Policy Points:
Latino immigrants have recently spread beyond traditional US enclaves to “emerging destinations.” The arrival of limited English proficiency (LEP) Spanish‐speakers to these areas can challenge the health care system, as translation services may not be readily available for LEP patients.
Trained auditors posed as family members of LEP patients seeking primary care in a safety net setting. We found substantially lower appointment availability for LEP adults in emerging destinations compared to traditional destinations.
Greater bilingual resources are needed within safety net clinics to accommodate LEP Spanish speakers as this population continues to grow and expand throughout the United States.
Context
Recent demographic trends show Latino immigrants moving to “emerging destinations” outside traditional Latino enclaves. Immigrants in emerging destinations with limited English proficiency (LEP) may experience greater challenges finding health care services oriented to their linguistic needs than those in traditional enclaves, especially if the supply of language resources in these areas has not kept pace with new demand.
Methods
This study uses an experimental audit design to directly compare the ability of uninsured Spanish‐speaking LEP adults to access interpreter services and to obtain new patient primary care appointments at federally qualified health centers (FQHCs) across traditional and emerging destinations. We additionally compare the appointment rates of English‐proficient uninsured and English‐proficient Medicaid patients across these destinations that contacted the same FQHCs. English‐proficient patients serve as an access benchmark that is independent of differences in Spanish language services.
Findings
Results indicate that LEP Spanish‐speaking patients within emerging destinations are 40 percentage points less likely to receive an appointment than those in traditional destinations. English‐proficient groups, by contrast, experience similar levels of access across destinations. Disparities in safety net provider access by destination status are consistent with differences in the availability of bilingual services. Ninety‐two percent of FQHCs in traditional destinations offered appointments with either Spanish‐speaking clinicians or translation services with non‐clinical bilingual staff, while only 54% did so in emerging destinations. LEP patients denied care in emerging destinations must also travel greater distances than in traditional destinations to reach the next available safety net provider.
Conclusions
Our findings highlight that current language resources in emerging destinations may be inadequate for keeping up with the transforming needs of the patient population. As the Latino immigrant population continues to expand and diffuse, better accommodation within the health care safety net is likely to increase in importance.
About one‐tenth of the us population ages 5 and over (25.3 million people) qualifies as having limited English proficiency (LEP), characterized by restricted ability to read, write, speak, or understand English. Over 80% of the LEP population is foreign‐born and more than 60% is Spanish‐speaking.1, 2 Of the foreign‐born Latino population, nearly two‐thirds are LEP.3 LEP populations are less educated than the general Latino population on average and more likely to be employed in manual and low‐skilled labor (men) or service and personal care (women). Relatedly, an elevated proportion of the LEP population lives below the federal poverty line, making this group a highly vulnerable subset of the broader Latino community.1
There have also been meaningful changes in the geographic location of LEP Latino individuals across the United States. Mexican immigrants traditionally settled in California, the broader Southwest, and large gateway cities (eg, Chicago). Cuban immigrants largely moved to South Florida, while Puerto Ricans and Dominicans established communities in New York. Yet, recent population flows have shifted toward “emerging destination” areas. These areas, often located in the Southeast and Midwest, lack long‐standing Latino immigrant communities, but have experienced some of the fastest rates of growth in recent years.4, 5, 6 Fifty percent of the immigrant population in these areas are LEP.7 Consequently, many Latino LEP individuals and families find themselves in areas with relatively little experience accommodating LEP Spanish speakers.
This diffusion has generated a rich area of research that investigates Latino experiences across established and emerging destinations in regards to spatial assimilation patterns,8, 9, 10, 11, 12, 13, 14 economic, political, and social integration,15, 16 children's educational development,17‐21and children's risk of being born into poverty.17 However, there has been far less research comparing health care access and outcomes for Latinos across the two destination types.
Because growth in the LEP Latino population has outpaced the supply of linguistic support services in other settings, such as in education,18, 20 there is a risk of similar challenges for community‐based health care. Studies have examined evolving health care needs of Latinos in rural areas22, 23 as well as issues facing a growing midwestern Latino population,24 but we are aware of only one published study that compares adult health outcomes across established and emerging destinations. Gresenz and colleagues show that US‐born Mexican immigrants in emerging destinations are less likely to have a usual source of care and are less satisfied with that care than their counterparts in traditional destinations.25 The authors’ findings are important since access to health care may be one of the salient resources that affect the health status of Latinos in different communities—and substantive health disparities are already a known problem for this particular group.26 In this way, Gresenz and colleagues’ work brings needed attention to a potentially overlooked population health issue and also highlights an important gap in the literature.25 However, Gresenz and colleagues do not examine bilingual resources, which may heavily influence the care experiences and options of LEP individuals.
