Abstract
Background
Care of patients with inflammatory bowel disease (IBD) poses a significant burden to the health-care system. Repeat hospitalization in subgroups of IBD patients seems to be a large part of this issue; however, there are limited data examining the characteristics of these patients. The aim of this study was to characterize admission patterns in patients with IBD at a tertiary-care center and to identify preventable risk factors of 90-day readmission after an index IBD admission.
Methods
Retrospective analysis was performed extracting data from an electronic medical record over a 2-year period.
Results
Three hundred fifty-six patients were admitted at least once during the 2-year study period for an unplanned IBD-related reason. Of these, 48.9% were admitted once, 38.2% were admitted 2 to 4 times, and 12.9% were admitted 5 or more times during the study period. Patients with any admission within 90 days before index were excluded; n = 33. One hundred two patients had experienced a readmission by 90 days after index admission. Numerous demographic and medical factors were examined for association with readmission. The final Cox model included 3 variables: depression (HR = 1.99, 1.33–3.00), chronic pain (HR = 1.88, 1.14–3.10), and steroid use in the previous 6 months (HR = 1.33, 0.92–2.04).
Conclusions
Our findings suggest that patients with depression and chronic pain are at greatest risk for a readmission within 90 days after an initial IBD admission. Disease activity, represented by steroid use in the previous 6 months, was not related to readmission. Addressing these problems in the outpatient setting may reduce future hospitalizations.
Keywords: hospitalization, Crohn’s disease, ulcerative colitis, inflammatory bowel disease
Previous studies have demonstrated that the care of patients with inflammatory bowel disease (IBD) poses a significant burden to the health-care system. More than one and a half million people in the United States suffer from ulcerative colitis (UC) and Crohn’s disease. Patients with IBD require more frequent hospital admissions than non-IBD patients, with an increased average length of stay not only in the United States but also globally.1,2 Moreover, hospital care for IBD patients has been shown to be twice as expensive as that for non-IBD controls.3 Repeat hospitalization in subgroups of IBD patients seems to be a large part of this issue4,5; however, there is only limited literature examining the characteristics of IBD patients who are associated with frequent hospital use.
In an effort to improve responsible health-care spending, a focus must be aimed at reducing preventable admissions. It has become increasingly important to limit unnecessary hospital use in chronic disease populations. A meta-analysis of 10 randomized controlled trials in heart failure patients—an analogous chronic disease population—demonstrated that intensive outpatient monitoring through specialty clinics significantly reduces unplanned hospital admissions.6 Although there is less published experience with specialty clinics in IBD, preliminary studies suggest that an IBD-specific specialty clinic model may have a similar impact on reducing inpatient health-care utilization among these patients.7 As more focus is placed on providing tailored outpatient care for IBD patients, it becomes increasingly important to identify those patients most at risk and the factors associated with high hospital utilization.
Risk factors for hospitalizations in IBD have been explored. One previous study found that patients with mild disease accounted for more hospitalizations than patients with more severe disease.8 However, a recent study assessed 30-day and 90-day readmissions in UC patients and found that certain risk factors for 90-day readmission were in fact related to disease severity.9 Several previous studies have investigated the relationship between IBD and psychiatric disease. There is evidence that both depression and anxiety are more common in IBD patients10 and that both are likely undertreated.10 Depression has been linked to increased disease activity and lower quality of life in patients with IBD,11 and psychological stress is thought to be a possible trigger for disease flares.11,12 Similarly, patients with IBD have been found to have high rates of chronic pain, which has also been linked to decreased quality of life and depression.13
We sought to investigate these issues in more detail with the aim of identifying high-risk patients more accurately and eventually developing targeted intervention programs based on these data to reduce preventable readmission. Early readmission has not been consistently defined in the literature, though 30 to 90 days seems to be the most commonly used metrics. Therefore, we hypothesize that 90-day readmissions after an index IBD admission are because of risk factors unrelated to IBD activity and may relate to modifiable risks.
