||||
| Risk | |||||
| 0–1 | 76 | 56.7 | 73 | 53.7 | |
| ≥2 | 58 | 43.3 | 63 | 46.3 | |
| HEART Score (HEART Pathway only) | |||||
| Low Risk | 61 | 45.5 | |||
| High Risk | 73 | 54.5 | |||
Table 3.
Cost Comparison Between Usual Care and the HEART Pathway
| Cost | Usual Care (N= 136) | HEART Pathway (N=134) | p-value |
|---|---|---|---|
| Index visit median cost (Q1, Q3); mean cost (SD) |
$1,412 ($993, $2,493), $,3194 ($6,064) |
$1,260 ($692, $2,348); $2,512 ($3,803) |
0.05 |
| 30-day median cost (Q1, Q3); mean cost (SD) |
$1,523 ($1,065, $2,693); $3323 ($6,064) |
$1,307 ($729, $2,457); $2,605 ($3,860) |
0.04 |
| 30-day median cardiac-related cost (Q1, Q3); mean cost (SD) |
$1,550 ($1,012, $2,780); $3,309 ($6,083) |
$1,375 ($727, $2,383); $2,764 ($4,166) |
0.10 |
Table 4.
Cost Comparison Between High and Low-risk Patients in the HEART Pathway Arm
| Cost | High-risk (N= 73) | Low-risk (N=61) | p-value |
|---|---|---|---|
| Index visit median cost (Q1, Q3); mean cost (SD) |
$2,129 ($1,397, $3,160); $3,862 ($4,739) |
$720 ($579, $1,119); $896 ($492) |
<0.01 |
| 30-day median cost (Q1, Q3); mean cost (SD) |
$2,349 ($1,400, $3,327); $4,000 ($4,794) |
$746 ($599, $1,148); $935 ($500) |
<0.01 |
| 30-day median cardiac-related cost (Q1, Q3); mean cost (SD) |
$2,263 ($1,444, $3,637); $4,252 ($5,185) |
$785 ($589, $1,268); $983 ($544) |
<0.01 |
Table 5.
Cost Comparison Between Low-risk Patients (TIMI 0–1) in the HEART Pathway Versus the Usual Care Arms
| Cost | Usual Care (N=73) | HEART Pathway (N=76) | p-value |
|---|---|---|---|
| Index visit median cost (Q1, Q3); mean cost (SD) |
$1,192 ($872, $1,552); $1,544 ($376) |
$966 ($610, $1,498); $1,334 ($1,242) |
0.04 |
| 30-day median cost (Q1, Q3); mean cost (SD) | $1,227 ($979, $1,604); $1,673 ($1,626) |
$974 ($619, $1,498); $1,402 ($1,282) |
0.02 |
| 30-day median cardiac-related cost (Q1, Q3); mean cost (SD) |
$1,258 ($877, $1,723); $1,631 ($1,524) |
$1,054 ($617, $1,621); $1,576 ($1,895) |
<0.01 |
On analysis of the breakdown of the 30-day total costs between the two treatment arms, there was no significant difference in the individual components of the total cost between the groups (Table 6). A similar comparison was made for the low-risk (TIMI 0/1) groups in both arms at 30-days, as shown in Table 7, which showed that there was a significant difference in cardiac diagnostics cost of $118 (p= 0.04) between these two groups.
Table 6.
Total Cost Breakdown Comparison Between Usual Care and the HEART Pathway Arms
| Cost Metric | Trial Arm | Median Cost (IQR); Mean Cost (SD) | p-value |
|---|---|---|---|
| Cardiac Diagnostics Cost | HEART Pathway Usual Care |
$301 ($80, $593); $782 ($1,855) $333 ($169, $543); $740 ($1,612) |
0.30 |
| Emergency Department Cost |
HEART Pathway Usual Care |
$380 ($288, $453); $425 ($199) $380 ($298, $453); $442 ($234) |
0.72 |
| Inpatient Cost (excluding Emergency Department cost) |
HEART Pathway Usual Care |
$0 ($0, $710); $741 ($2,067) $0 ($0, $834); $978 ($2,972) |
0.52 |
| Non-cardiac Diagnostics Cost |
HEART Pathway Usual Care |
$16 ($16, $51); $112 ($236) $18 ($16, $137); $255 ($728) |
0.38 |
| Outpatient Costs | HEART Pathway Usual Care |
$0 ($0, $82); $48 ($98) $0 ($0, $79); $39 ($73) |
0.66 |
Table 7.
