Abstract
AIM
To clarify the association of malignancy with mesenteric panniculitis-like changes on computed tomography (CT).
METHODS
All abdominal CT scans performed at NorthShore University HealthSystem showing mesenteric panniculitis from January 2005 to August 2010 were identified in the Radnet (RadNet Corporation, Los Angeles, CA) database. Patients with a new or known diagnosis of a malignancy were included for this analysis. Longitudinal clinical histories were obtained from electronic medical records.
RESULTS
In total, 147794 abdominal CT scans were performed during the study period. Three hundred and fifty-nine patients had mesenteric panniculitis (MP)-like abnormalities on their abdominal CT. Of these patients, 81 patients (22.6%) had a known history of cancer at the time of their CT scan. Nineteen (5.3%) had a new diagnosis of cancer in concurrence with their CT, but the majority of these (14/19, 74%) were undergoing CT as part of a malignancy evaluation. Lymphomas were the most common cancers associated with MP-like findings on CT (36 cases, 36%), with follicular lymphoma being the most frequent subtype (17/36). A variety of solid tumors, most commonly prostate (7) and renal cell cancers (6) also were seen. CT follow up was obtained in 56 patients. Findings in the mesentery were unchanged in 45 (80%), worsened in 6 (11%), and improved in 5 patients (9%). Positron emission tomography (PET) scans performed in 44 patients only showed a positive uptake in the mesenteric mass in 2 patients (5%).
CONCLUSION
A new diagnosis of cancer is uncommon in patients with CT findings suggestive of MP. MP-like mesenteric abnormalities on CT generally remain stable in patients with associated malignancies. PET scanning is not recommended in the evaluation of patients with mesenteric panniculitis-like findings on CT.
Keywords: Panniculitis, Peritoneal, X ray, Neoplasms, Computed tomography, Small intestine, Misty mesentery, Lymphoma, Tomography, Positron emission tomography
Core tip: The most important question when a patient has new mesenteric panniculitis - like findings on abdominal computed tomography (CT) scan is the likelihood that a malignancy is present. Based on our study, a first diagnosis of cancer occurs in approximately 5% and is unexpected diagnosis in 1.4% of these patients. Lymphomas are the most likely malignancies. A careful clinical evaluation for lymphoma as well as solid tumors is advised. Follow up is also important, as an additional 5% of patients will eventually be diagnosed with a malignancy. In patients with a malignancy, CT findings are likely to remain stable, and positron emission tomography scanning is not advised.
INTRODUCTION
The computed tomography (CT) finding of mesenteric panniculitis (MP) (defined as a “misty” or “hazy” mesentery and/or an unexplained mesenteric mass), is uncommon. When truly defined by mesenteric biopsy, MP is a rare disease characterized by unexplained inflammation of the mesentery[1-3]. A variety of conditions are associated with MP including abdominal trauma[4], lymphoma and other neoplasms[5,6] and autoimmune diseases[7-9]. Infectious associations with MP include mycobacterial[10] and cryptococcal[11] infections and cholera[12]. In some patients, especially those having an acute presentation of the disease, a viral mesenteritis is likely. Fever of unknown origin[13] and chylous ascites have also been described in patients with MP. CT imaging of the abdomen in these patients demonstrates a mass of the mesentery, characterized by fat enhancement and multiple soft tissue nodules along the root of the small bowel without vascular compromise; these are distinguishing radiographic features of MP. Histologically, MP is characterized by chronic inflammation, fat necrosis and fibrosis within the connective tissue of the mesentery[14-16].
CT findings suggestive of MP can be concurrent with a previously unidentified underlying malignancy[3]. Other patients with a known diagnosis of cancer will develop new mesenteric abnormalities on CT, raising the specter of mesenteric metastasis. The development of MP on CT imaging currently has an unclear influence on the natural history of cancer in these patients. The types of cancer likely to occur in the setting of MP also requires further exploration. We herein describe a group of patients with the CT finding of MP and the diagnosis of malignancy, in an attempt to clarify the clinical significance of the simultaneous presence of these two conditions in the same patient.
MATERIALS AND METHODS
A query of the, Radnet database (RadNet Corporation, Los Angeles, CA, United States) of the NorthShore University HealthSystem, (comprised of 4 hospitals in the Northern suburbs of Chicago, Illinois, United States) was performed. The terms used in the query were “mesenteric panniculitis” or “misty mesentery”. All charts of patients with these radiographic findings between January 1st 2005 and April 30th 2010 were reviewed. Some of these patients have been previously described3. Only patients that were undergoing a CT for follow up of a known cancer and patients with a new cancer diagnosed after the finding of the mesenteric abnormality were included in this analysis. Findings of follow up CT scans were evaluated. Results of mesenteric biopsies and positron emission tomography (PET) scanning were also noted.
