Abstract
Gardner syndrome is known as a variant of familial adenomatous polyposis. This syndrome is characterized by multiple intestinal polyposes, osteomas, and epidermoid cysts. In addition, dental abnormalities include an increased frequency of multiple odontomas, as well as supernumerary and impacted teeth. The authors report the case of a 7-year-old male patient with Gardner syndrome. Radiographic findings revealed multiple osteomas in both sides of the maxilla, multiple diffuse enostoses in both jaws, and a complex odontoma in the left mandibular body. Two years later, multiple epidermoid cysts on the scalp were found. Since this patient was suspected to have Gardner syndrome, the authors recommended gastrointestinal endoscopy to check for intestinal polyposis. Gastrointestinal endoscopic examination revealed multiple polyposes in the upper gastrointestinal tract and fundus of the stomach. As a result, the final diagnosis was Gardner syndrome.
Keywords: Gardner Syndrome; Osteoma; Adenomatous Polyposis Coli; Radiography, Dental
Gardner syndrome is considered a phenotypic variant of familial adenomatous polyposis.1,2 Different mutations in the adenomatous polyposis coli gene have been shown to be associated with Gardner syndrome.3,4 Gardner syndrome includes intestinal polyposis,1 multiple epidermoid cysts,5 osteomas,6 dental anomalies,4 and congenital hypertrophy of the retinal pigment epithelium.2 Chimenos-Küstner et al.7 reported that approximately 50% of these patients presented with 3 or more osteomas in the maxillae as well as in other locations. Ida et al.8 reported that Gardner syndrome should be considered if more than 3 osteomas are present. However, Herrmann et al.1 reported that only the presence of intestinal polyposis was a marker of Gardner syndrome. The intestinal polyposes have a 100% potential for malignant change,9,10 which usually occurs in the third to fifth decades of life.11,12 Due to the presence of multiple osteomas, multiple enostoses and dental abnormalities could often develop in the first or second decades of life, before the occurrence of intestinal polyposis,4 meaning that the early diagnosis of this syndrome might be a life-saving event. Therefore, dentists may play an important role for these patients.
Herein, we report a rare case of Gardner syndrome that was suspected before the detection of intestinal polyposis.
Case Report
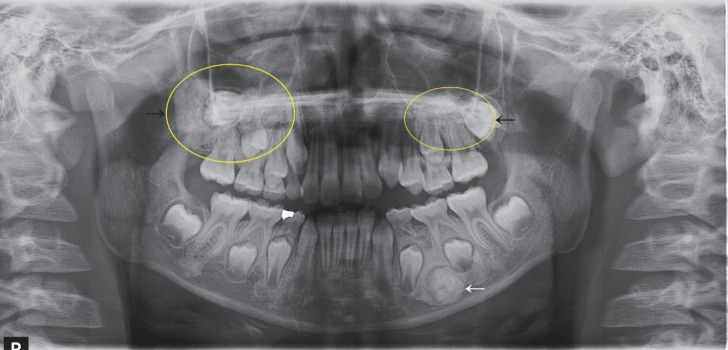
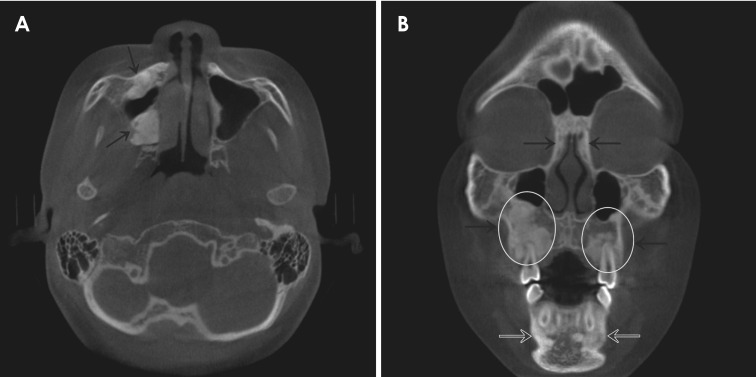
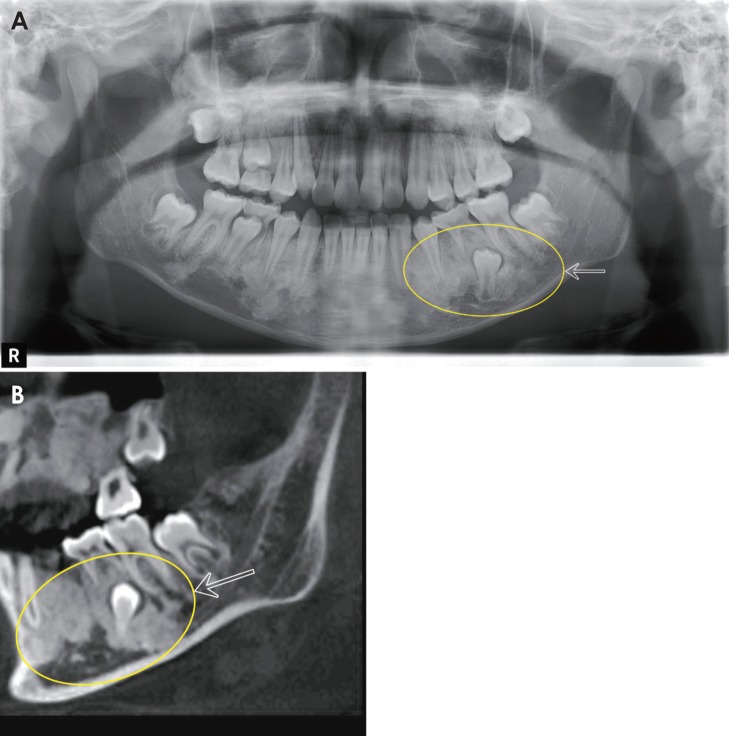
