Abstract
Systemic lupus erythematosus (SLE) is characterized by the second highest prevalence of pulmonary arterial hypertension (PAH), after systemic sclerosis, among the connective tissue diseases. SLE-associated PAH is hemodynamically defined by increased mean pulmonary artery pressure at rest (≥25 mmHg) with normal pulmonary capillary wedge pressure (≤15 mmHg) and increased pulmonary vascular resistance. Estimated prevalence ranges from 0.5% to 17.5% depending on the diagnostic method used and the threshold of right ventricular systolic pressure in studies using transthoracic echocardiogram. Its pathogenesis is multifactorial with vasoconstriction, due to imbalance of vasoactive mediators, leading to hypoxia and impaired vascular remodeling, collagen deposition, and thrombosis of the pulmonary circulation. Multiple predictive factors have been recognized, such as Raynaud’s phenomenon, pleuritis, pericarditis, anti-ribonuclear protein, and antiphospholipid antibodies. Secure diagnosis is based on right heart catheterization, although transthoracic echocardiogram has been shown to be reliable for patient screening and follow-up. Data on treatment mostly come from uncontrolled observational studies and consist of immunosuppressive drugs, mainly corticosteroids and cyclophosphamide, as well as PAH-targeted approaches with endothelin receptor antagonists (bosentan), phosphodiesterase type 5 inhibitors (sildenafil), and vasodilators (epoprostenol). Prognosis is significantly affected, with 1- and 5-year survival estimated at 88% and 68%, respectively.
Keywords: systemic lupus erythematosus, pulmonary arterial hypertension, immunosuppressive, transthoracic echocardiogram, endothelin receptor antagonists
Introduction
Pulmonary arterial hypertension (PAH) is classified into five distinct categories according to etiology.1 Group 1 PAH may be idiopathic, heritable, or drug or toxin induced, or it could be associated with human immunodeficiency virus, schistosomiasis, portal hypertension, and congenital heart disease as well as with connective tissue diseases (CTDs). PAH related to left heart diseases is classified in group 2, lung diseases in group 3, chronic thromboembolic pulmonary hypertension in group 4, while other, less well-known causes are included in group 5. CTD-associated PAH is hemodynamically defined by increased mean pulmonary artery pressure at rest (mPAP ≥25 mmHg), with normal pulmonary capillary wedge pressure (PCWP ≤15 mmHg) and increased pulmonary vascular resistance (PVR).2 Systemic lupus erythematosus (SLE) is characterized by the second highest prevalence of PAH, after systemic sclerosis, according to the REVEAL registry (Registry to Evaluate Early and Long-term Pulmonary Arterial Hypertension disease management), a 55-center longitudinal US-based registry with nearly 3,500 patients.3 The aim of this review is to present the current knowledge on the epidemiology, pathophysiology, diagnosis and treatment of SLE-associated PAH (SLE-PAH).
Epidemiology
The annual incidence of systemic-autoimmune-disease-associated PAH has been estimated to be between one and three cases per million population, with a prevalence ranging from 5 to 15 cases per million.4,5 Cohort studies have reported that PAH prevalence in SLE varies widely between 0.5% and 43%,6–8 although more recent reports estimate this as being between 0.5% and 17.5%.9 Other investigators estimated the prevalence of PAH to be 14% based on the first transthoracic echocardiogram (TTE) of lupus patients.10 The differences are mainly attributed to the method used for diagnosis (TTE vs right heart catheterization, RHC), the threshold for PAH (right ventricular systolic pressure, RVSP >30 mmHg or >40 mmHg), and the studied population.
The majority of patients with SLE-PAH are women (95% in the REVEAL registry with RHC confirmed disease) with a mean age of 45 years (45.5±11.9) at PAH diagnosis.11 In rare cases, PAH is the first manifestation leading to SLE diagnosis.12 Concerning severity, this is usually moderate with pulmonary artery systolic pressure (PASP) ranging between 40 and 60 mmHg and PVR between 5 and 15 Wood units.11,13
Predictive factors
Certain lupus manifestations and immunologic abnormalities have been identified as predictors of PAH in observational cohort studies. In this context, Raynaud’s phenomenon, active renal disease, and vasculitic manifestations (digital gangrene, cutaneous vasculitis, and livedo reticularis) were shown to independently predict PAH development.14,15 In another small prospective study with 34 patients, Raynaud’s phenomenon was strongly related to increased PASP as assessed by TTE.16 Pleural effusions were also demonstrated to occur with higher frequency in CTD-associated PAH; patients with pleural effusions had higher mean right atrial pressure (mRAP) and lower cardiac output.17 However, most patients in that study had overt right heart failure, which may have contributed to pleural effusion. In a recent analysis of a large Chinese cohort (n=1,934, 74 patients with PAH), pleuritis was an independent predictor of PAH in lupus and showed an odds ratio (OR) =3.06 (95% confidence interval [CI] =1.6–5.85).18 Additional clinical manifestations with an independent predictive ability for PAH were interstitial lung disease (OR =17, 95% CI =3.6–80) and pericardial effusion (OR =21.3, 95% CI =4.1–110.6).13 In the same study, it was shown that, paradoxically, lupus patients with PAH had less severe disease, as assessed by the SLE Disease Activity Index (SLEDAI); actually, a SLEDAI ≤9 was strongly predictive of PAH with an OR =26.4 (95% CI =6.6–105.5).13 Moreover, the lack of acute rash and low erythrocyte sedimentation rate (≤20 mm/h) were also independent predictors. The clinical significance of these findings is difficult to interpret since it is believed that systemic inflammation drives PAH in these patients.18
Immunological variables associated with PAH in lupus patients include positive anti-U1-RNP (ribonuclear protein) and antiphospholipid antibodies.13 Anti-U1-RNP antibodies, in particular, were strong predictors for PAH in several studies with a hazard ratio ranging from 2.6 to 12.4 (95% CI =3.6–42.9).12,13,18 Antiphospholipid antibodies, mainly anticardiolipin antibodies and lupus anticoagulant, were also associated with increased risk for PAH.6,13,19 Recently, anti-Sjogren’s Syndrome related antigen A antibodies were demonstrated as strong predictors with an OR =4.8 (95% CI =1.7–14).13 Details on the predictive factors for PAH in lupus patients are given in Table 1.