RESULTS
In total, 147794 CT scans reviewed. Within this group, there were 359 patients with MP-like CT abnormalities. Of these patients 19 (5.3%) had a new diagnosis of cancer. Eighty-one patients (22.6%) had a known previous history of cancer. Lymphomas were the most common cancers associated with MP (36 patients, 36%). Follicular lymphoma was the most common lymphoma subtype and was found in 17 patients. A variety of solid tumors were found, the most common being prostate (7), lung, and renal cell cancer (6). For additional details of these findings, see Table 1. Tables 2 and 3 show the distribution of cancers in patients with a new diagnosis and a known diagnosis of cancer at the time of their CT scan, respectively. Figures 1, 2 and 3 show representative examples of CT imaging in patients with lymphoma and MP-like findings.
Table 1.
Cancer types in patients with computed tomography findings of mesenteric panniculitis
| Total patients | n = 100 |
| Lymphomas | n = 36 |
| Follicular | 17 |
| Diffuse large B cell | 9 |
| Small lymphocytic | 3 |
| Mantle cell | 2 |
| T cell | 2 |
| Other (Burkitt, Hodgkin, Marginal zone B cell) | 3 |
| Solid tumors | n = 64 |
| Prostate | 7 |
| Renal cell | 6 |
| Lung | 6 |
| Chronic lymphocytic leukemia | 5 |
| Bladder | 5 |
| Endometrial | 5 |
| Breast | 4 |
| Colon | 3 |
| Rectal | 3 |
| Other | 20 |
Table 2.
Cancer subtypes in 19 patients with new malignancy and mesenteric panniculitis
| 6 | Follicular lymphoma |
| 2 | T cell lymphoma |
| 2 | Endometrial cancer |
| 1 | Acute myeloid leukemia |
| 1 | Diffuse large B cell lymphoma |
| 1 | Waldenstrom's macroglobulinemia |
| 1 | Esophageal cancer |
| 1 | Small cell lung cancer |
| 1 | Lung adenocarcinoma, with diffuse metastases |
| 1 | Intraductal papillary mucinous neoplasm |
| 1 | Bladder cancer |
| 1 | Melanoma, metastases to small bowel |
Table 3.
Cancer subtypes in 81 patients with known malignancy and mesenteric panniculitis-like findings on computed tomography n (%)
| Cancer subtype | Number of patients |
| Lymphomas | 27 (33) |
| Follicular | 11 (41) |
| Diffuse large B cell | 6 (30) |
| Small lymphocytic lymphoma | 3 (11) |
| Mantle cell | 2 (7) |
| Burkitt’s, Hodgkin’s, marginal zone B cell | 3 (11) |
| Solid tumors | 45 (67) |
| Prostate | 7 (9) |
| Renal cell | 6 (7) |
| Chronic lymphocytic leukemia | 5 (6) |
| Lung | 5 (6) |
| Bladder | 4 (5) |
| Breast | 4 (5) |
| Colon | 3 (4) |
| Endometrial | 3 (4) |
| Rectal | 3 (4) |
| Pancreatic | 2 (3) |
| Myelodysplasia | 2 (3) |
| Other - gallbladder, ampullary, chronic myeloid leukemia, gastric, glioma, IPMN, salivary gland adenocarcinoma, small bowel carcinoid, neuroendocrine tumor | 10 (12) total |
IPMN: Intraductal papillary mucinous neoplasm.
Figure 1.
