Abstract
Objectives Numerous surgical approaches have been developed to access the petroclival region. The Kawase approach, through the middle fossa, is a well-described option for addressing cranial base lesions of the petroclival region. Our aim was to gather data about the variation of cranial nerve locations in diverse petroclival pathologies and clarify the most common pathologic variations confirmed during the anterior petrosal approach.
Method A retrospective analysis was made of both videos and operative and histologic records of 40 petroclival tumors from January 2009 to September 2013 in which the Kawase approach was used. The anatomical variations of cranial nerves IV–VI related to the tumor were divided into several location categories: superior lateral (SL), inferior lateral (IL), superior medial (SM), inferior medial (IM), and encased (E). These data were then analyzed taking into consideration pathologic subgroups of meningioma, epidermoid, and schwannoma.
Results In 41% of meningiomas, the trigeminal nerve is encased by the tumor. In 38% of the meningiomas, the trigeminal nerve is in the SL part of the tumor, and it is in 20% of the IL portion of the tumor. In 38% of the meningiomas, the trochlear nerve is encased by the tumor. The abducens nerve is not always visible (35%). The pathologic nerve pattern differs from that of meningiomas for epidermoid and trigeminal schwannomas.
Conclusion The pattern of cranial nerves IV–VI is linked to the type of petroclival tumor. In a meningioma, tumor origin (cavernous, upper clival, tentorial, and petrous apex) is the most important predictor of the location of cranial nerves IV–VI. Classification of four subtypes of petroclival meningiomas using magnetic resonance imaging is very useful to predict the location of deviated cranial nerves IV–VI intraoperatively.
Keywords: anterior petrosal approach, cranial nerves, anatomical variation, petroclival lesions
Introduction
Tumors of the petroclival region usually extend into both the middle and posterior fossae and then pass through the Meckel cave, which interconnects the fossae.1 2 3 4 The most common tumor types found in this region are meningiomas affecting the Meckel cave, schwannomas of the trigeminal nerve, and epidermoid tumors.2 5 6 7 8
To address skull base lesions extending toward both the middle and posterior cranial fossa, Yoshida and Kawase,9 and Kawase and colleagues10 proposed anterior petrosectomy as an extension to the subtemporal approach. Compared with conventional surgical approaches, the Kawase approach allows for better exposure of the ventral brainstem and for multiple working angles, with minimal brain retraction, around the porus trigeminalis.11 12 13
Nevertheless, despite many improvements in surgical access, the diversity of origin and histopathologic characteristics of lesions located in this region makes the growth pattern of such tumors highly unpredictable.14
It is important to spare injury or even manipulation of cranial nerves during this approach; however, it is not easy to predict the deviation of cranial nerves preoperatively because they are not visible even on magnetic resonance imaging (MRI). This article clarifies the most common site of deviation of cranial nerves IV–VI by operative findings confirmed during the anterior petrosal approach.
Data regarding nerve location variation using the Kawase approach will allow the surgeons to become more familiarized with intraoperative findings when using the anterior petrosectomy during the approach to petroclival lesions.
Methods and Materials
We analyzed retrospectively a body of data composed of surgical videos and operative and histologic records of 40 petroclival tumors between January 2009 and September 2013 in which the Kawase approach was used.
Anatomical variations of cranial nerves IV–VI related to the tumor were identified and then divided into five categories: superolateral (SL), inferolateral (IL), superomedial, inferomedial, and encased.
Regarding the location of the trigeminal nerve, the visibility of the trigeminal nerve before or after cutting the tentorium and the attachment of the trigeminal nerve to the tentorium was also considered. This body of categorical data was then analyzed to test for differences in frequency distributions between the pathologic subgroups (meningioma, epidermoid, and schwannoma) and different meningioma subgroups. Meningiomas were classified into the four subtypes was according to their origin, suspected location of major attachment, and direction of trigeminal nerve shift, based on preoperative MRI with gadolinium contrast and T2 sequence imaging findings, as follows:
Upper clivus (UC) type: Tumors with main attachment on the UC, medial to the Meckel cave, and not invading the cavernous sinus. Lateral shift of the trigeminal nerve is seen at operation.
Cavernous sinus (CS) type: Tumors with attachment on the UC, invading the posterior CS. Lateral shift of the trigeminal nerve is seen.
Tentorium (TE) type: Tumors with main attachment on the petroclinoid fold, medial TE. Inferomedial shift of the trigeminal nerve is seen.
Petrous apex (PA) type: Tumors with main attachment on the pyramidal apex, with or without invasion into the internal auditory meatus. Medial shift of the trigeminal nerve is seen.
Statistical Analysis
The data were analyzed using SPSS software v.22.0 (IBM, Chicago, Illinois, United States). Percentages were used to describe the relative frequency of the different variables under consideration. A series of Fisher exact tests was then performed to make inferences about differences in frequencies between different tumor categories and types of meningiomas. In all the analytical procedures involved, a two-sided p value < 0.05 for the test statistic was considered a statistically significant difference in relative frequency between the groups.