Total Cost Breakdown Between Low-risk Patients (TIMI 0–1) in the HEART Pathway Versus the Usual Care Arms
| Cost Metric | Trial Arm | Median Cost (IQR); Mean Cost (SD) | p-value |
|---|---|---|---|
| Cardiac Diagnostics Cost | HEART Pathway Usual Care |
$208 ($16, $453); $328 ($501) $326 ($159, $532); $405 ($456) |
0.04 |
| Emergency Department Cost |
HEART Pathway Usual Care |
$380 ($283, $422); $414 ($205) $380 ($323, $453); $452 ($248) |
0.24 |
| Inpatient Cost (excluding Emergency Department cost) |
HEART Pathway Usual Care |
$0 ($0, $0); $466 ($2,000) $0 ($0, $0); $530 ($2,337) |
0.59 |
| Non-cardiac Diagnostics Cost |
HEART Pathway Usual Care |
$16 ($14, $40); $125 ($278) $16 ($16, $115); $160 ($360) |
0.35 |
| Outpatient Costs | HEART Pathway Usual Care |
$0 ($0, $82); $36 ($62) $0 ($0, 0); $32 ($64) |
0.41 |
Discussion
The HEART Pathway is a decision aid tool used to classify patients presenting with undifferentiated chest pain into high and low-risk for MACE during the index visit and at 30-day follow-up. Randomized data have shown that use of the HEART Pathway to risk stratify this group significantly decreases objective cardiac testing, increases rates of early discharge, and decreases median length of stay without increasing the risk for adverse events or recurrent evaluations for chest pain.3 This study adds to the previous literature by showing that use of the HEART Pathway not only increases the efficiency of healthcare utilization for the evaluation of this patient group but does so at a significant cost savings compared to usual care, most notable in the low-risk group and driven primarily by lower cardiac diagnostic costs in the HEART Pathway group.
The management of patients with chest pain is a common and challenging clinical problem, requiring the clinician to distinguish between those who require urgent management of more serious diagnoses such as ACS and those with more benign entities who do not require admission. Although clinical judgment continues to be paramount in meeting this challenge, new diagnostic modalities have been developed to assist in risk stratification. These include biomarkers of cardiac injury, risk scores, early stress testing, and noninvasive imaging of the heart. Multiple imaging strategies have been investigated to accelerate diagnosis and to provide further risk stratification of patients presenting withy chest pain and no initial evidence of ACS, including myocardial perfusion imaging, computed tomographic coronary angiography, and cardiac magnetic resonance imaging.11 Miller, et al demonstrated that use of cardiac imaging (CMR) decreased the cost of evaluating high-risk patients presenting with undifferentiated chest pain compared to standard care practices.10 However, when this same protocol was applied to lower-risk patients, the most cost effective strategy appeared to be provider-directed testing compared to a mandated specific imaging strategy protocol, which speaks to the paramount importance of the initial clinical evaluation in this group prior to stress testing or more invasive evaluations.12
Despite the increasing use of noninvasive testing in this patient group, the basic clinical tools of history, physical examination, electrocardiography and biomarker testing (i.e. troponin) are currently widely acknowledged to allow early identification of low-risk patients. The ACCF/AHA guidelines currently recommend that patients at low-risk for ACS should undergo routine evaluation utilizing these methods, followed by objective cardiac testing (stress testing or cardiac imaging).13 However, the value of objective cardiac testing in all low-risk patients is questionable, especially as cardiac testing for all patients at low-risk for ACS is not sustainable from a quality or economic standpoint. Risk assessment using decision aids such as the HEART Pathway mitigates the radiation exposure, exposure to contrast and/or vasodilatory/inotropic stress agents, false positive rate, and anxiety associated with stress testing low-risk patients, most of whom will not ultimately benefit from the testing. The combination of the primary analyses and this cost analysis illustrate that the HEART Pathway has proven to reliably predict low MACE rates in low-risk patients presenting with undifferentiated chest pain, obviating the need for stress testing, and resulting in improved economic efficiency. In our study, these savings were on average $216 per patient, which on an individual scale, may seem somewhat diminutive. However, when this savings is evaluated on a larger scale from a health systems perspective, this could result in over $2 billion in savings for the 8–10 million patients evaluated in the US for undifferentiated chest pain on an annual basis. Depending on a hospital or health system’s patient population distribution of CAD risk factors, this could result in even higher savings for those caring for lower-risk profile groups.