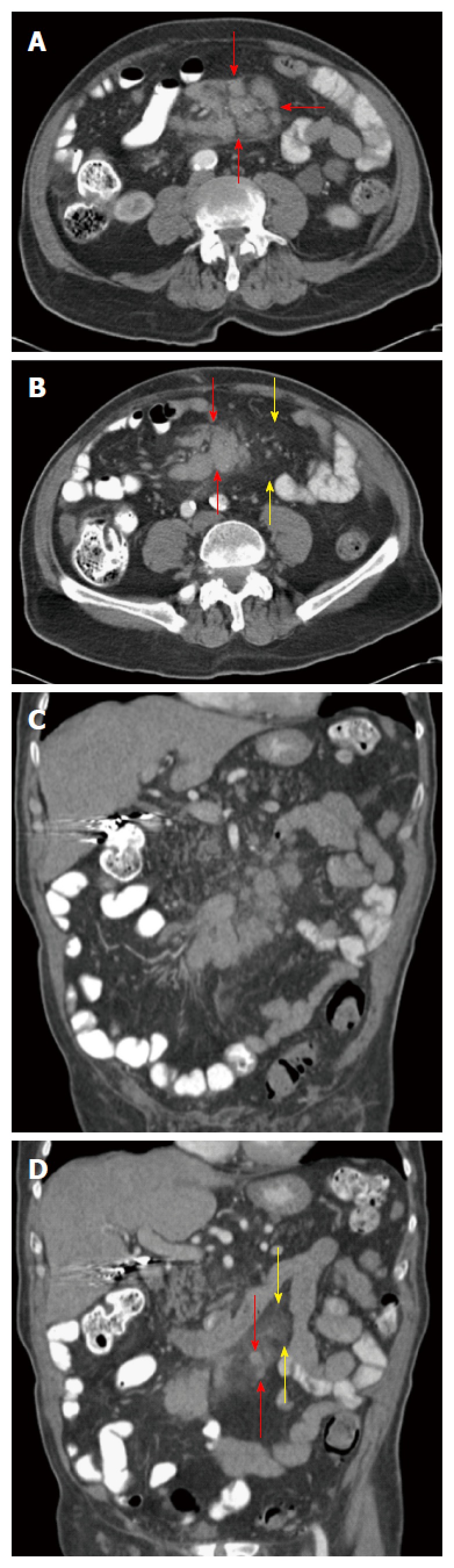
Mesenteric panniculitis in a patient with non-Hodgkin lymphoma. A: Axial computed tomography (CT) scan at the level of the inferior aspect of the kidneys shows extensive mesenteric adenopathy (red arrows); B: Axial CT image obtained more caudally, at the level of the iliac crest reveals mesenteric adenopathy (red arrows) and synchronous mesenteric panniculitis (yellow arrows) characterized by hazy mesenteric fat and separation of the mesenteric vessels; C: Coronal reformatted CT image demonstrates the extensive mesenteric adenopathy (red arrows); D: Coronal reformatted CT image, take dorsal to (C) depicts synchronous mesenteric adenopathy (red arrows) and mesenteric panniculitis (yellow arrows).
Figure 2.
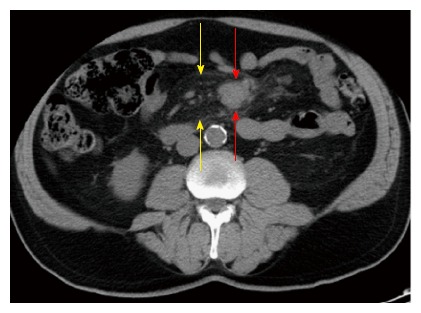
Mesenteric panniculitis in a patient with non-Hodgkin lymphoma. Axial computed tomography scan shows synchronous mesenteric panniculitis (yellow arrows), manifested by fat separating the mesenteric vessels, and mesenteric adenopathy (red arrows).
Figure 3.
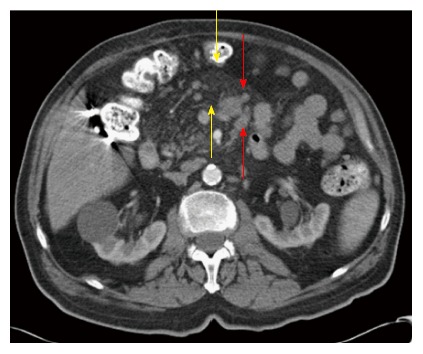
Mesenteric panniculitis in a patient with non-Hodgkin lymphoma. Axial computed tomography image shows synchronous mesenteric adenopathy (red arrows) and mesenteric adenopathy (yellow arrows).
Fourteen of the 19 patients with newly diagnosed cancers were undergoing abdominal CT scanning as part of a malignancy workup. The remaining five patients with newly diagnosed cancers underwent abdominal CT scanning for unexplained abdominal pain or other systemic symptoms.
The majority of the patients with a known history of malignancy underwent CT scanning for staging and tumor follow up (67/81, 83%).
Follow up CT scans were performed in 56 patients. No change in mesenteric abnormalities was seen in the majority of these, (45 patients, 80%). An increase in size of the mesenteric abnormality was seen in 6 patients (11%), and a decrease in size of the mesenteric abnormality was seen in 5 patients on follow up (9%). Figures 4 and 5 show follow up CT scans in patients with non-Hodgkins lymphoma.