Results
Forty tumors were evaluated in this study consisting of 32 meningiomas, 5 schwannomas, and 3 epidermoids. Table 1 summarizes the location and other characteristics of the trochlear, trigeminal, and abducens nerves in different types of tumor. Although the trochlear nerve was mostly encased by a meningioma in 40.6% of the cases, it was located superomedially and superolaterally in 60% and 100% of the patients with schwannoma and epidermoid tumors, respectively. The results of the Fisher exact test showed that these differences in the location of the trochlear nerve is statistically significant between different types of tumors (p = 0.007). Encasement of the trigeminal nerve by tumor was reported in 43.8% and 40% of the subjects with a meningioma and schwannoma, respectively. By contrast, in none of the cases with epidermoid tumor was the trigeminal nerve found encased, and it was mostly located inferolaterally (66.7%). In addition, the trigeminal nerve was attached to the TE in only 25% of the patients with meningioma and not the other types of tumor.
Table 1. Locations and characteristics of trochlear, trigeminal, and abducens nerves different types of tumora .
| Type of tumor | Nerve | |||||||
|---|---|---|---|---|---|---|---|---|
| Trochlear | Trigeminal | Abducens | ||||||
| Location, % | Encasement, % | Location, % | Encasement, % | Tentorium attachment, % | Visibility time, % | Location, % | Encasement, % | |
|
Meningioma
(n = 32) |
SL: 15.6 IL: 0 SM: 21.9 IM: 6.3 E: 40.6 NS: 15.6 |
E: 40.6 NE: 43.8 NS: 15.6 |
SL: 34.3 IL: 21.9 E: 43.8 |
E: 43.8 NE: 56.2 |
A: 25.0 NA: 75.0 |
BCT: 29.0 ACT: 71.0 |
IL: 3.1 IM: 46.9 E: 15.6 NS: 34.4 |
E: 15.6 NE: 50.0 NS: 34.4 |
|
Schwannoma
(n = 5) |
SL: 0 IL: 20.0 SM: 60.0 IM: 0 E: 0 NS: 20.0 |
E: 0 NE: 80.0 NS: 20.0 |
SL: 40.0 IL: 20.0 E: 40.0 |
E: 40.0 NE: 60.0 |
A: 0 NA: 100 |
BCT: 50.0 ACT: 50.0 |
IL: 0 IM: 0 E: 0 NS: 100 |
E: 0 NE: 0 NS: 100 |
|
Epidermoid
(n = 3) |
SL: 100 IL: 0 SM: 0 IM: 0 E: 0 NS: 0 |
E: 0 NE: 100 NS: 0 |
SL: 33.3 IL: 66.7 E: 0 |
E: 0 NE:100 |
A: 0 NA: 100 |
BCT: 33.3 ACT: 66.7 |
IL: 0 IM: 100 E: 0 NS: 0 |
E: 0 NE: 100 NS: 0 |
| p value | 0.007 a | 0.176 | 0.520 | 0.423 | 0.604 | 0.803 | 0.123 | 0.049 a |
Abbreviations: A, attached to the tentorium; ACT, seen after cutting tentorium; BCT, seen before cutting tentorium; E, encased by the tumor; IL, inferolateral; IM, inferomedial; NA, not attached to the tentorium; NE, not encased by the tumor; NS, not seen; SL, superolateral; SM, superomedial.
Note: All statistical comparisons were performed using the Fisher exact test.
Statistical significant difference (p < 0.05).
The appearance of the trigeminal nerve was not significantly different between different tumor types (p = 0.803); however, it was seen before cutting the TE in half of the cases with schwannoma and a lower proportion of cases with epidermoid (33.3%) and meningioma (29.0%). Encasement of the abducens nerve was seen only in patients with meningioma (15.6%) and not the other two types; this difference was statistically significant (p = 0.049). In all the patients with epidermoid tumor and nearly half of those with a meningioma, the abducens nerve was located inferomedially.
Further assessment of nerve location was performed with regard to different types of meningiomas (Table 2). As shown in Fig. 3, in most of the cases, all different subtypes were encased by tumor tissue. Fig. 4 illustrates more differences in the location of the trigeminal nerve between different subtypes of meningioma that reached the borderline significant level (p = 0.050). As also listed in Table 2, the superolateral location of the trigeminal nerve was considerably more common (57.1%) among those with UC meningioma compared with other subtypes. However, encasement of the trigeminal nerve was mostly seen among those with cavernous meningioma (66.7%) where it was mostly reached after cutting the TE in 88.9% of the cases. As shown in Fig. 5, the abducens nerve was located inferomedially in most cases with different subtypes except for those with cavernous meningioma. Encasement of the abducens nerve was observed in 14.3% and 33.3% of patients with an UC and cavernous meningioma, respectively, whereas the nerve was not encased by tumor tissue in any of those with the TE or PA subtypes.
Table 2. Trochlear, trigeminal and abducens nerves locations and characteristics in different types of meningiomaa .