METHODS
Study Population
This study was conducted at Brigham and Women’s Hospital, a tertiary-care referral center in Boston, MA. Study subjects included all patients aged 18 years or older with a known diagnosis of IBD, who were admitted at least once between January 1, 2011, and December 31, 2012, for a nonelective IBD-related reason. IBD was considered to include either UC or Crohn’s disease (International Classification of Diseases, Ninth Revision codes 556.X and 555.X, respectively). IBD diagnosis therefore was based on the above International Classification of Diseases, Ninth Revision codes and a stated established diagnosis in the medical record. Patients with a diagnosis of indeterminate or nonspecific colitis were excluded. All admissions for treatment of IBD disease activity, treatment of IBD-associated illness, or for treatment of complications related to IBD medications were considered IBD related.
For each eligible patient, the first chronological, nonelective IBD-related admission during the study period was considered to be the index hospitalization. All admissions for any reason within 90 days before the index admission were also identified. Patients with an admission 90 days before the index admission were excluded. The specific information extracted from the medical records included the following:
-
Patient demographics
Age, sex, marital status, ethnicity, employment status, insurance type, and education level.
-
Patient’s IBD history
Disease type (UC or Crohn’s), previous surgical history, and medication regimen before hospital admission.
Past hospitalizations.
-
Patient’s non-IBD history
Presence of comorbid psychiatric diagnosis. These were listed in the patient’s medical history. Specifically, psychiatric diagnoses had to be listed, such as major depressive disorder, bipolar disorder, or generalized anxiety disorder. Patient could not merely be described as being depressed or anxious.
History of chronic pain syndrome. This was defined as documentation in the patient’s medical history by a provider more than once at least 3 months apart.
-
Habits
History of substance abuse, including alcohol, opiates, cocaine, and marijuana. These were defined as documented abuse in the social history by at least a physician. Specifically, with regard to alcohol abuse, the terms current or previous alcohol abuse needed to be listed in the medical history or more than 3 alcoholic beverages a day documented. Opiate use refers specifically to illicit drug use, such as heroine, and not to the use of prescription opiates.
Former or current tobacco use.
After each patient’s baseline data were extracted, all other admissions for this patient during the study period were reviewed, specifically those that occurred within 90 days of the index admission. Case report forms were used for raw data abstraction, and data were then entered into a Research Electronic Data Capture database.
Statistical Analyses
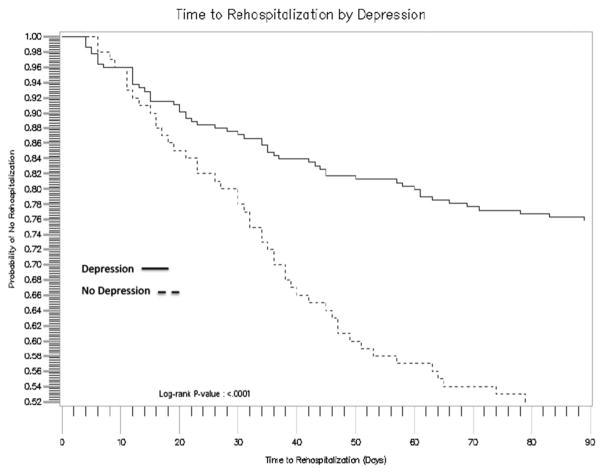
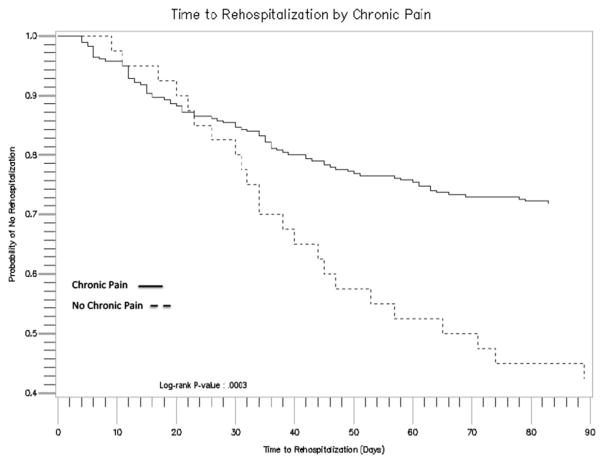
We developed a Cox proportional hazard model. Covariates that were felt a priori to be related to readmission were entered into the initial model. Two covariates of particular interest, depression and steroid use in the previous 6 months (this covariate served as a marker for disease activity), were forced into the model given that depression and disease activity have already been found to be associated with readmission in previous data. Stepwise selection was then performed with a significance level to enter 0.2 and a significance level to stay at 0.05 to allow for possible confounders into the model. Once our final model was constructed, we tested the proportional hazard assumption using Martingale residuals. Unadjusted survival curves were then constructed on significant covariates associated with the 90-day readmission.