Figure 4.
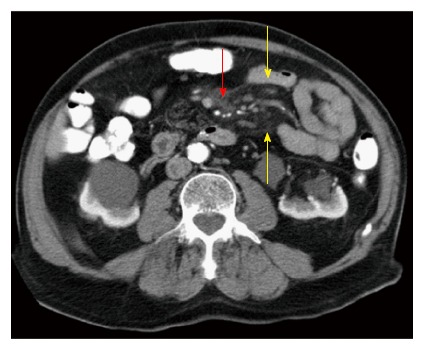
Mesenteric panniculitis in a patient with non-Hodgkin lymphoma (same patient as Figures 3 and 7) following chemotherapy. Axial computed tomography image shows almost complete resolution of the mesenteric adenopathy (red arrow) but persistent mesenteric panniculitis (yellow arrows).
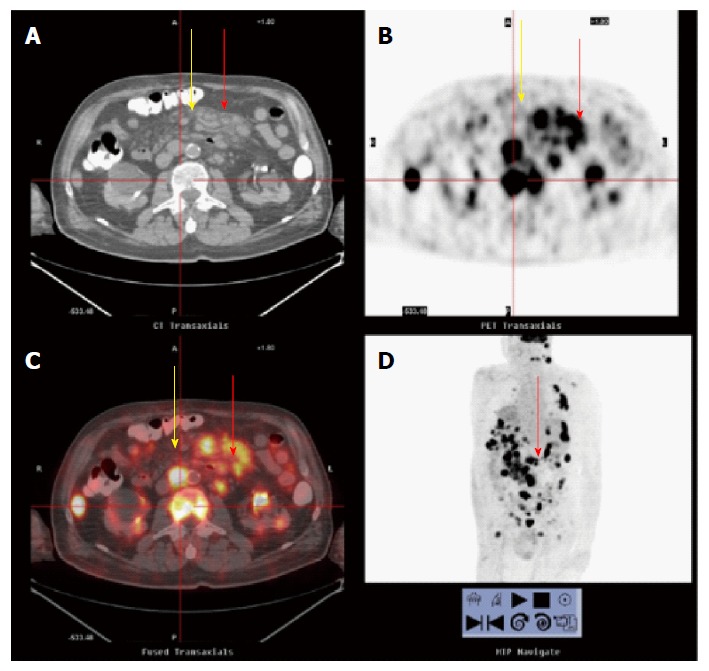
Figure 5.
Mesenteric panniculitis in a patient with non-Hodgkin lymphoma. Positron emission tomography-computed tomography (PET-CT) scan following chemotherapy (same patient as Figures 3, 4 and 7). Computed tomography (CT) image (A), PET image (B), fused PET-CT image (C), and whole body PET image (D) demonstrates almost complete resolution of the mesenteric adenopathy (red arrow) with no fludeoxyglucose uptake in the portion of mesentery involved by mesenteric panniculitis (yellow arrows). The disseminated adenopathy seen in Figure 5D has almost completely resolved.
Forty-four patients underwent PET scans. Only 2 (5%) of these patients, both with stage IV-B diffuse large B cell lymphoma, had positive uptake in the mesenteric mass. Both of these patients had resolution of this finding on repeat PET scan following treatment. CT and PET findings are shown in two patients with non-Hodgkins lymphoma in Figures 6 and 7.
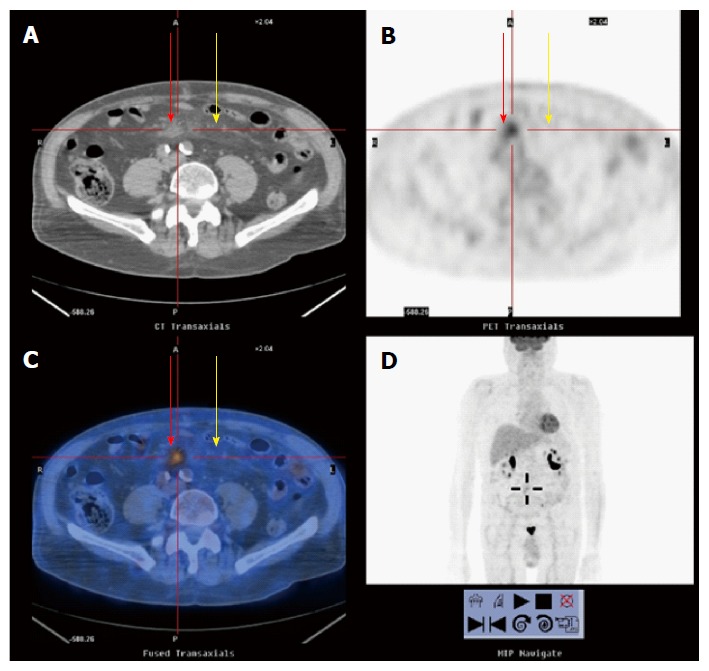
Figure 6.