A 7-year-old boy was referred to the Chonbuk National University Dental Hospital from a dental clinic in February 2012 for the further evaluation of radiopaque masses in the left mandibular body on panoramic view. A panoramic radiograph showed relatively well-defined multiple radiopacities in both maxillary posterior regions encroaching the maxillary sinuses, a well-defined round radiopacity surrounded by a radiolucent line in the left mandibular premolar area, and multiple diffuse radiopacities in both jaws (Fig. 1). A post-enhanced computed tomographic (CT) image showed multiple mildly enhanced soft tissue masses on the subcutaneous areas of the scalp (Fig. 2). Cone-beam CT (CBCT) images showed multiple radiopaque masses in the right maxilla encroaching the maxillary sinus (Fig. 3A, black arrows), multiple diffuse radiopacities in the mandible (Fig. 3B, white open arrows), and multiple radiopacities encroaching the maxillary sinuses and ethmoidal sinuses (Fig. 3B, black arrows).
Fig. 1. A panoramic image shows relatively well-defined multiple radiopacities in both maxillary posterior regions encroaching the maxillary sinuses (black arrows), a well-defined round radiopacity surrounded with a radiolucent line in the left mandibular premolar area (white arrow), and multiple diffuse radiopacities in both jaws.
Fig. 2. A post-enhanced coronal computed tomography image shows multiple mildly enhanced soft tissue masses on the subcutaneous areas of the scalp.
Fig. 3. A. An axial cone-beam computed tomography (CBCT) image shows multiple radiopaque masses in the right maxilla encroaching the maxillary sinus (black arrows). B. A coronal CBCT image shows multiple diffuse radiopacities in the mandible (white open arrows), and multiple radiopacities encroaching the maxillary sinuses and ethmoidal sinuses (black arrows).
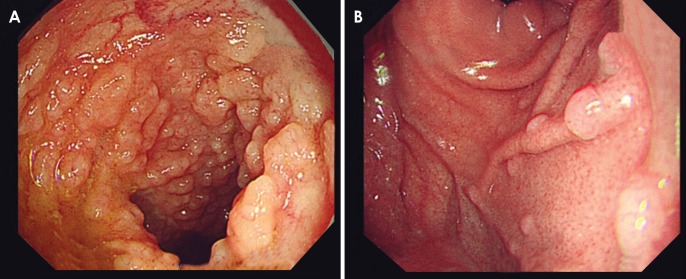
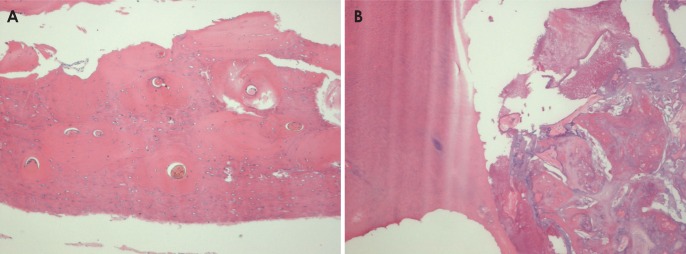
According to the medical history obtained at the Department of Dermatology in May 2008, the patient had multiple subcutaneous nodules on the scalp and the back without any clinical symptoms. In August 2010, histopathological findings of the lesions on the scalp (Fig. 4) revealed multiple epidermoid cysts (Fig. 5). In January 2014, because the patient exhibited multiple radiopaque masses in both jaws and multiple epidermoid cysts on the scalp, this case was suspected to be Gardner syndrome by diagnosticians at the Department of Oral and Maxillofacial Radiology. Therefore, a gastrointestinal endoscopy was recommended. In January 2015, a gastrointestinal endoscopic examination revealed multiple polyposes in the upper gastrointestinal tract (Fig. 6A) and fundus of the stomach (Fig. 6B). As a result, the final diagnosis was Gardner syndrome. This patient had no familial history of major illness. The multiple epidermoid cysts on the glabella and scalp were excised, and osteoma of the exposed bone on the vertex was removed at the Department of Plastic Surgery. Additionally, an osteoma in the right maxillary tuberosity (Fig. 7A) and a complex odontoma in the left mandibular body (Fig. 7B) were removed at the Department of Oral and Maxillofacial Surgery. Radiographic images revealed that the sizes of the radiopaque masses were the same as those observed in 2012. Two years later, delayed eruption of the left mandibular second premolar was observed (Fig. 8) (white open arrows). Therefore, the orthodontic treatment of the left mandibular second premolar is in process.
