Abstract
Nonsuicidal self-injury (NSSI) has been defined as deliberately damaging one's body tissue without conscious suicidal intent. NSSI is a robust predictor of suicidal ideation and attempts in adults. While NSSI has been associated with other-directed violence in adolescent populations, the link between NSSI and interpersonal violence in adults is less clear. The current study examined the cross-sectional relationship between NSSI and past-year interpersonal violence among 729 help-seeking veterans with posttraumatic stress disorder (PTSD). Veterans who reported a recent history of engaging in cutting, hitting, or burning themselves were significantly more likely to report making violent threats and engaging in violent acts, including the use of a knife or gun, in the past year than veterans without NSSI. NSSI was uniquely associated with interpersonal violence after controlling for a variety of dispositional, historical, contextual, and clinical risk factors for violence, including age, race, socio-economic status, marital status, employment status, combat exposure, alcohol misuse, depression, PTSD symptom severity, and reported difficulty controlling violence. These findings suggest that clinicians working with veterans with PTSD should review NSSI history when conducting a risk assessment of violence.
Keywords: PTSD, aggression, deliberate self-harm, NSSI, risk assessment
1. Introduction
Nonsuicidal self-injury (NSSI) is defined as deliberately damaging one's body tissue without conscious suicidal intent (Chapman et al., 2006; Kimbrel et al., 2016; Kimbrel et al., 2015; Kimbrel et al., 2014). The most common methods of NSSI include self-burning, self-cutting, self-hitting, and severe scratching (Klonsky, 2011). It is estimated that 6% of the U.S. general population will engage in NSSI at some point in their lifetime (Briere and Gil, 1998; Klonsky, 2011). Although NSSI has historically been viewed as more common among females than males, population-based studies of NSSI have consistently failed to find evidence for sex differences in rates of NSSI among adults (Kimbrel et al., 2016). NSSI has been associated with significantly increased risk of suicidal behavior in military and veteran samples (Bryan et al., 2015; Kimbrel et al., 2016; Kimbrel et al., 2014). Further, high rates of NSSI have been found among treatment seeking, psychiatric populations of veterans (Bryan and Bryan, 2014; Kimbrel et al., 2016; Kimbrel et al., 2015; Kimbrel et al., 2014). Studies of treatment seeking male veterans with posttraumatic stress disorder (PTSD) have documented that as many as 57%-66% have a lifetime history of NSSI (Kimbrel et al., 2016; Kimbrel et al., 2015; Kimbrel et al., 2014; Sacks et al., 2008). Although NSSI is a form of self-directed violence, it may also be associated with increased risk for interpersonal violence (Kleiman et al., 2015; Wolff et al., 2014), however, to date the association between NSSI and interpersonal violence has not been studied among veterans with PTSD.
PTSD has been shown to be associated with anger, aggressiveness, and interpersonal violence (Calhoun et al., 2002; Crawford et al., 2007). Help-seeking male veterans with PTSD are more likely to exhibit violence and report problems with violent behavior than help-seeking veterans without PTSD (Beckham et al., 1997; Elbogen et al., 2010b; Freeman and Roca, 2001). A recent study of U.S. Iraq and Afghanistan era veterans indicated that 67% reported that they had threatened someone or engaged in other types of aggressive behavior in the past month (Wright et al., 2012). Thus, it is critically important that the potential for aggression and violence in veterans with PTSD be systematically evaluated. Approaches to the assessment of violence potential in veterans have called for the application of empirically-supported models that examine dispositional factors (e.g., younger age), historical factors (e.g., combat exposure, past violent behavior), contextual factors (e.g., unemployment), and clinical factors such as PTSD, depression, and substance abuse (Elbogen et al., 2010a).
From this perspective, given that NSSI is associated with PTSD in veterans, which in turn has been shown to be related to elevated violence risk (Elbogen et al., 2010a), NSSI itself may be an important clinical factor to examine with respect to interpersonal violence. Indeed, several studies have indicated that NSSI is positively associated with aggression in adolescents in both community (Brunner et al., 2007; Fliege et al., 2009; Sourander et al., 2006) and psychiatric settings (Boxer, 2010; Vivona et al., 1995). To date, no studies have examined the association between NSSI and interpersonal violence in a veteran population.
The objective of the current study was to examine the association between NSSI and interpersonal violence in help-seeking male veterans with PTSD. We hypothesized that NSSI would be positively associated with aggression and reports of interpersonal violence. In order to examine whether NSSI might be an important clinical factor associated with identifying other-directed violence, the second objective of the present study was to examine whether NSSI was uniquely related to interpersonal violence after accounting for well-established dispositional, historical, contextual and clinical risk factors associated with violence including: age, race, marital status, unemployment, socioeconomic status (SES), combat exposure, PTSD symptom severity, depression, alcohol misuse, and reported difficulty controlling violence (Elbogen et al., 2010a). Given previous work documenting differential associations between NSSI and suicide as a function of NSSI severity (Kimbrel et al., 2014), we explored potential differences in the association between NSSI and violence among those who engaged in less severe forms of NSSI (e.g., only scratching/picking) and more severe NSSI (e.g., cutting/hitting/burning oneself).
2. Method
2.1 Participants and procedure
The study sample was drawn from an archival dataset that included 729 male, help-seeking veterans with PTSD who were evaluated at an outpatient Veterans Affairs (VA) specialty PTSD clinic from 2000-2014, who completed the measures described below. Veterans completed a structured clinical interview and a battery of self-report measures as part of their standard diagnostic procedure. PTSD diagnosis was based on the Clinician-Administered PTSD Scale [CAPS; (Blake et al., 1995)] following Diagnostic and Statistical Manual of Mental Disorders [(4th ed., text rev.; DSM-IV_TR; (American Psychiatric Association, 2000)] criteria. IRB approval for use of these data for research purposes was obtained. The association between deliberate self-harm and levels of PTSD and impulsivity (Sacks et al., 2008) and suicidal ideation (Kimbrel et al., 2014) has been previously described for a portion of the sample. Demographic characteristics of the sample are described in Table 1. The sample was predominately African-American (52%) and Caucasian (43%). The majority of the sample were Vietnam veterans (59%); 21% of the sample served during the recent wars in Afghanistan and Iraq. On average, participants were 48 years old (SD = 12.3).