Table 1.
Independent predictors of PAH in SLE
| Variable | Patients (n) | Hazard ratio | 95% CI | Reference |
|---|---|---|---|---|
| Disease duration | 111 | 1.12 | 1.03–1.21 | Huang et al13 |
| Raynaud’s phenomenon | 41 | 3.204 | 1.291–7.949 | Lian et al14 |
| Pleuritis | 74 | 3.061 | 1.602–5.85 | Li et al18 |
| Pericarditis | 111 | 21.3 | 4.1–110.6 | Huang et al13 |
| 74 | 4.248 | 2.261–7.98 | Li et al18 | |
| Interstitial lung disease | 111 | 17.03 | 3.6–80 | Huang et al13 |
| Anti-RNP antibodies | 111 | 12.4 | 3.6–42.9 | Huang et al13 |
| 74 | 2.559 | 1.312–4.993 | Li et al18 | |
| 41 | 5.393 | 2.073–14.028 | Lian et al14 | |
| Anti-SSA/Ro antibodies | 111 | 4.84 | 1.7–14 | Huang et al13 |
| Anticardiolipin antibodies | 41 | 3.753 | 1.532–9.197 | Lian et al14 |
Abbreviations: CI, confidence interval; PAH, pulmonary arterial hypertension; RNP, ribonuclear protein; SLE, systemic lupus erythematosus; SSA/Ro, Sjogren’s Syndrome related antigen A.
Pathogenesis
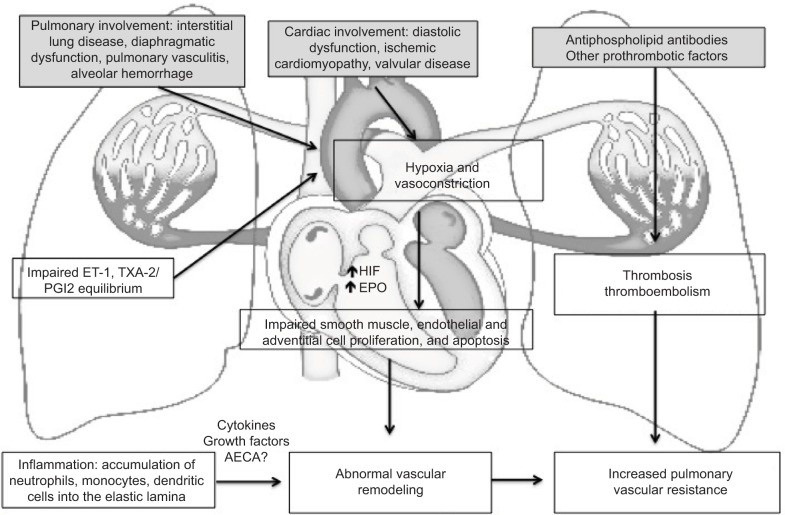
The pathogenetic mechanisms in SLE-PAH have not been elucidated yet. However, accumulating evidence suggests that multiple factors, such as genetic predisposition, environmental stimuli, and immune system dysfunction play a significant role.15 The net result is an imbalance between vasoconstrictive and vasodilating soluble mediators, which leads to vasoconstriction with increased PVR.20 Endothelin-1 (ET-1) and thromboxane A2 (TXA-2) are the main mediators that lead to vasoconstriction; their serum levels were significantly elevated in patients with SLE-PAH and correlated with PAH severity.21,22 In addition, about 42% of patients with SLE-PAH were found to have antibodies against the endothelin receptor type A; their titers correlated strongly with PASP.23 These antibodies promote endothelial dysfunction and probably contribute to the inhibition of prostacyclin production by endothelial cells, which is one of the main vasodilators.15,20 In line with the vasoconstriction theory, it was recently demonstrated that lupus patients with PAH have increased arterial stiffness (assessed by brachial–ankle pulse wave velocity), and this was an independent predictor of PAH.24 Vasoconstriction represents an early event in the PAH pathogenic cascade, and vasoresponders (patients with a >10 mmHg decrease in PASP upon inhalation of vasoactive compounds during RHC) have a good response to calcium channel blockers, regardless of PAH etiology.25,26
Pulmonary vasoconstriction will lead to decreased oxygen saturation and hyperexpression of the hypoxia-inducible factor (HIF) and erythropoietin (EPO), which may promote smooth muscle cell proliferation and extensive vascular remodeling.20,27 Several distinct pathways are implicated in vascular remodeling such as impaired apoptosis with upregulation of antiapoptotic proteins and abnormal proliferation of endothelial and adventitial cells.15,20 In parallel, the inflammatory response will drive the accumulation of monocytes, neutrophils, mast cells, and dendritic cells into the elastic lamina, which in turn induce the production of certain chemokines, cytokines, and growth factors that perpetuate abnormal remodeling.28 In later stages of PAH, microthrombi in the pulmonary vasculature will lead to further elevation of PASP.20
In the aforementioned pathogenetic model of PAH, many characteristics of SLE, such as vasculitis, thrombosis, and interstitial pulmonary fibrosis are implicated.15 Pulmonary vasculitis is mediated through immune complexes; both immunoglobulins and complement have been demonstrated to deposit on the arterial wall.29 Other pulmonary vascular pathologic findings were similar to those of idiopathic PAH and mainly consisted of plexiform lesions, smooth muscle cell hypertrophy, intimal proliferation, and collagen deposition.15,30 In addition, CTD-associated PAH was characterized by more frequent involvement of pulmonary veins and perivascular inflammatory infiltration.31 Thrombosis occurs more frequently in lupus patients, particularly in the presence of antiphospholipid antibodies. Although antiphospholipid syndrome per se may lead to chronic thromboembolic pulmonary hypertension, antiphospholipid antibodies have been shown to mediate endothelial dysfunction and induce the secretion of adhesion molecules.15 This may also occur in the presence of anti-endothelial cell antibodies – their binding to endothelial cells results in increased production of IL-6 and IL-8.32 The role of other immunological abnormalities in SLE-PAH, such as the decreased numbers of T regulatory cells and the more frequent presence of the anti-U1-RNP antibodies, has not been clarified yet.15,33 A schematic representation of the pathogenesis of PAH in the context of SLE is presented in Figure 1.
