Abstract
Context
Given recent Medicare rules reimbursing clinicians for engaging in advance care planning, there is heightened need to understand factors associated with the timing of advance directive (AD) completion before death and how the timing impacts care decisions.
Objective
The purpose of this study is to investigate patterns in timing of AD completion and the relationship between timing and documented care preferences. We hypothesize that ADs completed late in the course of illness or very early in the disease trajectory will reflect higher preferences for aggressive care.
Methods
We conducted a retrospective study using logistic regressions to analyze data from the Health and Retirement Study, a nationally representative longitudinal survey of older adults.
Results
The analytic sample included exit interviews conducted from 2000–2012 among 2,904 proxy reporters of deceased participants who had an AD. Nearly three-quarters (71%) of ADs were completed a year or more before death. Being younger or a racial/ethnic minority, and having lower education, a diagnosis of cancer or lung disease, and an expected death were associated with completing an AD within the three months prior to death, while having the lowest quartile of assets and memory problems were inversely associated with AD completion. Minorities, those with lower education, expected death, and timing of AD completion were associated with electing aggressive care.
Conclusion
Early documentation of care wishes may not be associated with in increased likelihood of electing aggressive care, however ADs completed in the last months of life have higher rates of election of aggressive care.
Keywords: Advance directives, care preferences, ethnic differences
INTRODUCTION
Improving completion rates of advance directive (AD) has been identified as a national priority and is the subject of several practice, policy, and research initiatives. (1–3) ADs are written instructions about the type of care an individual would like should they become unable to communicate this directly. The recent Institute of Medicine report on “Dying in America” identified the need for better education and support systems to foster advance directive completion. (2) This recommendation arises from a growing literature demonstrating that advance care planning, including completion of ADs, use of a health care durable power of attorney (identification of an individual to make health care decisions for you if you are unable), and/or having a discussion about care preferences with family members, is associated with improved quality of care, including greater and longer enrollment in hospice and fewer hospital deaths.(4–6) Studies also have found that patients with ADs are more likely to receive care consistent with their wishes. (7)
Yet, despite these recommendations and positive findings, many individuals do not develop advance directives. Recent literature suggests there may be a an ideal moment for completing ADs, an optimal time during the course of illness for completing advance directives that reflect both patient values and their prognosis.8 Billings and Bernacki (2014) posited that the timing of AD completion may influence desires to prolong care or seek aggressive care. (8) They suggest that completing an AD “too early” when a patient is in relative good health may result in a preference for more aggressive care, which may not be appropriate as health changes and declines toward end of life.(8) Conversely, completing an AD “too late” when patients are nearing death may be the result of rushed decision-making during moments of symptom exacerbation and medical crisis, with a greater focus on needed medical interventions and prolonged care.(8) Moreover, these late decisions may not reflect patient preferences for care at end of life and may result in unwanted, aggressive care.
Likewise, physicians, who struggle with having goals of care discussions, (9–11) also are grappling with timing on when to broach these conversations.(12, 13) They fear that broaching the topic too early may cause patients to lose hope (14, 15) and oftentimes wait for patients to initiate discussions.(16) As a result, physicians oftentimes delay or avoid having these conversations altogether.(9) With the U.S. now reimbursing physicians for advance care planning discussions, better understanding of AD completion timing and related care decisions will help inform physicians about potential impact of initiating early or late advance planning conversations.
To date, there has been no empirical research on timing of AD completion and little is known about the factors which influence care choices elected at different time points along the life span. The purpose of this study is to investigate patterns in timing of AD completion and the relationship between timing and documented care preferences. We hypothesize that ADs completed late in the course of illness (e.g., three months prior to death) or early in the disease trajectory (e.g., greater than two years before death) will reflect preferences for more aggressive care; those developed late may be done in the moment during medical crisis while those developed early may reflect care preferences during a healthier period. Additionally, we investigate patient characteristics associated with late completion of an AD and preferences for aggressive care.
METHODS
We use data from the Health and Retirement Study (HRS), a nationally representative longitudinal survey of Unites States adults, ages 51 and older.(17) These data are publicly available, de-identified, and exempt from human subjects review.
The HRS survey is conducted every two years until death, at which time an exit interview is conducted with a proxy, generally family members. We use data from exit interviews conducted from 2000–2013, representing decedents who died between 1997 and 2013.