| Type of tumor | Nerve | |||||||
|---|---|---|---|---|---|---|---|---|
| Trochlear | Trigeminal | Abducens | ||||||
| Location, % | Encasement, % | Location, % | Encasement, % | Tentorium attachment, % | Visibility time, % | Location, % | Encasement, % | |
|
Upper clivus
(n = 14) |
SL: 21.4 SM: 21.4 IM: 7.2 E: 35.7 NS: 14.3 |
E: 35.7 NE: 50.0 NS: 14.3 |
SL: 57.1 IL: 14.3 E: 28.6 |
E: 28.6 NE: 71.4 |
A: 28.6 NA: 71.4 |
BCT: 42.9 ACT: 57.1 |
IL: 7.1 IM: 50.0 E: 14.3 NS: 28.6 |
E: 14.3 NE: 57.1 NS: 28.6 |
|
CS
(n = 9) |
SL: 22.2 SM: 11.1 IM: 0 E: 44.5 NS: 22.2 |
E: 44.5 NE: 33.3 NS: 22.2 |
SL: 22.2 IL: 11.1 E: 66.7 |
E: 66.7 NE: 33.3 |
A: 22.2 NA: 77.8 |
BCT: 11.1 ACT: 88.9 |
IL: 0 IM: 22.2 E: 33.3 NS: 44.5 |
E: 33.3 NE: 22.2 NS: 44.5 |
|
Tentorium
(n = 7) |
SL: 0 SM: 42.9 IM: 14.2 E: 42.9 NS: 0 |
E: 42.9 NE: 57.1 NS: 0 |
SL: 0 IL: 42.9 E: 57.1 |
E: 57.1 NE:42.9 |
A: 14.3 NA: 85.7 |
BCT: 16.7 ACT: 83.3 |
IL: 0 IM: 71.4 E: 0 NS: 28.6 |
E: 0 NE: 71.4 NS: 28.6 |
|
Petrous apex
(n = 2) |
SL: 0 SM: 0 IM: 0 E: 50.0 NS: 50.5 |
E: 50.0 NE: 0 NS: 50.0 |
SL: 50.0 IL: 50.0 E: 0 |
E: 0 NE:100 |
A: 50.0 NA: 50.0 |
BCT: 50.0 ACT: 50.0 |
IL: 0 IM: 50.0 E: 0 NS: 50.0 |
E: 0 NE: 50.0 NS: 50.0 |
| p value | 0.801 | 0.673 | 0.050 a | 0.161 | 0.759 | 0.302 | 0.612 | 0.422 |
Abbreviations: A, attached to the tentorium; ACT, (has been seen) after cutting tentorium; BCT, (has been seen) before cutting tentorium; E, encased by the tumor; IL, inferolateral; IM, inferomedial; NA, not attached to the tentorium; NE, not encased by the tumor; NS, not seen; SL, superolateral; SM, superomedial.
Note: All statistical comparisons are performed using the Fisher exact test.
Borderline significant difference (p < 0.05).
Fig. 3.
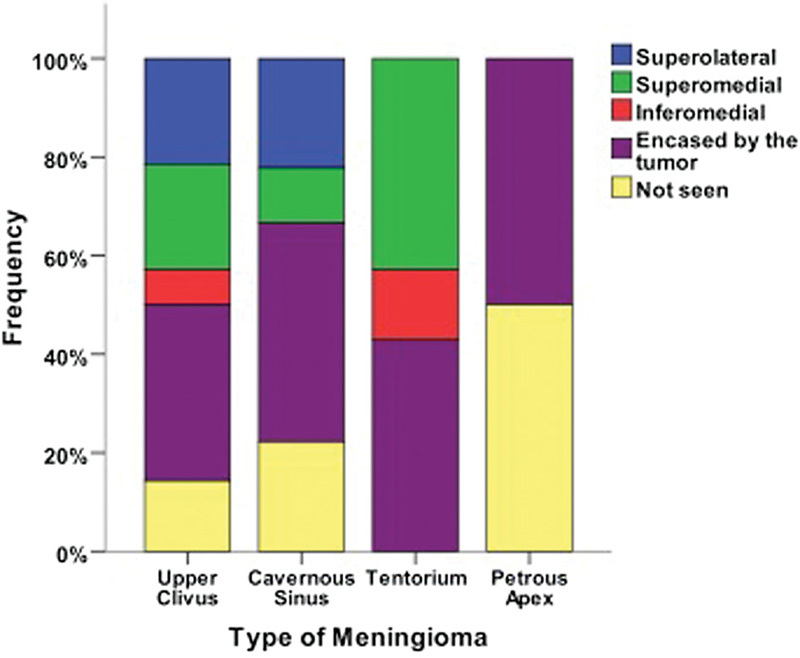
Frequency of different locations of the trochlear nerve regarding the type of meningioma in the study population.
Fig. 4.
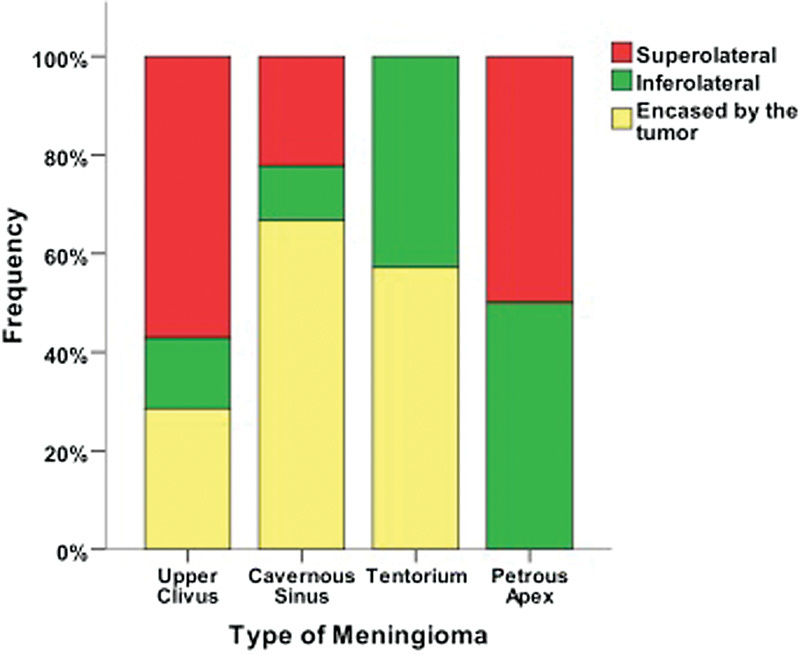
Frequency of different locations of the trigeminal nerve regarding the type of meningioma in the study population.