RESULTS
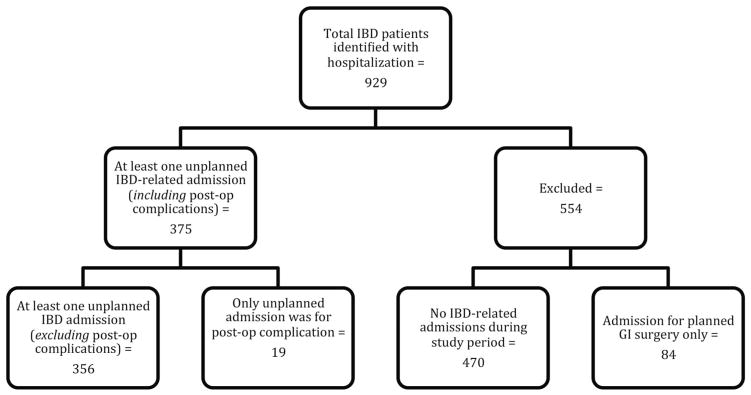
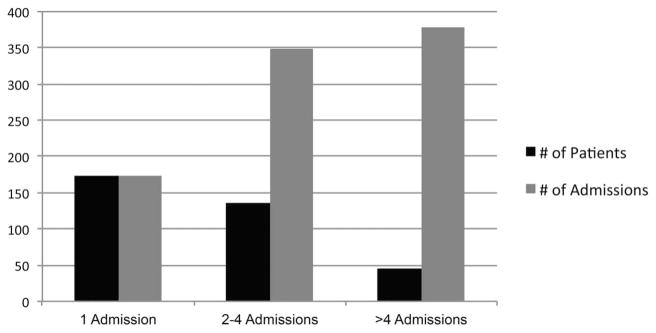
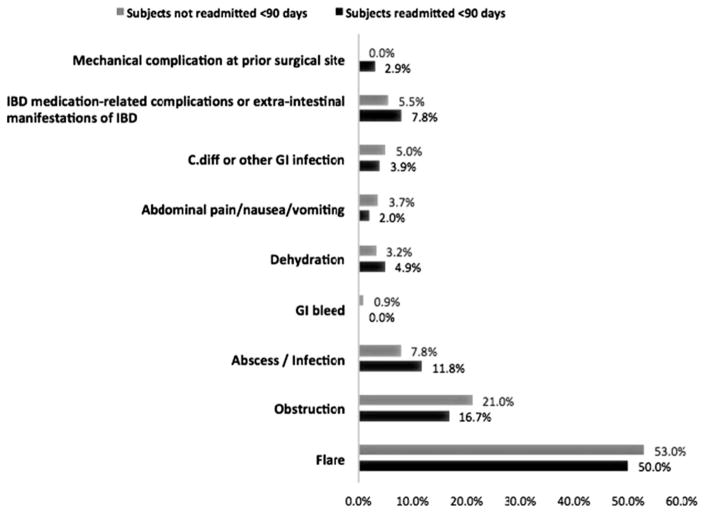
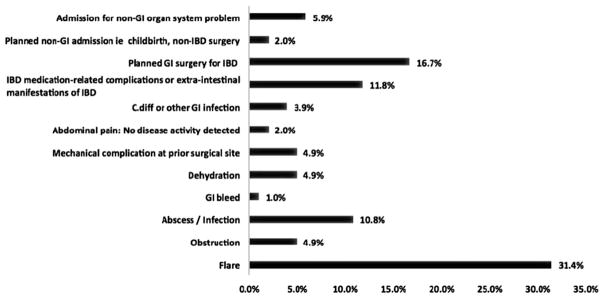
We identified a total of 356 patients (Fig. 1) who were admitted at least once during the 2-year study period for an unplanned IBD-related reason (Table 1). These 356 patients accounted for a total of 861 admissions over the study period. Of these patients, 209 (58.7%) had Crohn’s disease and 147 (41.2%) had UC. The mean age at the time of index admission was 41.7 years (SD ± 17). Women accounted for 62% (n = 220) of the cohort while men accounted for 38% (n = 136). Forty-six patients in the cohort were admitted 5 or more times (Fig. 2). All patients had an index IBD admission; 125 patients had experienced a readmission (for any reason) by 90 days. However, 33 patients had an admission 90 days before their index admission and were excluded, leaving 324 patients in the data set. Of those 324, 102 experienced a readmission by 90 days. No patients were censored before 90 days. All patients with admission after day 90 or without a readmission within the study period were considered censored. Reason for index admission was IBD flare in more than half of the cohort regardless of readmission status (Fig. 3). Reasons for all-cause readmission were mainly related to IBD with 31.4% for flare, 16.7% for a planned IBD operation, and 11.8% for IBD medication–related complication (Fig. 4). Only 5.9% of all readmissions were not related to gastrointestinal disease. The initial model contained 19 variables hypothesized to be likely risk factors for readmission. These included age, length of stay, depression, anxiety, sex, race, chronic pain, type of IBD, previous abdominal operation, tobacco use, ETOH abuse, opiate use, steroids in the previous 6 months, infliximab use at index admission, pain clinic follow-up scheduled after discharge, gastrointestinal follow-up scheduled after discharge, and psychiatric follow-up scheduled after discharge. Categorical variables included employment (1, employed; 2, not employed; 3, disabled; 4, student), insurance (1, private; 