Outcomes
Our primary outcome variables were derived from exit interview proxy responses to questions about whether the decedent had written instructions for the treatment or care he/she wanted in the final days of life, as well as the approximate year and month in which the instructions were completed. For the purpose of this paper, we are categorizing this variable as completing an AD, although we recognize that this variable may include other written documentation such as a Physician/Medical Order for Life Sustaining Treatment (POLST/MOLST; form that serves as a medical order for documented care preferences) or a do not resuscitate (DNR) order. We calculated timing of AD completion in months by subtracting the reported month and year the written instructions were completed from the month and year of death. We characterized “late” AD completion as an AD completed in the last 3 months of life. A previous study found that individuals without an AD are more likely to have a burdensome transition, defined in part as moving between care settings in the last three months of life (18), thus we adopted this time frame for our study. For our study, we examined preferences for aggressive care among those decedents with an AD. For this variable, proxies were asked if the decedent’s instructions involved “a desire to give all care possible unconditionally in order to prolong life” (i.e. aggressive care).
Covariates
Our covariates include demographic and socioeconomic characteristics (age at time of death, gender, race/ethnicity, marital status, education, and assets), and medical conditions (history of cancer, lung or heart disease, stroke, memory-related disease). Race and Hispanic ethnicity were reported by respondents using categories provided by the interviewer. Respondents are first asked if they consider themselves Hispanic or Latino, for those not responding yes, they are then asked if they are primarily white or Caucasian, Black or African American, American Indian, or Asian, or something else. For this paper, we group non-whites (Hispanics and Blacks) into one minority category.
We also included proxy indicators of whether the death was expected. Covariates were drawn from both the HRS core interviews conducted while respondents were alive as well as from the exit interview.
Analysis
We conducted bivariate analyses of sociodemographic and health status by AD timing within three months of death and aggressive care preference. Next, we conducted multivariate logistic regressions to examine factors associated with completing an AD in the last three months of life as well as factors associated with documenting preferences for aggressive care. All analyses were weighted using the last sample weight available prior to death to correct for differential probability of sample selection and survey response. Analyses were conducted using Stata version 14 (StataCorp, College Station, TX). Alpha level was set at .05.
RESULTS
Study Sample
Of the 9,164 respondents with an exit interview 3,810 (45%; weighted percentage) had completed an AD prior to death. We excluded from the analytic sample 442 cases with missing data on AD timing or timing values that occurred after the death of the decedent. In comparing those missing AD timing to those with timing information, we found only one difference between the groups; those with heart disease were less likely to be missing information on AD timing. We also excluded 48 cases for which the exit interview was conducted with a proxy more than three years after the respondent’s death in order to minimize potential for recall error. After excluding 416 cases with missing information on model covariates, the final analytic sample consisted of 2,904 decedents.
On average, proxies were interviewed at 11 months following the death of their family member. About 75% of the sample was interviewed within 1 ½ years following the respondent’s death. Only 5% had a recall period greater than 2 years and 1% had recall 2 ½ years or longer.
Table 1 presents characteristics for those with an AD. Just over half the decedents (55.6%) were female and 40.1% were 85 years old or older, 34.5% aged 75–84, and 25.4% 50 to 74 years old. The vast majority (94.4%) of those with ADs were White. About 37% were married. About one-third (35.2%) had less than a high school education.
Table 1.