Table 1.
Sample Demographics and Clinical Characteristics of Help-Seeking Veterans with PTSD with past-year Non-suicidal self-injury (NSSI)
| Full Sample N = 729 | Positive for NSSI n = 366 | Negative for NSSI n = 363 | |||||
|---|---|---|---|---|---|---|---|
| Characteristic | n | (%) | n | (%) | n | (%) | p-value |
| Race | n.s. | ||||||
| African-American/Black | 377 | (52) | 200 | (53) | 177 | (47) | |
| Caucasian/White | 310 | (43) | 142 | (46) | 168 | (54) | |
| Other | 42 | (6) | 24 | (57) | 18 | (43) | |
| Era | n.s. | ||||||
| Vietnam | 430 | (59) | 232 | (54) | 198 | (46) | |
| Gulf War | 68 | (9) | 33 | (49) | 35 | (51) | |
| OEF/OIF | 153 | (21) | 67 | (44) | 86 | (56) | |
| Other | 78 | (11) | 34 | (44) | 44 | (56) | |
| Marital Status | .014 | ||||||
| Unmarried | 314 | (43) | 174 | (55) | 140 | (45) | |
| Married | 415 | (57) | 192 | (46) | 223 | (54) | |
| Currently Working | n.s. | ||||||
| No | 368 | (50) | 193 | (52) | 175 | (48) | |
| Yes, Part time | 72 | (10) | 41 | (57) | 31 | (43) | |
| Yes, Full time | 289 | (40) | 132 | (46) | 157 | (54) | |
| Major Depression | .016 | ||||||
| No | 260 | (36) | 115 | (44) | 145 | (56) | |
| Yes | 469 | (64) | 251 | (53) | 218 | (47) | |
| m | (sd) | m | (sd) | m | (sd) | ||
|---|---|---|---|---|---|---|---|
| Age | 48.74 | (11.98) | 49.20 | (11.81) | 48.27 | (12.16) | n.s. |
| SES (Hollingshead) | 56.95 | (11.57) | 57.74 | (10.89) | 56.16 | (12.19) | n.s. |
| Combat Exposure (CES) | 20.23 | (11.07) | 20.24 | (11.00) | 20.20 | (11.16) | n.s. |
| PTSD Severity (CAPS) | 80.62 | (19.79) | 82.78 | (19.40) | 78.44 | (19.98) | .003 |
| Alcohol Misuse (AUDIT) | 8.64 | (9.77) | 9.27 | (10.03) | 8.01 | (9.46) | n.s. |
Note. SES=Socioeconomic Status; Hollingshead=Hollingshead Index of Social Position; CES=Combat Exposure Scale; CAPS = Clinician Administered PTSD Scale; AUDIT=Alcohol Use Disorders Identification Test;
2.2 Measures
2.2.1 Non-Suicidal Self Injury
The Habit Questionnaire [HQ: (Resnick and Weaver, 1994)] is an 11-item self-report measure that assesses NSSI and body-focused repetitive behavior. NSSI was assessed using the 4-item deliberate self-harm subscale (Kimbrel et al., 2014; Sacks et al., 2008) which has demonstrated validity (Kimbrel et al., 2014; Sacks et al., 2008). NSSI is assessed with the following items: (1) “Have you ever scratched or picked at your skin so that it left a mark?” (2) Have you ever deliberately cut yourself in any way?” (3) “Have you ever hit yourself?” and (4) “Have you burned yourself with a cigarette, match, or other way?” Participants who reported engaging in any of these behaviors during the previous two weeks were considered to have current NSSI.
2.2.2. Violence
The Conflict Tactics Scale [CTS; Form N; (Straus, 1979)] is a widely used 20-item measure of interpersonal violence with demonstrated reliability and validity (Straus, 1989; Straus, 1979, 1990). CTS items were used to identify the proportion of patients who endorsed engaging in threats of violence, minor violence, and severe violence following previously established methods [e.g., (McFall et al., 1999; Straus, 1979)]. Threats included “Threatening to hit or throw something at the other person”. Minor violence included the items: “Threw something at the other person”; “Pushed, grabbed, or shoved the other person” and “Slapped a person”. Severe violence included the items: “Kicked, bit, or hit with a fist”; “Beat up the other person”; “Threatened the other person with a knife or gun” and “Used a knife or gun”. Weapon related violence was defined as violent threats with a knife or gun or the use of a knife or gun. Items are rated for occurrence in the past year on a scale ranging from 0 (never), 1 (once), 2 (twice), 3 (3 to 5 times), 4 (6 to 10 times), 5 (11 to 20 times), to 6 (more than 20 times). In order to examine the proportion of the sample engaging in each violence domain, scores were transformed to dichotomous indicators, where 0 = never and 1 = one or more occurrences of the index behavior. Additionally, a total measure of the count of violent acts (i.e., minor and severe violence) committed in the past year was scored by assigning the mid-points of the latter four response categories and summing the items (Straus, 1979). Following previous research using the CTS with veterans (Crawford et al., 2007; Jordan et al., 1992; Van Voorhees et al., 2014), high violence was defined as 13 or more violent acts in the past year. Internal consistency of these scoring methods is adequate [alpha .79-.83; (Straus, 1979, 1990)].
2.2.4 Demographic information
Demographic information included age, race, socioeconomic status (SES) based on the Hollingshead Index of Social Status (Hollingshead and Redlich, 1958), employment status, and marital status.
2.2.5. Combat exposure
Combat exposure was measured with the Combat Exposure Scale [CES: (Keane et al., 1989)] a well-validated 7-item scale measuring exposure to combat-related traumatic experiences. This measure has excellent psychometric properties including reliability and temporal stability (Keane et al., 1989).
2.2.6. PTSD and Depression
The Clinician-Administered PTSD Scale (CAPS) is a structured clinical interview that assesses DSM-IV PTSD symptom frequency and intensity and is considered to be the “gold-standard” for PTSD assessment (Weathers et al., 2001; Weathers et al., 2004). For diagnostic purposes, a PTSD symptom was considered present on the CAPS based on a rule of frequency > 1 and severity > 2 (Blake et al., 1995). The CAPS was administered or directly supervised by a licensed clinical psychologist. Fleiss’ kappa among interviewers in the clinic across a series of 5 training tapes was .94. PTSD symptom severity was measured as the total CAPS score (Weathers et al., 2001). The presence of major depression was assessed using the Major Depressive Disorder Module of the Structured Clinical Interview for DSM-IV [SCID; (First et al., 1994)].
