Abstract
Purpose
Many patients with inflammatory bowel disease (IBD) have impaired health-related quality of life (HRQOL). The influence of psychological and economic factors on HRQOL has not been fully elucidated in IBD. Therefore, we aimed to identify the predictors of HRQOL in an IBD cohort.
Patients and methods
This was a cross-sectional cohort study of patients presenting to our tertiary IBD center. HRQOL was measured using the 36-item Short Form Health Survey (SF-36) and the Inflammatory Bowel Disease Questionnaire (IBDQ). Anxiety and depression were assessed by the Hospital Anxiety and Depression Scale (HADS). Perceived stress and perceived social support were also assessed by standardized scales. Demographic, socioeconomic and clinical data were obtained from a prespecified questionnaire and patients’ medical records. Univariate analyses and multiple regression analysis were performed to identify predictors of HRQOL.
Results
A total of 242 IBD patients were recruited, and the questionnaire return rate was 90.5% (219/242). The prevalence rates of anxiety and depression were 24.7% and 17.4%, respectively. In all, 30.6% of the patients spent over half of their income to cover medical costs. Multivariate analysis revealed that anxiety symptoms (P<0.001), active disease (P<0.001) and higher medical expenditures (P=0.001) were strong and independent predictors of reduced HRQOL.
Conclusion
Psychological factors and costs of medical care strongly impair HRQOL in IBD, independent of the disease activity. Psychological counseling and socioeconomic support programs should be considered for integration into the management of IBD patients.
Keywords: inflammatory bowel disease, Crohn’s disease, health-related quality of life, anxiety, depression, stress
Introduction
Inflammatory bowel disease (IBD) is a chronic relapsing disease that affects the gastrointestinal tract and encompasses Crohn’s disease (CD) and ulcerative colitis (UC). The clinical course is characterized by alternating periods of remission and exacerbations, with possible complications of intestinal stricture, fistula and intra-abdominal abscess, in the case of CD. These clinical characteristics often mandate long-term treatment, frequent physician visits, repeated hospitalizations and even surgeries. Thus, patients with IBD are inflicted with heavy physical, emotional and economic burden, leading to impaired quality of life (QOL)1–3 and decreased functioning and activity participation.4
Health-related quality of life (HRQOL) is defined as a multidimensional concept representing the physiological, psychological and social functioning of health perceived by individuals.5 Impaired HRQOL is very common in chronic disorders such as IBD.6
Although psychological disorders were found to be prevalent among IBD patients,7 the specific correlation between psychological factors and HRQOL has been hitherto poorly defined.8 Psychological distress such as anxiety and depression may affect the QOL and outcome of treatment in IBD patients.9,10 Previous studies have demonstrated that disease activity was associated with HRQOL.11 However, a reduced HRQOL is also found during remission periods,12 implying that other factors are also involved in the QOL of IBD patients, possibly psychological or socioeconomic. Thus, elucidating the factors that influence HRQOL in patients with IBD will fill an important knowledge gap that may lead to strategies improving the QOL and care of these challenging patients. Moreover, because psychological factors may be heavily dependent on specific cultural conceptions,13 studies investigating them in one ethnic group may not be readily applicable to other cultural or ethnic groups.
There have been tremendous increases in the numbers of Asian IBD patients who have distinct disease phenotype, genetic background, environmental exposures, socioeconomic changes and health care systems from Caucasian subjects.14 Therefore, the purpose of the present study was to explore the broad risk factors, psychological and socioeconomic, beyond disease activity per se that may be associated with impaired HRQOL in IBD patients, in a previously little investigated Asian IBD population.
Patients and methods
Design and population
This was a cross-sectional cohort study to explore the influence of psychological, clinical and demographic variables on HRQOL among patients with IBD. The study population was recruited between December 2014 and December 2015 from the tertiary IBD center of the First Affiliated Hospital of Sun Yat-sen University, China. Patients completed several questionnaires related to HRQOL and psychological factors (described in the Variables section). Clinical and demographic data were extracted from the questionnaires and patients’ charts.
Eligible patients were older than 18 years and were previously diagnosed with CD or UC based on clinical, endoscopic, radiographic and histological criteria. The exclusion criteria included patients who were unable to complete the questionnaires or understand the consent form. Patients with unclassified IBD were also excluded. The study protocol was approved by the Clinical Research Ethics Committee of the First Affiliated Hospital of Sun Yat-sen University. All patients gave a written informed consent to participate in this study.
Variables
Health-related quality of life
The Inflammatory Bowel Disease Questionnaire (IBDQ) is a disease-specific instrument that measures HRQOL of patients with IBD.15 The IBDQ explores four dimensions, including bowel symptoms, systemic symptoms, emotional function and social impairment. It contains 32 questions using a 7-point Likert scale, ranging from 1 to 7 (designating the worst possible and best QOL, respectively). The total scores range from 32 to 224. Higher scores mean better HRQOL. The Chinese version of IBDQ had been validated previously.16 Furthermore, we used the median level of IBDQ total scores as a cutoff value to differentiate low and high HRQOL. IBDQ total scores less than or equal to the median level were defined as low HRQOL, while IBDQ total scores more than the median level were considered as high HRQOL.
The 36-item Short Form Health Survey (SF-36) is a generic scale that assesses the health status of diverse patients as well as the general population.17 The SF-36 contains eight domains (physical functioning, role-physical, bodily pain, general health, vitality, social functioning, role-emotional and mental health). There are 35 items in the scale, with scores of subscales ranging from 0 to 100 (0 being the worst functional level and 100 the best).
