Highlights
-
•
Prevalence of reflux after sleeve gastrectomy.
-
•
Introduction of new device to treat reflux after sleeve gastrectomy.
-
•
The use of LINX system in treating reflux after sleeve gastrectomy.
Keywords: Case report, Reflux, GERD, Sleeve gastrectomy, Roux-en-Y gastric bypass, LINX®
Abstract
Introduction
Management of severe reflux after sleeve gastrectomy (SG) usually requires converting to Roux-en-y gastric bypass (RYGB). We present a case of managing this problem using the LINX® system.
Presentation of case
In February 2015, we performed a laparoscopic placement of LINX® system to treat severe reflux after sleeve gastrectomy on a 25-year-old female. The operative time was 47 min. There were no intra or postoperative complications. The hospital stay was one day. The postoperative UGI showed no reflux. Ten days after surgery her Quality of life score (QOL) changed from 64/75 to 7/75 after the LINX® placement. One year later the patient continued to enjoy no reflux and stayed off medication.
Discussion
Reflux after sleeve gastrectomy is usually managed by conversion to RYGB by most surgeons. This case report opens the door for an alternative management of this problem while maintaining the original sleeve gastrectomy. This technique is reasonably easy to perform in comparison to the conversion to RYGB with less potential post-operative complications. A one year follow up showed good control of reflux without medication.
Conclusion
Laparoscopic placement of the LINX® system to correct severe reflux after sleeve gastrectomy is a safe alternative procedure to conversion to a RYGB.
1. Introduction
Sleeve gastrectomy is gaining wide acceptance as the procedure of choice surpassing RYGB [1]. Several reports have shown an increase in de novo reflux, as well as worsening of pre-operative reflux in some patients [2], [3], [4]. Management of this problem is usually medical with proton pump inhibitors (PPI). After medical management, conversion to RYGB is usually recommended for severe reflux that is uncontrolled medically [5]. With our experience in placing the LINX® system for managing reflux in non-obese patients, we decided to offer this procedure to one of the patients who had been suffering from severe uncontrolled reflux after sleeve gastrectomy. The patient had failed medical management over a two-year period and did not want to have conversion of her SG to RYGB. The patient did not have dilation of her gastric pouch. The LINX® system (Torax Medical, Inc., Shoreview, MN, USA) was approved by the FDA in 2012 for the treatment of refractory esophageal reflux by using magnetic beads to augment the lower esophageal sphincter. This system was introduced as an alternative to the traditional Nissen fundoplication technique in controlling the esophageal reflux [6], [7]. This case has been reported in line with the SCARE Group [8].
2. Presentation of case
A 25-year-old female presented to our office two and half years after having SG in September 2013 at another institution. The patient’s initial weight before the SG was 282 lbs. with a BMI of 54.2 kg/m2. She had a history of reflux before her SG surgery. The patient lost 109 lbs. with total percent excess BMI loss (%EBL) of 96.2%. Her reflux, however, did not improve with this great weight loss in spit of intense medical management using double dose PPI for over two years. At the time of her presentation, unfortunately, her reflux became worse and her quality of life score. using the GERD-HRQL symptom severity instrument, increased from 30/75 before the SG to 64/70 after surgery [9]. Her weight was 173 lbs. and her BMI was 27.9 kg/m2. Her pre-operative upper gastro-intestinal contrast study (UGI) showed a small hiatal hernia with reflux (Fig. 1). There was no dilatation in the proximal gastric pouch. Her upper endoscopy with a Bravo pH capsule (GIVIN imaging, Duluth, GA) showed esophagitis with small hiatal hernia. Her pH DeMeester score was 66.6 (normal <14.7). Her esophageal motility was normal. The patient was offered the placement of the LINX® system to augment the lower esophageal sphincter pressure and to prevent the transient lower esophageal sphincter relaxation (TLESR) along with repair of the small hiatal hernia. She was advised about the novelty of this approach and that there were no reports of this procedure being done after SG in the United Stats so far. She was also advised that the normal management of her reflux problem would be by a conversion of the SG to RYGB. Other bariatric surgeons had offered her this option and she had declined it. Because the patient did not have dilation in her proximal gastric pouch, she could not be a candidate for the use of such gastric dilation as an anterior fundoplication to correct her reflux.