Figure 1.
A schematic representation of the pathogenesis of PAH in SLE.
Notes: Pulmonary and cardiac involvement as well as disequilibrium between vasodilators (prostacyclin, PGI2) and vasoconstrictors (ET-1 and, TXA-2) will lead to hypoxia and vasoconstriction. Hyperexpression of HIF and EPO will drive impaired smooth muscle, endothelial, and adventitial cell proliferation and apoptosis. In parallel, the accumulation of inflammatory cells into the elastic lamina of the pulmonary arteries and the secretion of certain cytokines and growth factors will lead to abnormal vascular remodeling, and thus increased PVR. In selected cases, thrombosis of the pulmonary circulation in the presence of antiphospholipid antibodies and other prothrombotic factors, will also contribute to increased PVR and PAH. The role of the anti-endothelial cell antibodies AECA and other immune mediators has not been clarified yet.
Abbreviations: PAH, pulmonary arterial hypertension; SLE, systemic lupus erythematosus; ET-1, endothelin-1; TXA-2, thromboxane A2; HIF, hypoxia-inducible factor; EPO, erythropoietin; PVR, pulmonary vascular resistance; AECA, anti-endothelial cell antibodies.
Clinical presentation and diagnosis
Dyspnea (initially exertional), dry cough, chest pain, exercise intolerance, and fatigue are the cardinal clinical manifestations of PAH. Physical findings may include elevated jugular venous pressure, accentuated S2 cardiac sound, and murmurs indicative of tricuspid and/or pulmonic valve insufficiency. In late stages, right heart failure with liver enlargement due to congestion, ascites, and/or lower limb edema may be seen.
The gold standard for PAH diagnosis is RHC, which precisely assesses PASP, diastolic PAP, PCWP, PVR, and cardiac output.1 Secure diagnosis requires a mean PAP ≥25 mmHg at rest.34 Documentation of all these parameters also allows for rough etiologic characterization of PAH; a PCWP ≤15 mmHg is required to exclude cases of heart failure. However, it was shown that many patients with heart failure and preserved ejection fraction have low PCWP (16–18 mmHg).35 PVR ≥3 Wood units should also be included in the characterization of PAH.34 During the procedure, vasoreactivity can be assessed with the use of nitric oxide, epoprostenol, or adenosine. Most SLE patients are not vasoreactive, and therapy with calcium channel blockers has not proven to be beneficial.15 RHC is not always feasible due to availability and/or procedure-related complications (mild-to-moderate in 1.1%, mortality 0.055%).36
TTE can provide a reliable estimation of the RVSP and tricuspid valve insufficiency.15 RVSP is calculated by the modified Bernoulli equation as RVSP =4v2 + mRAP, where v equals the tricuspid regurgitant jet velocity (a reflection of the right ventricular-to-atrial systolic pressure gradient) and mRAP is estimated from the diameter and respirophasic variability of the inferior vena cava during normal respiration.37 RVSP does not necessarily correlate with the measurement of PASP as obtained with RHC.38 In that study, TTE and RHC provided comparable measurements of PASP (77.2±35 mmHg vs 76.9±21.7 mmHg, respectively). However, TTE was inaccurate (over- or underestimating PASP by >10 mmHg) in 57% of the cases. Other studies showed that the correlation between TTE and RHC was satisfactory, at least for the initial evaluation of such patients.39 Moreover, it was recently demonstrated that two consecutive TTEs with an RVSP ≥40 mmHg were the most accurate predictors for PAH with a sensitivity of 100%, specificity 97%, positive predictive value of 70%, and negative predictive value of 100%.40 In general, TTE is recommended for the initial screening of patients with suspected PAH as well as for the evaluation of response to treatment.34 Of note, TTE may lead to PAH diagnosis in asymptomatic patients, although the threshold used in that study was rather low (RVSP =30 mmHg).41
Additional investigations are warranted for the precise etiologic diagnosis of PAH. High-resolution computed tomography of the thorax will help exclude any concomitant interstitial lung disease, while ventilation/perfusion scan for acute or chronic thromboemboli will rule out chronic thromboembolic pulmonary hypertension.15,34 Rare causes of PAH such as sleep apnea syndrome (assessed by polysomnography), human immunodeficiency virus, schistosomiasis, and portopulmonary hypertension should also be excluded. Pulmonary function tests reveal isolated decreased diffusing capacity for carbon monoxide (DLCO).
Therapeutic approach
Treatment of SLE-PAH should be prompt and aim at PASP normalization in order to maximize survival. Thorough diagnostic evaluation is of utmost importance since patients with no other risk factors (eg, left heart failure, chronic thromboembolic PAH) should be treated accordingly (diuretics, anticoagulants, etc).42 Existing randomized controlled trials have solely assessed the effect of PAH-targeted therapies with endothelin receptor antagonists (bosentan), phosphodiesterase type 5 inhibitors (PDE5 inhibitors, sildenafil), and vasodilators (treprostinil, a synthetic analog of prostacyclin, PGI2).43–45 In these studies, patients with different CTDs, mainly mixed connective tissue disease (MCTD) and systemic scleroderma, were also included, and a subanalysis of the lupus patients was not performed.
Additional data come from observational cohort studies using immunosuppressive therapies that have shown a considerable benefit in such patients. Tanaka et al46 reported a significant reduction of RVSP in seven out of eight patients who received corticosteroids ± cyclophosphamide (CYC) – two patients relapsed and were again treated successfully. Intravenous CYC pulses (dose ranging from 500 mg/month to 1,000 mg/m2/month) were also administered in five cohort studies in conjunction with prednisone (0.5–1 mg/kg/day with slow tapering)47,48 and vasodilators49,50 or PDE5 inhibitors.51 Gonzalez-Lopez et al47 showed that CYC in combination with low doses of prednisone (<15 mg/day) was effective in 16 patients with moderate SLE-PAH as assessed by TTE. In another study with CYC, five out of 12 lupus patients responded and showed improved survival.48 More recent studies demonstrated that the addition of vasodilators and supportive treatment with diuretics and anticoagulants may benefit patients with more severe PAH at diagnosis; in those studies, patients with MCTD were also included.49 Finally, Kommireddy et al51 reported a mean reduction of 16 mmHg in PASP (assessed by TTE) with three intravenous CYC pulses plus oral prednisone and PDE5 inhibitors in 11/24 patients with SLE-PAH. Moreover, rituximab was shown to provide benefit in a refractory case of SLE-PAH,52 while another patient was successfully managed with mycophenolate mofetil and cyclosporine.12 Details on the studies that used immunosuppressive treatment for SLE-PAH are given in Table 2.