Characteristics of Analytic Sample, Respondents with AD Completion 0–3 Months Prior to Death, and Respondents with Preference for All Care Possible, (n=2,904) HRS
| AD | AD <3 Months Prior to Death |
Preference All Care Possible |
||||
|---|---|---|---|---|---|---|
| N | % | % | p-Value | % | p-Value | |
| Age | p<.001 | p<.01 | ||||
| 50–74 | 737 | 25.4 | 27.0 | 6.4 | ||
| 75–84 | 1002 | 34.5 | 11.5 | 4.6 | ||
| 85+ | 1165 | 40.1 | 6.5 | 2.9 | ||
| Gender | p<.05 | NS | ||||
| Male | 1290 | 44.4 | 15.1 | 4.5 | ||
| Female | 1614 | 55.6 | 12.1 | 4.3 | ||
| Race | p<.001 | p<.001 | ||||
| White | 2659 | 91.6 | 11.8 | 3.3 | ||
| Black | 165 | 5.7 | 23.0 | 26.7 | ||
| Hispanic | 80 | 2.8 | 25.0 | 13.8 | ||
| Education | NS | p<.001 | ||||
| 12 years or more | 2058 | 70.9 | 12.9 | 3.4 | ||
| Less than 12 years | 845 | 29.1 | 14.9 | 6.7 | ||
| Assets | p<.05 | p<.05 | ||||
| Top 75% | 2255 | 77.7 | 14.6 | 4.8 | ||
| Lowest 25% | 649 | 22.3 | 9.3 | 2.9 | ||
| Marital Status | p<.001 | NS | ||||
| Married | 1124 | 38.7 | 16.9 | 5.0 | ||
| Not married | 1780 | 61.3 | 11.3 | 4.0 | ||
| Cancer | p<.001 | NS | ||||
| No | 1754 | 60.4 | 9.6 | 4.8 | ||
| Yes | 1150 | 39.6 | 19.4 | 3.7 | ||
Timing of AD Completion
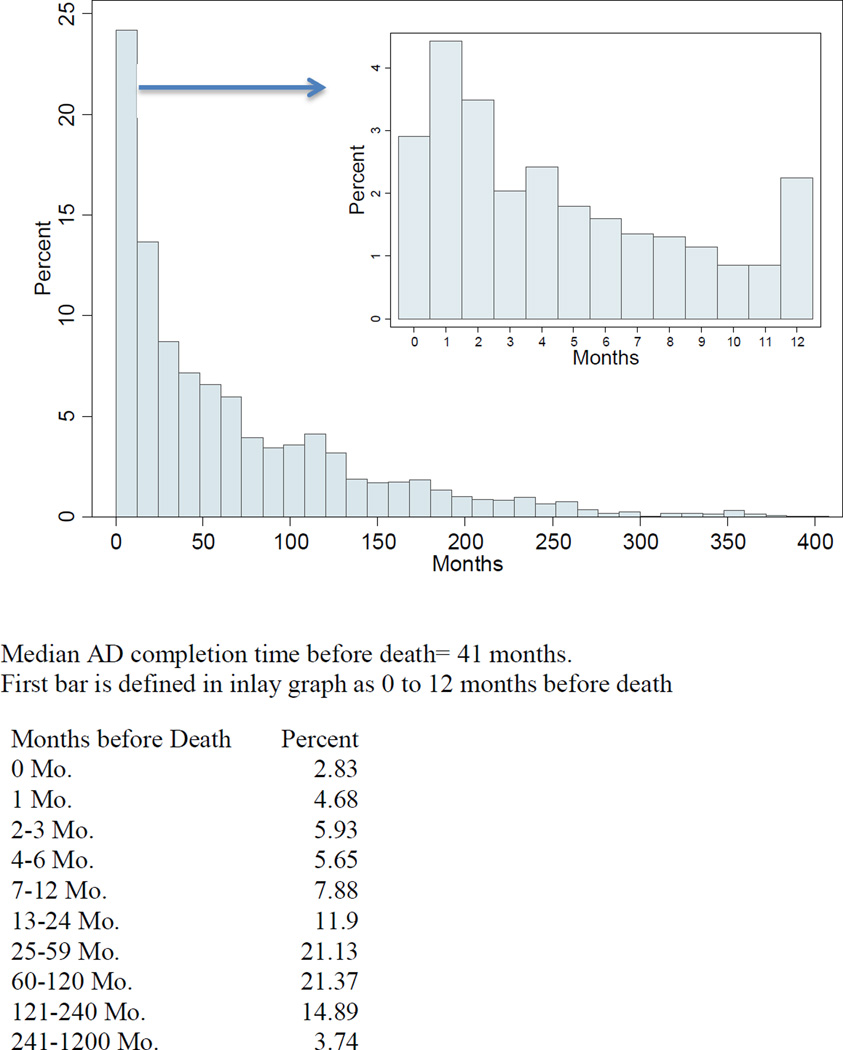
Timing of AD completion ranged from 0 to 591 months before death, with a median of 41 months. Figure 1 shows the distribution of AD completion timing in the months prior to death, truncated at 400 months prior to death. Nearly three-quarters (71%) of ADs were completed a year of more before death, with 24% completed in the last year (also depicted in Figure 1).