Fig. 4. A photograph of the patient's scalp shows multiple nodules on the scalp.

Fig. 5. Histopathologic examination of the nodules on the scalp shows a cystic wall with lining epithelium (H&E stain, ×200).
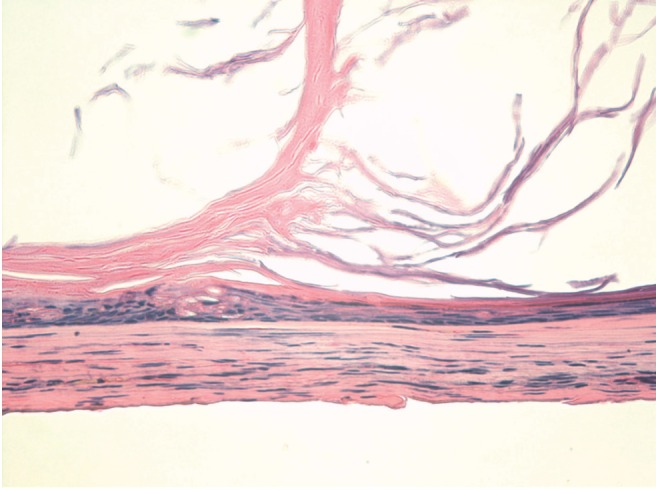
Fig. 6. A. An endoscopic examination shows multiple polyposes on the upper gastrointestinal tract. B. Endoscopic examination showing multiple polyposes on the fundus of the stomach.
Fig. 7. A. A photomicrograph of the decalcified section of the radiopaque mass in right maxillary posterior region shows dense and lamellar cortical bone with narrow bone marrow spaces (H&E stain, ×50). B. A photomicrograph of the decalcified section of radiopaque mass in the left mandibular body shows irregularly deposited cementum, dentin, and enamel matrix (H&E stain, ×50).
Fig. 8. A. Two years after removal of the complex odontoma in the left mandibular body and osteoma in the right tuberosity, a panoramic image shows the remaining radiopaque lesions in both sides of the maxilla and diffuse enostoses in both jaws (white open arrow). B. A sagittal cone-beam computed tomography image shows multiple enostoses with impaction of the left mandibular second premolar (white open arrow).
Discussion
Some studies have reported that 30%-75% of patients with Gardner syndrome have dental anomalies,9,13 and that 68%-82% of patients with familial adenomatous polyposis have osteomas.13,14 Cankaya et al.15 reported a case of a Gardner syndrome with jaw deformities.
Osteomas are benign tumors composed of mature compact or medullary bone and are classified as either peripheral or central.6,16 The most common site for the occurrence of osteomas is the mandible, where they appear as radiopaque masses attached to the surface of the cortex. They may be attached by a broad base, or they may be pedunculated. In the skull, osteomas form on the surface of the external table, and they may also project in the sinuses.17 However, the osteomas that originate in the bone medulla mimic enostoses.7 The central portion of the jaws may exhibit multiple areas of radiopacity. Enostoses are localized growths of compact bone that extend from the endosteal surface of cortical bone into the cancellous bone. They are more common in the mandible than in the maxilla. Their periphery is usually well defined but occasionally blends into the surrounding bone. However, they have no radiolucent line surrounding the radiopaque mass. The internal structure of an enostosis usually appears as a homogeneous radiopacity. In very rare cases, enostoses can inhibit the eruption of a tooth. The present case had multiple enostoses in both jaws, and the eruption of the left mandibular second premolar was delayed by the adjacent enostoses.