Mesenteric panniculitis in a patient with non-Hodgkin lymphoma (same patient as Figure 2). Positron emission tomography-computed tomography (PET-CT) scan. CT image (A), PET image (B), fused PET-CT image (C), and whole body PET image (D) shows abnormal fludeoxyglucose uptake in the mesenteric lymph nodes containing tumor (red arrows) but not in the portion of mesentery involved by mesenteric panniculitis (yellow arrows).
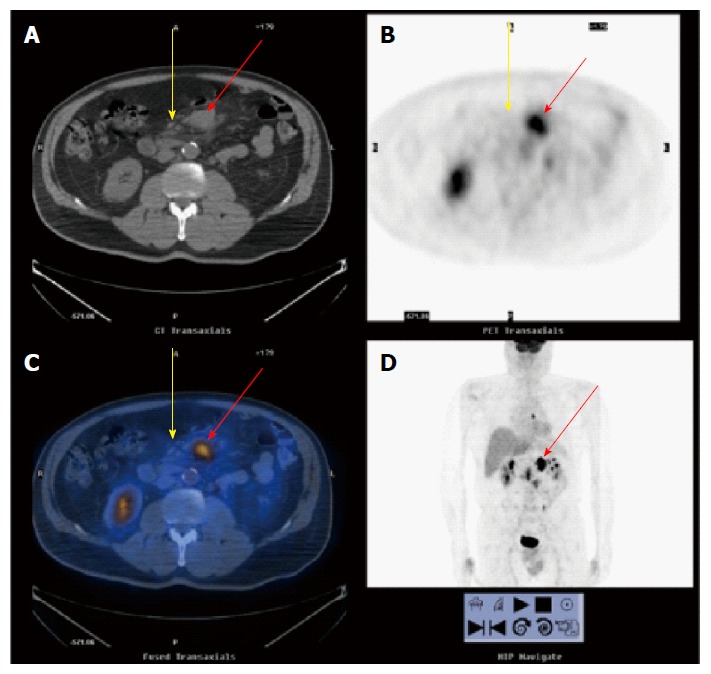
Figure 7.
Mesenteric panniculitis in a patient with non-Hodgkin lymphoma (same patient as Figure 3). Positron emission tomography-computed tomography (PET-CT) scan. Computed tomography image (A), PET image (B), fused PET-CT image (C), and whole body PET image (D) shows abnormal fludeoxyglucose (FDG) uptake in the mesenteric lymph nodes containing tumor (red arrows) but not in the portion of mesentery involved by mesenteric panniculitis (yellow arrows). Notice the innumerable regions of abnormal FDG uptake (black regions in D) corresponding to the patient’s disseminated adenopathy.
Five patients underwent a mesenteric biopsy. Four patients had biopsies of mesenteric lymph nodes, all showing lymphoma (two with diffuse large B-cell lymphoma and two with follicular lymphoma). One patient had a biopsy of a mesenteric mass that showed fibrosis and benign mesothelial cells, consistent with mesenteric panniculitis.
DISCUSSION
Biopsy-proven MP is an autoimmune disease, characterized by the histologic findings of fat necrosis and chronic inflammatory infiltrates of the mesentery. However, the diagnosis of MP is often made empirically based on characteristic radiographic findings, and not all patients with these findings will require a biopsy. It is imperative to fully characterize the clinical significance of MP-like findings on abdominal CT. The risk for the presence of malignancy, in patients having MP-like abnormalities on abdominal CT creates great concern for patients and clinicians alike. Prior studies that have suggested the finding of MP-like abnormalities on abdominal CT are associated with a very high risk of malignancy that ranges between 30 and 63%. Our study on the other hand shows a much lower rate of 5.3% of new cancers associated with the currents of the CT findings. In fact, our data suggests that only five of the total of 359 patients having MP -like abnormalities on abdominal CT were not suspected of having cancer at the time performance of the examination. This would suggest that the rate of completely new cancers found in the setting of MP- like mesenteric abnormalities on abdominal CT scan is only 1.4%. The discrepancy between the high rate of cancer associated with MP-like abnormalities in previous studies and the very low rate in our study may be explained in part by the inclusion of patients with known malignancy in prior studies that calculated the rate of association of these two conditions. In our study, if all patients with known and newly suspected cancers are included, 100 of the 359 number of patients with MP-like abnormalities on abdominal CT (or 28% of the total group) had an associated cancer. In our view, the most important question to the clinician having a patient with new MP -like findings on abdominal CT is the likelihood that a further evaluation will reveal the presence of malignancy. Based on these data, the likelihood that a cancer is initially present is approximately 5% and is a new diagnosis in 1.4%. Newly diagnosed malignancies in association with the CT findings are likely to be lymphomas, and careful clinical evaluation for lymphoma and some of the associated solid tumors found in our study is advised. Follow up is also important as an additional 5% of patients will eventually be diagnosed with a malignancy[17].