Table 2.
Studies with immunosuppressive medications for SLE-PAH
| Reference | Year | N (SLE) | Baseline characteristics | Intervention | Outcome | Notes/side effects | ||
|---|---|---|---|---|---|---|---|---|
| Tanaka et al46 | 2002 | 12 | Age RVSP |
38.3±14.2 years 55.5±10.7 mmHg |
8/12 received corticosteroids and/or CYC | 7/8 responded (significant decrease in RVSP), 2/7 relapsed (treated with corticosteroids plus CYC successfully) | Retrospective, four patients had SLE + SSc overlap syndrome One patient died due to sepsis, one developed hemorrhagic cystitis |
|
| GonzalezLopez et al47 | 2004 | 34 | Age mPASP |
38± 11 years 39±6 mmHg |
IV CYC (500 mg/m2/month × 6 months) n= 16 vs enalapril 10 mg/day for 6 months, n=18 + oral prednisone < 15 mg/day | 1. Significant reduction in PASP in both groups (13 mmHg for CYC, 8 mmHg for enalapril) 2. CYC performed better in moderate PAH (initial PASP >35 mmHg), enalapril was not effective 3. NYHA functional class improved only with CYC |
Randomized controlled trial, PAH defined as RVSP >30 mmHg by TTE Patients on CYC had more infections and gastrointestinal side effects |
|
| Sanchez et al48 | 2006 | 28 (12) | Age mPAP PVR NYHA 6MWD |
29 years 54 mmHg 19 WU II, III 370 m |
IV CYC (600 mg/m2/month ×3 months) + oral prednisone (0.5–1 mg/kg for 4 weeks, then slow tapering) 22/28 |
5/12 SLE patients responded (mPAP decreased from 49±16 to 34±11 mmHg, PVR from 15.6±4 to 10.1 ±4 WU) Responders had improved survival (100% vs 38% at 5 years) |
Patients with MCTD and SSc were also included Two of 28 patients died due to sepsis; minor side effects (leukopenia, thrombocytopenia) were infrequent |
|
| Jais et al49 | 2008 | 23 (13)* | Age mPAP PVR NYHA 6MWD |
IS =9 31 ±10 years 48±12 mmHg 8.6±3.5 WU II, III 347±80 m |
IS+ VD =4 38±9 years 58±10 mmHg 14.3± 1.3 WU III, IV 381 ±71 m |
IV CYC (600 mg/m2/month ×6 months) + oral prednisone (0.5–1 mg/kg for 4 weeks, then slow tapering) + VDs + supportive treatment (diuretics, anticoagulants) | 1. Patients with less severe PAH (NYHA class I or II) may respond to IS alone 2. Patients with more severe disease may benefit from the addition of VDs |
Patients with MCTD were also included in the analysis Only minor side effects (leukopenia, thrombocytopenia) were reported |
| Miyamichi- Yamamoto et al50 | 2011 | 13 (7) | Age mPAP PVR NYHA 6MWD |
42±8 years 39.5±9.2 mmHg 8.75±5.43 WU I, II, III 442±54 m |
IV CYC (500 mg/month ×10 months) + oral prednisone (1 mg/kg for 1 month, then slow tapering) + VDs (more than one could be used in a single patient) | 1. mPAP significantly decreased from 39.5±9.1 to 28.9±11 mmHg 2. PVR: trend for decrease (700±434 to 481 ±418 dynessec/cm5) 3. Improved long-term prognosis |
Analysis for 13 patients with CTDs. Among seven SLE patients, five responded quickly (in months) Two patients developed mild liver dysfunction |
|
| Kommireddy et al51 | 2015 | 24 | Age mPASP NYHA 6MWD |
25.4±8 years 59.3±18.7 mmHg I, II, III, IV 312 m |
IV CYC (500–1,000 mg/m2/month ×3 months) + oral prednisone (0.5–1 mg/kg for 4 weeks, then slow tapering) + PDE5 inhibitors in 20/24 | 11/24 responders PASP reduced from 59.3±18.7 to 43.3±20.9 mmHg at 6 months | Retrospective, PAH defined as RVSP >30 mmHg by TTE 2/24 deaths, one from resistant PAH and one from septic shock | |
Note:
Within the 13 SLE patients of this study, 9 received immunosuppressive treatment and 14 vasodilators.
Abbreviations: IV, intravenous; mPAP, mean pulmonary artery pressure; SLE-PAH, SLE-associated PAH; SLE, systemic lupus erythematosus; PAH, pulmonary arterial hypertension; PDE5, phosphodi-esterase type 5 inhibitors; RVSP, right ventricular systolic pressure; CYC, cyclophosphamide; SSc, systemic sclerosis; PASP, pulmonary artery systolic pressure; mPASP, mean PASP; TTE, transthoracic echocardiogram; PVR, pulmonary vascular resistance; NYHA, New York Heart Association; IS, immunosuppressive; VD, vasodilator; 6MWD, 6-minute walk distance; MCTD, mixed connective tissue disease; WU, Woods units.
Other studies have used only PAH-targeted approaches in SLE-PAH. Robbins et al53 administered intravenous epoprostenol in six patients and observed a significant improvement in PAH hemodynamics and functional class according to the New York Heart Association. Other investigators reported similar results along with better survival in epoprostenol-treated patients.54 Oudiz et al45 showed a favorable hemodynamic response and trend toward improved quality of life in 25 lupus patients with subcutaneous treprostinil, a prostacyclin analog. Endothelin receptor antagonists, particularly bosentan, have been shown to improve functional New York Heart Association class and exercise tolerance (assessed with the 6-minute walk distance) in a randomized, placebo-controlled trial, which included 16 lupus patients, as well as other small observational studies.43,55,56 Moreover, sildenafil in low doses improved PAH hemodynamics and functional capacity after 12 weeks of treatment; in that study, 84 patients with CTD-associated PAH (19 with SLE) were subanalyzed.44 Finally, a randomized, placebo-controlled trial with riociguat, a soluble guanylate cyclase stimulator with vasoactive, antifibrotic, and anti-inflammatory effects, showed favorable results in PAH associated with CTDs.57 In that study, 18 patients with SLE were included; however, specific details for these patients were not provided. Details on the studies that used PAH-targeted therapies for SLE-PAH are given in Table 3.