Our study has several limitations. There was missing data on the first 12 patients due to implementation of a new electronic medical record system. While there is no reason to believe this would skew the results in a meaningful way based on the results of the randomization seen in Table 2, there is still the possibility for bias as they were recruited during the initial recruitment stages of the study, which could have had variable adherence to the guidelines in the study protocol. The study is also a single-center study, so the results may not yet be generalizable to other regions.
In conclusion, the HEART Pathway is a decision tool that has been shown to reliably risk stratify patients presenting with undifferentiated chest pain into high and low-risk for MACE at 30 days. This risk stratification has been shown to decrease healthcare utilization in the low-risk population without untoward clinical events. This study illustrates that it decreases the cost of healthcare delivery to this group as well, especially in the low-risk group.
Acknowledgments
Funding Source: This study was funded by the American Heart Association (AHA) Clinical Research Program. The AHA had no role in the design, analysis, interpretation, or writing of this report. The corresponding author had complete access to all study data and final responsibility for article submission. Use of Research Electronic Data Capture was supported by the Wake Forest Translational Science Institute via a grant from National Center for Catalysis Research (M01 RR007122).
Footnotes
None of the Authors have any disclosures to report.
References
- 1.Owens PL, Barrett ML, Gibson TB, Andrews RM, Weinick RM, Mutter RL. Emergency department care in the united states: A profile of national data sources. Ann Emerg Med. 2010;56:150–165. doi: 10.1016/j.annemergmed.2009.11.022. [DOI] [PubMed] [Google Scholar]
- 2.Mahler SA, Hiestand BC, Goff DC, Hoekstra JW, Miller CD. Can the heart score safely reduce stress testing and cardiac imaging in patients at low-risk for major adverse cardiac events? Crit Pathw Cardiol. 2011;10:128–133. doi: 10.1097/HPC.0b013e3182315a85. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mahler SA, Riley RF, Hiestand BC, Russell GB, Hoekstra JW, Lefebvre CW, Nicks BA, Cline DM, Askew KL, Elliott SB, Herrington DM, Burke GL, Miller CD. The heart pathway randomized trial: Identifying emergency department patients with acute chest pain for early discharge. Circ Cardiovasc Qual Outcomes. 2015;8:195–203. doi: 10.1161/CIRCOUTCOMES.114.001384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Wright RS, Anderson JL, Adams CD, Bridges CR, Casey DE, Ettinger SM, Fesmire FM, Ganiats TG, Jneid H, Lincoff AM, Peterson ED, Philippides GJ, Theroux P, Wenger NK, Zidar JP, Jacobs AK. 2011 accf/aha focused update of the guidelines for the management of patients with unstable angina/ non-st-elevation myocardial infarction (updating the 2007 guideline): A report of the american college of cardiology foundation/american heart association task force on practice guidelines. Circulation. 2011;123:2022–2060. doi: 10.1161/CIR.0b013e31820f2f3e. [DOI] [PubMed] [Google Scholar]