Fig. 5.
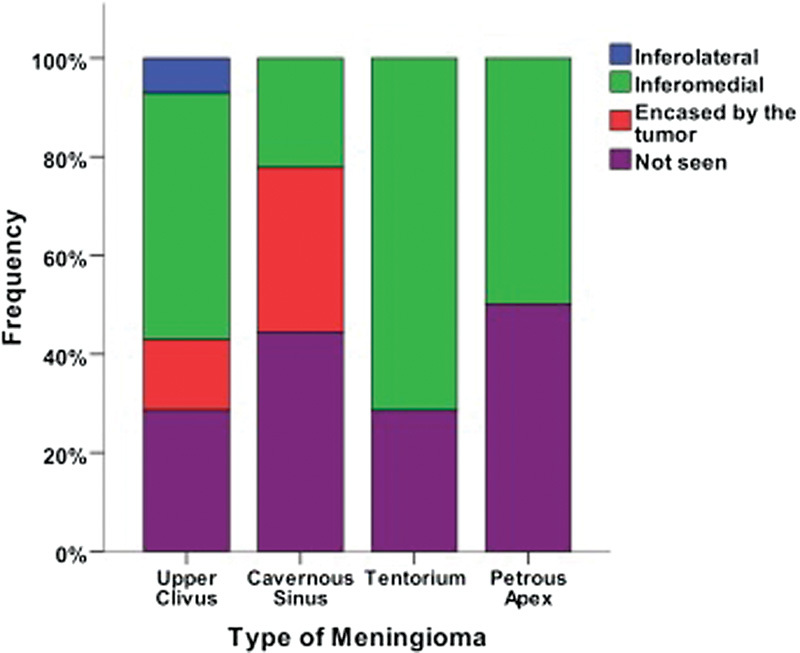
Frequency of different locations of the abducens nerve regarding the type of meningioma in the study population.
Discussion
Depending on the zone of adherence, basal posterior fossa meningiomas can be classified into clival, petroclival, spheno-petroclival, foramen magnum, and cerebellopontine angle (CPA) types.15 16
The tumors known as petroclival meningiomas can be broadly defined as those attached to the lateral sites along the petroclival borderline where the sphenoid, petrous, and occipital bone meet.17 18 19 20
It is not unusual that in some descriptions CPA meningiomas are erroneously interpreted as petroclival meningiomas. A more specific definition that distinguishes petroclival meningiomas from CPA meningiomas is that petroclival tumors originate at the petrous tip medial to the internal auditory canal.2
Petroclival tumors are located in an anatomically complex area containing dural folds, venous sinuses, and cranial nerves IV–XII. Therefore, even very small anatomical variations in the zone of origin can influence the outcome and present drastically different clinical features and choices of surgical approach.15 21
Based on MRI and surgical observations, Kawase et al preliminarily classified petroclival meningioma into the four subtypes listed earlier.15
Later, Ichimura et al focused on the study of clinical differences between these subtypes via the anterior transpetrosal approach.22 They evaluated 91 adults with petroclival meningioma who had undergone anterior petrosectomy for tumor removal excluding those with giant petroclival tumors with multiple attachments. Notably, they found trigeminal nerve symptoms in 80% of the patients and intraoperative invasion of the Meckel cave in 70% of the patients. For such tumors, these findings suggest using the Kawase approach because it provides a very suitable view for trigeminal porus and the Meckel cave when compared with other approaches such as the retrosigmoid suprameatal approach.23
The technique of surgically removing the PA to access the posterior cranial fossa was first reported by Kawase et al as an approach to aneurysms of the mid-basilar artery.13 Later they reported the use of this technique for meningiomas involving the petroclival region.
To avoid complications during this approach, it is necessary to identify anatomical structures and establish a reliable nerve identification and location system.
The petrous ridge, greater superficial petrosal nerve, mandibular nerve, and nerves inside the internal auditory canal limit the Kawase approach. However, the following surgical techniques can be used to deal with these limitations.
To access the posterior fossa from the middle fossa in the Kawase approach, the dura of the middle fossa must be peeled from the skull base until the petrous ridge is identified. The middle meningeal artery should be interrupted after coagulation to allow the manipulation beside the foramen spinosum. Also, it is easier to expose the anterior petrous bone over the arcuate eminence when the axis of the microscope is deviated anteriorly.11 24 25 26
The greater superficial petrosal nerve (GSPN) is the most reliable superficial landmark on the middle cranial fossa for drilling the PA (Kawase triangle) in the extradural anterior transpetrosal approach.10
Both facial nerve-evoked electromyogram (EMG) by antidromic GSPN stimulation and free-running facial muscle EMG monitoring are useful to confirm the GSPN as a landmark for safe extradural anterior petrosectomy and for the preservation of the GSPN itself.26
After drilling the anterior part of the petrous bone, the dura of the posterior fossa is exposed (Fig. 1). In this part of the approach, dural incisions are made above and below the superior petrosal sinus. At this point, a double Weck clip or ligature is applied to close the superior petrosal sinus and cuts are made toward an edge of the TE, behind the entrance point of the trochlear nerve, to preserve it.
Fig. 1.