Table 3.
Studies with PAH-targeted therapy medications for SLE-PAH
| Reference | Year | N (SLE) | Baseline characteristics | Intervention | Outcome | Notes/side effects | |
|---|---|---|---|---|---|---|---|
| Robbins et al53 | 2000 | 6 | Age mPASP PVR NYHA |
26–35 years 57±9 mmHg 14±7 WU III, IV |
IV epoprostenol | Significant improvement in hemodynamics (PAP reduced by 38±21%, PVR reduced by 58±12%), and NYHA functional class from III–IV to I–II for all patients | SLE relapsed in one patient |
| Rubin et al43 | 2002 | 213 (16) | Age mPAP PVR NYHA 6MWD |
49± 16 years 55 ±16 mmHg 12.7±8.5 WU III, IV 330±74 m |
Bosentan | Significant improvement in exercise capacity (6MWD increased by 36 m in cases, decreased by 8 m in controls), NYHA functional class (42% in bosentan group), and time to clinical worsening | Double-blind, placebo-controlled trial No significant differences in side effects between groups |
| Oudiz et al45 | 2004 | 90 (25) | Age mPASP NYHA 6MWD |
54±2 years 52 ±2 mmHg II, III, IV 280±13 m |
SC treprostinil | Improved exercise capacity (6MWD increased by 25 m), dyspnea, hemodynamics (PVR decreased by 4±2 WU), and trend toward improved quality of life | Double-blind, placebo-controlled trial Patients with MCTD and SSc were also included Minor side effects (infusion site pain) only |
| Mok et al56 | 2007 | 4 | Age mPAP PVR NYHA 6MWD |
42±8 years 39.5±9.2 mmHg 8.75±5.43 WU I, II, III 442±54 m |
Bosentan | 6MWD significantly improved in 3 (+24.8 m), 6 (+26.2 m), 9 (+54 m), and 12 (+62.7 m) months | Liver toxicity in one patient, PASP assessed with TTE |
| Badesch et al44 | 2007 | 284(19) | Age mPAP PVR NYHA 6MWD |
53±15 years 47±11 mmHg 10.1 ±5.5 WU II, III, IV 342±76 m |
Sildenafil 20, 40, or 80 mg/d | Patients with CTD-associated PAH had improved exercise capacity (6MWD increased by 42 m in cases and decreased by 13 m in controls), hemodynamics, and NYHA functional class (29%–42% improvement, 5% for placebo) after 12 weeks of treatment with sildenafil 20 mg/day | 12-week double-blind study (SUPER-1) Subgroup analysis of 84 patients with CTD-associated PAH Patients with SSc and other CTDs were also included in the analysis No significant side effects |
| Shirai et al54 | 2013 | 16 (6) | Age mPAP PVR NYHA |
43 ±14 years 56 ±9 mmHg 21 ±9 WU III, IV |
IV epoprostenol | mPAP (26% reduction from baseline), PVR (41% reduction from baseline), and functional class were improved after 6 months. Treated patients had better survival (3-year survival 55% vs 6%) | Patients with MCTD and SSc were also included All patients had treatment-related side effects (headache, flushing, diarrhea) Seven of 16 patients had catheter-related infections and required admission |
Abbreviations: IV, intravenous; PAP, pulmonary artery pressure; mPAP, mean PAP; PAH, pulmonary arterial hypertension; SLE-PAH, SLE-associated PAH; SLE, systemic lupus erythematosus; SC, subcutaneous; SSc, systemic sclerosis; PASP, pulmonary artery systolic pressure; mPASP, mean PASP; PVR, pulmonary vascular resistance; NYHA, New York Heart Association; 6MWD, 6-minute walk distance; CTD, connective tissue disease; MCTD, mixed CTD; TTE, transthoracic echocardiogram; WU, Woods units.
Prognosis
PAH significantly affects survival and quality of life in CTDs.58 Direct comparisons from the REVEAL registry showed that patients with CTD-associated PAH had poorer 1-year survival as compared to patients with idiopathic PAH (86% vs 93%).11 Among the CTDs group, however, SLE patients had the best rates for 1-year survival (94% vs 82% for scleroderma and 88% for MCTD), although all patients had comparable hemodynamic characteristics at PAH diagnosis. Data from the Korean CTD-PAH registry, with 174 patients enroled, demonstrated that the 1- and 3-year survival were 90.7% and 87.3%, respectively.59 In that study, low DLCO, diabetes, and pleural effusion were poor prognostic factors, while anti-U1-RNP antibodies seemed to be protective. A recent meta-analysis of six studies encompassing 323 lupus patients with PAH demonstrated that the pooled 1-, 3-, and 5-year survival were 88%, 81%, and 68%, respectively.60 Higher mPAP, PVR, and brain natriuretic peptide and lower 6-minute walk distance were related to poor survival. In an older systematic review of 23 observational studies, higher mPAP at diagnosis, Raynaud’s phenomenon, thrombocytopenia, pregnancy, pulmonary vasculitis, and anticardiolipin antibodies were associated with decreased survival.61
Conclusion
PAH affects 0.5%–17.5% of patients with SLE and has significant effects on prognosis. Its pathogenesis is multifactorial and mediated through vasoconstriction, hypoxia, and impaired vascular remodeling. Immunosuppressive treatment is efficacious in selected cases, while PAH-targeted therapies may provide additional benefit.
Footnotes
Disclosure
The authors report no conflicts of interest in this work.