2.2.7. Alcohol misuse
The Alcohol Use Disorders Identification Test [AUDIT; (Saunders et al., 1993)] is a ten-item measure assessing three factors: alcohol consumption, alcohol dependence, and adverse consequences of alcohol use. The range of possible scores is 0-40 with higher scores indicating increased probability of an alcohol use disorder. The AUDIT has been found to have high test-retest reliability (r = .86) and a high level of agreement with other measures of alcohol use disorders (Babor et al., 2001).
2.2.8. Recent history of violence
A single item was used to assess recent history of difficulty controlling violent behavior, “During the past thirty days, have you had trouble controlling violent behavior (that is, hitting someone)?” [see e.g., (Crawford et al., 2007; McFall et al., 1999)].
2.3. Analytic strategy
Bivariate analyses examined the association of any NSSI with demographic and clinical variables. The association between violence and NSSI was examined where NSSI was coded as a three group variable including 1) no NSSI, 2) scratching/picking only, and 3) any cutting, hitting, or burning. In order to examine the incremental utility of NSSI as a predictor of violence, multivariable models were run that included dispositional, historical, contextual and clinical factors associated with violence (Elbogen et al., 2010b) including a simple yes-no admission of difficulty controlling violent behavior in the past 30 days. Logistic regression was used to examine the proportion of patients reporting making threats, engaging in any minor violence, and engaging in any severe violence. Because weapon related violence is particularly dangerous, we further evaluated severe violence by examining the proportion of patients who endorsed making violent threats with a weapon as well as those who endorsed violence using a knife or gun. Logistic regression was also used to examine the association between NSSI and high levels of violence (i.e., reporting 13 or more violent acts). All models were adjusted for age, race (minority vs. White), marital status (unmarried vs. married), employment status (unemployed vs. working full or part time), SES (Hollingshead Index), alcohol misuse (AUDIT total score), presence of major depression, PTSD symptom severity (CAPS total score) and reported difficulty controlling violence.
The total number of violent acts in the past year was modeled with negative binomial regression and zero-inflated negative binomial regression. Negative binomial regression is appropriate for the analysis of highly skewed and overdispersed (i.e., with variance greater than the mean) count data such as the number of violent acts in the past year (Elhai et al., 2008). Zero-inflated negative binomial (ZINB) models account for excessive zero responses. The Vuong test (macro available at http://support.sas.com/kb/42/514.html) was used to compare model fit between the negative-binomial regression model and the ZINB model (Elhai et al., 2008). As in Poisson regression analysis, each negative binomial regression coefficient, when exponentiated, is an estimate of the incidence rate ratio, e.g., the ratio of the incidence of violent acts in the NSSI positive group to that in the NSSI negative group (Elhai et al., 2008). All statistical analyses were performed with SAS PC, Version 9.4 (SAS Inc.., Cary NC).
3. Results
3.1. Rates of NSSI and Violence among Help-Seeking Veterans
High levels of combat exposure and PTSD symptoms were present in the sample of male, help-seeking veterans with PTSD (see Table 1). Rates of violence were also highly prevalent in the sample. The majority of the sample of veterans with PTSD (64%, n=473) reported making violent threats at least once in the past year. Almost half of the sample (49%, n=355) reported engaging in minor violence (e.g., pushing, shoving, slapping someone). Forty-four percent (n=320) engaged in one or more forms of severe violence with 24% (n=177) making violent threats with a weapon and 18% (n=131) using a knife or gun. In total, 57% (n=414) of the sample reported engaging in either minor or major violence. The majority (74%; n=261) of those who engaged in any minor violence also engaged in any major violence.
Half of the sample (50%, n=366) endorsed one or more behaviors indicative of current NSSI. Approximately, five percent of the sample (n=36) endorsed self-cutting, 8% (n=55) endorsed self-burning, 19% (n=138) endorsed self-hitting, and 40% (n=289) endorsed severe scratching or picking at skin. Those who endorsed any NSSI did not differ in age, race, service era, SES, or combat exposure from those who did not report NSSI. Veterans with PTSD who endorsed NSSI, however, were less likely to be currently married. Reporting behaviors representative of NSSI was significantly associated with depression and more severe PTSD symptoms (see Table 1).
Of those who engaged in any form of NSSI, 31% (n=112) engaged in multiple NSSI behaviors. The most common NSSI behavior, severe scratching or picking at the skin, was the behavior most likely to be done in isolation from other NSSI behaviors. Seventy-five percent (n=188) of those who reported only one NSSI behavior (n=254) engaged only in scratching/picking. In contrast, it was much less common to engage only in cutting (1%, n=3), hitting only (18%, n=46) or burning only (7%, n=17). Contrasts comparing veterans who endorsed scratching/picking only to veterans that engaged in other forms of NSSI, indicated that those engaging in cutting, hitting or burning behaviors had higher PTSD symptom severity [mean difference=5.66 (95% CI=0.8-10.45), p<.05], increased depression, OR=1.75 (95% CI = 1.12-2.75), and increased odds of being unmarried, OR=1.58 (95% CI = 1.05-2.39) but did not differ in term of age, era of service, employment, combat exposure or alcohol misuse.