Figure 1.
Distribution of Respondents by Length of Time from AD Completion to Death (each bar=12 months) with Detailed View of Last Year of Life (inlay)
AD Preference for Aggressive Care
About 5.35% had AD care preferences for prolonged, aggressive care. Bivariate analysis of decedents’ sociodemographic characteristics by their care preferences revealed several significant differences. Younger decedents, ethnic minorities, those with lower education levels, and those with greater assets were significantly more likely to elect prolonged, aggressive care as compared with their counterparts. Health conditions were not associated with aggressive care preference. See Table 1.
Factors Associated with Late AD Completion
We examined factors associated with completing ADs in the last three months of life (see Table 2). As compared with those younger decedents (age 50–74), those age 75 to 84 (adjusted odds ratio, .40; 95% CI, .29 to .54) and 85 and over (adjusted odds ratio, .27; 95% CI, .18 to .39) had lower odds of late AD completion. Minorities (adjusted odds ratio, 1.89; 95% CI, 1.25 to 2.85) had significantly higher odds of completing an AD in the last three months of life as compared with Whites. Those with cancer (adjusted odds ratio, 1.64; 95% CI, 1.25 to 2.16) and lung disease (adjusted odds ratio, 1.50; 95% CI, 1.13 to 1.98) had significantly higher odds of completing an AD in the last three month of life while those with memory problems had lower odds of late AD completion (adjusted odds ratio, 0.46; 95% CI, .31 to .69). Having an expected death was associated with completing an AD in the last three months of life (adjusted odds ratio, 1.46; 95% CI, 1.09 to 1.96). Finally, those with the lowest quartile of assets had lower odds of late AD completion as compared with those with higher assets (adjusted odds ratio, .58; 95% CI, .30 to .68).
Table 2.
Logistic Regression Models of AD Completion Timing 0–3 Months and AD Preference All Care (N=2,903), HRS
| DV: AD Completion 0–3 Months Prior to Death |
DV: AD Preference for All Care Possible |
|||||||
|---|---|---|---|---|---|---|---|---|
| Variables | OR | P>z | [95% CI] | OR | P>z | [95% CI] | ||
| Age (ref=50–74) | ||||||||
| 75–84 | 0.40 | 0.00 | 0.29 | 0.54 | 0.88 | 0.64 | 0.53 | 1.47 |
| 85+ | 0.27 | 0.00 | 0.18 | 0.39 | 0.71 | 0.31 | 0.37 | 1.36 |
| Female | 1.08 | 0.60 | 0.81 | 1.46 | 1.15 | 0.53 | 0.74 | 1.80 |
| Minority | 1.89 | 0.00 | 1.25 | 2.85 | 6.69 | 0.00 | 4.23 | 10.57 |
| Education <12 yrs | 1.27 | 0.11 | 0.95 | 1.69 | 1.61 | 0.03 | 1.04 | 2.51 |
| Assets lowest 25% | 0.57 | 0.00 | 0.40 | 0.82 | 0.87 | 0.63 | 0.49 | 1.53 |
| Not married | 0.85 | 0.32 | 0.62 | 1.17 | 0.64 | 0.10 | 0.38 | 1.08 |