Most studies and reviews on MP recommend follow-up evaluation with abdominal imaging[18-21]. Our data also suggests that at least in patients with a malignancy, mesenteric findings are likely to remain stable.
Mesenteric uptake of fludeoxyglucose (FDG) during PET scanning within the thickened area of mesentery is rare, and was only seen in 5% of patients undergoing PET in our study. These findings are consistent with our prior observation in a case report[22]. On the other hand, Zissin et al[23] suggested that the addition of PET to CT scanning may help to differentiate between inflammatory and neoplastic forms of mesenteric thickening. Our data suggest that PET will not be useful to distinguish an inflammatory mesenteric mass due to MP from a malignant mesenteric mass, or rule out the possibility that a patient has a neoplasm. In fact, our data appears to demonstrate that the MP-like mesenteric abnormality that occurs in patients with malignancy may in fact be an epiphenomenon of the underlying neoplasm. Because most patients with malignancy demonstrate little change in this mesenteric abnormality on follow up CT, MP-like findings appear to have little influence on the natural history of neoplastic disease. As noted by prior authors, MP may in fact represent a paraneoplastic process[6].
Since this was a retrospective study, evaluation including the performance of follow up CT was variable and not controlled. In addition, although our radiology practice has agreed to use the terms “misty mesentery” and “mesenteric panniculitis” when describing an MP-like finding on abdominal CT scanning, it is feasible but some cases in which the aforementioned terms were not used in the radiology reports could have been missed. Since the vast majority of the patients in our practice with MP did not receive a biopsy of the mesenteric mass, this study does not reveal whether these abnormalities represent inflammation or neoplastic extension.
In conclusion, our study shows that a new and unexpected diagnosis of malignancy is rare in patients with MP-like abnormalities on CT scan. These CT findings generally remain stable in patients with known malignancies, and appear to represent a paraneoplastic process. PET scanning does not appear to have a role in assisting with the further characterization of MP-like findings in the mesentery.
COMMENTS
Background
Mesenteric panniculitis (MP) is a rare disease characterized by unexplained inflammation of the mesentery. Computed tomography (CT) scan imaging of the abdomen demonstrates thickening of mesenteric tissue and lymphadenopathy at the root of the small bowel mesentery without vascular compromise. Chronic inflammation, fat necrosis and fibrosis are a variety of conditions are associated seen on biopsy. MP is associated with neoplastic disease, abdominal trauma, autoimmune diseases and infections. MP-like findings on abdominal CT can occur in patients with previously unidentified cancers and in those with a known diagnosis of cancer. The development of MP on CT imaging currently has an unclear influence on the natural history of cancer in these patients. The authors herein describe a group of patients with the CT finding of MP and the diagnosis of malignancy, in an attempt to clarify the relationship between these conditions.
Research frontiers
Currently, little is known about MP, including its etiology, pathophysiology and clinical outcome in individual patients. Few studies have addressed appropriate evaluation and treatment with MP. Appropriate algorithms for diagnosis and treatment of MP are lacking in the medical literature.
Innovations and breakthroughs
Although prior studies have described the association of MP and malignancy, the current study shows that only 1.4% of patients with a CT finding of MP will be found to have a previously undiagnosed or suspected cancer. The higher rate of association of MP and cancer described in prior studies likely represents inclusion of patients with a known history of cancer. Additionally, this study shows that follow up abdominal CT in patients with cancer shows stability and not worsening of MP. Finally, the study shows that in patients with cancer, PET scanning rarely shows uptake within the mesenteric abnormality.
