Introduction
Focal fatty replacement is a common degenerative lesion of pancreas. Total fat replacement of pancreas is rare. Pancreatic lipomatosis is seen as fatty infiltration or replacement of part or whole of the pancreas. The exact etiopathogenesis behind fatty replacement is unknown; however, it is reported to be associated with elderly age; obesity; diseases such as diabetes mellitus, Cushing disease, chronic pancreatitis, haemochromatosis and malnutrition; congenital abnormalities such as cystic fibrosis and Shwachman–Diamond syndrome; viral infections.
Fatty replacement of entire pancreas, with increase in pancreatic size due to fat accumulation, is known as lipomatous pseudohypertrophy.1
Lipomatous pseudohypertrophy of the pancreas is characterised by the disappearance of pancreatic exocrine tissue due to adipose tissue replacement, although the pancreatic duct and islets remain intact.
In this case report, the patient had lipomatous pseudohypertrophy of pancreas with coexisting chronic calcific pancreatitis resulting exocrine insufficiency, which is a very rare entity.
Case report
A 49-year-old female patient presented with complaints of foul smelling loose motions of semisolid consistency, three to four times a day, since last six months with vague discomfort in the epigastric region. There was no history of haematochesia, malena, nausea, vomiting, fever, weight loss or acute pain abdomen at the time of presentation. She was post-menopausal, normotensive and non-diabetic. There was no contributory family history. There was history of getting hospitalised multiple times since last six months during which she was diagnosed as acute gastroenteritis and was managed with proton pump inhibitors and antibiotics. On examination, the general and systemic physical examination was within normal limits. Investigations reveal normal fasting and post-prandial sugar levels. The serum levels of the pancreatic enzyme amylase were found to be considerably low at 8 unit/l (normal range is 25–120 unit/l). Stool examination confirmed steatorrhoea.
Ultrasound of the abdomen revealed enlarged hyperechoic pancreas with multiple calcific foci measuring 3–10 mm in the uncinate process and head region of pancreas. The main pancreatic duct is undilated (Fig. 1).
Fig. 1.

Ultrasound image shows hyperechoic pancreas with calcification in head and uncinate process of pancreas.
Computed tomography (CT) scan of abdomen showed enlargement of body and tail of pancreas with body measuring 53.8 mm and tail measuring 41.1 mm in anteroposterior dimension. The body and tail of pancreas were totally replaced by fat (Hounsfield units were −70 to −100). The uncinate process and the head of pancreas show multiple calcific foci within, suggestive of chronic calcific pancreatitis (Fig. 2, Fig. 3, Fig. 4). The pancreatic ductal anatomy was normal for this patient.
Fig. 2.
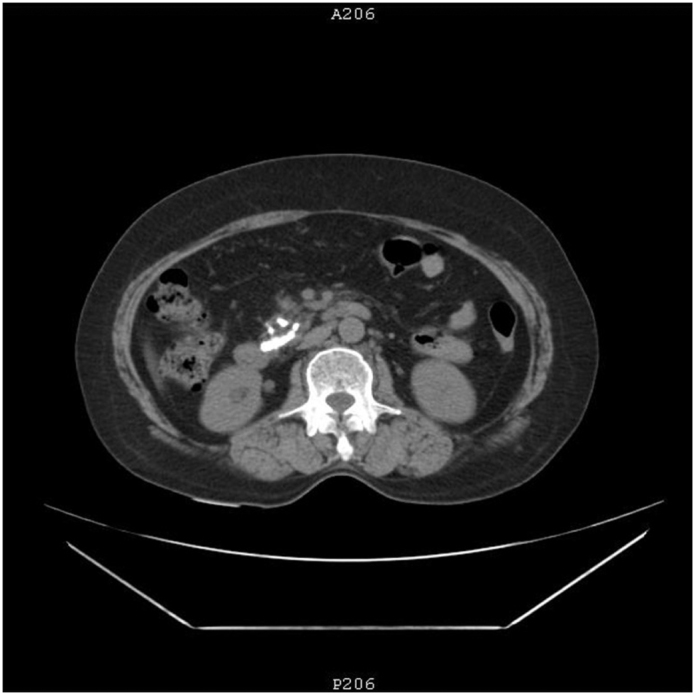
Non-contrast enhanced computed tomography image shows calcification in head of pancreas.
Fig. 3.