| Cancer | 1.64 | 0.00 | 1.25 | 2.16 | 0.78 | 0.25 | 0.51 | 1.19 |
| Lung disease | 1.49 | 0.01 | 1.13 | 1.97 | 1.25 | 0.32 | 0.81 | 1.92 |
| Heart disease | 0.88 | 0.33 | 0.67 | 1.15 | 1.17 | 0.46 | 0.77 | 1.80 |
| Stroke | 0.80 | 0.17 | 0.59 | 1.10 | 1.39 | 0.16 | 0.88 | 2.20 |
| Memory | 0.46 | 0.00 | 0.31 | 0.69 | 0.70 | 0.17 | 0.42 | 1.16 |
| Death expected | 1.46 | 0.01 | 1.09 | 1.96 | 0.48 | 0.00 | 0.32 | 0.73 |
| Timing AD to death, months |
1.00 | 0.03 | 0.99 | 1.00 | ||||
| Constant | 0.23 | 0.00 | 0.15 | 0.35 | 0.08 | 0.00 | 0.04 | 0.15 |
AD = Advanced Directive; HRS = Health and Retirement Study; DV = Dependent Variable
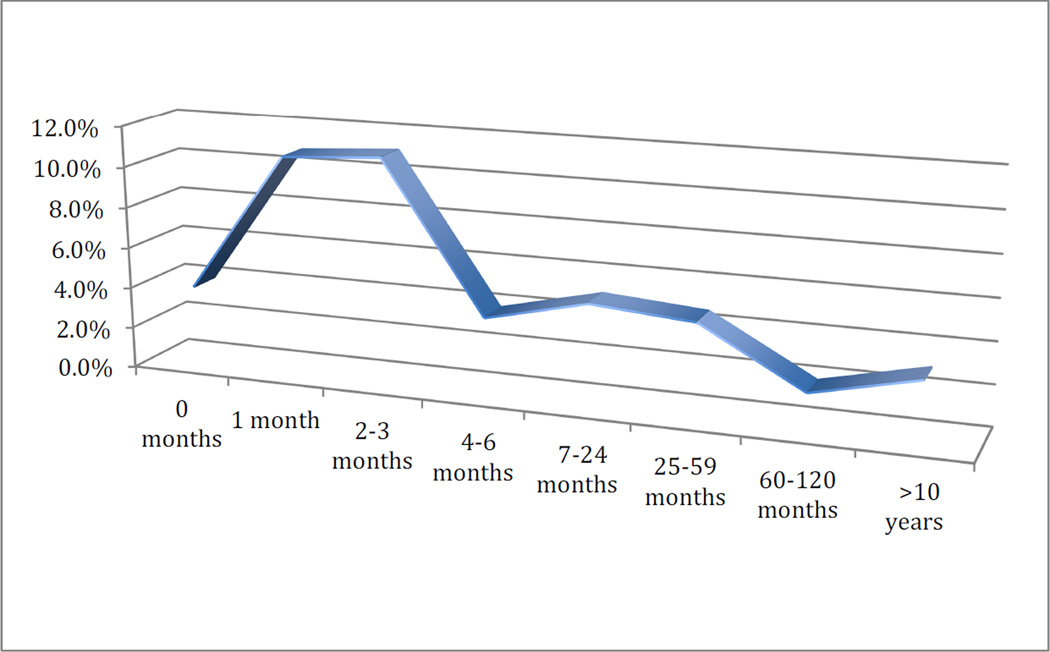
AD Preference for Aggressive Care by Timing of AD Completion
Next, we examined care preferences by AD timing prior to death. Among those with ADs completed more than 10 years prior to death, about 3% of decedents elected aggressive care. This rate dipped to 1.8% for those completing ADs five to 10 years prior to death and increased to 4.6% and 5.0% for ADs completed between 25 and 59 months and seven to 24 months respectively. These rates more than double to 12% among those completing ADs in the last three months of life, decreasing to 3.9% for ADs completed in less than a month prior to death. See Figure 2.
Figure 2.
Percent Electing All Care Possible in AD by Timing between AD Completion and Death
Results from multivariate logistic regression (Table 2) indicate that timing was negatively associated with electing aggressive care, with odds of electing aggressive care reduced by .05% for each month prior to death the AD was completed (adjusted odds ratio, 0.995; 95% CI, 0.99 to 1.00). Findings shown in Table 2 indicate that minorities had significantly higher odds of electing aggressive care as compared with Whites (adjusted odds ratio, 6.69; 95% CI, 4.23 to 10.57). Additionally, having less than a high school education (adjusted odds ratio, 1.61; 95% CI, 0.03 to 1.04) was associated with greater odds of electing aggressive care while having an expected death reduced the odds of electing aggressive care by 52% (adjusted odds ratio, 0.32; 95% CI, 0.32 to 0.73).
DISCUSSION
This study is the first to examine timing of AD completion prior to death and we use a nationally representative dataset to do so. Our findings also illuminate differences in care preferences related to timing of AD completion, information that can inform physicians engaging in advance care planning. Our study found that the majority (60.6%) of ADs were completed more than two years prior to death and nearly three-quarters (71%) were completed a year or more before death.