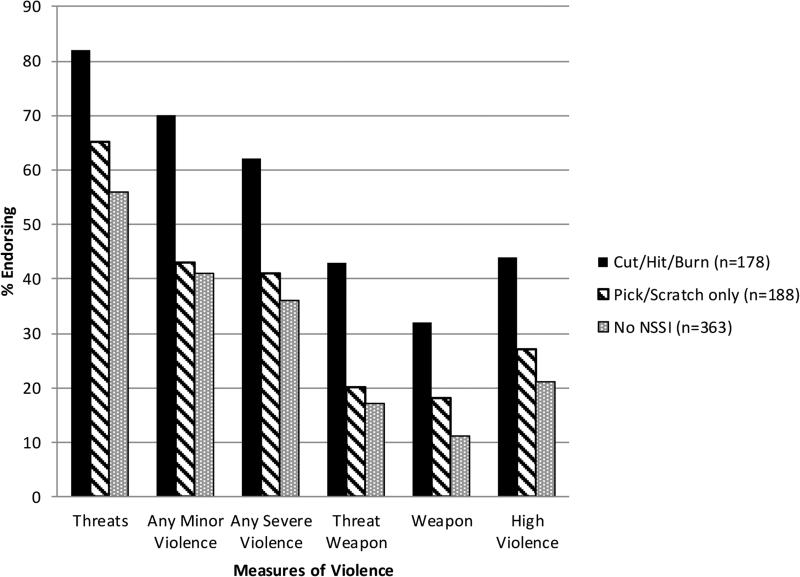
As illustrated in Figure 1, results examining the bivariate association between NSSI and violence indicated that veterans who engaged in picking/scratching only were more likely to make violent threats than those with no NSSI behaviors. Veterans who engaged in picking/scratching only were also more likely to report using a weapon than those reporting no NSSI in bivariate analyses (see Table 2). As shown in Table 2, NSSI in the form of cutting, hitting, or burning was significantly related to all of the violence outcomes in bivariate results.
Fig 1.
Percent endorsing past-year aggression and violent acts among help-seeking veterans with PTSD by NSSI status. Threats = Threatened to hit or throw something at a person. Any Minor Violence = threw something at a person; pushed, grabbed, or shoved a person; slapped a person. Any Severe Violence = kicked, bit or hit a person; beat up a person; threatened a person with a knife or gun; used a knife or gun. Threat Weapon = threatened a person with a knife or gun. Weapon = used a knife or gun. High violence = Thirteen or more minor and/or severe violent acts reported in the past year.
Table 2.
Interpersonal Violence among help-seeking veterans with PTSD by NSSI status
| No NSSI (n=363) |
NSSI: Pick or Scratch Only (n=188) |
NSSI: Cut/Hit/Burn (n=178) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Endorsed | Endorsed | Unadjusted OR | Adjusted ORa | Endorsed | Unadjusted OR | Adjusted ORa | |||||
| % | % | OR | 95% CI | OR | 95% CI | % | OR | 95% CI | OR | 95% CI | |
| Threats | 56.2 | 65.4 | 1.48 | (1.02, 2.13) | 1.40 | (0.96, 2.06) | 82.0 | 3.56 | (2.30, 5.50) | 2.63 | (1.65, 4.18) |
| Minor Violence | 41.3 | 42.6 | 1.05 | (0.74, 1.50) | 0.96 | (0.65, 1.40) | 70.2 | 3.35 | (2.28, 4.91) | 2.36 | (1.56, 3.57) |
| Severe Violence | 36.4 | 41.5 | 1.24 | (0.87, 1.78) | 1.14 | (0.77, 1.68) | 61.8 | 2.83 | (1.96, 4.10) | 1.87 | (1.24, 2.82) |
| Threats -Weapon | 17.4 | 19.7 | 1.17 | (0.74, 1.83) | 1.07 | (0.66, 1.73) | 43.3 | 3.63 | (2.43, 5.43) | 2.34 | (1.51, 3.64) |
| Use of a Weapon | 11.3 | 17.6 | 1.67 | (1.02, 2.75) | 1.64 | (0.97, 2.77) | 32.0 | 3.70 | (2.35, 5.82) | 2.47 | (1.51, 4.01) |
| High Violence | 21.5 | 27.1 | 1.36 | (0.91, 2.05) | 1.26 | (0.81, 1.96) | 43.82 | 2.85 | (1.93, 4.20) | 1.98 | (1.28, 3.04) |
Note. NSSI = Nonsuicidal self-injury, OR=Odds Ratio; CI=Confidence Interval.
Adjusted for age, race, marital status, employment status, socioeconomic status, combat exposure, presence of major depression, alcohol misuse severity, PTSD symptom severity, and difficulty controlling violence in past 30 days. The referent category for all odds ratios is Veterans without NSSI. Odds Ratios with confidence intervals that do not contain 1 are statistically significant at p<0.05.
3.2. Multivariable models of violence
Logistic regression was used to examine the association between NSSI and each violence domain after adjusting for dispositional, historical, contextual and clinical factors associated with violence including a recent history of difficulty controlling violence. While bivariate results indicated that those individuals engaging only in picking/scratching were more likely to make violent threats and use a weapon than those reporting no NSSI, there were no significant differences between veterans who engaged in picking/scratching only and veterans without NSSI in fully adjusted models (see Table 2). In contrast, veterans engaging in any cutting, hitting or burning were significantly more likely to make threats, engage in minor violence, and engage in severe violence, even after accounting for age, race, marital status, unemployment, SES, combat exposure, depression, alcohol misuse, PTSD symptom severity, and self-reported difficulty controlling violence. NSSI in the form of cutting, hitting or burning was related to weapon related violence including making threats with a weapon and actual violent acts involving a gun or knife. Patients who reported current NSSI were significantly more likely to be categorized as highly violent even after adjusting for other demographic and clinical risk factors (see Table 2).
Negative binomial regression and a ZINB model were used to examine the association of NSSI with the number of violent acts in the past year. As expected the count of violent acts was overdispersed. The mean number of violent acts for the sample was 14.88 (s.d. = 27.49), median = 4. The Vuong test comparing the ZINB to the negative binomial model indicated that the ZINB model did not significantly improve model fit (z=1.79, n.s.), thus results of the negative binomial model are presented. Results are summarized in Table 3. PTSD symptom severity and alcohol misuse were each independently associated with increased reports of violence in the past year. Not surprisingly, reported difficulty controlling violence in the past 30 days was a strong indicator of violence. NSSI explained unique variance in the number of violent acts in the past year beyond these demographic and clinical risk factors. Veterans with PTSD who endorsed any cutting/hitting/burning had an estimated rate of interpersonal violence 63% higher than help-seeking veterans with PTSD without NSSI after controlling for other dispositional, historical, contextual and clinical factors. Veterans who engaged in scratching/picking only did not significantly differ from those with no NSSI in rates of violence.
Table 3.