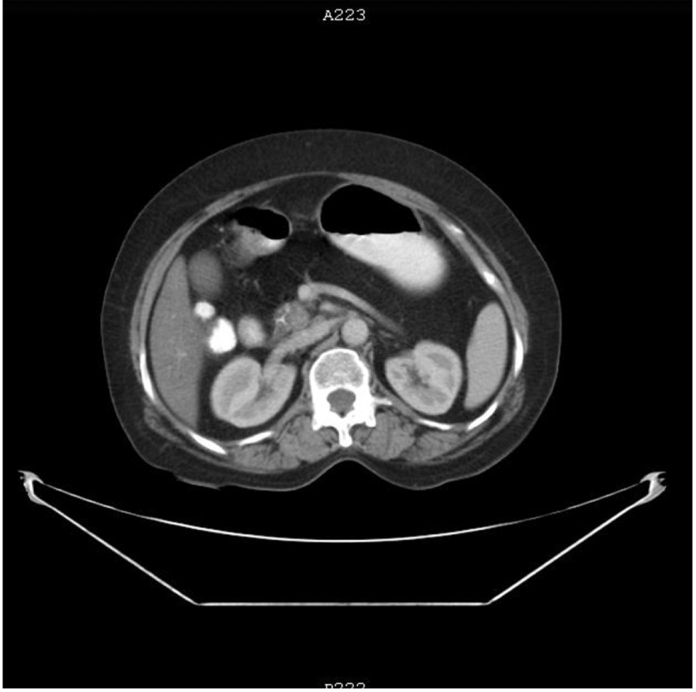
Contrast enhanced computed tomography image shows lipomatous pseudohypertrophy of body and tail region of pancreas.
Fig. 4.
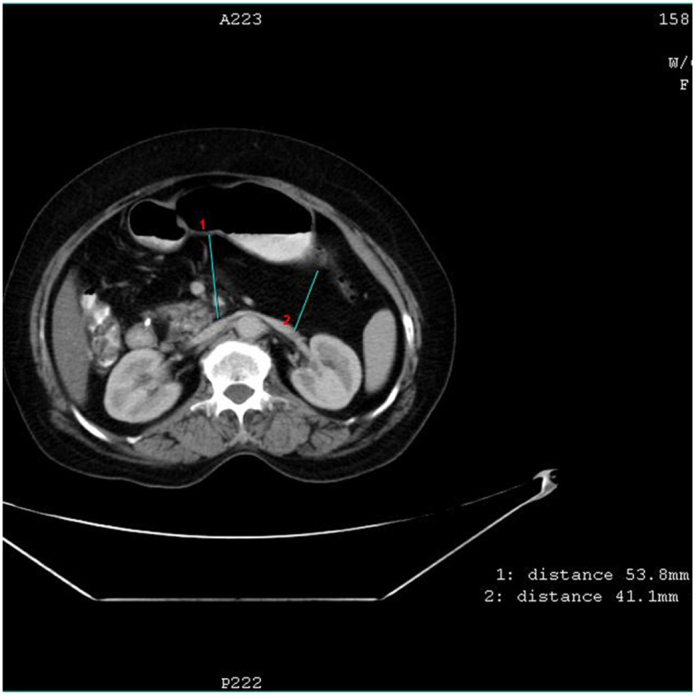
Contrast enhanced computed tomography image shows measurement of pancreatic body (53.8 mm) and tail (41.1 mm) anteroposterioly. Normal measurement upper range is 30 mm in AP dimension.
Again, a detailed history was taken. The history and the relevant investigations were non-contributory. There was no history of alcoholism or steroid intake. There is no family history of pancreatitis. Investigations showed no evidence of hyperlipidaemia or hypercalcaemia. There was no history of structural abnormality like pancreas divisum or choledochocele. Based on the negative history and investigations, the most likely cause of chronic calcific pancreatitis was considered as idiopathic.
On the basis of above-mentioned clinical features and imaging findings, diagnosis of lipomatous pseudohypertrophy of the pancreas with coexisting chronic calcific pancreatitis, resulting in malabsorption due to exocrine pancreatic enzyme insufficiency was made.
Discussion
Lipomatous pseudohypertrophy of the pancreas is an extremely rare entity. First described by Hantelmann in 1931, this entity was further characterised by Siegler.2
The cause of lipomatous pseudohypertrophy of the pancreas might be of viral aetiology or abnormal lipid metabolism.3
However, in this case, the lipomatous pseudohypertrophy was the end result of chronic inflammation due to chronic calcific pancreatitis.
Evaluation of pancreas for this entity can be done by several modalities.