Psychological variables
The Hospital Anxiety and Depression Scale (HADS) is a self-reported instrument that measures anxiety and depressive symptoms of patients.18 The HADS includes 14 items. Each item scores on a 4-point Likert scale from 0 to 3. There are two subscales, one that assesses anxiety (seven questions) and another for depression (seven questions). The scores of subscales range from 0 to 21. Higher scores represent a greater level of anxiety or depression. In the present study, subscale scores >7 were used to indicate possible anxiety and depression (not equated to a clinical diagnosis of depression or anxiety disorder).18
The Perceived Stress Scale (PSS) is the most widely used psychological instrument for measuring the perception of stress. It is a measure of the degree to which situations in one’s life are appraised as stressful. Items were designed to indicate how unpredictable, uncontrollable and overloaded respondents find their lives.19 The scale contains 10 items, and each item scores from 0 to 5. Higher scores of PSS-10 indicate greater level of perceived stress. The total scores range from 0 to 56.
The Multidimensional Scale of Perceived Social Support (MSPSS) is used to assess the level of social support that is available for the patients, as per his/her subjective perception.20 The MSPSS is a 12-item questionnaire. Each item ranges from 1 (very strongly disagree) to 7 (very strongly agree). Higher scores on the MSPSS represent greater level of social support perceived by the patient.
Demographic and clinical variables
A prespecified questionnaire was used to collect demographic data when patients were enrolled in the present study (Table 1). The information of educational level, marital status, procreation status, employment status, type of medical costs and the proportion of medical costs relative to personal income was acquired from this questionnaire.
Table 1.
Demographic characteristics of patients included in the study (n=219)
| Variable | All patients (n=219) |
Low HRQOLa (n=111) |
High HRQOLb (n=108) |
P-value |
|---|---|---|---|---|
| Female, n (%) | 81 (37.0) | 43 (38.7) | 38 (35.2) | 0.586 |
| Age, mean ± SD | 34.1±11.2 | 34.7±11.9 | 33.4±10.4 | 0.396 |
| Educational level, n (%) | 0.978 | |||
| Middle school | 52 (23.7) | 27 (24.3) | 25 (23.1) | |
| High school | 62 (28.3) | 31 (27.9) | 31 (28.7) | |
| College | 105 (47.9) | 53 (47.7) | 52 (48.1) | |
| Marital status, n (%) | 0.129 | |||
| Single | 81 (37.0) | 39 (35.1) | 42 (38.9) | |
| Married | 134 (61.2) | 68 (61.3) | 66 (61.1) | |
| Divorced | 4 (1.8) | 4 (3.6) | 0 (0.0) | |
| Procreation status, n (%) | 0.961 | |||
| Childless | 99 (45.2) | 50 (45.0) | 49 (45.4) | |
| Have children | 120 (54.8) | 61 (55.0) | 59 (54.6) | |
| Employment status, n (%) | 0.028 | |||
| Unemployment | 40 (18.3) | 23 (20.7) | 17 (15.7) | |
| Previous employment | 48 (21.9) | 31 (27.9) | 17 (15.7) | |
| Current employment | 131 (59.8) | 57 (51.4) | 74 (68.5) | |
| Type of medical costs, n (%) | 0.207 | |||
| Self-pay | 128 (58.4) | 60 (54.1) | 68 (63.0) | |
| Medical insurance | 91 (41.6) | 51 (45.9) | 40 (37.0) | |
| Proportion of medical costs relative to personal income, n (%) | 0.003 | |||
| <50% | 152 (69.4) | 67 (60.4) | 85 (78.7) | |
| ≥50% | 67 (30.6) | 44 (39.6) | 23 (21.3) | |
Notes:
IBDQ total scores were lower or equal to the median level of IBDQ scores.
IBDQ total scores were more than the median level of IBDQ scores. Median IBDQ total scores =173.
Abbreviations: HRQOL, health-related quality of life; SD, standard deviation; IBDQ, Inflammatory Bowel Disease Questionnaire.
The Harvey and Bradshaw Index (HBI) was used to evaluate disease activity for CD patients21 and the partial Mayo score (PMS) for UC patients.22 The disease activity was assessed by the doctor with >3 years of experience in the IBD field who distributed the questionnaires. A score of HBI >4 was defined as active disease for CD patients, while a PMS >2 was considered as active disease in UC patients, according to previous studies.21–23 The IBD relapses of patients in the last year were based on the European Crohn’s and Colitis Organisation (ECCO) guideline’s definition,24,25 and we collected the data from recorded follow-up forms in our database. Background clinical data were retrieved from the patients’ charts (Table 2).
Table 2.