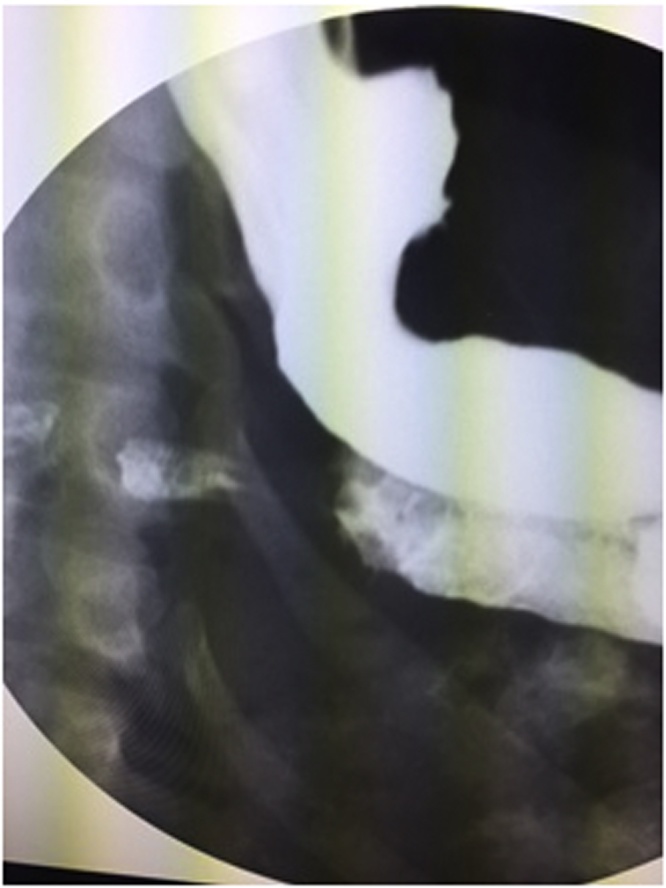
Fig. 1.
Pre-operative upper gastrointestinal X-Ray: Hiatal hernia with reflux.
In February 2015 the patient underwent laparoscopic repair of the small hiatal hernia and placement of the LINX® system. The operation went without any intra-operative or post-operative complications. The operative time was 47 min. The hospital stay was one day. Her post-operative UGI showed no reflux (Fig. 2). Ten days after the procedure the patient’s HQOL score went down to 7/70 and she had stopped the use of PPI completely. There were no 30-day or 90-day post operative complications. In June 2015, her repeat UGI showed no reflux. A recent follow up of the patient one year post-LINX® placement showed continued resolution of her symptoms. The patient was very happy with her results, however, she refused to repeat the upper endoscopy or allow re-measurement of her DeMeester score.
Fig. 2.
Post-operative upper gastrointestinal X-Ray: LINX in position with no reflux.
3. Technique
The procedure was done using the same trocars positioning as with the SG. There were four trocars and five incisions. Lysis of adhesions was done over the proximal stomach and the esophagus. The crura of the diaphragm were exposed. The small hiatal hernia was identified and repaired using 0-Ethibond sutures to allow the hiatus to accept a 60 fr. bougie. The bougie was then removed to be able to size the esophagus without any stretching. The posterior vagus nerve was identified and the LINX® system’s sizer was placed between the posterior vagus nerve and esophagus. It was very important to not to stretch the esophagus. In addition, there could not be any tubes inside the esophagus as this would preclude accurate measurement of the esophagus at a resting state. The measurement was repeated several times to assure accuracy and prevent placement of the wrong size device. A 14 mm LINX® device was then selected and introduced into the abdomen through the LUQ 10 mm trocar site. The LINX® system was placed around the esophagus anterior to the posterior vagus nerve and buckled in place to augment the lower esophageal sphincter pressure, hence, control the esophageal reflux (Fig. 3). A video of the technique can be viewed at: https://www.youtube.com/watch?v=fjC0r88zz54
Fig. 3.