2, medicare; 3, medicaid; 4, self-pay), education (1, high school; 2, college; 3, graduate), and marital status (1, single; 2, married; 3, divorced; 4, widowed). The final model (Table 2) included 3 variables: depression (HR = 1.99, 1.33–3.00), chronic pain (HR = 1.88, 1.14–3.10), and steroid use in the previous 6 months (HR = 1.33, 0.92–2.04). The proportional hazard assumption was then tested using Martingale residuals for each of the 4 variables in the final model, and all resulted in non-significant P value. Therefore, the model did not violate the proportional hazard assumption and we proceeded with the Cox model. Unadjusted curves were constructed for each of the 2 significant variables (Figs. 5 and 6). The median time to readmission for patients with depression was 69.5 days, resulting in a log rank P value <0.0001. The median time to readmission for patients with chronic pain was 55 days, resulting in a log rank P value of 0.0003.
FIGURE 1.
Study inclusion and exclusion.
TABLE 1.
Study Population
| Variable | Study Population n = 356, n (%) |
|---|---|
| Male | 136 (38.2) |
| Mean age (±SD) | 41.7 (±17) |
| White race | 294 (82.5) |
| Crohn’s disease | 209 (58.7) |
| Marital statusa | |
| Single | 157 (44.1) |
| Married | 149 (41.8) |
| Divorced | 33 (9.2) |
| Widowed | 16 (4.4) |
| Educationb | |
| High school | 86 (24.1) |
| College | 83 (23.3) |
| Graduate | 3 (0.8) |
| Insurance | |
| Private | 235 (66.0) |
| Medicare | 73 (20.5) |
| Medicaid | 41 (11.5) |
| Self-pay | 8 (2.2) |
| Employment statusc | |
| Employed | 181 (50.8) |
| Not employed | 114 (32.0) |
| Disabled | 30 (8.4) |
| Student | 25 (7.0) |
| History of depression | 114 (32.0) |
| History of anxiety | 94 (26.4) |
| ETOH abuse | 16 (4.5) |
| Opiate abuse | 12 (3.3) |
| Tobacco use | 127 (35.6) |
| Chronic paind | 44 (12.3) |
| Cardiac History | 32 (8.9) |
| Previous gastrointestinal operation | 188 (52.8) |
| Other medications at index admission | |
| Immunomodulators | 41 (11.5) |
| Steroids | 87 (24.4) |
| Mesalamine | 24 (6.7) |
| Antibiotic | 41 (11.5) |
| Median length of stay (interquartile range) | 5 (5) |
2 values missing.