- 5.O'Connor RE, Bossaert L, Arntz HR, Brooks SC, Diercks D, Feitosa-Filho G, Nolan JP, Vanden Hoek TL, Walters DL, Wong A, Welsford M, Woolfrey K. Collaborators ACSC. Part 9: Acute coronary syndromes: 2010 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Circulation. 2010;122:S422–S465. doi: 10.1161/CIRCULATIONAHA.110.985549. [DOI] [PubMed] [Google Scholar]
- 6.Backus BE, Six AJ, Kelder JC, Mast TP, van den Akker F, Mast EG, Monnink SH, van Tooren RM, Doevendans PA. Chest pain in the emergency room: A multicenter validation of the heart score. Crit Pathw Cardiol. 2010;9:164–169. doi: 10.1097/HPC.0b013e3181ec36d8. [DOI] [PubMed] [Google Scholar]
- 7.Backus BE, Six AJ, Kelder JC, Bosschaert MA, Mast EG, Mosterd A, Veldkamp RF, Wardeh AJ, Tio R, Braam R, Monnink SH, van Tooren R, Mast TP, van den Akker F, Cramer MJ, Poldervaart JM, Hoes AW, Doevendans PA. A prospective validation of the heart score for chest pain patients at the emergency department. Int J Cardiol. 2013;168:2153–2158. doi: 10.1016/j.ijcard.2013.01.255. [DOI] [PubMed] [Google Scholar]
- 8.Six AJ, Backus BE, Kelder JC. Chest pain in the emergency room: Value of the heart score. Neth Heart J. 2008;16:191–196. doi: 10.1007/BF03086144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Six AJ, Cullen L, Backus BE, Greenslade J, Parsonage W, Aldous S, Doevendans PA, Than M. The heart score for the assessment of patients with chest pain in the emergency department: A multinational validation study. Crit Pathw Cardiol. 2013;12:121–126. doi: 10.1097/HPC.0b013e31828b327e. [DOI] [PubMed] [Google Scholar]
- 10.Miller CD, Hwang W, Hoekstra JW, Case D, Lefebvre C, Blumstein H, Hiestand B, Diercks DB, Hamilton CA, Harper EN, Hundley WG. Stress cardiac magnetic resonance imaging with observation unit care reduces cost for patients with emergent chest pain: A randomized trial. Ann Emerg Med. 2010;56:209.e202–219.e202. doi: 10.1016/j.annemergmed.2010.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kontos MC, Diercks DB, Kirk JD. Emergency department and office-based evaluation of patients with chest pain. Mayo Clin Proc. 2010;85:284–299. doi: 10.4065/mcp.2009.0560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Miller CD, Hoekstra JW, Lefebvre C, Blumstein H, Hamilton CA, Harper EN, Mahler S, Diercks DB, Neiberg R, Hundley WG. Provider-directed imaging stress testing reduces health care expenditures in lower-risk chest pain patients presenting to the emergency department. Circ Cardiovasc Imaging. 2012;5:111–118. doi: 10.1161/CIRCIMAGING.111.965293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Amsterdam EA, Wenger NK, Brindis RG, Casey DE, Ganiats TG, Holmes DR, Jaffe AS, Jneid H, Kelly RF, Kontos MC, Levine GN, Liebson PR, Mukherjee D, Peterson ED, Sabatine MS, Smalling RW, Zieman SJ, Cardiology ACo. Guidelines AHATFoP, Interventions SfCAa, Surgeons SoT, Chemistry AAfC. 2014 aha/acc guideline for the management of patients with non-st-elevation acute coronary syndromes: A report of the american college of cardiology/american heart association task force on practice guidelines. J Am Coll Cardiol. 2014;64:e139–e228. doi: 10.1016/j.jacc.2014.09.017. [DOI] [PubMed] [Google Scholar]