Intra-operative image of the LINX system in place.
4. Discussion
In patients who develop de novo reflux, some dilation in the proximal gastric pouch may be present and may be blamed for the development of reflux. In others, however, there is no dilation of the proximal gastric pouch where the weakening of the lower esophageal sphincter or the TLESR is the only reason for the development of their de novo reflux [5], [10], [11]. The presence or development of a hiatal hernia may be a contributing factor as well. Until now, managing such patients has been through conversion of the SG to RYGB [12]. In patients who develop dilation in the proximal gastric pouch; however, the senior author (AH) has performed an anterior fundoplication as an alternative method to the conversion to RYGB to correct both the dilated gastric pouch and the reflux problem with excellent results [13]. At the time when we did this procedure, there were no reports on management of this problem using the LINX® system in the bariatric literature. Later, however, in July 2015, the BenDavid group in Florida reported online [14] a series of such procedures in managing their patients’ reflux after SG with the LINX® system with good results. Their follow up, however, was only 2–4 weeks’ post-surgery.
The use of the LINX® device in patients who develop reflux after SG are encouraging, as patients are able to avoid being converted to RYGB. In the last two months of 2015 we performed this procedure on three additional patients with same good short term results.
5. Conclusion
Until recently, patients who developed reflux after sleeve gastrectomy or suffered from worsening of their reflux had no other option to treat their condition except by conversion of their SG into RYGB. In our patient, the LINX® system controlled the symptoms of reflux after SG. It is a safe operation with a relatively short operative time and minimal complications if any. The ability of keeping the SG without conversion to RYGB should be an option for these patients who suffer from uncontrolled reflux after SG. To our knowledge, this is the first case report in the literature that addresses the treatment of severe uncontrolled reflux after sleeve gastrectomy using a new device with one year follow up.
Conflict of interest
No conflict of interest.
Author contribution
Abdelkader Hawasli, MD: Original idea and design.
Mark Tarakji, MD: Review of manuscript and preparation of the video.
Moayad Tarboush, MD: Collecting data on patient.
Ahmed Meguid, MD: Review and edit manuscript.
Funding
No funding.
Ethical approval
IRB has reviewed this case.
Consent
The IRB reviewed and approved this case report.
Guarantor
Abdelkader Hawasli, MD.
Acknowledgment
The authors would like to acknowledge the contributions of Susan Szpunar, PhD. in reviewing this manuscript.
Footnotes
Supplementary data associated with this article can be found, in the online version, at http://dx.doi.org/10.1016/j.ijscr.2016.11.050.