4 values missing.
7 values missing.
3 values missing.
FIGURE 2.
Disproportionate number of admissions in small subgroups of IBD patients.
FIGURE 3.
Reasons for index admissions.
FIGURE 4.
Reasons for ≥90-day Readmissions.
TABLE 2.
Cox Proportional Hazard Model for 90-day Readmission
| Variable | Hazard Ratio | 95% Confidence Interval | P |
|---|---|---|---|
| Depression | 1.99 | 1.33–3.00 | 0.0009 |
| Chronic pain | 1.88 | 1.14–3.10 | 0.013 |
| Steroids in the previous 6 mo | 1.33 | 0.92–2.04 | 0.118 |
FIGURE 5.
Unadjusted Kaplan–Meir curve for depression.
FIGURE 6.
Unadjusted Kaplan–Meir curve for chronic pain.
DISCUSSION
Despite multiple factors that were felt to be associated with readmission, our findings suggest that patients with a history of depression and chronic pain are at greatest risk for a readmission within 90 days after an initial IBD admission. Despite the fact that the readmissions were for disease-related reasons, disease activity, represented by steroid use in the previous 6 months, was not significantly associated with readmission. Our study identified that a history of comorbid psychiatric disease and chronic pain are associated with repeat hospitalization. Addressing these problems in the outpatient setting may reduce future hospitalizations in IBD patients.
Several recent studies have shown an increase in IBD hospitalization rates in the United States.8,14,15 However, only one group previously investigated hospitalization rates as a function of disease severity, finding that patients with mild-to-moderate disease severity account for most of the hospitalizations.8 Our study was able to show that a small number of patients seem to be responsible for a majority of readmissions. The index admission in our cohort was always for an IBD-related reason, and among the patients readmitted, a majority of the readmission diagnoses were secondary to flare or indirectly related to disease activity. Two previous studies investigated the variability in admission diagnosis for IBD patients. One study found that IBD patients were being admitted more frequently for treatment of cardiovascular disease than for treatment of their bowel disease.16 Another recent study analyzed admission diagnoses for IBD patients readmitted within 30 days of an index hospitalization. This study found that reasons for 30-day readmission were related to documented flare, infections, or need for pain control.17 Our study corroborates these previous data. In our cohort, patients with IBD readmitted within 90 days of an index IBD admission were more likely to have underlying depression or chronic pain regardless of the reason for readmission, as opposed to disease type, recent steroid use, or biological use. These findings underscore the importance of a multidisciplinary approach in treating patients with IBD.
Several previous studies have investigated the relationship between IBD, psychiatric disease, and hospitalization. Both depression and anxiety are more common in IBD patients,10 and both are likely undertreated.10 Depression has been linked to increased disease activity and lower quality of life in patients with IBD,11,18 and psychological stress is thought to be a possible trigger for disease flares. A recent meta-analysis of 18 randomized controlled trials concluded that although psychotherapy as a nontargeted intervention may show promise in reducing hospitalization, an even greater impact may be made by targeting specific psychiatric diagnoses.19 This cohort demonstrates an association between history of depression and increased rehospitalization rates, confirming that psychiatric disease leads to increased health-care utilization in IBD patients and likely worsening of disease given that reasons for readmission were largely disease related.