Clinical characteristics of patients included in the study (n=219)
| Variable | All patients (n=219) |
Low HRQOL (n=111) |
High HRQOL (n=108) |
P-value |
|---|---|---|---|---|
| CD, n (%) | 146 (66.7) | 76 (68.5) | 70 (64.8) | 0.566 |
| Active disease, n (%) | 56 (25.6) | 46 (41.4) | 10 (9.3) | <0.001 |
| HBI (CD, n=146), median (range) | 2.0 (0–11) | 4.0 (0–11) | 1.0 (0–7) | |
| PMS (UC, n=73), median (range) | 1.0 (0–9) | 3.0 (0–9) | 0.0 (0–4) | |
| Disease duration (years), mean ± SD | 5.2±4.1 | 5.6±4.5 | 5.5±4.4 | 0.916 |
| Age of diagnosis, years (CD, n=146), n (%) | 0.606 | |||
| A1 (≤16) | 6 (4.1) | 3 (3.9) | 3 (4.3) | |
| A2 (17–40) | 125 (85.6) | 67 (88.2) | 58 (82.9) | |
| A3 (>40) | 15 (10.3) | 6 (7.9) | 9 (12.9) | |
| Location (CD, n=146), n (%) | 0.574 | |||
| L1 (ileal) | 16 (11) | 10 (13.2) | 6 (8.6) | |
| L2 (colonic) | 11 (7.6) | 4 (5.3) | 7 (10.0) | |
| L3 (ileocolonic) | 98 (67.1) | 52 (68.4) | 46 (65.7) | |
| L4 (upper GI tract) | 21 (14.4) | 10 (13.2) | 11 (15.7) | |
| Behavior (CD, n=146), n (%) | 0.910 | |||
| B1 (inflammatory) | 62 (42.5) | 31 (40.8) | 31 (44.3) | |
| B2 (stricturing) | 47 (32.2) | 25 (32.9) | 22 (31.4) | |
| B3 (penetrating) | 37 (25.3) | 20 (26.3) | 17 (24.3) | |
| Perianal disease (CD, n=146), n (%) | 0.692 | |||
| No | 102 (69.9) | 52 (68.4) | 50 (71.4) | |
| Yes | 44 (30.1) | 24 (31.6) | 20 (28.6) | |
| Extent of colitis (UC, n=73), n (%) | 0.161 | |||
| E1 (proctitis) | 10 (13.7) | 2 (5.7) | 8 (21.1) | |
| E2 (left side) | 30 (41.1) | 16 (45.7) | 14 (36.8) | |
| E3 (pancolitis) | 33 (45.2) | 17 (48.6) | 16 (42.1) | |
| Treatment, n (%) | 0.011 | |||
| No treatment | 11 (5.0) | 7 (6.3) | 4 (3.7) | |
| Mesalazine | 19 (8.7) | 14 (12.6) | 5 (4.6) | |
| Steroid | 18 (8.2) | 14 (12.6) | 4 (3.7) | |
| Immunosuppressive | 110 (50.2) | 47 (42.3) | 63 (58.3) | |
| Biologics | 61 (27.9) | 29 (26.1) | 32 (29.6) | |
| Relapses of IBD in last year, n (%) | 75 (34.2) | 50 (45.0) | 25 (23.1) | 0.001 |
| Hospitalizations for IBD in last year, n (%) | 85 (38.8) | 54 (48.6) | 31 (28.7) | 0.002 |
| History of surgical resection, n (%) | 50 (22.8) | 28 (25.2) | 22 (20.4) | 0.392 |
Abbreviations: HRQOL, health-related quality of life; CD, Crohn’s disease; HBI, Harvey and Bradshaw Index; PMS, partial Mayo score; UC, ulcerative colitis; GI, gastrointestinal; IBD, inflammatory bowel disease.
Statistical analysis
Descriptive analyses were performed for all clinical, demographic and psychological variables. Continuous variables were provided as mean (standard deviation [SD]) or median (range), and categorical variables were displayed as frequencies (proportions). Differences of each variable between patients with low and high HRQOL were compared using Student’s t-test, chi-square test or Fisher’s exact test, as appropriate.
IBDQ total scores were used as the dependent variable. Univariate analyses (Pearson’s correlation or Spearman’s rank correlation for continuous variables and independent two-sample t-test or analysis of variance [ANOVA] for categorical variables) were first performed between each variable and the IBDQ total scores.
Factors significantly associated with HRQOL in univariate analyses were entered into the multiple linear regression analysis with the IBDQ total score as the dependent variable. All data were analyzed in the Statistical Package for the Social Sciences (SPSS), version 13.0. Statistical significance was set at 0.05, and all tests were two tailed.
Results
Demographic and clinical characteristics
Of 242 IBD patients who were invited to participate in this study, 219 (90.5%) completed all questionnaires and comprised the study population. In total, 81 (37.0%) were women. The mean age of participants was 34.1 years (SD=11.2) and ranged from 18 to 74 years. The number of patients in early adulthood (20–39 years), mid adulthood (40–64 years) and late adulthood (>65 years) was 154, 61 and 4, respectively. Additional demographic characteristics of patients are summarized in Table 1.
Overall, a total of 146 (66.7%) patients had CD and 73 (33.3%) had UC. There were 56 (25.6%) participants with active disease when included in this study. In addition, 75 (34.2%) patients had disease relapses in the past year, and 85 (38.8%) patients had IBD-related hospitalizations during the year prior to inclusion in the study. Additional clinical features are shown in Table 2.
IBDQ scores and SF-36 scores
The mean IBDQ total score was 168.2 (SD=31.4, median 173, range 79–223). The mean scores of four dimensions (bowel symptoms, systemic symptoms, emotional function and social impairment) were all higher in the high HRQOL group compared with those in the low HRQOL group (P<0.001 for all comparisons; Table 3). The scores of SF-36 are described in Table 3. The scores of eight domains in SF-36 were all higher in the high HRQOL group than those in the low HRQOL group (P<0.001; Table 3).
Table 3.