Negative Binomial Regression Model of Past-Year Interpersonal Violence
| Variable | β | SE β | Chi-Square | IRR | 95% CI |
|---|---|---|---|---|---|
| Age | −0.0046 | .0067 | 0.47 | 0.94 | [0.98, 1.01] |
| Minority Race | 0.3399 | 0.1464 | 5.39* | 1.40 | [1.05,1.87] |
| Unemployed | 0.1265 | 0.1696 | 0.56 | 1.01 | [0.81, 1.58] |
| SES | −0.0005 | 0.0066 | 0.01 | 1.00 | [0.99, 1.01] |
| Marital Status-Unmarried | 0.2479 | 0.1407 | 3.10 | 1.30 | [0.97, 1.69] |
| Combat Exposure (CES) | −0.0001 | 0.0063 | 0.00 | 1.00 | [.99, 1.01] |
| Alcohol Misuse (AUDIT) | 0.0196 | 0.0066 | 8.78** | 1.02 | [1.01, 1.03] |
| Major Depression | 0.2953 | 0.1503 | 3.86 | 1.34 | [1.00, 1.80] |
| PTSD Severity (CAPS) | 0.0082 | 0.0041 | 4.03* | 1.01 | [1.00, 1.02] |
| Difficulty Controlling Violence | 0.8152 | 0.1458 | 31.26*** | 2.27 | [1.70, 3.01] |
| NSSI: Picking/Scratching only | 0.1587 | 0.1692 | 0.88 | 1.17 | [0.84, 1.63] |
| NSSI: Any Cut/Hit/Burn | 0.4936 | 0.1733 | 8.11** | 1.63 | [1.17, 2.30] |
Note. IRR = Incident Rate Ratio. Race modeled as Minority vs. White, Employment modeled as Unemployed vs. Employed; Marital status modeled as Unmarried vs. Married. CES = Combat Exposure Scale, AUDIT = Alcohol Use Disorders Identification Test; CAPS = Clinician Administered PTSD Scale; PAI = Personality Assessment Inventory; NSSI = Non-suicidal Self Injury
p<0.05
p<0.01
p<0.0001
4. Discussion
Consistent with other studies of veterans with PTSD (Calhoun et al., 2002; Elbogen et al., 2010a; Jakupcak et al., 2007; Wright et al., 2012), high rates of violence were found in the current sample. Results are comparable to data collected as part of the National Vietnam Veterans Readjustment Study (NVVRS) which found that Vietnam veterans with PTSD reported significantly higher levels of interpersonal violence than era veterans without PTSD (McFall et al., 1999). As hypothesized, the current study found that NSSI was uniquely associated with violence among help-seeking veterans with PTSD, even after accounting for other factors previously demonstrated to be risks for the commission of violence among veterans (Elbogen et al., 2010a). Veterans who injured themselves through cutting, hitting, or burning were much more likely to engage in interpersonal violence than those without NSSI, however, veterans who engaged in picking/scratching only were not at higher risk of interpersonal violence than those without any NSSI. To our knowledge, this is the first study to examine the connection between NSSI and interpersonal violence in a veteran population. Although previous research has demonstrated the importance of NSSI as a behavioral marker for suicide risk among veterans (Kimbrel et al., 2016; Kimbrel et al., 2015; Kimbrel et al., 2014), results from the current study indicate that NSSI, particularly in the form of cutting/hitting/burning may be a significant behavioral marker for increased interpersonal violence as well.
Results from the current study are consistent with studies examining the relationship between NSSI and interpersonal violence in adolescents (Boxer, 2010; Brunner et al., 2007; Sourander et al., 2006; Vivona et al., 1995). Results are also consistent with a study of college students that found NSSI was positively associated with trait aggression (Kleiman et al., 2015). NSSI and interpersonal violence may have shared etiologic factors. Decreased serotonin [5-hydroxytryptamine (5-HT)] has been implicated in the pathophysiology of self-injurious behavior with and without suicidal intent (Crowell et al., 2008; McCloskey et al., 2009; Steiger et al., 2001). Similarly, lower levels of central 5-HT functioning has been posited as a neurochemical basis of human aggression with results of meta-analytic analyses of 175 independent samples suggesting a small inverse correlation (r= −.12) between measures of central 5-HT functioning and aggression (Duke et al., 2013). Others have speculated that dysfunction in the endogenous opioid system (EOS) may underlie self-injury and aggressive behavior (Bandelow et al., 2010; Siever, 2008). More research is needed to understand the neurobiology of NSSI and interpersonal violence.
4.1. Clinical implications
Current findings have important clinical implications. Routine screening for a wide variety of NSSI behaviors, especially in Veteran Health Administration (VHA) psychiatric settings, is warranted. Clinicians should be aware that NSSI is prevalent among male help-seeking veterans with PTSD regardless of age, race, SES, working status, or combat era. Previous studies indicate that NSSI is a robust predictor of suicidal ideation and suicide attempts in veterans with PTSD (Kimbrel et al., 2016; Kimbrel et al., 2015; Kimbrel et al., 2014). Results from the current study indicate that the assessment of NSSI may also help in identifying those at highest risk for engaging in interpersonal violence. In particular, it has been recommended that clinicians working with veterans systematically examine risk and protective factors that have empirical support in order to improve decision-making (Elbogen et al., 2010a). As such, the current study attests to the need for clinicians to assess NSSI history, and in particular a history of cutting/hitting/burning, when conducting risk assessments for violence as well as suicide.
Veterans who reported engaging in NSSI in the past year reported heightened levels of PTSD symptoms and depression. More work is needed to examine the functions of NSSI in this population. Veterans with PTSD may engage in NSSI in an attempt to cope with severe levels of psychological distress. Clinicians working with veterans with PTSD who engage in NSSI may consider specifically targeting the reduction of NSSI behaviors. Currently, there are few psychological interventions for NSSI that meet the standards for empirically supported psychosocial interventions (Stanley et al., 2014). Cognitive and behavioral interventions have the most support for efficacy in reducing NSSI (Stanley et al., 2014). Interventions that specifically target emotional regulation skills [e.g, (Gratz et al., 2014; Linehan, 1993; Ford et al., 2011; Cloitre et al., 2010)] may be particularly useful. However, more research aimed at treating NSSI in veterans is clearly needed.