Applications
This study demonstrates reassurance to the clinician and patient that findings suggestive of MP on abdominal CT rarely represent the occurrence of a new cancer. Initial standard evaluation to rule out cancer and appropriate follow up is advised by the authors. Furthermore, these findings do not appear to represent a poorer prognosis in patients with existing cancer. Frequent monitoring with abdominal CT does not appear to be of benefit in these patients. PET scanning does not appear to have a role for follow up in these patients.
Terminology
Mesenteric panniculitis is a rare idiopathic inflammatory disorder of the mesentery characterized by the biopsy findings of fat necrosis, mesenteric infiltration with chronic inflammatory cells and fibrosis. Its natural history is unclear and diagnostic and treatment algorithms are incomplete.
Peer-review
This study represented an interesting advance toward the understanding of this condition.
Footnotes
Manuscript source: Invited manuscript
Specialty type: Gastroenterology and hepatology
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B, B, B
Grade C (Good): 0
Grade D (Fair): 0
Grade E (Poor): 0
Conflict-of-interest statement: The authors declare that there are no conflicts of interest related to this study.
Institutional review board statement: This study was approved by the Institutional Review Board of NorthShore University HealthSystem.
Informed consent statement: Informed consent for this retrospective study was waived by the Institutional Review Board.
Data sharing statement: No additional data is available.
Peer-review started: October 16, 2016
First decision: October 28, 2016
Article in press: November 28, 2016
P- Reviewer: Aosasa S, Sayegh AI, Tarnawski AS S- Editor: Yu J L- Editor: A E- Editor: Wang CH
References
- 1.Coulier B. Mesenteric panniculitis. Part 2: prevalence and natural course: MDCT prospective study. JBR-BTR. 2011;94:241–246. doi: 10.5334/jbr-btr.659. [DOI] [PubMed] [Google Scholar]
- 2.Nabzdyk CS, Dermody M, Rhee J, Bankoff M, Weinstein B, Orkin BA. Progression of sclerosing mesenteritis into intra-abdominal abscesses. Am Surg. 2013;79:E25–E27. [PubMed] [Google Scholar]
- 3.Smith ZL, Sifuentes H, Deepak P, Ecanow DB, Ehrenpreis ED. Relationship between mesenteric abnormalities on computed tomography and malignancy: clinical findings and outcomes of 359 patients. J Clin Gastroenterol. 2013;47:409–414. doi: 10.1097/MCG.0b013e3182703148. [DOI] [PubMed] [Google Scholar]
- 4.Emory TS, Monihan JM, Carr NJ, Sobin LH. Sclerosing mesenteritis, mesenteric panniculitis and mesenteric lipodystrophy: a single entity? Am J Surg Pathol. 1997;21:392–398. doi: 10.1097/00000478-199704000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Okamoto M, Ohkubo N, Yamanaka M, Kimura A, Takagi T, Iwao A, Kawaguchi M, Iwasaki N, Takagi T, Sho KE, et al. [A case of mesenteric panniculitis complicated with malignant lymphoma] Nihon Shokakibyo Gakkai Zasshi. 1998;95:884–889. [PubMed] [Google Scholar]
- 6.Wilkes A, Griffin N, Dixon L, Dobbs B, Frizelle FA. Mesenteric panniculitis: a paraneoplastic phenomenon? Dis Colon Rectum. 2012;55:806–809. doi: 10.1097/DCR.0b013e318252e286. [DOI] [PubMed] [Google Scholar]
- 7.Sugihara T, Koike R, Nosaka Y, Ogawa J, Hagiyama H, Nagasaka K, Nonomura Y, Nishio J, Nanki T, Kohsaka H, et al. Case of subcutaneous and mesenteric acute panniculitis with Sjögren’s syndrome. Nihon Rinsho Meneki Gakkai Kaishi. 2002;25:277–284. doi: 10.2177/jsci.25.277. [DOI] [PubMed] [Google Scholar]
- 8.Tejón Menéndez P, Alonso S, Alperi M, Ballina J. Mesenteric panniculitis in a patient with ankylosing spondylitis. Reumatol Clin. 2013;9:197. doi: 10.1016/j.reuma.2012.10.014. [DOI] [PubMed] [Google Scholar]