Psychological characteristics of patients included in the study (n=219)
| Variable | All patients (n=219) |
Low HRQOL (n=111) |
High HRQOL (n=108) |
P-value |
|---|---|---|---|---|
| IBDQ, mean ± SD | ||||
| Total scores | 168.2±31.4 | 144.0±24.4 | 193.1±13.0 | <0.001 |
| Bowel symptoms | 56.4±9.4 | 50.0±8.4 | 63.0±4.6 | <0.001 |
| Systemic symptoms | 23.9±5.8 | 19.9±4.9 | 28.0±3.2 | <0.001 |
| Emotional function | 61.1±12.4 | 52.1±9.8 | 70.4±6.8 | <0.001 |
| Social impairment | 26.8±7.0 | 22.0±6.4 | 31.7±3.0 | <0.001 |
| SF-36, mean ± SD | ||||
| PF | 86.7±15.8 | 81.2±18.3 | 92.4±9.9 | <0.001 |
| RP | 60.8±39.1 | 41.2±38.5 | 81.0±27.9 | <0.001 |
| BP | 68.8±18.8 | 61.0±19.9 | 76.8±13.5 | <0.001 |
| GH | 47.0±20.1 | 38.2±16.3 | 56.0±19.6 | <0.001 |
| VT | 63.5±18.8 | 55.0±19.0 | 72.2±14.1 | <0.001 |
| SF | 69.3±22.7 | 56.1±21.8 | 82.9±13.8 | <0.001 |
| RE | 62.7±38.5 | 43.2±38.0 | 82.7±27.1 | <0.001 |
| MH | 68.3±17.3 | 60.6±16.6 | 76.2±14.2 | <0.001 |
| HADS | ||||
| HADS-Anxiety, mean ± SD | 5.5±3.7 | 7.5±3.6 | 3.4±2.4 | <0.001 |
| HADS-Depression mean ± SD | 4.7±3.7 | 6.5±3.9 | 2.9±2.5 | <0.001 |
| HADS-Anxiety >7, n (%) | 54 (24.7) | 48 (43.2) | 6 (5.6) | <0.001 |
| HADS-Depression >7, n (%) | 38 (17.4) | 34 (30.6) | 4 (3.7) | <0.001 |
| PSS-10, mean ± SD | 15.7±6.4 | 18.0±6.1 | 13.3±5.9 | <0.001 |
| MSPSS, mean ± SD | 64.9±10.7 | 63.4±12.0 | 66.5±9.1 | 0.033 |
Abbreviations: HRQOL, health-related quality of life; IBDQ, Inflammatory Bowel Disease Questionnaire; SD, standard deviation; SF-36, 36-item Short Form Health Survey; PF, physical functioning; RP, role-physical; BP, bodily pain; GH, general health; VT, vitality; SF, social functioning; RE, role-emotional; MH, mental health; HADS, Hospital Anxiety and Depression Scale; PSS-10, Perceived Stress Scale-10; MSPSS, Multidimensional Scale of Perceived Social Support.
Correlation of anxiety and depression with IBDQ scores
The proportion of patients with anxiety (24.7%) was higher than that of patients with depression (17.4%). Among the entire sample, a total of 157 (71.7%, designated as group 1) patients had neither anxiety nor depression, 32 (14.6%) had only anxiety without depression or only depression without anxiety (group 2) and 30 (13.7%) had both anxiety and depression (group 3). Patients of group 1 had the highest mean IBDQ total scores (177.8, SD=25.3), while those of group 3 had the lowest (131.4, SD=29.4). A significant difference in IBDQ scores was found between the three groups (P<0.001, ANOVA test). The results of this analysis are presented in Figure 1. In addition, anxiety scores negatively correlated with the IBDQ emotional function scores (r=−0.720, P<0.001). Similarly, depression scores negatively correlated with IBDQ emotional function scores (r=−0.612, P<0.001).
Figure 1.
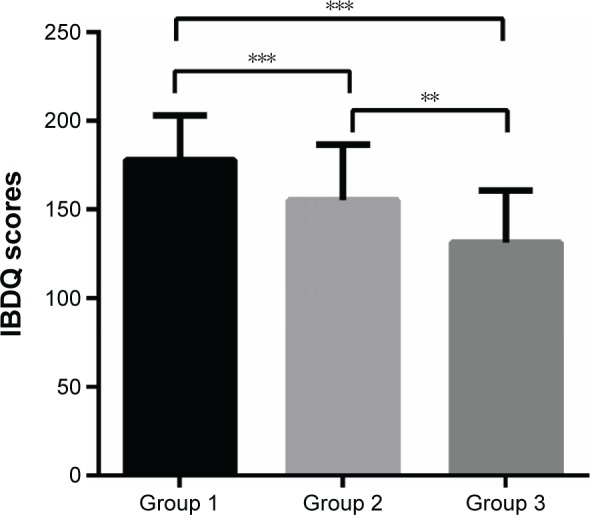
Comparison of IBDQ total scores between three groups.
Notes: Group 1: patients with neither anxiety nor depression, group 2: patients with either anxiety or depression and group 3: patients with both anxiety and depression. **P<0.01 and ***P<0.001
Abbreviation: IBDQ, Inflammatory Bowel Disease Questionnaire.
PSS-10 scores and MSPSS scores
The low HRQOL group had significantly higher PSS-10 stress scores than the high HRQOL group (P<0.001, t-test). Furthermore, the patients in the low HRQOL group had lower MSPSS social support scores compared with those in the high HRQOL group (P=0.033, t-test). More information is provided in Table 3.