Chronic pain is a common sequela of IBD. There are little data on the relationship between chronic pain and IBD care. Morrison et al13 surveyed IBD patients and found higher disease activity, reduced quality of life, and more reports of depression and anxiety in patients who report pain everyday for at least 3 months. Long et al20 investigated narcotic use among hospitalized patients. This study found that narcotic use was not associated with disease severity. Similarly, chronic pain was a significant risk factor for readmission in this cohort irrespective of disease activity. Interestingly, narcotic use was not associated with readmission. This does lead to the hypothesis that IBD patients with chronic pain come to the hospital for narcotics. This again reinforces the importance of intensive outpatient programs to address pain control with other methods aside from narcotic use.
A notable negative finding from our study was the lack of association between race and 90-day readmission. Previous data found that in the United States, IBD was more prevalent overall in non-Hispanic Whites; however, IBD-related rehospitalization rates were disproportionately higher in non-Hispanic Blacks.21 Eighty-two percent of this cohort comprised White non-Hispanic patients. Of those who were rehospitalized within 90 days, 86.4% were Whites. This, however, is more likely a representation of the population in Boston, MA, and not necessarily representative of trends nationwide.
The primary limitations of our study include its retrospective design and reliance on data extracted from nonstandardized medical records. Very few patients had psychiatric records available in our system. Psychiatric records are often restricted for privacy reasons and patients may be receiving psychiatric care outside of our institution, thus leading to an underestimation of psychiatric comorbidities. Detection of chronic pain diagnoses, although consistent with Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition criteria, relied on interpretation of nonstandardized records and is therefore subject to bias. We were able to extract medication records, and narcotic use was not associated with readmissions. We also used steroid use within the previous 6 months as a surrogate for disease activity in the absence of standardized disease activity indices.
In summary, disease activity alone is not a good predictor for identifying patients at risk for early readmission. Patients with a history of depression and chronic pain are at risk for a readmission by 90 days after an initial IBD admission, regardless of the reason for readmission. Addressing these problems in the outpatient setting with a multidisciplinary approach may reduce future hospitalizations in IBD patients.
Footnotes
The authors have no conflicts of interest to disclose.
References
- 1.van Langenberg DR, Simon SB, Holtmann GJ, et al. The burden of inpatient costs in inflammatory bowel disease and opportunities to optimize care: a single metropolitan Australian center experience. J Crohns Colitis. 2010;4:413–421. doi: 10.1016/j.crohns.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 2.Sandberg KC, Davis MM, Gebremariam A, et al. Increasing hospitalizations in inflammatory bowel disease among children in the United States, 1988–2011. Inflamm Bowel Dis. 2014;20:1754–1760. doi: 10.1097/MIB.0000000000000195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bernstein CN, Longobardi T, Finlayson G, et al. Direct medical cost of managing IBD patients: a Canadian population-based study. Inflamm Bowel Dis. 2012;18:1498–1508. doi: 10.1002/ibd.21878. [DOI] [PubMed] [Google Scholar]
- 4.Nabalamba A, Bernstein CN, Seko C. Inflammatory bowel disease–hospitalization. Health Rep. 2004;15:25–40. [PubMed] [Google Scholar]
- 5.Nguyen GC, Bollegala N, Chong CA. Factors associated with readmissions and outcomes of patients hospitalized for inflammatory bowel disease. Clin Gastroenterol Hepatol. 2014;12:1897–1904. e1. doi: 10.1016/j.cgh.2014.02.042. [DOI] [PubMed] [Google Scholar]