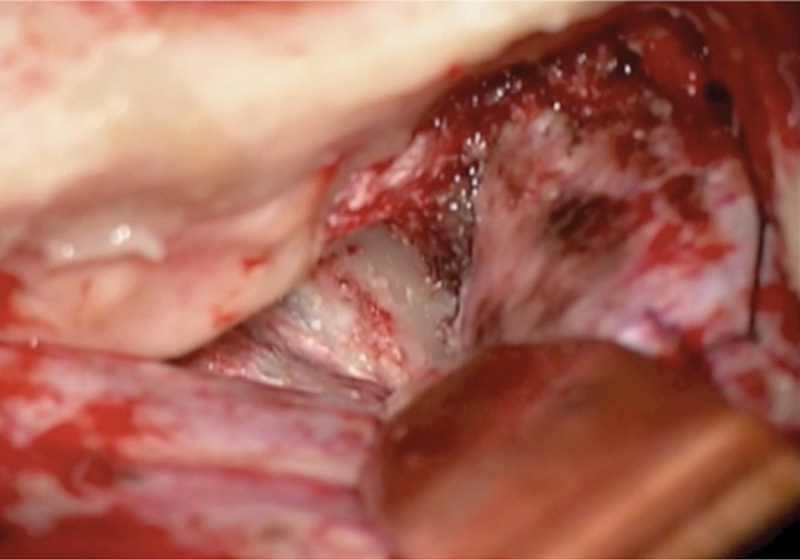
After drilling the anterior part of the petrous bone, the dura of the posterior fossa appeared.
Special care must be taken to keep a large enough distance between the petrosal vein and the anterior part of the sinus.10 Then the TE is cut until the TE notch is opened (Video 1).
Video 1
Appearance of the trochlear and trigeminal nerve at the lateral side of the pre-pontine epidermoid tumor after cutting and opening of the tentorium. Surgeon: Prof. Kazunari Yoshida. Online content including video sequence is available at: www.thieme-connect.com/products/ejournals/html/10.1055/s-0035-1555137
In cases where the tumor has invaded the TE, the incision can be made along the posterior margin of the lesions. Bilateral retraction of the tentorial leaflets with sutures allows for the visualization of the posterior fossa and anterior part of the pons. The dura incision of the middle fossa is then extended anteriorly to expose the lateral wall of the CS.
The central finding of this study is that during these multiple steps, a great deal of variation in the positions of cranial nerves is encountered. Also, the study's data suggest that these findings are not only limited to meningioma but also apply to epidermoid tumor of the CPA and trigeminal nerve schwannoma.
Trigeminal nerve visibility considering the attachment to the TE was also analyzed. Our data show that if the trigeminal nerve is located most laterally to the tumor, it is visible just after cutting the posterior fossa dura and before cutting the superior petrosal sinus (SPS). Otherwise trigeminal nerve location can be confirmed after cutting the SPS.
When considering pathologic subgroups (meningioma, epidermoid, and schwannoma) as well as meningioma origin (based on preoperative MRI),22 anatomical variations of the cranial nerves in epidermoid tumors show far fewer variations compared with meningioma subtypes and trigeminal schwannomas (p = 0.007 for trochlear nerve and 0.049 for abducens nerve; see Table 1).
Epidermoid Tumor
In our epidermoid series, the trochlear nerve was located in 33% of the cases at the superolateral part of the tumor and in 66% of the cases at the inferolateral part, but it was always visible directly after opening the TE (not encased) (Table 1, Fig. 2, and Video 1).
Fig. 2.

The position of the trochlear nerve in a prepontine epidermoid tumor after opening the tentorium. Black arrow denotes trigeminal nerve and blue arrow denotes trochlear nerve.
The trigeminal nerve was always not encased, and in 66% of the cases it was visible after cutting the TE. The abducens nerve was also always at the inferomedial part of the tumor and not encased.
All of our data about nerve variation in epidermoid tumors show that the removal of this type of tumor via anterior petrosectomy is easier than when dealing with other tumors, which is compatible with the histopathologic characteristics of this tumor.27 28
Meningioma
A key finding of our study is that statistical analysis of nerve position differs according to the type of petroclival meningioma. Our statistical analysis shows that the location of the trigeminal nerve (not trochlear and abducens nerve) differs (statistically significant) according to the subtypes of petroclival meningioma, based on tumor origin, just as described by Kawase et al and Ichimura et al22 (Table 2; Figs. 3 4 5).
The different trochlear and abducens nerve positions according to petroclival meningioma type were not statistically significant in this study. Figs. 3 4 5 show the various location and characteristics of cranial nerves IV–VI by subtype of petroclival meningioma. The schematic view in Fig. 6 highlights the definition of various positions of the trigeminal nerve described in our study. The different variations of trigeminal nerve position based on meningioma's subtypes are described in Fig. 4.
Fig. 6.