References
- 1.Simonneau G, Gatzoulis MA, Adatia I, et al. Updated clinical classification of pulmonary hypertension. J Am Coll Cardiol. 2013;62(Suppl 25):D34–D41. doi: 10.1016/j.jacc.2013.10.029. [DOI] [PubMed] [Google Scholar]
- 2.McLaughlin VV, Archer SL, Badesch BD, et al. ACCF/AHA 2009 Expert consensus document on pulmonary hypertension. A report of the American College of Cardiology Foundation Task Force on Expert Consensus documents and the American Heart Association developed in collaboration with the American College of Chest Physicians, American Thoracic Society Inc and the Pulmonary Hypertension Association. J Am Coll Cardiol. 2009;53:1573–1619. doi: 10.1016/j.jacc.2009.01.004. [DOI] [PubMed] [Google Scholar]
- 3.McGoon MD, Miller DP. REVEAL: a contemporary US pulmonary arterial hypertension registry. Eur Respir Rev. 2012;21:8–18. doi: 10.1183/09059180.00008211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peacock AJ, Murphy NE, McMurrey JJ, Caballero L, Stewart S. An epidemiological study of pulmonary arterial hypertension. Eur Respir J. 2007;30:104–109. doi: 10.1183/09031936.00092306. [DOI] [PubMed] [Google Scholar]
- 5.Humbert M, Sitbon O, Chaouat A, et al. Pulmonary arterial hypertension in France: results from a national registry. Am J Resp Crit Care Med. 2006;173:1023–1030. doi: 10.1164/rccm.200510-1668OC. [DOI] [PubMed] [Google Scholar]
- 6.Prabu A, Patel K, Yee CS, et al. Prevalence and risk factors for pulmonary arterial hypertension in patients with lupus. Rheumatology (Oxford) 2009;48:1506–1511. doi: 10.1093/rheumatology/kep203. [DOI] [PubMed] [Google Scholar]
- 7.Simonson JS, Schiller NB, Petri M, Hellmann DB. Pulmonary hypertension in systemic lupus erythematosus. J Rheumatol. 1989;16:918–925. [PubMed] [Google Scholar]
- 8.Winslow TM, Ossinov MA, Fazio GP, Simonson JS, Redberg RF, Schiller NB. Five-year follow-up study of the prevalence and progression of pulmonary hypertension in systemic lupus erythematosus. Am Heart J. 1995;129:510–515. doi: 10.1016/0002-8703(95)90278-3. [DOI] [PubMed] [Google Scholar]
- 9.Arnaud L, Agard C, Haroche J, Cacoub P, Piette JC, Amoura Z. Pulmonary arterial hypertension in systemic lupus erythematosus. Rev Med Interne. 2011;32:689–697. doi: 10.1016/j.revmed.2011.01.002. [DOI] [PubMed] [Google Scholar]
- 10.Johnson SR, Gladman DD, Urowitz MB, Ibanez DD, Granton JT. Pulmonary hypertension in systemic lupus. Lupus. 2004;13:506–509. doi: 10.1191/0961203303lu1051oa. [DOI] [PubMed] [Google Scholar]
- 11.Chung L, Liu J, Parsons L, et al. Characterization of connective tissue disease-associated pulmonary arterial hypertension from REVEAL: identifying systemic sclerosis as a unique phenotype. Chest. 2010;138:1383–1394. doi: 10.1378/chest.10-0260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Prete M, Fatone MC, Vacca A, Racanelli V, Perosa F. Severe pulmonary hypertension as the initial manifestation of systemic lupus erythematosus: a case report and review of the literature. Clin Exp Rheumatol. 2014;32:267–274. [PubMed] [Google Scholar]
- 13.Huang C, Li M, Liu Y, et al. Baseline characteristics and risk factors of pulmonary arterial hypertension in systemic lupus erythematosus patients. Medicine (Baltimore) 2016;95:e2761. doi: 10.1097/MD.0000000000002761. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lian F, Chen D, Wang Y, et al. Clinical features and independent predictors of pulmonary arterial hypertension in systemic lupus erythematosus. Rheumatol Int. 2012;32:1727–1731. doi: 10.1007/s00296-011-1880-4. [DOI] [PubMed] [Google Scholar]
- 15.Dhala A. Pulmonary arterial hypertension in systemic lupus erythematosus: current status and future directions. Clin Dev Immunol. 2012;2012:854941. doi: 10.1155/2012/854941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kasparian A, Floros A, Gialafos E, et al. Raynaud’s phenomenon is correlated with elevated systolic pulmonary arterial pressure in patients with systemic lupus erythematosus. Lupus. 2007;16:505–508. doi: 10.1177/0961203307080629. [DOI] [PubMed] [Google Scholar]
- 17.Luo YE, Robbins IM, Karatas M, Brixey AG, Rice TW, Light RW. Frequency of pleural effusions in patients with pulmonary arterial hypertension associated with connective tissue diseases. Chest. 2011;140:42–47. doi: 10.1378/chest.10-0227. [DOI] [PubMed] [Google Scholar]
- 18.Li M, Wang Q, Zhao J, et al. Chinese SLE Treatment and Research Group (CSTAR) registry: II. Prevalence and risk factors of pulmonary arterial hypertension in Chinese patients with systemic lupus erythematosus. Lupus. 2014;23:1085–1091. doi: 10.1177/0961203314527366. [DOI] [PubMed] [Google Scholar]
- 19.Xia YK, Tu SH, Hu YH, et al. Pulmonary hypertension in systemic lupus erythematosus: a systematic review and analysis of 642 cases in Chinese population. Rheumatol Int. 2013;33:1211–1217. doi: 10.1007/s00296-012-2525-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Huber LC, Bye H, Brock M, Swiss Society of Pulmonary Hypertension The pathogenesis of pulmonary hypertension-an update. Swiss Med Wkly. 2015;145:w14202. doi: 10.4414/smw.2015.14202. [DOI] [PubMed] [Google Scholar]