Contrary to our research hypothesis, study findings show that early completion of an AD is not associated with a preference for more aggressive. Additionally, even ADs completed 10 years or more before death were associated with lower rates of preferences for aggressive care. This finding is in keeping with recent research that suggests that early adopters of ADs are more likely to prefer limited care than later adopters. (19) This pattern makes sense when you consider that our health system’s “standard” of care is aggressive care; thus, if you want to limit that care at end of life, you would be motivated to complete an AD. If you prefer aggressive care, you need not complete an AD. Moreover, studies have found that some patients cannot visualize future states that involve severe illness and disability and thus elect to forgo aggressive care.(20)
A key finding of our study was the higher prevalence of preference for aggressive care associated with ADs completed in the last three months of life. There are several potential explanations for this effect. As others have suggested, (8) these ADs may be the result of hurried discussions around urgent treatment procedures rather than in-depth goals of care discussion. Additionally, given the proximity to death, these conversations may have been conducted during a medical crisis or in-the-moment, (21) placing added pressure on patients and family members to make quick decisions about care preferences. Studies have found that decisions made during medical crisis may be incomplete, lack adequate conversation and understanding, and result in decisions that are uninformed. (22, 23) In a study of conversations on life-sustaining interventions, researchers found that many patients did not understand the decisions they were making and were often making these decisions autonomously, without physician input within a shared decision-making context. (22)
Another possibility may be that individuals completing ADs in the last months of life may represent a higher portion of those preferring aggressive care. Individuals completing ADs late in life may be doing so in response to pressure from the health care system, thus there may be a broader distribution of care preferences present in the ADs. This is supported by our findings demonstrating higher rates of ADs completed in the last months of life among ethnic minorities, who are generally more likely to prefer aggressive care(24, 25) and oftentimes are distrustful of the health care system.(26) A recent study on care preferences documented in POLST forms found significantly higher rates of documented preferences for aggressive care among an ethnically diverse California nursing facility sample (27) as compared with other studies of predominantly white nursing facility residents. Likewise, our study demonstrated a strong relationship between electing aggressive care and ADs among minority patients.(28) Finally, some of those completing ADs in the months immediately preceding death may be afraid of dying, thus electing to try all possible means to prolong survival up to the last weeks of life, when the fatality of the condition is more transparent and inevitable.
In considering the optimal moment for advance care planning and AD completion, timing may not be as important as quality of conversations, although additional research is needed to determine the quality of conversations related to AD completion in the last months of life.
Limitations
Our study examines written documentation of care preferences that may include documents other than advance directives (such as POLST of DNR). Additionally, it is not uncommon for patients to change their care preferences and subsequently their directive over the course of an illness and as illness progresses. (29) Our study does not include information about changes patients (or proxies) may have made in ADs over time nor does it delineate whether the AD was an original or revised document. Studies suggest that those with a living will (eg, documented health care preferences for life sustaining treatments) and those that elect to forgo aggressive treatment make very few changes in their care preference. (30,31) In a systematic review of stability of care preferences, researchers found that those with serious illness and individuals who engage in advance care planning have relatively stable care preferences over time. (29) However, other studies suggest that changes in health and psychological status influence changes in care preferences.(32) Additionally, our study relies on proxy reports of ADs and documented care preferences gathered after the death of a family member, and therefore may be biased due to emotional factors and memory limitations in recalling past events.
CONCLUSION
This study provides insight into policy recommendations for advance care planning and completion of ADs. Clinicians and researchers debate over timing of AD completion and advance care planning conversations. Our study suggests that early advance care planning and documentation of care wishes through ADs may not be associated with greater election of aggressive care, and that late ADs completed in the last months of life are associated with higher rates of preferences for aggressive care. This finding supports recommendations to begin advance care planning discussions early in the disease trajectory (21), particularly as studies have found that having an advance care discussion with a physician is highly associated with completing an AD before death.(33) Thus earlier conversations and documentation in medical records or through completion of ADs provides clinicians with documented knowledge of the patients’ values driving their care preferences. This documentation can provide the clinician with greater understanding of the patients’ core values as they near end of life.
Additional research is needed to understand the clinical context in which late AD decisions are being made, for example, whether the AD was developed in the presence or absence of life-threatening illnesses, and the quality of advance care planning discussions near end of life. Moreover, better understanding of factors related to patient decision-making in the last months of life will better inform practitioners.