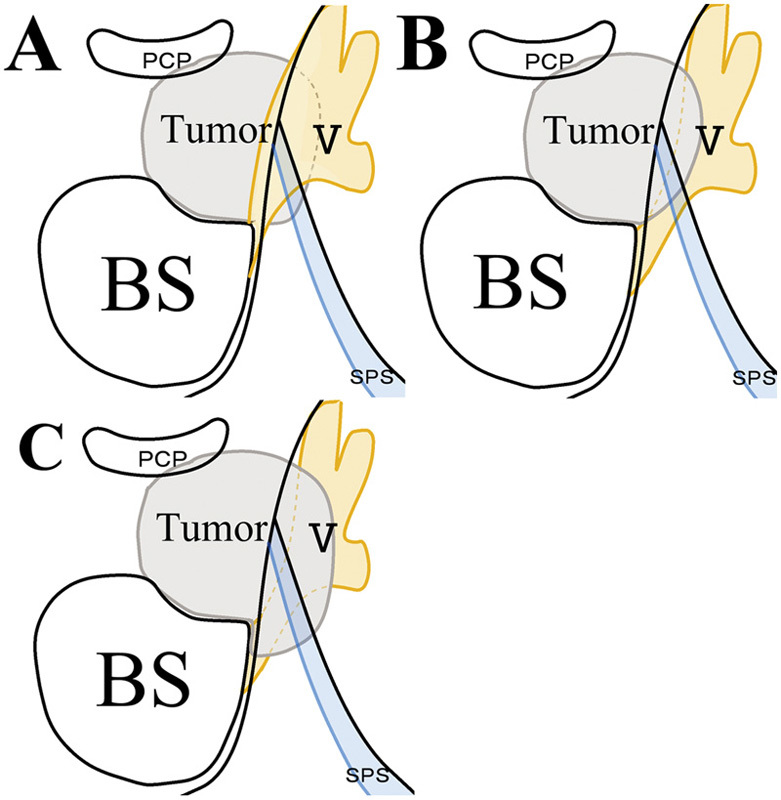
Schematic highlight of trigeminal nerve position described in our study. (A) Superolateral to the tumor. (B) Inferolateral to the tumor. (C) Encased in the tumor. BS, brainstem; PCP, posterior clinoid process, SPS, superior petrosal sinus (Schematic drawing: Ryosuke Tomio, MD, Keio University, Tokyo, Japan).
As described in the study by Ichimura et al, the invasion rate of the meningioma to the middle fossa and Meckel cave is significantly linked to tumor origin. For instance, in this study only 20% of PA meningioma cases showed trigeminal nerve symptoms clinically and invasion to the Meckel cave intraoperatively. In this study, the absence of encased trigeminal nerve in a PA-type tumor was identified. In contrast, for CS-type tumors, the trigeminal nerve is often encased (> 65%). Our intraoperative results confirmed those of Ichimura et al in that the most common type of tumor with clinical findings of hypoesthesia occurs when the tumor is of the CS type (p < 0.002).
The pattern of the trochlear nerve also differs by type of meningioma. Our statistical analysis shows that depending on the type of meningioma, it is not always easy to identify the trochlear nerve (Fig. 3). Personal clinical experience also emphasizes this finding because our data show that a rate of ∼ 20% of temporary trochlear paresis occurs after anterior petrosectomy.22 25
In some cases of petroclival meningioma (between 10% and 30% based on tumor origin), due to incomplete tumor removal, it is not possible to see the abducens nerve intraoperatively. The visualization of the abducens nerve is a very reliable sign for complete tumor removal10 (Figs. 5 and 7).
Fig. 7.
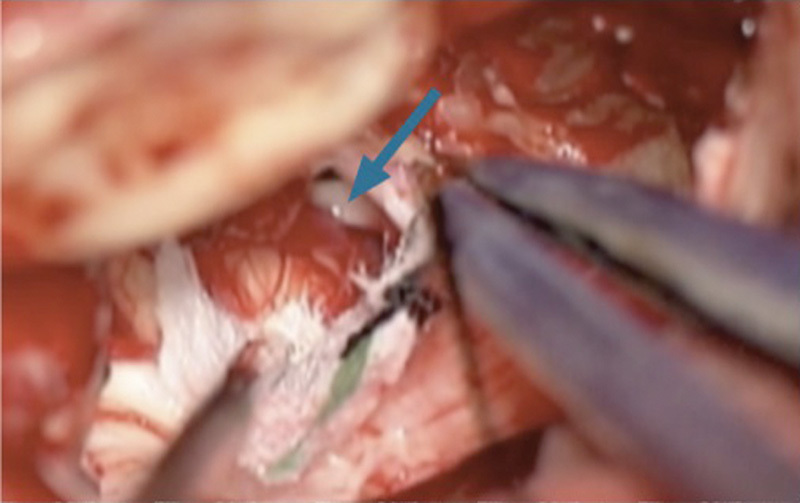
Visualization of the abducens nerve (arrow) after removing the tumor is a reliable sign for complete tumor removal.
Technical Pearls in Meningioma Microsurgery
The experience of our senior author (T.K.) confirms our statistical analysis of the location of cranial nerves as we describe in this section.
These technical pearls will help plan surgery in a way that preserves nerve function and leads to improved surgical outcomes:
In the upper clival type, cranial nerve V is compressed under the SPS (superior petrosal sinus), and ligation and cutting of the SPS must avoid injuring the nerve. SPS ligation close to Meckel cave is dangerous, and it is better made more posteriorly (above the internal auditory meatus [IAM]). For tumor removal, mobilization of the fifth nerve covering the tumor is necessary, and the opening of Meckel cave is beneficial to mobilize and remove the tumor in the cave. The sixth nerve appears in the medial side of the tumor between the anterior inferior cerebellar artery and basilar artery, and they are good landmarks. The sixth nerve is sometimes encased at the dural entrance point, but the cisternal portion is mostly free from the tumor. Cerebrospinal fluid leakage from the prepontine cistern is a reliable sign for the final stage of tumor removal. The seventh and eighth nerves are well preserved by this approach, since they are protected by a posteriorly elongated fifth nerve, and it is an advantage of this approach compared with suboccipital approach.