Compound odontomas17 and hypercementosis4,9,18 have also been reported to develop in patients with Gardner syndrome. The present case showed a complex odontoma in the left mandibular body and impacted teeth with multiple enostoses, but the involved teeth did not show hypercementosis.
It is important for dentists to be aware of this syndrome, since multiple osteomas often precede the onset of colonic polyps.6 The osteomas of the jaw most frequently appear during the second and third decades of life,7 and they are often detected due to a deformity of the jaw or face. These patients are then frequently seen by a dentist before any symptoms in the colon are apparent. Since malignant changes occur in 100% of these polyps, and because the syndrome is transmitted as an autosomal dominant trait, the familial history should be checked.9
The radiographic findings of this patient revealed osteomas in both sides of the maxilla encroaching the maxillary sinuses, ethmoidal sinuses, and calvaria. Additionally, the dental radiographs revealed multiple enostoses in both the maxilla and mandible. However, Herrmann et al.1 reported that the concomitant occurrence of multiple epidermoid cysts, osteomas, and thyroid gland nodules may not be diagnostic for Gardner syndrome in the absence of intestinal polyposis. Since the radiographic findings of this patient showed multiple osteomas, multiple enostoses, and a complex odontoma, the authors were able to suspect Gardner syndrome before the detection of intestinal polyposis. In light of the association between osteomas of the jaw and multiple intestinal polyposes, it seemed reasonable to suspect Gardner syndrome. This patient and his family members had no history of malignancy or familial history of familial adenomatous polyposis.
Multiple radiopaque masses should be differentiated from florid osseous dysplasia (FOD)19 or familial gigantiform cementoma.12,20 FOD is a widespread form of periapical cemental dysplasia (PCD). Normal cancellous bone is replaced with dense, cemento-osseous tissue in fibrous connective tissue. FOD lesions usually are bilateral and present in both jaws. The lesions usually occur in periapical and interdental areas. In the mandible, lesions occur above the mandibular canal. They usually have well-defined borders similar to PCD. The internal structure can vary from mixed radiolucent and radiopaque regions to radiopaque areas according to the growth stage of the lesions. The radiopaque regions show an amorphous area of calcification. These calcified masses are similar in appearance to those seen in mature PCD lesions. Large FOD lesions can displace the mandibular canal inferiorly, displace the antral floor superiorly, and cause expansion of the jaw.19 The well-defined nature of FOD with its radiolucent line is useful in radiographic findings for making the differential diagnosis. CBCT and CT images of this patient showed multiple well-defined radiopacities, but the multiple radiopaque lesions did not show surrounding radiolucent lines, except for the radiopaque mass in the left mandibular body region.
On the basis of the simultaneous observation of multiple osteomas, complex odontoma, and multiple enostoses, we were able to predict a diagnosis of Gardner syndrome before the detection of intestinal polyposis. Thus, dentists might have an important role to play in the early diagnosis of Gardner syndrome.