Acknowledgments
Financial Support:
This study was funded by USC/UCLA Center on Biodemography and Population Health (P30-AG017265) and NIH (R00-AG039528). The funders had no involvement in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
All work was conducted at the Leonard Davis School of Gerontology, University of Southern California
REFERENCES
- 1.Morhaim DK, Pollack KM. End-of-life care issues: A personal, economic, public policy, and public health crisis. Am J Public Health. 2013;103(6):e8–e10. doi: 10.2105/AJPH.2013.301316. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Institute of Medicine. Dying in america: Improving quality and honoring individual preferences near the end of life. 2014 [Google Scholar]
- 3.CMS. Proposed policy, payment, and quality provisions changes to the medicare physician fee schedule for calendar year 2016. 2015 [Google Scholar]
- 4.Bischoff KE, Sudore R, Miao Y, Boscardin WJ, Smith AK. Advance care planning and the quality of end-of-life care in older adults. J Am Geriatr Soc. 2013;61(2):209–214. doi: 10.1111/jgs.12105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Silveira MJ, Kim SY, Langa KM. Advance directives and outcomes of surrogate decision making before death. New Engl J Med. 2010;362(13):1211–1218. doi: 10.1056/NEJMsa0907901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Teno JM, Gruneir A, Schwartz Z, Nanda A, Wetle T. Association between advance directives and quality of end-of-life care: A national study. J Am Geriatr Soc. 2007;55(2):189–194. doi: 10.1111/j.1532-5415.2007.01045.x. [DOI] [PubMed] [Google Scholar]
- 7.Mack JW, Weeks JC, Wright AA, Block SD, Prigerson HG. End-of-life discussions, goal attainment, and distress at the end of life: Predictors and outcomes of receipt of care consistent with preferences. J Clin Oncol. 2010;28(7):1203–1208. doi: 10.1200/JCO.2009.25.4672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Billings JA, Bernacki R. Strategic targeting of advance care planning interventions: The goldilocks phenomenon. JAMA Intern Med. 2014;174(4):620–624. doi: 10.1001/jamainternmed.2013.14384. [DOI] [PubMed] [Google Scholar]
- 9.Barclay S, Momen N, Case-Upton S, Kuhn I, Smith E. End-of-life care conversations with heart failure patients: a systematic literature review and narrative synthesis. Br J Gen Pract. 2011;61(582):e49–e62. doi: 10.3399/bjgp11X549018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Heyland DK, Barwich D, Pichora D, et al. Failure to engage hospitalized elderly patients and their families in advance care planning. JAMA Intern Med. 2013;173(9):778–787. doi: 10.1001/jamainternmed.2013.180. [DOI] [PubMed] [Google Scholar]
- 11.Ahluwalia SC, Enguidanos S. Advance care planning among patients with heart failure: A review of challenges and approaches to better communication. JCOM. 2015;22(2):73–82. [Google Scholar]
- 12.Knauft E, Nielsen EL, Engelberg RA, Patrick DL, Curtis J. Barriers And Facilitators To End-Of-Life Care Communication For Patients With COPD. Chest. 2005;127(6):2188–2196. doi: 10.1378/chest.127.6.2188. [DOI] [PubMed] [Google Scholar]
- 13.Robinson, Louise, et al. A qualitative study: Professionals’ experiences of advance care planning in dementia and palliative care, ‘a good idea in theory but…’. Palliative Medicine. 2013;27.5:401–408. doi: 10.1177/0269216312465651. [DOI] [PubMed] [Google Scholar]
- 14.Mack JW, Smith TJ. Reasons why physicians do not have discussions about poor prognosis, why it matters, and what can be improved. J Clin Oncol. 2012;30(22):2715–2717. doi: 10.1200/JCO.2012.42.4564. [DOI] [PubMed] [Google Scholar]
- 15.Enguidanos S, Housen P, Goldstein R, Vesper E, Allen J, Braun W. Physician and nurse perceptions of a new inpatient palliative care consultation project: implications for education and training. J Palliat Med. 2009;12(12):1137–1142. doi: 10.1089/jpm.2009.0131. [DOI] [PubMed] [Google Scholar]
- 16.Tung EE, North F. Advance Care Planning in the Primary Care Setting: A Comparison of Attending Staff and Resident Barriers. J Hosp Palliat Care. 2009;26(6):456–463. doi: 10.1177/1049909109341871. [DOI] [PubMed] [Google Scholar]