4.2. Limitations
There are a number of important limitations to the current study. First, cross-sectional data collection limits the ability to draw conclusions about temporal relationships in the present study. Longitudinal research is needed to examine whether NSSI is prospectively predictive of interpersonal violence. Given that the sample was limited to male, help-seeking veterans with PTSD, results may not generalize to other veterans (e.g., women veterans). While the clinic from which these data were collected is generally representative of specialty PTSD clinics within the VHA, results may not generalize to all veterans with PTSD. More work examining interpersonal violence and NSSI in more diverse samples of veterans is needed. While the HQ has been used in several studies to examine NSSI (Kimbrel et al., 2014; Sacks et al., 2008; Weaver et al., 2004); it only contains four items traditionally considered as NSSI. The HQ is also limited in that the assessment of antecedents and consequences of engaging in NSSI is limited to the most recent episode. Thus, it may be difficult to know whether engaging in a certain NSSI behavior was the product of intentional self-harm or a byproduct of reflexive distress-related behaviors, e.g., picking/scratching of the skin as a manifestation of anxiety. Future studies that use measures that assess a broader array of NSSI behaviors [e.g., the Deliberate Self-Harm Inventory; (Gratz, 2001)] in veterans are also needed. Finally, the sample size and relatively low-base rate of certain forms of NSSI, precluded an examination of individual NSSI behaviors. Studies of latent classes of NSSI have indicated that there may be classes of individuals who prefer one type or types of NSSI over others (Klonsky & Olino, 2008; Kleiman et al., 2015). More work is needed to examine the reliability of subtypes of self-injurers and the predictive validity of subtypes for specific risk-factors such as interpersonal violence.
4.3. Conclusion
Despite these limitations, the present study demonstrates that engaging in NSSI in the form of cutting, hitting or burning is significantly associated with increased interpersonal violence among help-seeking veterans with PTSD. NSSI explained unique variance in interpersonal violence beyond well-known clinical and demographic risk factors. Although additional research is needed to replicate these findings in other clinical samples, results suggest clinicians working with veterans with PTSD should consider assessment of NSSI as part of a comprehensive approach to risk assessment.
Highlights.
Veterans with PTSD are at increased risk for engaging in other-directed violence.
Nonsuicidal self-injury (NSSI) is a form of self-directed violence.
This study examined NSSI and interpersonal violence in 729 veterans with PTSD.
NSSI in the form of cutting, hitting or burning oneself predicted violence after accounting for well-known violence risk factors.
Clinicians should assess NSSI when conducting risk assessments for violence as well as suicide.
Acknowledgements
This work was supported in part by the VA Mid-Atlantic Mental Illness Research, Education, and Clinical Center. Dr. Van Voorhees is supported by a VA Career Development Award from the Rehabilitation Research and Development Service of VA Office of Research and Development (ORD) (IK2RX001298). Dr. Beckham is supported by a VA Research Scientist Award from the Clinical Sciences Research and Development Service (CSR&D) of VA Office of Research and Development (ORD). Dr. Dedert is supported by a VA Career Development Award from the CSR&D of VA ORD (IK2CX000718). Dr Kimbrel was supported by a Career Development Award (IK2 CX000525) from the Clinical Science Research and Development Service of the VA ORD. The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the VA or the United States government or any of the institutions with which the authors are affiliated.
References
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. Fourth Edition, text revision American Psychiatric Association; Washington, DC: 2000. [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. In: AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care. 2nd ed. Department of Mental Health and Substance Dependence, editor. World Health Organization; Geneva, Switzerland.: 2001. [Google Scholar]
- Bandelow B, Schmahl C, Falkai P, Wedekind D. Borderline personality disorder: A dysregulation of the endogenous opioid system? Psychological Review. 2010;117(2):623–636. doi: 10.1037/a0018095. [DOI] [PubMed] [Google Scholar]
- Beckham JC, Feldman ME, Kirby AC, Hertzberg MA, Moore SD. Interpersonal violence and its correlates in Vietnam veterans with chronic posttraumatic stress disorder. Journal of Clinical Psychology. 1997;53:859–869. doi: 10.1002/(sici)1097-4679(199712)53:8<859::aid-jclp11>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, Keane TM. The development of a clinician-administered posttraumatic stress disorder scale. Journal of Traumatic Stress. 1995;8:75–80. doi: 10.1007/BF02105408. [DOI] [PubMed] [Google Scholar]
- Boxer P. Covariation of self- and other-directed aggression among inpatient youth: continuity in the transition to treatment and shared risk factors. Aggressive Behavior. 2010;36(3):205–217. doi: 10.1002/ab.20343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briere J, Gil E. Self-mutilation in clinical and general population samples: prevalence, correlates, and functions. The American Journal of Orthopsychiatry. 1998;68(4):609–620. doi: 10.1037/h0080369. [DOI] [PubMed] [Google Scholar]
- Brunner R, Parzer P, Haffner J, Steen R, Roos J, Klett M, Resch F. Prevalence and psychological correlates of occasional and repetitive deliberate self-harm in adolescents. Archives of pediatrics & adolescent medicine. 2007;161(7):641–649. doi: 10.1001/archpedi.161.7.641. [DOI] [PubMed] [Google Scholar]
- Bryan C, Bryan A. Nonsuicidal self-injury among a sample of United States military personnel and veterans enrolled in college classes. Journal of Clinical Psychiatry. 2014;70(9):874–885. doi: 10.1002/jclp.22075. [DOI] [PubMed] [Google Scholar]