In the CS type, the clival dura is compressed posteriorly by the tumor, and the subdural space is very narrow. All cranial nerves are mostly encased and vulnerable to injury. Total removal is not possible, and surgery is less successful.
In the tentorial type, the fourth nerve is usually encased at the entrance point to the TE. However if the nerve is sacrificed, incidence of radical removal is very high with this approach, since attached TE can be removed with the tumor. The sixth nerve is seldom encased because it is protected by the medially shifted fifth nerve.
In the PA type, the fifth nerve is sometimes compressed and flattened by the tumor at its entry point, causing trigeminal neuralgia. Radical removal is easy, because the fourth and sixth nerves are not mostly encased, except for the tumor invading the IAM.
Trigeminal Schwannoma
The pattern of nerves in trigeminal schwannoma showed unexpected results. In 60% of trigeminal nerve schwannomas, the trigeminal nerve is not encased in the tumor. This means that the tumor pushes the trigeminal nerve to the lateral side of the tumor (Table 1).
Also, in 80% of trigeminal schwannomas, it was easy to identify the trochlear nerve at the inferolateral part (20%) before tumor resection or at the superomedial part (60%) after tumor resection. Yet in 20% of trigeminal schwannoma cases, it was not possible to see and identify the trochlear nerve. The abducens nerve was not observed in 100% of these tumors. This means that the invasion of the trigeminal nerve is frequently in the longitudinal axis rather than crosswise.9
To summarize, the various types of meningiomas, based on origin, show significantly different variations in nerve location. Also, that variation of the trigeminal nerve in meningioma cases is statistically relevant both clinically and anatomically.22
The main complications of anterior petrosectomy beside drilling of vital structures such as semicircular canals and facial or cochlear nerve injury because of opening the internal auditory canal unintentionally, is nerve injury due to adhesion with the tumor or tumor encasement.25 29 The incidence of these severe complications could be reduced by taking advantage of data that we described in our study.
Conclusion
The location pattern of cranial nerves IV–VI of different types of petroclival tumors was analyzed, and statistically significant differences were found. For meningioma, tumor type (cavernous, upper clival, tentorial, and PA) is the most important predictor of IV–VI nerve location.
Classification of four subtypes of petroclival meningiomas using MRI is very useful to predict the location of deviated cranial nerves IV–VI intraoperatively. Technical points of how to preserve them using the anterior petrosal approach were discussed.
Understanding theses variations and a way to estimate nerve position will help plan surgery in a way that preserves nerve function and leads to improved surgical outcomes.
Footnotes
Disclosure Hamid Borghei-Razavi (MD) received Carl-Zeiss Scholarship from German Society of Neurosurgery (DGNC) for German/Japan exchange program.
References
- 1.Al-Mefty O, Ayoubi S, Smith R R. The petrosal approach: indications, technique, and results. Acta Neurochir Suppl (Wien) 1991;53:166–170. doi: 10.1007/978-3-7091-9183-5_27. [DOI] [PubMed] [Google Scholar]
- 2.Al-Mefty O, Fox J L, Smith R R. Petrosal approach for petroclival meningiomas. Neurosurgery. 1988;22(3):510–517. doi: 10.1227/00006123-198803000-00010. [DOI] [PubMed] [Google Scholar]
- 3.Cheung S W, Jackler R K, Pitts L H, Gutin P H. Interconnecting the posterior and middle cranial fossae for tumors that traverse Meckel's cave. Am J Otol. 1995;16(2):200–208. [PubMed] [Google Scholar]
- 4.Spetzler R F, Hamilton M G, Daspit C P. Petroclival lesions. Clin Neurosurg. 1994;41:62–82. [PubMed] [Google Scholar]
- 5.Aziz K M Tew J M Jr Chicoine M R Chicoine M R; van Loveren HR. The Kawase approach to retrosellar and upper clival basilar aneurysms Neurosurgery 19994461225–1234.; discussion 1234–1236 [PubMed] [Google Scholar]
- 6.Al-Mefty O, Ayoubi S, Gaber E. Trigeminal schwannomas: removal of dumbbell-shaped tumors through the expanded Meckel cave and outcomes of cranial nerve function. J Neurosurg. 2002;96(3):453–463. doi: 10.3171/jns.2002.96.3.0453. [DOI] [PubMed] [Google Scholar]
- 7.Bricolo A P Turazzi S Talacchi A Cristofori L Microsurgical removal of petroclival meningiomas: a report of 33 patients Neurosurgery 1992315813–828.; discussion 828 [DOI] [PubMed] [Google Scholar]
- 8.Day J D Fukushima T The surgical management of trigeminal neuromas Neurosurgery 1998422233–240.; discussion 240–241 [DOI] [PubMed] [Google Scholar]