Factors associated with HRQOL
Univariate analyses
Univariate analyses revealed several variables to be significantly associated with HRQOL. Anxiety scores negatively correlated with IBDQ scores (r=−0.660, P<0.001). Similarly, depression scores negatively correlated with IBDQ scores (r=−0.533, P<0.001). PSS-10 scores were negatively associated with IBDQ scores (r=−0.433, P<0.001), while MSPSS scores were positively although weakly correlated with IBDQ scores (r=0.163, P=0.016). Regarding clinical variables, patients with active disease had lower IBDQ scores than those in remission (138.9±31.8 versus 178.3±24.2, respectively, P<0.001). No difference was seen in the measurement when stratified by the type of disease (CD or UC). In addition, occurrence of relapses and hospitalizations in the last year correlated with impaired HRQOL (Table 4). Socioeconomic variable analysis showed that the unemployment status correlated with lower IBDQ scores (unemployment versus employment, P=0.015). Moreover, a higher proportion of medical costs relative to one’s income was associated with lower IBDQ scores (<50% versus ≥50%, P=0.001; Table 4).
Table 4.
Univariate relationships between variables and IBDQ total scores
| Variable | t | r | F | P-value |
|---|---|---|---|---|
| Demographic factors | ||||
| Gender | 0.554 | 0.580 | ||
| Age | −0.087 | 0.201 | ||
| Educational level | 0.113 | 0.893 | ||
| Marital status | 0.854 | 0.394 | ||
| Procreation status | 0.901 | 0.368 | ||
| Employment statusa | −2.452 | 0.015 | ||
| Proportion of medical costs relative to personal incomeb | 3.345 | 0.001 | ||
| Clinical factors | ||||
| Type of disease | −0.150 | 0.881 | ||
| Disease activity | 8.459 | <0.001 | ||
| Disease duration (≤5 versus >5 years) | 1.448 | 0.149 | ||
| Relapses for IBD in last year | 4.109 | <0.001 | ||
| Hospitalizations for IBD in last year | 3.315 | 0.001 | ||
| Previous IBD surgery | 0.371 | 0.711 | ||
| Psychological factors | ||||
| HADS-Anxiety | −0.660 | <0.001 | ||
| HADS-Depression | −0.533 | <0.001 | ||
| PSS-10 | −0.433 | <0.001 | ||
| MSPSS | 0.163 | 0.016 | ||
Notes:
Unemployment versus employment.
<50% versus ≥50%.
Abbreviations: IBDQ, Inflammatory Bowel Disease Questionnaire; IBD, inflammatory bowel disease; HADS, Hospital Anxiety and Depression Scale; PSS-10, Perceived Stress Scale-10; MSPSS, Multidimensional Scale of Perceived Social Support; t, Student’s t-test; r, Pearson’s correlation coefficient; F, analysis of variance.
Multivariate analysis
Based on the findings from the univariate analyses, the variables that were significantly correlated with IBDQ scores were subsequently entered into the multiple linear regression analysis. The results of this multivariate analysis showed that anxiety symptoms (P<0.001), active disease (P<0.001) and higher proportion of medical cost (P=0.001) were retained as independently and strongly associated with poor IBDQ scores, which explained 61% of the variation in this assessment of HRQOL (Table 5).
Table 5.
Multiple linear regression analyses between variables and IBDQ total scores
| Variable | B | Standard error | Beta coefficient | t | P-value |
|---|---|---|---|---|---|
| HADS-Anxiety | −4.691 | 0.369 | −0.549 | −12.730 | <0.001 |
| Disease activity | −30.234 | 3.118 | −0.421 | −9.696 | <0.001 |
| Medical costa | −9.381 | 2.904 | −0.138 | −3.231 | 0.001 |
| Adjusted R2 | 0.611 |
Note:
Proportion of medical costs relative to personal income: <50% versus ≥50%.
Abbreviations: IBDQ, Inflammatory Bowel Disease Questionnaire; HADS, Hospital Anxiety and Depression Scale; t, Student’s t-test.
Discussion
In the present study, we focused on the influence of psychological, clinical and socioeconomic variables on HRQOL of IBD patients in a tertiary center. We found that anxiety symptoms, active disease and need for higher medical expenditures were strong and independent risk factors for impaired HRQOL in this IBD cohort.
Our observations are in line with previous studies that had indicated psychological factors being an independent predictor of reduced HRQOL among IBD patients.26,27 Strikingly however, our results showed that anxiety may be a stronger determinant for impaired HRQOL than disease activity alone. Moreover, patients with one or more mood disorders had lower HRQOL than those without psychological disorder. In our study, the prevalence of anxiety was ~25%, while that of depression was 17% in the entire cohort. These rates generally align with the rates reported in other populations and ethnicities. A study from Austria indicated that the rate of depression was 28% during remission periods of IBD.10 A recent study from South Korea showed that anxiety and depression were identified in 27% and 33% of IBD patients, respectively.28 Interestingly, a previous study from France reported that 41% of IBD patients were anxious and 11% were depressed,29 which was a higher proportion of patients with anxiety than that of our study. The reason could be that in the Western cohort, most of the patients had severe disease. The disease activity and severity had negative effect on the psychiatric disorders of patients. In addition, some studies reported a higher prevalence of anxiety and depression in IBD patients compared with other chronic diseases or compared to in the general population.30,31 Moreover, Walker et al32 found that depression and anxiety disorders may affect response to treatment and HRQOL in IBD patients. Unlike our study, in which anxiety but not depression remained independently associated with HRQOL in multivariate analysis, a survey by Zhang et al33 identified depression rather than anxiety as a more significant risk factor of poor HRQOL than disease severity solely. The reasons for this discordant finding may be due to the different sample included in the studies and the dissimilar instruments used to measure anxiety and depression in the previous study.33
Higher level of perceived stress was associated with poor HRQOL in univariate analysis. Previous studies indicated that psychological stress may correlate with flares and disease exacerbation of IBD patients.34 Moreover, Boye et al35 found that stress management psychotherapy might improve HRQOL in IBD patients with a high level of stress. Similar to prior report,36 we additionally found that the level of perceived social support was positively correlated with HRQOL in univariate analysis, although this association did not retain independent impact on multivariate analysis.
