As per the 2014 Census, there were 8.6 million Puerto Ricans in the U.S., including 5.1 million residents of the continental U.S. and 3.5 million residents of the island of Puerto Rico (a U.S. territory). In the U.S., Puerto Ricans report the largest proportion of families below the poverty level (24%)1.
Puerto Ricans are disproportionately affected with asthma. In the U.S., the prevalence of asthma is higher in Puerto Ricans (16.1%) than in NH blacks (11.2%), NH whites (7.7%) or Mexicans (5.4%)2. Moreover, morbidity and mortality from asthma are higher in Puerto Ricans than in other racial or ethnic groups3. Studying Puerto Ricans or other high-risk groups is not only important for public health but may also yield new insights into asthma pathogenesis. A growing body of evidence supports a multi-factorial etiology of asthma in Puerto Ricans, with yet-to-be identified interactions between heredity and environmental risk factors.
Puerto Ricans can be of any race, but most have variable proportions of European, West African and Native American ancestry. Recent work using ancestry-informative genetic markers shows that, on average, Puerto Ricans are 60–70% European, 18–25% African, and 12–15% Native American4,5. Among Hispanic children (including Puerto Ricans), African ancestry is inversely associated with lung function (FEV1 and FVC) but positively associated with asthma, while Native American ancestry is positively associated with lung function but inversely associated with asthma4,5. Whether ancestral effects are explained by allelic variants or environmental factors correlated with racial ancestry is unknown, but extrapolating reference values for lung function from other ethnic groups (e.g., Mexican Americans) to Puerto Ricans can lead to erroneous conclusions. This could be ameliorated if reference values were developed for Puerto Ricans, preferably having ancestry data (from genetic markers) incorporated into equations to calculate such values.
GWAS have identified SNPs that increase susceptibility to asthma across racial/ethnic groups (“cosmopolitan”), including Puerto Ricans. Asthma-susceptibility loci replicated in Puerto Ricans include the chromosome 17q21 locus and IL33, with other loci replicated in Hispanic cohorts that include but are not limited to Puerto Ricans (i.e. TSLP)3,6. Although some susceptibility variants for asthma may exclusively affect Puerto Ricans (“ethnic-specific”), no such variant has been confidently identified. Few studies have examined gene-by-environment interactions or epigenetic mechanisms for asthma in Puerto Ricans3.
Published evidence supports the following environmental or behavioral risk factors for asthma or asthma morbidity (e.g., severe exacerbations) in Puerto Ricans: cigarette smoking and SHS, prematurity, allergens, air pollution, diet, vitamin D insufficiency, obesity, exposure to violence, chronic psychosocial stress, inadequate access to healthcare, low health literacy, and poor adherence to prescribed treatment (i.e. due to concerns about side effects or medication costs)3,7. To date, little is known about viral infections or the host microbiome and asthma in Puerto Ricans.
Chronic stress may be particularly relevant to asthma in Puerto Ricans, who are often exposed to violence and other stressors. Indeed, recent findings implicate parental stress, physical or sexual abuse, and violence in the etiology of childhood asthma in Puerto Ricans8, partly through genetic and epigenetic mechanisms. In a study of Puerto Rican school-aged children, exposure to violence was associated with methylation of the promoter of ADCYAP1R1, which was in turn associated with asthma. Moreover, an ADCYAP1R1 SNP was associated with asthma in Puerto Rican children9.
Chronic stress has also been associated with reduced expression of the gene for the β2-adrenergic receptor (ADRB2, key for BDR) in WBCs of subjects with asthma10. Interestingly, Puerto Ricans have reduced BDR11, raising the possibility that chronic stress lead to asthma morbidity through down-regulation of ADRB2. In support of this hypothesis, we recently showed that high perceived stress is associated with reduced BDR in Puerto Rican and non-Puerto Rican children with or at risk for asthma12. In that study, we also demonstrated that an ADCYAP1R1 SNP is associated with: reduced BDR in children with asthma, reduced ADRB2 expression in unstimulated CD4+ T cells of subjects with asthma, and increased functional connectivity of the amygdala and insula (an anxiety marker). We also provided preliminary evidence for an interaction between the risk SNP and high stress, further suggesting that stress leads to reduced BDR through down-regulation of ADRB2 by persistent secretion of catecholamines, particularly in genetically susceptible individuals12.
FUTURE DIRECTIONS
A birth cohort study has yet to be conducted in Puerto Ricans, despite clear evidence of a key role for early-life exposures in asthma causation. Such study should use an “exposome” approach13 instead of a reductionist strategy (focusing on one risk factor), given the complex etiology of asthma in Puerto Ricans. Moreover, including other racial or ethnic groups within the same birth cohort study would be ideal, as it would provide additional opportunities for discovery of risk or protective factors across populations.
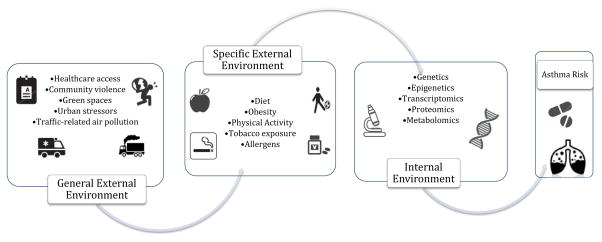
The exposome encompasses the totality of environmental or behavioral exposures from conception onwards, complementing the genome (Figure 1)13. In this context, the external exposome (comprising the individual and community-level external environments) and the internal exposome (host biologic factors) need to be characterized through all life stages, given their dynamic nature. Thus, repeated assessment of objective measures of exposure and biomarkers are needed to capture both the exposome and its cumulative impact on asthma risk. As for the internal exposome, an “omics” approach (integrating genetics, epigenetics, transcriptomics, proteomics and metabolomics) is justifiable and more likely to yield groundbreaking insights than compartmental approaches (i.e. GWAS).