- 9.Yoshida K, Kawase T. Trigeminal neurinomas extending into multiple fossae: surgical methods and review of the literature. J Neurosurg. 1999;91(2):202–211. doi: 10.3171/jns.1999.91.2.0202. [DOI] [PubMed] [Google Scholar]
- 10.Kawase T Shiobara R Toya S Anterior transpetrosal-transtentorial approach for sphenopetroclival meningiomas: surgical meningiomas: surgical method and results in 10 patients Neurosurgery 1991286869–875.; discussion 875–876 [PubMed] [Google Scholar]
- 11.Kawase T, Shiobara R, Toya S. Middle fossa transpetrosal-transtentorial approaches for petroclival meningiomas. Selective pyramid resection and radicality. Acta Neurochir (Wien) 1994;129(3–4):113–120. doi: 10.1007/BF01406489. [DOI] [PubMed] [Google Scholar]
- 12.Abdel Aziz K M Sanan A van Loveren H R Tew J M Jr Keller J T Pensak M L Petroclival meningiomas: predictive parameters for transpetrosal approaches Neurosurgery 2000471139–150.; discussion 150–152 [PubMed] [Google Scholar]
- 13.Kawase T, Toya S, Shiobara R, Mine T. Transpetrosal approach for aneurysms of the lower basilar artery. J Neurosurg. 1985;63(6):857–861. doi: 10.3171/jns.1985.63.6.0857. [DOI] [PubMed] [Google Scholar]
- 14.Ahlhelm F, Nabhan A, Naumann N, Grunwald I, Shariat K, Reith W. Skull base tumors [in German] Radiologe. 2005;45(9):807–815. doi: 10.1007/s00117-005-1259-1. [DOI] [PubMed] [Google Scholar]
- 15.Kawase T, Shiobara R, Ohira T, Toya S. Developmental patterns and characteristic symptoms of petroclival meningiomas. Neurol Med Chir (Tokyo) 1996;36(1):1–6. doi: 10.2176/nmc.36.1. [DOI] [PubMed] [Google Scholar]
- 16.Yasargil M G, Mortara R W, Cruic M. Vienna, Austria: Springer; 1980. Meningiomas of basal posterior cranial fossa; pp. 3–115. [Google Scholar]
- 17.Markham J W, Fager C A, Horrax G, Poppen J L. Meningiomas of the posterior fossa; their diagnosis, clinical features, and surgical treatment. AMA Arch Neurol Psychiatry. 1955;74(2):163–170. [PubMed] [Google Scholar]
- 18.Mayberg M R, Symon L. Meningiomas of the clivus and apical petrous bone. Report of 35 cases. J Neurosurg. 1986;65(2):160–167. doi: 10.3171/jns.1986.65.2.0160. [DOI] [PubMed] [Google Scholar]
- 19.Umansky F, Elidan J, Valarezo A. Dorello's canal: a microanatomical study. J Neurosurg. 1991;75(2):294–298. doi: 10.3171/jns.1991.75.2.0294. [DOI] [PubMed] [Google Scholar]
- 20.Bricolo A P Turazzi S Talacchi A Cristofori L Microsurgical removal of petroclival meningiomas: a report of 33 patients Neurosurgery 1992315813–828.; discussion 828 [DOI] [PubMed] [Google Scholar]
- 21.Sekhar L N, Wright D C, Richardson R, Monacci W. Petroclival and foramen magnum meningiomas: surgical approaches and pitfalls. J Neurooncol. 1996;29(3):249–259. doi: 10.1007/BF00165655. [DOI] [PubMed] [Google Scholar]
- 22.Ichimura S, Kawase T, Onozuka S, Yoshida K, Ohira T. Four subtypes of petroclival meningiomas: differences in symptoms and operative findings using the anterior transpetrosal approach. Acta Neurochir (Wien) 2008;150(7):637–645. doi: 10.1007/s00701-008-1586-x. [DOI] [PubMed] [Google Scholar]
- 23.Chang S W Wu A Gore P et al. Quantitative comparison of Kawase's approach versus the retrosigmoid approach: implications for tumors involving both middle and posterior fossae Neurosurgery 200964(3, Suppl):ons44–ons51.; discussion ons51–ons52 [DOI] [PubMed] [Google Scholar]
- 24.Borghei-Razavi H, Tomio R, Toda M, Schick U, Kawase T, Yoshida K. The safety of Kawase triangle as an anatomical landmark for anterior petrosectomy in petroclival meningiomas. J Neurol Surg B. Skull Base. 2014;75(2):a163. doi: 10.1016/j.clineuro.2015.10.032. [DOI] [PubMed] [Google Scholar]
- 25.Tomio R, Toda M, Yoshida K, Borghei-Razavi H. Anterior petrosal approach [letter to the editor] J Neurosurg. 2014;120(5):1249–1250. doi: 10.3171/2013.10.JNS132121. [DOI] [PubMed] [Google Scholar]
- 26.Tomio R, Akiyama T, Ohira T, Horikoshi T, Yoshida K. Usefulness of facial nerve monitoring for confirmation of greater superficial petrosal nerve in anterior transpetrosal approach. Acta Neurochir (Wien) 2014;156(10):1847–1852. doi: 10.1007/s00701-014-2162-1. [DOI] [PubMed] [Google Scholar]
- 27.Sabin H I, Bordi L T, Symon L. Epidermoid cysts and cholesterol granulomas centered on the posterior fossa: twenty years of diagnosis and management. Neurosurgery. 1987;21(6):798–805. doi: 10.1227/00006123-198712000-00004. [DOI] [PubMed] [Google Scholar]
- 28.Schroeder H W, Oertel J, Gaab M R. Endoscope-assisted microsurgical resection of epidermoid tumors of the cerebellopontine angle. J Neurosurg. 2004;101(2):227–232. doi: 10.3171/jns.2004.101.2.0227. [DOI] [PubMed] [Google Scholar]
- 29.Gupta S K, Salunke P. Intradural anterior petrosectomy for petroclival meningiomas: a new surgical technique and results in 5 patients: technical note. J Neurosurg. 2012;117(6):1007–1012. doi: 10.3171/2012.9.JNS12429. [DOI] [PubMed] [Google Scholar]