Appendix A. Supplementary data
The following is Supplementary data to this article:
References
- 1.Reames B.N., Finks J.F., Bacal D., Carlin A.M., Dimick J.B. Changes in bariatric surgery procedure use in Michigan. JAMA. 2014;312(September (9)):959–961. doi: 10.1001/jama.2014.7651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Bragheto L., Csendes A., Lanzarini E., Papapietro K., Carcamo C., Molina J. Is laparoscopic sleeve gastrectomy an acceptable primary bariatric procedure in obese patients? Early and 5-year postoperative results. Surg. Laparosc. Endosc. Percutaneous Tech. 2012;22:479–486. doi: 10.1097/SLE.0b013e318262dc29. [DOI] [PubMed] [Google Scholar]
- 3.Lacy A., Ibarzabal A., Pando E., Adelsdorfer C., Delitala A., Corcelles R., Delgado S., Vidal J. Revisional surgery after sleeve gastrectomy. Surg. Laparosc. Endosc. Percutaneous Tech. 2010;20:428. doi: 10.1097/SLE.0b013e3181f62895. [DOI] [PubMed] [Google Scholar]
- 4.Keidar A., Appelbaum L., Schweiger C., Elazary R., Baltasar A. Dilated upper sleeve can be associated with severe postoperative gastroesophageal dysmotility and reflux. Obes. Surg. 2010;20:140–147. doi: 10.1007/s11695-009-0032-3. [DOI] [PubMed] [Google Scholar]
- 5.Kleidi E., Theodorou D., Albanopoulos K., Menenakos E., Karvelis M.A., Papailiou J., Stamou K., Zografos G., Katsaragakis S., Leandros E. The effect of laparoscopic sleeve gastrectomy on the antireflux mechanism: can it be minimized? Surg. Endosc. 2013:9. doi: 10.1007/s00464-013-3083-4. [DOI] [PubMed] [Google Scholar]
- 6.Reynolds J.L., Zehetner J., Bildzukewicz N., Katkhouda N., Dandekar G., Lipham J.C. Magnaetic sphincter augmentation with th LINX device for gastroesophageal reflux disease after U.S. Food and Drug Administration approval. Am. Surg. 2014;80(10):1034–1038. [PubMed] [Google Scholar]
- 7.Bonavina L., DeMeesterT. Fockens P., Dunn D., Saino G., Bona D., Lipham J., Bemelman W., Ganz R.A. Laparoscopic sphincter augmentation device eliminates reflux symptoms and normalizes esophageal acid exposure: one and 2-year results of feasibility trial. Ann. Surg. 2010;252(5):857–862. doi: 10.1097/SLA.0b013e3181fd879b. [DOI] [PubMed] [Google Scholar]
- 8.Agha R.A., Fowler A.J., Saeta A., Barai I., Rajmohan S., Orgill D.P., SCARE Group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34(October):180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 9.Velanovich V. The development of GERD-HRQL symptom severity instrument. Dis. Esophagus. 2007;20:130–134. doi: 10.1111/j.1442-2050.2007.00658.x. [DOI] [PubMed] [Google Scholar]
- 10.Braghetto I., Lanzarini E., Korn O., Valladares H., Molina J.C., Henriquez A. Manometric changes of the lower esophageal sphincter after sleeve gastrectomy in obese patients. Obes. Surg. 2010;20:357–362. doi: 10.1007/s11695-009-0040-3. [DOI] [PubMed] [Google Scholar]
- 11.Mittal R.K., Holloway R.H., Penagini R., Blackshaw L.A., Dent J. Transient lower esophageal sphincter relaxation. Gastroenterology. 1995;109(2):601–610. doi: 10.1016/0016-5085(95)90351-8. [DOI] [PubMed] [Google Scholar]
- 12.Mahawar K., Jennings N., Balupuri S., Small P. Sleeve gastrectomy and gastro-oesophageal reflux disease: a complex relationship. Obes. Surg. 2013;23:987–991. doi: 10.1007/s11695-013-0899-x. [DOI] [PubMed] [Google Scholar]
- 13.Hawasli A., Bush A., Hare B., Meguid A., Thatimatla N., Szpunar S. Laparoscopic management of severe reflux after sleeve gastrectomy, in selected patients, without conversion to roux-en-Y gastric bypass. J. Laparoendosc. Adv. Surg. Tech. 2015;2(August (58)):631–635. doi: 10.1089/lap.2015.0079. [DOI] [PubMed] [Google Scholar]
- 14.Desart K., Rossidis G., Michel M., Lux T., Ben-David K. Gatroesophageal reflux management with the LINX system for gastroesophageal reflux disease following laparoscopic sleeve gastrectomy. J. Gastrointest. Surg. 2015 doi: 10.1007/s11605-015-2887-z. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.