In ultrasonography, this entity can be identified by enlarged hyperechoic, hyper-reflective pancreas. In past, ultrasonography was used by Lee et al.,4 to evaluate the fatty content of the pancreas. However, the role of ultrasonography in the diagnosis of pancreatic lipomatosis is very limited.
Cross-sectional imaging, namely, CT and magnetic resonance imaging (MRI) play a vital role in the evaluation of pancreas.
CT plays an important role in the evaluation of pancreas as fatty infiltration of pancreas is seen as pancreatic parenchyma intermixed with adipose tissue.
CT is instrumental in diagnosing pancreatic lipomatosis and is particularly useful in detecting other structural abnormalities also. Unenhanced CT shows negative attenuation value i.e. −70 to −100 Hounsfield unit in pancreas as it is replaced by fat.
Recognition of total fatty replacement of pancreas is important as it results in malabsorption due to pancreatic exocrine insufficiency.5
Chemical shift MRI has advantage over CT in confirming the presence of focal lipomatosis of the pancreas.6
In our case, she was having chronic diarrhoea with multiple hospitalisations. The management done during that time was targeted towards an infective cause. She was given multiple antibiotics for a long time. Accurate diagnosis changed the management of the patient. She was given pancreatic enzyme replacement therapy (PERT) and vitamin supplementation for fat soluble vitamins (vitamins A, D, E and K). Lifestyle modifications in the form of balanced diet and avoidance of fatty food were advised. She improved significantly and will remain on long-term follow-up.
Extensive lipomatous pancreas has been reported in the past by few authors. Patel et al. demonstrated pancreatic lipomatosis with dilated pancreatic duct due to an obstructing calculus in distal pancreatic duct.1 Haunz et al. reported lipomatosis in pancreatic tail in a clinical study of 80 cases of carcinoma head of pancreas.7 In these cases, no increase in pancreatic size suggesting pseudohypertrophy was noted.
In recent past, Reddy et al. reported a case of chronic pancreatitis who developed the total fat replacement of pancreatic parenchyma with associated multiple calculi that simulates lipomatous pseudohypertrophy of pancreas. However, the size of pancreas was not increased in that case, so it was not a case of true lipomatous pseudohypertrophy of pancreas.8
In our case, the picture of coexisting lipomatous pseudohypertrophy of the pancreatic parenchyma with multiple calcific foci at the uncinate process and head of pancreas secondary to chronic pancreatitis (chronic calcific pancreatitis), with exocrine deficiency manifestations is never reported in literature before. The aim of this case report is to bring forward this extremely rare presentation and to sensitise clinicians that this entity can be a cause of exocrine pancreatic insufficiency leading to malabsorption.
Conflicts of interest
The authors have none to declare.
References
- 1.Patel S., Bellon E.M., Haaga J., Park C.H. Fat replacement of the exocrine pancreas. Am J Roentgenol. 1980;135(October (4)):843–845. doi: 10.2214/ajr.135.4.843. [DOI] [PubMed] [Google Scholar]
- 2.Siegler D.I. Lipomatous pseudohypertrophy of the pancreas associated with chronic pulmonary suppuration in an adult. Postgrad Med J. 1974;50:53–55. doi: 10.1136/pgmj.50.579.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hoyer A. Lipomatous pseudohypertrophy of the pancreas with complete absence of exocrine tissue. J Pathol Bacteriol. 1949;61:93–100. [Google Scholar]
- 4.Lee J.S., Kim S.H., Jun D.W. Clinical implications of fatty pancreas: correlations between fatty pancreas and metabolic syndrome. World J Gastroenterol. 2009;15(April (15)):1869–1875. doi: 10.3748/wjg.15.1869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Soyer P., Spelle L., Pelage J.P. Cystic fibrosis in adolescents and adults: fatty replacement of the pancreas-CT evaluation and functional correlation. Radiology. 1999;210(March (3)):611–615. doi: 10.1148/radiology.210.3.r99mr08611. [DOI] [PubMed] [Google Scholar]
- 6.Kim H.J., Byun J.H., Park S.H. Focal fatty replacement of the pancreas: usefulness of chemical shift MRI. Am J Roentgenol. 2007;188:429–432. doi: 10.2214/AJR.05.1095. [DOI] [PubMed] [Google Scholar]
- 7.Haunz E.A., Baggenstoss A.H. Carcinoma of head of the pancreas. Arch Pathol. 1950;49:367–386. [Google Scholar]
- 8.Reddy O.J., Gafoor J.A., Reddy G.M., Prasad P.O. Total pancreatic lipomatosis: a rare presentation. J NTR Univ Health Sci. 2015;4:272–274. [Google Scholar]