- 21.Lai YC, Potoka KC, Champion HC, Mora AL, Gladwin MT. Pulmonary arterial hypertension: the clinical syndrome. Circulation Res. 2014;115:115–130. doi: 10.1161/CIRCRESAHA.115.301146. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shen JY, Chen SL, Wu YX, et al. Pulmonary hypertension in systemic lupus erythematosus. Rheumatology Int. 1999;18:147–151. doi: 10.1007/s002960050074. [DOI] [PubMed] [Google Scholar]
- 23.Guo L, Li M, Chen Y, et al. Anti-endothelin receptor type A autoantibodies in systemic lupus erythematosus-associated pulmonary arterial hypertension. Arthritis Rheumatol. 2015;67:2394–2402. doi: 10.1002/art.39212. [DOI] [PubMed] [Google Scholar]
- 24.Lee JH, Im Cho K. Arterial stiffness, antiphospholipid antibodies and pulmonary arterial hypertension in systemic lupus erythematosus. J Cardiol. 2014;64:450–455. doi: 10.1016/j.jjcc.2014.02.030. [DOI] [PubMed] [Google Scholar]
- 25.Sitbon O. Long-term response to calcium channel blockers in idiopathic pulmonary arterial hypertension. Circulation. 2005;111:3105–3111. doi: 10.1161/CIRCULATIONAHA.104.488486. [DOI] [PubMed] [Google Scholar]
- 26.Montani D, Savale L, Natali D, et al. Long-term response to calcium channel blockers in non-idiopathic pulmonary arterial hypertension. Eur Heart J. 2010;31:1898–1907. doi: 10.1093/eurheartj/ehq170. [DOI] [PubMed] [Google Scholar]
- 27.Karamanian VA, Harhay M, Grant GR, et al. Erythropoietin up-regulation in pulmonary arterial hypertension. Pulm Circ. 2014;4:269–279. doi: 10.1086/675990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Pullamsetti SS, Savai R, Janssen W, et al. Inflammation, immunological reaction and role of infection in pulmonary hypertension. Clin Microbiol Infect. 2011;17:7–14. doi: 10.1111/j.1469-0691.2010.03285.x. [DOI] [PubMed] [Google Scholar]
- 29.Sasaki N, Kamataki A, Sawai T. A histopathological study of pulmonary hypertension in connective tissue diseases. Allergol Int. 2011;60:411–417. doi: 10.2332/allergolint.11-RAI-0337. [DOI] [PubMed] [Google Scholar]
- 30.Roncoroni AJ, Alvarez C, Molinas F. Plexogenic arteriopathy associated with pulmonary vasculitis in systemic lupus erythematosus. Respiration. 1992;59:52–56. doi: 10.1159/000196025. [DOI] [PubMed] [Google Scholar]
- 31.Dorfmuller P, Humbert M, Perros F, et al. Fibrous remodelling of the pulmonary venous system in pulmonary arterial hypertension associated with connective tissue diseases. Hum Pathol. 2007;38:893–902. doi: 10.1016/j.humpath.2006.11.022. [DOI] [PubMed] [Google Scholar]
- 32.Arends SJ, Damoiseaux JG, Duijvestijn AM, et al. Functional implications of IgG anti-endothelial cell antibodies in pulmonary arterial hypertension. Autoimmunity. 2013;46:463–470. doi: 10.3109/08916934.2013.812080. [DOI] [PubMed] [Google Scholar]
- 33.Nicolls MR, Taraseviciene-Stewart L, Rai PR, Badesch DB, Voelkel NF. Autoimmunity and pulmonary hypertension: a perspective. Eur Respir J. 2005;26:1110–1118. doi: 10.1183/09031936.05.00045705. [DOI] [PubMed] [Google Scholar]
- 34.Hoeper MM, Bogaard HJ, Condliffe R, et al. Definitions and diagnosis of pulmonary hypertension. J Am Coll Cardiol. 2013;62(Suppl 25):D42–D50. doi: 10.1016/j.jacc.2013.10.032. [DOI] [PubMed] [Google Scholar]
- 35.Frost AE, Farber HW, Barst RJ, Miller DP, Elliott CG, McGoon MD. Demographics and outcomes of patients diagnosed with pulmonary hypertension with pulmonary capillary wedge pressures 16 to 18 mmHg: insights from the REVEAL registry. Chest. 2013;143:185–195. doi: 10.1378/chest.11-1387. [DOI] [PubMed] [Google Scholar]
- 36.Hoeper MM, Lee SH, Voswinckel R, et al. Complications of right heart catheterization procedures in patients with pulmonary hypertension in experienced centres. J Am Coll Cardiol. 2006;48:2546–2552. doi: 10.1016/j.jacc.2006.07.061. [DOI] [PubMed] [Google Scholar]
- 37.Kircher BJ, Himelman RB, Schiller NB. Noninvasive estimation of right atrial pressure from the inspiratory collapse of the inferior vena cava. Am J Cardiol. 1990;66:493–496. doi: 10.1016/0002-9149(90)90711-9. [DOI] [PubMed] [Google Scholar]
- 38.Farber HW, Foreman AJ, Miller DP, Mcgoon MD. REVEAL Registry: correlation of right heart catheterization and echocardiography in patients with pulmonary arterial hypertension. Congest Heart Fail. 2011;17:56–64. doi: 10.1111/j.1751-7133.2010.00202.x. [DOI] [PubMed] [Google Scholar]
- 39.Rich JD, Shah SJ, Swamy RS, Kamp A, Rich S. Inaccuracy of Doppler echocardiographic estimates of pulmonary artery pressures in patients with pulmonary hypertension: implications for clinical practice. Chest. 2011;139:988–993. doi: 10.1378/chest.10-1269. [DOI] [PubMed] [Google Scholar]
- 40.Ruiz-Irastorza G, Garmendia M, Villar I, Egurbide MV, Aguirre C. Pulmonary hypertension in systemic lupus erythematosus: prevalence, predictors and diagnostic strategy. Autoimmun Rev. 2013;12:410–415. doi: 10.1016/j.autrev.2012.07.010. [DOI] [PubMed] [Google Scholar]
- 41.Kamel SR, Omar GM, Darwish AF, Asklany HT, Ellabban AS. Asymptomatic pulmonary hypertension in systemic lupus erythematosus. Clin Med Insights Arthritis Musculoskelet Disord. 2011;4:77–86. doi: 10.4137/CMAMD.S7667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Akdogan A, Kilic L, Dogan I, et al. Pulmonary hypertension in systemic lupus erythematosus: pulmonary thromboembolism is the leading cause. J Clin Rheumatol. 2013;19:421–425. doi: 10.1097/RHU.0000000000000037. [DOI] [PubMed] [Google Scholar]