The present results confirm that active disease was a strong risk factor for impaired HRQOL among IBD patients. This is in accordance with previous studies37,38 that have found patients with active disease to have lower QOL than those in remission. Relapses and hospitalizations in the last year were associated with diminished HRQOL in univariate analyses, echoing several studies similarly indicating relapses and hospitalizations correlated with poor HRQOL in IBD.39,40 However, when adjusting for the effects of disease activity indices and psychological factors in the multivariate analysis, the rate of relapse and hospitalizations no longer retained its significant association with HRQOL, suggesting that its effects are perhaps mediated via influence on anxiety state and/or are overshadowed by the impact of disease activity at the time of HRQOL assessment.
Of note, to the best of our knowledge, there are limited data on how personal, economic and fiscal consequences of disease impact HRQOL of IBD patients. Naturally, such analysis is heavily dependent on local reimbursement policies in different countries and even within each country as per different health payer programs. Nonetheless, several studies reported a substantial health and economic burden in European and American IBD patients.41–43 In this context, a striking finding of the present study was that incurring a higher medical cost and expenditure in proportion to one’s personal income was a strong and independent risk factor of impaired HRQOL. When assessing the total medical costs, including outpatient care, diagnostics, hospitalization, surgery and medications, we found that 30.6% of the patients had spent over half of their income to cover medical costs, and this economic burden had an independent detrimental impact on HRQOL (Tables 4 and 5). Interestingly, HRQOL was only associated with the direct burden of medical costs, but was not independently associated with employment status or education level (Table 5). This may suggest that patients ascribe a different meaning to direct medical costs as opposed to general economic or educational status when they conceptualize their HRQOL. This hypothesis was not addressed in the present study, but may merit direct investigation by appropriate psycho-assessment tools in future studies. Furthermore, these findings have to be interpreted in the context of the medical reimbursement situation in China whereby not all patients are under an efficient national reimbursement program by the state. In China, the IBD care is based on tertiary referral centers. There are three major types of public insurance covering most of the rural and urban residents. According to the current reimbursement policy, the IBD patients need to co-pay for the cost of medical investigations and medications. In addition, studies to address the impact of medical costs in other countries in relation to reimbursement and private medicine costs are warranted.
There are several strengths in this study. It is one of the few studies that has comprehensively assessed the risk factors of HRQOL in an Asian IBD population. Furthermore, we focused on the psychological factors associated with HRQOL as well as clinical and socioeconomic variables in the same IBD cohort. In addition, the use of validated questionnaires provided a quantitative evaluation of psychological characteristics and HRQOL, which is beneficial for horizontal comparison between studies.
It should be noted that the present study has a few limitations. The primary limitation is the cross-sectional study design, precluding the possibility to ascertain the causality between risk factors and HRQOL. Second, the participants were from a single tertiary IBD center, and most of them were afflicted with a complicated disease course. Therefore, the severe spectrum of the IBD population may be overrepresented in this study. Finally, the small sample size of UC patients precluded performance of separate subanalyses for patients with CD and UC, which will merit future investigation.
Conclusion
Our study indicates that anxiety symptoms, active disease and higher economic burden of medical expenditures are significant determinants of poor HRQOL in IBD patients. These findings shed light on the broad and complex factors that affect QOL of IBD patients and indicate the need for comprehensive strategies beyond medical care alone to improve HRQOL in these challenging patients.
Acknowledgments
This study was financially supported in part by the National Natural Science Foundation of China (NSFC grant nos 81470821, 81270473 and 81500501). We appreciate Ying-fan Zhang for collecting data during this study. We also appreciate Doctor Rui Feng and Doctor Rupert WL Leong for critically reviewing this article.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Bassi A, Dodd S, Williamson P, Bodger K. Cost of illness of inflammatory bowel disease in the UK: a single centre retrospective study. Gut. 2004;53(10):1471–1478. doi: 10.1136/gut.2004.041616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Casellas F, López-Vivancos J, Casado A, Malagelada JR. Factors affecting health related quality of life of patients with inflammatory bowel disease. Qual Life Res. 2002;11(8):775–781. doi: 10.1023/a:1020841601110. [DOI] [PubMed] [Google Scholar]