- 9.Watanabe I, Taneichi K, Baba Y, Sakai I, Chimoto T, Shibaki H. A case of mixed connective tissue disease with mesenteric panniculitis. Nihon Naika Gakkai Zasshi. 1989;78:93–94. doi: 10.2169/naika.78.93. [DOI] [PubMed] [Google Scholar]
- 10.Borde JP, Offensperger WB, Kern WV, Wagner D. Mycobacterium genavense specific mesenteritic syndrome in HIV-infected patients: a new entity of retractile mesenteritis? AIDS. 2013;27:2819–2822. doi: 10.1097/01.aids.0000433820.25415.17. [DOI] [PubMed] [Google Scholar]
- 11.Alonso Socas MM, Valls RA, Gómez Sirvent JL, López Lirola A, Aix SP, Higuera AC, Santolaria F. Mesenteric panniculitis by cryptococcal infection in an HIV-infected man without severe immunosuppression. AIDS. 2006;20:1089–1090. doi: 10.1097/01.aids.0000222093.05400.bb. [DOI] [PubMed] [Google Scholar]
- 12.Roginsky G, Mazulis A, Ecanow JS, Ehrenpreis ED. Mesenteric Panniculitis Associated With Vibrio cholerae Infection. ACG Case Rep J. 2015;3:39–41. doi: 10.14309/crj.2015.95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Avelino-Silva VI, Leal FE, Coelho-Netto C, Cotti GC, Souza RA, Azambuja RL, Rocha Mde S, Kallas EG. Sclerosing mesenteritis as an unusual cause of fever of unknown origin: a case report and review. Clinics (Sao Paulo) 2012;67:293–295. doi: 10.6061/clinics/2012(03)16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Guettrot-Imbert G, Boyer L, Piette JC, Delèvaux I, André M, Aumaître O. [Mesenteric panniculitis] Rev Med Interne. 2012;33:621–627. doi: 10.1016/j.revmed.2012.04.011. [DOI] [PubMed] [Google Scholar]
- 15.Nicholson JA, Smith D, Diab M, Scott MH. Mesenteric panniculitis in Merseyside: a case series and a review of the literature. Ann R Coll Surg Engl. 2010;92:W31–W34. doi: 10.1308/147870810X12699662981393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Shin NY, Kim MJ, Chung JJ, Chung YE, Choi JY, Park YN. The differential imaging features of fat-containing tumors in the peritoneal cavity and retroperitoneum: the radiologic-pathologic correlation. Korean J Radiol. 2010;11:333–345. doi: 10.3348/kjr.2010.11.3.333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Badet N, Sailley N, Briquez C, Paquette B, Vuitton L, Delabrousse É. Mesenteric panniculitis: still an ambiguous condition. Diagn Interv Imaging. 2015;96:251–257. doi: 10.1016/j.diii.2014.12.002. [DOI] [PubMed] [Google Scholar]
- 18.Hussein MR, Abdelwahed SR. Mesenteric panniculitis: an update. Expert Rev Gastroenterol Hepatol. 2015;9:67–78. doi: 10.1586/17474124.2014.939632. [DOI] [PubMed] [Google Scholar]
- 19.Robbrecht DG, Alidjan F, Eikemans B, Haans DA, van Guldener C, van Wijngaarden P. [Mesenteric panniculitis: variable presentations] Ned Tijdschr Geneeskd. 2012;155:A4555. [PubMed] [Google Scholar]
- 20.van Putte-Katier N, van Bommel EF, Elgersma OE, Hendriksz TR. Mesenteric panniculitis: prevalence, clinicoradiological presentation and 5-year follow-up. Br J Radiol. 2014;87:20140451. doi: 10.1259/bjr.20140451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Orcajo Rincón J, Rotger Regi A, Mari Hualde A, Reguera Berenguer L, Hernandez Moreno L, Alonso Farto JC. A prospective study to determine the real value of mesenteric 18F-FDG uptake in cancer patients. inflammatory or tumoral mesenteric paniculitis? Rev Esp Med Nucl Imagen Mol. 2014;33:352–357. doi: 10.1016/j.remn.2014.03.006. [DOI] [PubMed] [Google Scholar]
- 22.Ehrenpreis ED, Rao AS, Aki R, Brown H, Pae T, Boiskin I. Normal Positron Emission Tomography-Computerized Tomogram in a Patient with Apparent Mesenteric Panniculitis: Biopsy Is Still the Answer. Case Rep Gastroenterol. 2009;3:131–137. doi: 10.1159/000213653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zissin R, Metser U, Hain D, Even-Sapir E. Mesenteric panniculitis in oncologic patients: PET-CT findings. Br J Radiol. 2006;79:37–43. doi: 10.1259/bjr/29320216. [DOI] [PubMed] [Google Scholar]