- 17.Sonnega A, Faul JD, Ofstedal MB, Langa KM, Phillips JW, Weir DR. Cohort profile: The health and retirement study (HRS) Int J Epidemiol. 2014;43(2):576–585. doi: 10.1093/ije/dyu067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gozalo P, Teno JM, Mitchell SL, Skinner J, Bynum J, Tyler D, Mor V. End-of-life transitions among nursing home residents with cognitive issues. NEJM. 2011;365(13):1212–1221. doi: 10.1056/NEJMsa1100347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Pew Research Center. Views on end-of-life medical treatments. Pew Res Cent Relig Public Life Proj. 2013 [Google Scholar]
- 20.Halpern J, Arnold RM. Affective forecasting: an unrecognized challenge in making serious health decisions. J Gen Intern Med. 2008;23(10):1708–1712. doi: 10.1007/s11606-008-0719-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sudore RL, Fried TR. Redefining the "planning" in advance care planning: Preparing for end-of-life decision making. Ann Intern Med. 2010;153(4):256–261. doi: 10.1059/0003-4819-153-4-201008170-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Deep KS, Griffith CH, Wilson JF. Communication and decision making about life-sustaining treatment: Examining the experiences of resident physicians and seriously-ill hospitalized patients. J Gen Intern Med. 2008;23(11):1877–1882. doi: 10.1007/s11606-008-0779-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Anderson W, Chase R, Pantilat S, et al. Code status discussions between attending hospitalist physicians and medical patients at hospital admission. J Gen Intern Med. 2011;26(4):359–366. doi: 10.1007/s11606-010-1568-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Johnson KS, Kuchibhatla M, Tulsky JA. What explains racial differences in the use of advance directives and attitudes toward hospice care? J Am Geriatr Soc. 2008;56(10):1953–1958. doi: 10.1111/j.1532-5415.2008.01919.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Garrido MM, Harrington ST, Prigerson HG. End-of-life treatment preferences: A key to reducing ethnic/racial disparities in advance care planning? Cancer. 2014;120(24):3981–3986. doi: 10.1002/cncr.28970. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Washington KT, Bickel-Swenson D, Stephens N. Barriers to hospice use among African Americans: A systematic review. Health Soc Work. 2008;33:267–274. doi: 10.1093/hsw/33.4.267. [DOI] [PubMed] [Google Scholar]
- 27.Rahman A, Bressette M, Gassoumis Z, Enguidanos S. Nursing home residents' preferences on physician orders for life sustaining treatment (POLST) The Gerontologist. doi: 10.1093/geront/gnv019. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hickman SE, Nelson CA, Moss AH, et al. The consistency between treatments provided to nursing facility residents and orders on the physician orders for life-sustaining treatment form. JAGS. 2011;59(11):2091–2099. doi: 10.1111/j.1532-5415.2011.03656.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ditto PH, Jacobson JA, Smucker WD, et al. Context changes choices: A prospective study of the effects of hospitalization on life-sustaining treatment preferences. Med Decis Making. 2006;26(4):313–322. doi: 10.1177/0272989X06290494. [DOI] [PubMed] [Google Scholar]
- 30.Ditto PH, Smucker WD, Danks JH, Jacobson JA, Houts RM, Fagerlin A, Coppola KM, Gready RM. Stability of older adults' preferences for life-sustaining medical treatment. Health Psychol. 2003;22(6):605–615. doi: 10.1037/0278-6133.22.6.605. [DOI] [PubMed] [Google Scholar]
- 31.Auriemma CL, Nguyen CA, Bronheim R, et al. Stability of end-of-life preferences: A systematic review of the evidence. JAMA Intern Med. 2014;174(7):1085–1092. doi: 10.1001/jamainternmed.2014.1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Janssen DJ, Spruit MA, Schols JM, Cox B, Nawrot TS, Curtis JR, Wouters EF. Predicting changes in preferences for life-sustaining treatment among patients with advanced chronic organ failure. Chest. 41(5):1251–1259. doi: 10.1378/chest.11-1472. 12012. [DOI] [PubMed] [Google Scholar]
- 33.Alano, Gloria J, et al. Factors influencing older adults to complete advance directives. Pall and Supp Care. 2010:267–275. doi: 10.1017/S1478951510000064. [DOI] [PubMed] [Google Scholar]