- 3.Bernklev T, Jahnsen J, Lygren I, Henriksen M, Vatn M, Moum B. Health-related quality of life in patients with inflammatory bowel disease measured with the short form-36: psychometric assessments and a comparison with general population norms. Inflamm Bowel Dis. 2005;11(10):909–918. doi: 10.1097/01.mib.0000179467.01748.99. [DOI] [PubMed] [Google Scholar]
- 4.Leong RW, Huang T, Ko Y, et al. Prospective validation study of the international classification of functioning, disability and health score in Crohn’s disease and ulcerative colitis. J Crohns Colitis. 2014;8(10):1237–1245. doi: 10.1016/j.crohns.2014.02.028. [DOI] [PubMed] [Google Scholar]
- 5.Irvine EJ. Quality of life issues in patients with inflammatory bowel disease. Am J Gastroenterol. 1997;92(12 suppl):18S–24S. [PubMed] [Google Scholar]
- 6.Lönnfors S, Vermeire S, Greco M, Hommes D, Bell C, Avedano L. IBD and health-related quality of life – discovering the true impact. J Crohns Colitis. 2014;8(10):1281–1286. doi: 10.1016/j.crohns.2014.03.005. [DOI] [PubMed] [Google Scholar]
- 7.Graff LA, Walker JR, Bernstein CN. Depression and anxiety in inflammatory bowel disease: a review of comorbidity and management. Inflamm Bowel Dis. 2009;15(7):1105–1118. doi: 10.1002/ibd.20873. [DOI] [PubMed] [Google Scholar]
- 8.Sajadinejad MS, Asgari K, Molavi H, Kalantari M, Adibi P. Psychological issues in inflammatory bowel disease: an overview. Gastroenterol Res Pract. 2012;2012:106502. doi: 10.1155/2012/106502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Persoons P, Vermeire S, Demyttenaere K, et al. The impact of major depressive disorder on the short- and long-term outcome of Crohn’s disease treatment with infliximab. Aliment Pharmacol Ther. 2005;22(2):101–110. doi: 10.1111/j.1365-2036.2005.02535.x. [DOI] [PubMed] [Google Scholar]
- 10.Mittermaier C, Dejaco C, Waldhoer T, et al. Impact of depressive mood on relapse in patients with inflammatory bowel disease: a prospective 18-month follow-up study. Psychosom Med. 2004;66(1):79–84. doi: 10.1097/01.psy.0000106907.24881.f2. [DOI] [PubMed] [Google Scholar]
- 11.Blondel-Kucharski F, Chircop C, Marquis P, et al. Groupe d’Etudes Thérapeutique des Affections Inflammatoires Digestives (GETAID) Health-related quality of life in Crohn’s disease: a prospective longitudinal study in 231 patients. Am J Gastroenterol. 2001;96(10):2915–2920. doi: 10.1111/j.1572-0241.2001.4681_b.x. [DOI] [PubMed] [Google Scholar]
- 12.Simrén M, Axelsson J, Gillberg R, Abrahamsson H, Svedlund J, Björnsson ES. Quality of life in inflammatory bowel disease in remission: the impact of IBS-like symptoms and associated psychological factors. Am J Gastroenterol. 2002;97(2):389–396. doi: 10.1111/j.1572-0241.2002.05475.x. [DOI] [PubMed] [Google Scholar]
- 13.Dunlop DD, Song J, Lyons JS, Manheim LM, Chang RW. Racial/ethnic differences in rates of depression among preretirement adults. Am J Public Health. 2003;93(11):1945–1952. doi: 10.2105/ajph.93.11.1945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Leong RW, Lawrance IC, Ching JY, et al. Knowledge, quality of life, and use of complementary and alternative medicine and therapies in inflammatory bowel disease: a comparison of Chinese and Caucasian patients. Dig Dis Sci. 2004;49(10):1672–1676. doi: 10.1023/b:ddas.0000043384.26092.f4. [DOI] [PubMed] [Google Scholar]
- 15.Guyatt G, Mitchell A, Irvine EJ, et al. A new measure of health status for clinical trials in inflammatory bowel disease. Gastroenterology. 1989;96(3):804–810. [PubMed] [Google Scholar]
- 16.Ren WH, Lai M, Chen Y, Irvine EJ, Zhou YX. Validation of the mainland Chinese version of the Inflammatory Bowel Disease Questionnaire (IBDQ) for ulcerative colitis and Crohn’s disease. Inflamm Bowel Dis. 2007;13(7):903–910. doi: 10.1002/ibd.20128. [DOI] [PubMed] [Google Scholar]
- 17.Ware JJ, Sherbourne CD. The MOS 36-item short-form health survey (SF-36). I. Conceptual framework and item selection. Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 18.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 19.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 20.Zimet GD, Powell SS, Farley GK, Werkman S, Berkoff KA. Psychometric characteristics of the multidimensional scale of perceived social support. J Pers Assess. 1990;55(3–4):610–617. doi: 10.1080/00223891.1990.9674095. [DOI] [PubMed] [Google Scholar]
- 21.Harvey RF, Bradshaw JM. A simple index of Crohn’s-disease activity. Lancet. 1980;1(8167):514. doi: 10.1016/s0140-6736(80)92767-1. [DOI] [PubMed] [Google Scholar]
- 22.Schroeder KW, Tremaine WJ, Ilstrup DM. Coated oral 5-aminosalicylic acid therapy for mildly to moderately active ulcerative colitis. A randomized study. N Engl J Med. 1987;317(26):1625–1629. doi: 10.1056/NEJM198712243172603. [DOI] [PubMed] [Google Scholar]
- 23.Gibson PR, Vaizey C, Black CM, et al. Relationship between disease severity and quality of life and assessment of health care utilization and cost for ulcerative colitis in Australia: a cross-sectional, observational study. J Crohns Colitis. 2014;8(7):598–606. doi: 10.1016/j.crohns.2013.11.017. [DOI] [PubMed] [Google Scholar]
- 24.Van Assche G, Dignass A, Panes J, et al. The second European evidence-based consensus on the diagnosis and management of Crohn’s disease: definitions and diagnosis. J Crohns Colitis. 2010;4:7–27. doi: 10.1016/j.crohns.2009.12.003. [DOI] [PubMed] [Google Scholar]