- 6.Thomas R, Huntley A, Mann M, et al. Specialist clinics for reducing emergency admissions in patients with heart failure: a systematic review and meta-analysis of randomised controlled trials. Heart. 2013;99:233–239. doi: 10.1136/heartjnl-2012-302313. [DOI] [PubMed] [Google Scholar]
- 7.Sack C, Phan VA, Grafton R, et al. A chronic care model significantly decreases costs and healthcare utilisation in patients with inflammatory bowel disease. J Crohns Colitis. 2012;6:302–310. doi: 10.1016/j.crohns.2011.08.019. [DOI] [PubMed] [Google Scholar]
- 8.Ananthakrishnan AN, McGinley EL, Binion DG, et al. A nationwide analysis of changes in severity and outcomes of inflammatory bowel disease hospitalizations. J Gastrointest Surg. 2011;15:267–276. doi: 10.1007/s11605-010-1396-3. [DOI] [PubMed] [Google Scholar]
- 9.Tinsley A, Naymagon S, Mathers B, et al. Early readmission in patients hospitalized for ulcerative colitis: incidence and risk factors. Scand J Gastroenterol. 2015:1–7. doi: 10.3109/00365521.2015.1020862. [DOI] [PubMed] [Google Scholar]
- 10.Bennebroek Evertsz’ F, Thijssens NA, Stokkers PC, et al. Do inflammatory bowel disease patients with anxiety and depressive symptoms receive the care they need? J Crohns Colitis. 2012;6:68–76. doi: 10.1016/j.crohns.2011.07.006. [DOI] [PubMed] [Google Scholar]
- 11.Bernstein CN, Singh S, Graff LA, et al. A prospective population-based study of triggers of symptomatic flares in IBD. Am J Gastroenterol. 2010;105:1994–2002. doi: 10.1038/ajg.2010.140. [DOI] [PubMed] [Google Scholar]
- 12.Triantafillidis JK, Merikas E, Gikas A. Psychological factors and stress in inflammatory bowel disease. Expert Rev Gastroenterol Hepatol. 2013;7:225–238. doi: 10.1586/egh.13.4. [DOI] [PubMed] [Google Scholar]
- 13.Morrison G, Van Langenberg DR, Gibson SJ, et al. Chronic pain in inflammatory bowel disease: characteristics and associations of a hospital-based cohort. Inflamm Bowel Dis. 2013;19:1210–1217. doi: 10.1097/MIB.0b013e318280e729. [DOI] [PubMed] [Google Scholar]
- 14.Bewtra M, Su C, Lewis JD. Trends in hospitalization rates for inflammatory bowel disease in the United States. Clin Gastroenterol Hepatol. 2007;5:597–601. doi: 10.1016/j.cgh.2007.01.015. [DOI] [PubMed] [Google Scholar]
- 15.Nguyen GC, Tuskey A, Dassopoulos T, et al. Rising hospitalization rates for inflammatory bowel disease in the United States between 1998 and 2004. Inflamm Bowel Dis. 2007;13:1529–1535. doi: 10.1002/ibd.20250. [DOI] [PubMed] [Google Scholar]
- 16.Marrie RA, Garland A, Peschken CA, et al. Increased incidence of critical illness among patients with inflammatory bowel disease: a population-based study. Clin Gastroenterol Hepatol. 2014;12:2063–2070. e4. doi: 10.1016/j.cgh.2014.03.033. [DOI] [PubMed] [Google Scholar]
- 17.Hazratjee N, Agito M, Lopez R, et al. Hospital readmissions in patients with inflammatory bowel disease. Am J Gastroenterol. 2013;108:1024–1032. doi: 10.1038/ajg.2012.343. [DOI] [PubMed] [Google Scholar]
- 18.Panara AJ, Yarur AJ, Rieders B, et al. The incidence and risk factors for developing depression after being diagnosed with inflammatory bowel disease: a cohort study. Aliment Pharmacol Ther. 2014;39:802–810. doi: 10.1111/apt.12669. [DOI] [PubMed] [Google Scholar]
- 19.McCombie AM, Mulder RT, Gearry RB. Psychotherapy for inflammatory bowel disease: a review and update. J Crohns Colitis. 2013;7:935–949. doi: 10.1016/j.crohns.2013.02.004. [DOI] [PubMed] [Google Scholar]
- 20.Long MD, Barnes EL, Herfarth HH, et al. Narcotic use for inflammatory bowel disease and risk factors during hospitalization. Inflamm Bowel Dis. 2012;18:869–876. doi: 10.1002/ibd.21806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nguyen GC, Chong CA, Chong RY. National estimates of the burden of inflammatory bowel disease among racial and ethnic groups in the United States. J Crohns Colitis. 2014;8:288–295. doi: 10.1016/j.crohns.2013.09.001. [DOI] [PubMed] [Google Scholar]