- Bryan CJ, Rudd MD, Wertenberger E, Young-McCaughon S, Peterson A. Nonsuicidal self-injury as a prospective predictor of suicide attempts in a clinical sample of military personnel. Comprehensive Psychiatry. 2015;59:1–7. doi: 10.1016/j.comppsych.2014.07.009. [DOI] [PubMed] [Google Scholar]
- Calhoun PS, Beckham JC, Bosworth HB. Caregiver burden and psychological distress in partners of veterans with chronic posttraumatic stress disorder. Journal of Traumatic Stress. 2002;15:205–212. doi: 10.1023/A:1015251210928. [DOI] [PubMed] [Google Scholar]
- Chapman AL, Gratz KL, Brown MZ. Solving the puzzle of deliberate self-harm: the experiential avoidance model. Behavior Research and Therapy. 2006;44(3):371–394. doi: 10.1016/j.brat.2005.03.005. [DOI] [PubMed] [Google Scholar]
- Cloitre M, Stovall-McClough KC, Nooner K, Zorbaz P, Cherry S, Jackson CL, Gan W, Petkova E. Treatment for PTSD related to childhood abuse: a randomized controlled trial. American Journal of Psychiatry. 2010;167:915–924. doi: 10.1176/appi.ajp.2010.09081247. [DOI] [PubMed] [Google Scholar]
- Crawford EF, Calhoun PS, Braxton LE, Beckham JC. Validity of the Personality Assessment Inventory aggression scales and Violence Potential Index in veterans with PTSD. Journal of Personality Assessment. 2007;88:91–99. doi: 10.1080/00223890709336839. [DOI] [PubMed] [Google Scholar]
- Crowell SE, Beauchaine TP, McCauley E, Smith CJ, Vasilev CA, Stevens AL. Parent-child interactions, peripheral serotonin, and self-inflicted injury in adolescents. Journal of Consulting and Clinical Psychology. 2008;76:15–21. doi: 10.1037/0022-006X.76.1.15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Duke AA, Begue L, Bell R, Eisenlohr-Moul T. Revisiting the serotonin-aggression relation in humans: A meta-analysis. Psychological Bulletin. 2013;139(5):1148–1172. doi: 10.1037/a0031544. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elbogen EB, Fuller S, Johnson SC, Brooks S, Kinneer P, Calhoun PS, Beckham JC. Improving risk assessment of violence among military veterans: An evidence-based approach for clinical decision-making. Clinical Psychology Review. 2010a;30(6):595–607. doi: 10.1016/j.cpr.2010.03.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elbogen EB, Wagner HR, Fuller SR, Calhoun PS, Kinneer PM, Beckham JC. Correlates of anger and hostility in Iraq and Afghanistan war veterans. American Journal of Psychiatry. 2010b;167(9):1051–1058. doi: 10.1176/appi.ajp.2010.09050739. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elhai JD, Calhoun PS, Ford J. Statistical procedures for analyzing mental health services and cost data. Psychiatric Research. 2008;160:129–136. doi: 10.1016/j.psychres.2007.07.003. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for Axis I DSM-IV Disorders. 2nd ed. Biometrics Research Department; New York, NY.: 1994. [Google Scholar]
- Fliege H, Lee JR, Grimm A, Klapp BF. Risk factors and correlates of deliberate self-harm behavior: A systematic review. Journal of Psychosomatic Research. 2009;66(6):477–493. doi: 10.1016/j.jpsychores.2008.10.013. [DOI] [PubMed] [Google Scholar]
- Ford JD, Steinberg KL, Zhang W. A randomized clinical trial comparing affect regulation and social problem-solving psychotherapies for mothers with victimization-related PTSD. Behavior Therapy. 2011;42:560–578. doi: 10.1016/j.beth.2010.12.005. [DOI] [PubMed] [Google Scholar]
- Freeman TW, Roca V. Gun use, attitude toward violence, and agression among combat veterans with chronic posttraumatic stress disorder. Journal of Nervous & Mental Disease. 2001;189(5):317–320. doi: 10.1097/00005053-200105000-00008. [DOI] [PubMed] [Google Scholar]
- Gratz KL. Measurement of deliberate self-harm: Preliminary data on the Deliberate Self-Harm Inventory. Journal of Psychopathology & Behavioral Assessment. 2001;23(4):253–263. [Google Scholar]
- Gratz KL, Tull MT, Levy R. Randomized controlled trial and uncontrolled 9-month follow-up of an adjunctive emotion regulation group therapy for deliberate self-harm among women with borderline personality disorder. Psychological Medicine. 2014;44(10):2099–2112. doi: 10.1017/S0033291713002134. [DOI] [PubMed] [Google Scholar]
- Hollingshead AB, Redlich RL. Social class and mental illness. John Wiley; New York: 1958. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jakupcak M, Conybeare D, Phelps L, Hunt S, Holmes HA, Felker B, Klevens M, McFall M. Anger, hostility, and aggression among Iraq and Afghanistan War veterans reporting PTSD and subthreshold PTSD. Journal of Traumatic Stress. 2007;20(6):945–954. doi: 10.1002/jts.20258. [DOI] [PubMed] [Google Scholar]
- Jordan BK, Marmar CR, Fairbank JA, Schlenger WE, Kulka RA, Hough RL, Weiss DS. Problems in families of male Vietnam Veterans with Posttraumatic stress disorder. Journal of Consulting & Clinical Psychology. 1992;60(6):916–926. doi: 10.1037//0022-006x.60.6.916. [DOI] [PubMed] [Google Scholar]
- Keane TM, Fairbank JA, Caddell JM, Zimering RT, Taylor KL, Mora CA. Clinical evaluation of a measure to assess combat exposure. Psychological Assessment: A Journal of Consulting and Clinical Psychology. 1989;1:53–55. [Google Scholar]
- Kimbrel NA, DeBeer BB, Meyer EC, Gulliver SB, Morissette SB. Nonsuicidal self-injury and suicide attempts in Iraq/Afghanistan war veterans. Psychiatry Research. 2016 doi: 10.1016/j.psychres.2016.06.039. E-pub ahead of print: 28 June. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbrel NA, Gratz KL, Tull MT, Morissette SB, Meyer EC, DeBeer BB, Silvia PJ, Calhoun PC, Beckham JC. Non-suicidal self-injury as a predictor of active and passive suicidal ideation among Iraq/Afghanistan war veterans. Psychiatry Research. 2015;227(2-3):360–362. doi: 10.1016/j.psychres.2015.03.026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kimbrel NA, Johnson ME, Clancy C, Hertzberg M, Collie C, Van Voorhees EE, Dennis MF, Calhoun PS, Beckham JC. Deliberate self-harm and suicidal ideation among male Iraq/Afghanistan-era veterans seeking treatment for PTSD. Journal of Traumatic Stress. 2014;27(4):474–477. doi: 10.1002/jts.21932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kleiman EM, Ammerman BA, Kulper DA, Uyeji LL, Jenkins AL, McCloskey MS. Forms of non-suicidal self-injury as a function of trait aggression. Comprehensive Psychiatry. 2015;59:21–27. doi: 10.1016/j.comppsych.2014.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Klonsky ED. Non-suicidal self-injury in United States adults: Prevalence, sociodemographics, topography and functions. Psychological Medicine. 2011;41(9):1981–1986. doi: 10.1017/S0033291710002497. [DOI] [PubMed] [Google Scholar]