- 43.Rubin LJ, Badesch DB, Barst RJ, et al. Bosentan therapy for pulmonary arterial hypertension. N Engl J Med. 2002;346:896–903. doi: 10.1056/NEJMoa012212. [DOI] [PubMed] [Google Scholar]
- 44.Badesch DB, Hill NS, Burgess G, et al. Sildenafil for pulmonary arterial hypertension associated with connective tissue diseases. J Rheumatol. 2007;34:2417–2422. [PubMed] [Google Scholar]
- 45.Oudiz RJ, Schilz RJ, Barst RJ, et al. Treprostinil, a prostacyclin analogue, in pulmonary arterial hypertension associated with connective tissues disease. Chest. 2004;126:420–427. doi: 10.1378/chest.126.2.420. [DOI] [PubMed] [Google Scholar]
- 46.Tanaka E, Harigai M, Tanaka M, Kawaguchi Y, Hara M, Kamatani M. Pulmonary hypertension in systemic lupus erythematosus: evaluation of clinical characteristics and response to immunosuppressive treatment. J Rheumatol. 2002;29:282–287. [PubMed] [Google Scholar]
- 47.Gonzalez-Lopez L, Cardona-Munoz EG, Celis A, et al. Therapy with intermittent pulse cyclophosphamide for pulmonary hypertension associated with systemic lupus erythematosus. Lupus. 2004;13:105–112. doi: 10.1191/0961203304lu509oa. [DOI] [PubMed] [Google Scholar]
- 48.Sanchez O, Sitbon O, Jais X, Simonneau G, Humbert M. Immunosuppressive therapy in connective tissue diseases-associated pulmonary arterial hypertension. Chest. 2006;130:182–189. doi: 10.1378/chest.130.1.182. [DOI] [PubMed] [Google Scholar]
- 49.Jais X, Launay D, Yaici A, et al. Immunosuppressive therapy in lupus-and mixed connective tissue disease-associated pulmonary arterial hypertension: a retrospective analysis of twenty-three cases. Arthritis Rheum. 2008;58:521–531. doi: 10.1002/art.23303. [DOI] [PubMed] [Google Scholar]
- 50.Miyamichi-Yamamoto S, Fukumoto Y, Sugimura K, et al. Intensive immunosuppressive therapy improves pulmonary hemodynamics and long-term prognosis in patients with pulmonary arterial hypertension associated with connective tissue disease. Circ J. 2011;75:2668–2674. doi: 10.1253/circj.cj-11-0473. [DOI] [PubMed] [Google Scholar]
- 51.Kommireddy S, Bhyravavajhala S, Kurimeti K, et al. Pulmonary arterial hypertension in systemic lupus erythematosus may benefit by addition of immunosuppression to vasodilator therapy: an observational study. Rheumatology (Oxford) 2015;54:1673–1679. doi: 10.1093/rheumatology/kev097. [DOI] [PubMed] [Google Scholar]
- 52.Hennigan S, Channick RN, Silverman GJ. Rituximab treatment of pulmonary arterial hypertension associated with systemic lupus erythematosus: a case report. Lupus. 2008;17:754–756. doi: 10.1177/0961203307087610. [DOI] [PubMed] [Google Scholar]
- 53.Robbins IM, Gaine SP, Schilz R, Tapson VE, Rubin LJ, Loyd JE. Epoprostenol for treatment of pulmonary hypertension in patients with systemic lupus erythematosus. Chest. 2000;117:14–18. doi: 10.1378/chest.117.1.14. [DOI] [PubMed] [Google Scholar]
- 54.Shirai Y, Yasuoka H, Takeuchi T, Satoh T, Kuwana M. Intravenous epoprostenol treatment of patients with connective tissue disease and pulmonary arterial hypertension at a single centre. Mod Rheumatol. 2013;23:1211–1220. doi: 10.1007/s10165-012-0828-1. [DOI] [PubMed] [Google Scholar]
- 55.Denton CP, Humbert M, Rubin L, Black CM. Bosentan treatment for pulmonary arterial hypertension related to connective tissue disease: a subgroup analysis of the pivotal clinical trials and their open-label extensions. Ann Rheum Dis. 2006;65:1336–1340. doi: 10.1136/ard.2005.048967. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Mok MY, Tsang PL, Lam YM, Lo Y, Wong WS, Lau CS. Bosentan use in systemic lupus erythematosus patients with pulmonary arterial hypertension. Lupus. 2007;16:279–285. doi: 10.1177/0961203307076509. [DOI] [PubMed] [Google Scholar]
- 57.Humbert M, Coghlan JG, Ghofrani HA, et al. Riociguat for the treatment of pulmonary arterial hypertension associated with connective tissue diseases: results from PATENT-1 and PATENT-2. Ann Rheum Dis. 2016 doi: 10.1136/annrheumdis-2015-209087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wang H, Guo X, Lai J, et al. Predictors of health-related quality of life in patients with systemic lupus erythematosus associated pulmonary arterial hypertension. Clin Exp Rheumatol. 2016;34:291–295. [PubMed] [Google Scholar]
- 59.Kang KY, Jeon CH, Choi SJ, et al. Survival and prognostic factors in patients with connective tissue disease-associated pulmonary hypertension by echocardiography: results from a Korean nationwide registry. Int J Rheum Dis. 2015 doi: 10.1111/1756-185X.12645. [DOI] [PubMed] [Google Scholar]
- 60.Qian J, Wang Y, Huang C, et al. Survival and prognostic factors of systemic lupus erythematosus-associated pulmonary arterial hypertension: a PRISMA-compliant systematic review and meta-analysis. Autoimmun Rev. 2016;15:250–257. doi: 10.1016/j.autrev.2015.11.012. [DOI] [PubMed] [Google Scholar]
- 61.Chow SL, Chandran V, Fazelzad R, Johnson SR. Prognostic factors for survival in systemic lupus erythematosus associated pulmonary hypertension. Lupus. 2012;21:353–364. doi: 10.1177/0961203311429815. [DOI] [PubMed] [Google Scholar]