FIGURE 1.
The external exposome (comprising multiple risk factors operating at the individual and community or societal levels) interacts with the internal exposome (host biologic factors) to cause asthma in Puerto Ricans.
Studies using an exposome approach require analytical methods to assess multiple and combined exposures, ranging from evaluating the simultaneous effects of multiple exposures (i.e. using a regression framework and allowing for interactions) to evaluating risk estimates for combined exposures (i.e. using a score “summing” the weighted contributions of individual exposures, or employing data-driven dimension reduction methods) 13.
Under the “exposome” causal framework, multi-factorial interventions are more likely to be effective in preventing or treating asthma in Puerto Ricans than clinical trials of a single intervention. For example, modifying diet, physical activity and SHS could impact not only asthma but also other health conditions (i.e. obesity) during childhood, particularly if a school-based approach is expanded to include caregivers, thus leading to lifestyle changes at both the school and home environments.
In parallel with multifactorial clinical trials, sound public health policy is needed to alleviate the burden of asthma in Puerto Ricans. Such efforts should include campaigns for: smoking prevention and cessation, “clean air”, prevention of violence, and adequate care for mental illnesses linked to asthma morbidity. In this context, clinicians caring for Puerto Ricans with asthma should provide counseling aimed to modify risk factors (i.e. cigarette smoking), treat common co-morbidities (i.e. depression, PTSD, allergic rhinitis, and obesity) and remove barriers to care (i.e. by communicating and educating in a patient-appropriate literacy and language levels, and addressing culturally-specific beliefs about asthma or its treatment).
Abbreviations
- ADCYAP1R1
pituitary adenylate cyclase activating polypeptide 1 type 1 receptor
- ADRB2
β2-adrenergic receptor
- BDR
Bronchodilator response
- GWAS
Genome-wide association studies
- ICS
Inhaled corticosteroids
- NH
Non-Hispanic
- PTSD
Post-traumatic stress disorder
- SES
Socioeconomic status
- SHS
Second-hand smoke
- SNP
Single nucleotide polymorphism
- TSLP
thymic stromal lymphopoietin
- WBCs
white blood cells
Footnotes
Declaration of conflicts of interest
This work was supported by grants HL079966 and HL117191 from the U.S. National Institutes of Health (NIH), and by The Heinz Endowments. Dr. Forno’s contribution was partially funded by NIH grant HL125666. The authors have no conflicts of interest to declare.
References
- 1. [Accessed on June 14, 2016]; http://centropr.hunter.cuny.edu/research/datacenter/puerto-ricans-us-earn-less-money-and-pay-more-housing.
- 2.Akinbami LJ, Moorman JE, Bailey C, et al. Trends in asthma prevalence, health care use, and mortality in the United States, 2001–2010. NCHS Data Brief. 2012:1–8. [PubMed] [Google Scholar]
- 3.Rosser FJ, Forno E, Cooper PJ, Celedon JC. Asthma in Hispanics. An 8-year update. Am J Respir Crit Care Med. 2014;189:1316–27. doi: 10.1164/rccm.201401-0186PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brehm JM, Acosta-Perez E, Klei L, et al. African ancestry and lung function in Puerto Rican children. J Allergy Clin Immunol. 2012;129:1484–90. e6. doi: 10.1016/j.jaci.2012.03.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pino-Yanes M, Thakur N, Gignoux CR, et al. Genetic ancestry influences asthma susceptibility and lung function among Latinos. J Allergy Clin Immunol. 2015;135:228–35. doi: 10.1016/j.jaci.2014.07.053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Galanter JM, Torgerson D, Gignoux CR, et al. Cosmopolitan and ethnic-specific replication of genetic risk factors for asthma in 2 Latino populations. J Allergy Clin Immunol. 2011;128:37–43. e12. doi: 10.1016/j.jaci.2011.03.050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Castro-Rodriguez JA, Forno E, Rodriguez-Martinez CE, Celedon JC. Risk and Protective Factors for Childhood Asthma: What Is the Evidence? J Allergy Clin Immunol Pract. 2016 doi: 10.1016/j.jaip.2016.05.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rosenberg SL, Miller GE, Brehm JM, Celedon JC. Stress and asthma: novel insights on genetic, epigenetic, and immunologic mechanisms. J Allergy Clin Immunol. 2014;134:1009–15. doi: 10.1016/j.jaci.2014.07.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chen W, Boutaoui N, Brehm JM, et al. ADCYAP1R1 and asthma in Puerto Rican children. Am J Respir Crit Care Med. 2013;187:584–8. doi: 10.1164/rccm.201210-1789OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Miller GE, Chen E. Life stress and diminished expression of genes encoding glucocorticoid receptor and beta2-adrenergic receptor in children with asthma. Proc Natl Acad Sci U S A. 2006;103:5496–501. doi: 10.1073/pnas.0506312103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Choudhry S, Ung N, Avila PC, et al. Pharmacogenetic differences in response to albuterol between Puerto Ricans and Mexicans with asthma. Am J Respir Crit Care Med. 2005;171:563–70. doi: 10.1164/rccm.200409-1286OC. [DOI] [PubMed] [Google Scholar]
- 12.Brehm JM, Ramratnam SK, Tse SM, et al. Stress and Bronchodilator Response in Children with Asthma. Am J Respir Crit Care Med. 2015;192(1):47–56. doi: 10.1164/rccm.201501-0037OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Vrijheid M. The exposome: a new paradigm to study the impact of environment on health. Thorax. 2014;69:876–8. doi: 10.1136/thoraxjnl-2013-204949. [DOI] [PubMed] [Google Scholar]