- Klonsky ED, Olino TM. Identifying clinically distinct subgroups of self-injurers among young adults: A latent class analysis. Journal of Consulting and Clinical Psychology. 2008;76:22–27. doi: 10.1037/0022-006X.76.1.22. [DOI] [PubMed] [Google Scholar]
- Linehan M. Cognitive-behavioral treatment of borderline personality disorder. Guilford; New York: 1993. [Google Scholar]
- McCloskey MS, Ben-Zeev D, Lee R, Berman ME, Coccaro EF. Acute tryptophan depletion and self-injurious behavior in aggressive patients and healthy volunteers. Psychopharmacology (Berl) 2009;203(1):53–61. doi: 10.1007/s00213-008-1374-6. [DOI] [PubMed] [Google Scholar]
- McFall M, Fontana A, Raskind M, Rosenheck R. Analysis of violent behavior in Vietnam combat Veteran Psychiatric inpatients with posttraumatic stress disorder. Journal of Traumatic Stress. 1999;12(3):501–517. doi: 10.1023/A:1024771121189. [DOI] [PubMed] [Google Scholar]
- Resnick HS, Weaver T. Habit Questionnaire. Department of Psychiatry and Behavioral Sciences, Medical University of South Carolina; Charleston SC, Charleston, SC: 1994. Unpublished mansucript. [Google Scholar]
- Sacks MB, Flood AM, Dennis MF, Hertzberg MA, Beckham JC. Self-mutilative behaviors in male veterans with posttraumatic stress disorder. Journal of Psychiatric Research. 2008;42(6):487–494. doi: 10.1016/j.jpsychires.2007.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Puente JR, Grant M. Development of the alcohol use disorders screening Test (AUDIT). WHO collaborative project on early detection of persons with harmful alcohol consumption II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Siever LJ. Neurobiology of aggression and violence. American Journal of Psychiatry. 2008;165(4):429–442. doi: 10.1176/appi.ajp.2008.07111774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sourander A, Aromaa M, Pihlakoski L, Haavisto A, Rautava P, Helenius H, Sillanpaa M. Early predictors of deliberate self-harm among adolescents. A prospective follow-up study from age 3 to age 15. Journal of Affective Disorders. 2006;93(1-3):87–96. doi: 10.1016/j.jad.2006.02.015. [DOI] [PubMed] [Google Scholar]
- Stanley B, Fineran V, Brodsky B. Psychological Treatment for Nonsuicidal Self-Injury. In: Nock MK, editor. The Oxford Handbook of Suicide and Self Injury. Oxford University Press; New York: 2014. [Google Scholar]
- Steiger H, Koerner N, Engelberg MJ, Israel M, Ng Ying Kin NM, Young SN. Self-destructiveness and serotonin function in bulimia nervosa. Psychiatry Research. 2001;103(1):15–26. doi: 10.1016/s0165-1781(01)00264-5. [DOI] [PubMed] [Google Scholar]
- Straus M. New scoring methods for violence and new norms for the Conflict Tactics Scales. Transaction. New Brunswick, NJ.: 1989. Physical violoence in American familiies: Risk factors and adaptations to violence in 8145 families; pp. 535–559. [Google Scholar]
- Straus MA. Measuring intrafamily conflict and violence: The Conflict Tactics Scales. Journal of Marriage and the Family. 1979;41:75–88. [Google Scholar]
- Straus MA. Measuring intrafamily conflict and violence: The Conflict Tactics Scale. In: Straus MA, Gelles RJ, editors. Physical violence in American families. The Transaction Publishers; New Brunswick, NJ.: 1990. [Google Scholar]
- Van Voorhees EE, Dennis PA, Elbogen EB, Clancy CP, Hertzberg MA, Beckham JC, Calhoun PS. Personality assessment inventory internalizing and externalizing structure in veterans with posttraumatic stress disorder: associations with aggression. Aggressive Behavior. 2014;40(6):582–592. doi: 10.1002/ab.21554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vivona JM, Ecker B, Halgin RP, Cates D, Garrison WT, Friedman M. Self- and other-directed aggression in child and adolescent psychiatric inpatients. Journal of the American Academy of Child and Adolescent Psychiatry. 1995;34(4):434–444. [PubMed] [Google Scholar]
- Weathers FW, Keane TM, Davidson JR. Clinician-administered PTSD scale: A review of the first ten years of research. Depression and Anxiety. 2001;13:132–156. doi: 10.1002/da.1029. [DOI] [PubMed] [Google Scholar]
- Weathers FW, Newman E, Blake DD, Nagy LM, Schnurr P, Kaloupek DG, Charney DS, Keane TM. Clinician-Administered PTSD Scale (CAPS): Interviewer's Guide. Western Psychological Services; Los Angeles, CA.: 2004. [Google Scholar]
- Weaver TL, Chard KM, Mechanic MB, Etzel JC. Self-injurious behaviors, PTSD arousal, and general health complaints within a treatment-seeking sample of sexually abused women. Journal of Interpersonal Violence. 2004;19(5):558–575. doi: 10.1177/0886260504262965. [DOI] [PubMed] [Google Scholar]
- Wolff JC, Frazier EA, Esposito-Smythers C, Becker SJ, Burke TA, Cataldo A, Spirito A. Negative cognitive style and perceived social support mediate the relationship between aggression and NSSI in hospitalized adolescents. Journal of Adolescence. 2014;37(4):483–491. doi: 10.1016/j.adolescence.2014.03.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wright KM, Foran HM, Wood MD, Eckford RD, McGurk D. Alcohol problems, aggression, and other externalizing behaviors after return from deployment: Understanding the role of combat exposure, internalizing symptoms, and social environment. Journal of Clinical Psychiatry. 2012;68(7):782–800. doi: 10.1002/jclp.21864. [DOI] [PubMed] [Google Scholar]