References
- 1.Herrmann SM, Adler YD, Schmidt-Petersen K, Nicaud V, Morrison C, Paul M, et al. The concomitant occurrence of multiple epidermal cysts, osteomas and thyroid gland nodules is not diagnostic for Gardner syndrome in the absence of intestinal polyposis: a clinical and genetic report. Br J Dermatol. 2003;149:877–883. doi: 10.1046/j.1365-2133.2003.05640.x. [DOI] [PubMed] [Google Scholar]
- 2.Tan KL, Wilson S, O'Neill C, Gordon D, Napier S. Something not quite right: Gardner syndrome diagnosed by multiple cutaneous lesions and genetic testing. Surgeon. 2005;3:412–415. doi: 10.1016/s1479-666x(05)80052-6. [DOI] [PubMed] [Google Scholar]
- 3.Fearnhead NS, Britton MP, Bodmer WF. The ABC of APC. Hum Mol Genet. 2001;10:721–733. doi: 10.1093/hmg/10.7.721. [DOI] [PubMed] [Google Scholar]
- 4.Ramaglia L, Morgese F, Filippella M, Colao A. Oral and maxillofacial manifestations of Gardner's syndrome associated with growth hormone deficiency: case report and literature review. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2007;103:e30–e34. doi: 10.1016/j.tripleo.2007.01.013. [DOI] [PubMed] [Google Scholar]
- 5.Perniciaro C. Gardner's syndrome. Dermatol Clin. 1995;13:51–56. [PubMed] [Google Scholar]
- 6.Herford AS, Stoffella E, Tandon R. Osteomas involving the facial skeleton: a report of 2 cases and review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol. 2013;115:e1–e6. doi: 10.1016/j.oooo.2011.09.033. [DOI] [PubMed] [Google Scholar]
- 7.Chimenos-Küstner E, Pascual M, Blanco I, Finestres F. Hereditary familial polyposis and Gardner's syndrome: contribution of the odonto-stomatology examination in its diagnosis and a case description. Med Oral Patol Oral Cir Bucal. 2005;10:402–409. [PubMed] [Google Scholar]
- 8.Ida M, Nakamura T, Utsunomiya J. Osteomatous changes and tooth abnormalities found in the jaw of patients with adenomatosis coli. Oral Surg Oral Med Oral Pathol. 1981;52:2–11. doi: 10.1016/0030-4220(81)90164-x. [DOI] [PubMed] [Google Scholar]
- 9.Butler J, Healy C, Toner M, Flint S. Gardner syndrome - review and report of a case. Oral Oncol Extra. 2005;41:89–92. [Google Scholar]
- 10.Lew D, DeWitt A, Hicks RJ, Cavalcanti MG. Osteomas of the condyle associated with Gardner's syndrome causing limited mandibular movement. J Oral Maxillofac Surg. 1999;57:1004–1009. doi: 10.1016/s0278-2391(99)90026-5. [DOI] [PubMed] [Google Scholar]
- 11.Bilkay U, Erdem O, Ozek C, Helvaci E, Kilic K, Ertan Y, et al. Benign osteoma with Gardner syndrome: review of the literature and report of a case. J Craniofac Surg. 2004;15:506–509. doi: 10.1097/00001665-200405000-00032. [DOI] [PubMed] [Google Scholar]
- 12.Lee BD, Lee W, Oh SH, Min SK, Kim EC. A case report of Gardner syndrome with hereditary widespread osteomatous jaw lesions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2009;107:e68–e72. doi: 10.1016/j.tripleo.2008.10.018. [DOI] [PubMed] [Google Scholar]
- 13.Wolf J, Jarvinen HJ, Hietanen J. Gardner's dento-maxillary stigmas in patients with familial adenomatosis coli. Br J Oral Maxillofac Surg. 1986;24:410–416. doi: 10.1016/0266-4356(86)90054-9. [DOI] [PubMed] [Google Scholar]
- 14.Carl W, Sullivan MA. Dental abnormalities and bone lesions associated with familial adenomatous polyposis: report of cases. J Am Dent Assoc. 1989;119:137–139. doi: 10.14219/jada.archive.1989.0142. [DOI] [PubMed] [Google Scholar]
- 15.Cankaya AB, Erdem MA, Isler SC, Cifter M, Olgac V, Kasapoglu C, et al. Oral and maxillofacial considerations in Gardner's syndrome. Int J Med Sci. 2012;9:137–141. doi: 10.7150/ijms.3989. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ortakoglu K, Gunaydin Y, Aydintug YS, Safali M. Osteoma of the mandibular condyle: report of a case with 5-year follow-up. Mil Med. 2005;170:117–120. [PubMed] [Google Scholar]
- 17.Fonseca LC, Kodama NK, Nunes FC, Maciel PH, Fonseca FA, Roitberg M, et al. Radiographic assessment of Gardner's syndrome. Dentomaxillofac Radiol. 2007;36:121–124. doi: 10.1259/dmfr/18554322. [DOI] [PubMed] [Google Scholar]
- 18.Madani M, Madani F. Gardner's syndrome presenting with dental complaints. Arch Iran Med. 2007;10:535–539. [PubMed] [Google Scholar]
- 19.Melrose RJ, Abrams AM, Mills BG. Florid osseous dysplasia. A clinical-pathologic study of thirty-four cases. Oral Surg Oral Med Oral Pathol. 1976;41:62–82. doi: 10.1016/0030-4220(76)90254-1. [DOI] [PubMed] [Google Scholar]
- 20.Waldron C. Bone pathology. Oral and maxillofacial pathology. Philadelphia: WB Saunders Comp; 1995. pp. 460–491. [Google Scholar]