- 25.Dignass A, Eliakim R, Magro F, et al. Second European evidence-based consensus on the diagnosis and management of ulcerative colitis part 1: definitions and diagnosis. J Crohns Colitis. 2012;6:965–990. doi: 10.1016/j.crohns.2012.09.003. [DOI] [PubMed] [Google Scholar]
- 26.Guthrie E, Jackson J, Shaffer J, Thompson D, Tomenson B, Creed F. Psychological disorder and severity of inflammatory bowel disease predict health-related quality of life in ulcerative colitis and Crohn’s disease. Am J Gastroenterol. 2002;97(8):1994–1999. doi: 10.1111/j.1572-0241.2002.05842.x. [DOI] [PubMed] [Google Scholar]
- 27.Vidal A, Gomez-Gil E, Sans M, et al. Health-related quality of life in inflammatory bowel disease patients: the role of psychopathology and personality. Inflamm Bowel Dis. 2008;14(7):977–983. doi: 10.1002/ibd.20388. [DOI] [PubMed] [Google Scholar]
- 28.Kim ES, Cho KB, Park KS, et al. Daegukyungbook Gastrointestinal Study Group (DGSG) Predictive factors of impaired quality of life in Korean patients with inactive inflammatory bowel disease: association with functional gastrointestinal disorders and mood disorders. J Clin Gastroenterol. 2013;47(4):e38–e44. doi: 10.1097/MCG.0b013e318266fff5. [DOI] [PubMed] [Google Scholar]
- 29.Nahon S, Lahmek P, Durance C, et al. Risk factors of anxiety and depression in inflammatory bowel disease. Inflamm Bowel Dis. 2012;18(11):2086–2091. doi: 10.1002/ibd.22888. [DOI] [PubMed] [Google Scholar]
- 30.Häuser W, Janke KH, Klump B, Hinz A. Anxiety and depression in patients with inflammatory bowel disease: comparisons with chronic liver disease patients and the general population. Inflamm Bowel Dis. 2011;17(2):621–632. doi: 10.1002/ibd.21346. [DOI] [PubMed] [Google Scholar]
- 31.Loftus EJ, Guerin A, Yu AP, et al. Increased risks of developing anxiety and depression in young patients with Crohn’s disease. Am J Gastroenterol. 2011;106(9):1670–1677. doi: 10.1038/ajg.2011.142. [DOI] [PubMed] [Google Scholar]
- 32.Walker JR, Ediger JP, Graff LA, et al. The Manitoba IBD cohort study: a population-based study of the prevalence of lifetime and 12-month anxiety and mood disorders. Am J Gastroenterol. 2008;103(8):1989–1997. doi: 10.1111/j.1572-0241.2008.01980.x. [DOI] [PubMed] [Google Scholar]
- 33.Zhang CK, Hewett J, Hemming J, et al. The influence of depression on quality of life in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2013;19(8):1732–1739. doi: 10.1097/MIB.0b013e318281f395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mawdsley JE, Rampton DS. Psychological stress in IBD: new insights into pathogenic and therapeutic implications. Gut. 2005;54(10):1481–1491. doi: 10.1136/gut.2005.064261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Boye B, Lundin KE, Jantschek G, et al. INSPIRE study: does stress management improve the course of inflammatory bowel disease and disease-specific quality of life in distressed patients with ulcerative colitis or Crohn’s disease? A randomized controlled trial. Inflamm Bowel Dis. 2011;17(9):1863–1873. doi: 10.1002/ibd.21575. [DOI] [PubMed] [Google Scholar]
- 36.Oliveira S, Zaltman C, Elia C, et al. Quality-of-life measurement in patients with inflammatory bowel disease receiving social support. Inflamm Bowel Dis. 2007;13(4):470–474. doi: 10.1002/ibd.20071. [DOI] [PubMed] [Google Scholar]
- 37.Larsson K, Lööf L, Rönnblom A, Nordin K. Quality of life for patients with exacerbation in inflammatory bowel disease and how they cope with disease activity. J Psychosom Res. 2008;64(2):139–148. doi: 10.1016/j.jpsychores.2007.10.007. [DOI] [PubMed] [Google Scholar]
- 38.Graff LA, Walker JR, Lix L, et al. The relationship of inflammatory bowel disease type and activity to psychological functioning and quality of life. Clin Gastroenterol Hepatol. 2006;4(12):1491–1501. doi: 10.1016/j.cgh.2006.09.027. [DOI] [PubMed] [Google Scholar]
- 39.Casellas F, Arenas JI, Baudet JS, et al. Impairment of health-related quality of life in patients with inflammatory bowel disease: a Spanish multicenter study. Inflamm Bowel Dis. 2005;11(5):488–496. doi: 10.1097/01.mib.0000159661.55028.56. [DOI] [PubMed] [Google Scholar]
- 40.Moradkhani A, Beckman LJ, Tabibian JH. Health-related quality of life in inflammatory bowel disease: psychosocial, clinical, socioeconomic, and demographic predictors. J Crohns Colitis. 2013;7(6):467–473. doi: 10.1016/j.crohns.2012.07.012. [DOI] [PubMed] [Google Scholar]
- 41.Odes S, Vardi H, Friger M, et al. Clinical and economic outcomes in a population-based European cohort of 948 ulcerative colitis and Crohn’s disease patients by Markov analysis. Aliment Pharmacol Ther. 2010;31(7):735–744. doi: 10.1111/j.1365-2036.2009.04228.x. [DOI] [PubMed] [Google Scholar]
- 42.Burisch J, Jess T, Martinato M, Lakatos PL, ECCO-EpiCom The burden of inflammatory bowel disease in Europe. J Crohns Colitis. 2013;7(4):322–337. doi: 10.1016/j.crohns.2013.01.010. [DOI] [PubMed] [Google Scholar]
- 43.Kappelman MD, Rifas-Shiman SL, Porter CQ, et al. Direct health care costs of Crohn’s disease and ulcerative colitis in US children and adults. Gastroenterology. 2008;135(6):1907–1913. doi: 10.1053/j.gastro.2008.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]