While there now exists a substantial evidence base for the existence of health disparities between LEP and non‐LEP populations,27, 28, 29 there is comparatively little evidence about how much of this disparity might be attributable to health system factors (after adjusting for other patient‐level disadvantages). If the health care resources, especially those in safety net settings that provide care to the underserved, are failing to reach these groups, then an already vulnerable population may be further burdened by unmet medical needs.
In this study, we compare the ability of Spanish‐speaking uninsured LEP adults to access interpreter services and obtain new patient primary care appointments at federally qualified health centers (FQHCs) at traditional versus emerging destinations. Our focus on FQHCs stems from their mandate to care for low‐income and underserved populations. Recent work shows their importance for these patient populations,30, 31 which suggests that FQHCs could be a needed resource for LEP individuals. Additionally, of the 24 million patients seen within FQHCs annually, roughly one‐third belong to Latino groups,32 and disparities in access to care between LEP and non‐LEP populations narrow with closer proximity to an FQHC.33 That said, some FQHCs may not be sufficiently equipped or adapting fast enough to meet the needs of a patient population undergoing a demographic shift.
To simulate the real‐world experience of patients seeking medical care, we employ an experimental audit methodology. The audit methodology uses standardized callers posing as real patients to help separate differences in the behavior of clinic schedulers from differences in the types of patients seeking care across areas. We also measure the access experiences of English‐proficient uninsured and Medicaid‐insured adults at these same clinics to benchmark against the uninsured Spanish‐speaking LEP findings and to help disentangle the influences of language barriers from other local environmental factors. As a complementary investigation, we estimate the distance to the geographically closest alternative FQHC for LEP patients unable to receive care at the contacted FQHC. This analysis further illuminates how limited access can lead to additional travel burdens among this vulnerable population when seeking care.
Research Motivation
LEP Barriers to Health Care
Access to health care is a long‐standing issue for LEP individuals. Nearly 40% of the LEP population is uninsured,34 reducing their likelihood of pursuing care and effectively barring them from large swaths of the health care system. Although growing numbers of Latinos are gaining health insurance coverage under the Patient Protection and Affordable Care Act of 2010 (ACA)—especially low‐income, US‐born Latinos and documented Latino immigrants—these benefits may not apply to all Latinos.35 Many members of the LEP community are undocumented, and the ACA specifically excludes undocumented immigrants from Medicaid expansions as well as subsidized private insurance through health insurance marketplaces.36, 37 Moreover, only a minority of states have taken it upon themselves to increase coverage for these individuals.38 LEP individuals' lower than average socioeconomic status also implies a limited ability to personally finance their current or future health care needs; low‐income households typically hold less than two weeks’ worth of income in cash, checking, or banking accounts.39 Even when LEP individuals access care, navigating the system is challenging due to language difficulties. Within a national sample of insured Latinos seeking primary care services, LEP individuals were significantly more likely to struggle with appointment scheduling, waiting for care, and obtaining information over the phone.40 Similarly, a comparison of LEP and non‐LEP adults with poor health found that LEP individuals were more likely to report difficulty understanding their doctor.41 Availability of interpreter services (particularly services provided by a trained, rather than a lay, interpreter) can attenuate these issues for the LEP population,42, 43 but such resources are not always widely available.
Legislative Landscape
FQHCs are subject to state and federal oversight. In principle, some level of access to interpreter services at FQHCs is guaranteed under federal law. Under the prohibition against national origin discrimination, outlined in Title VI of the Civil Rights Act, the US Department of Health and Human Services (HHS) requires all entities receiving federal funding (including private entities accepting payment from Medicare or Medicaid) to “take reasonable steps to ensure meaningful access to their programs and activities by LEP persons.”44 When deciding the priority of offering LEP services, each organization or program—including hospitals, physicians, and community health centers—must take into account the number or proportion of the eligible patient population that is LEP, the frequency of contact with LEP individuals, the implications of the program for patients’ lives, and the available resources and costs. Upon an analysis of these factors, each federal funding recipient is expected to determine the appropriate level of language assistance.
At the same time, the Public Health Service Act45 includes requirements about facilities, staffing, and acceptance of patients. It requires all organizations wishing to serve as FQHCs to fulfill a language services requirement if the center's patient population consists of a “substantial number” of LEP individuals, though what represents “substantial” is undefined.45 Each center then must develop a plan for providing services specific to the language needs of the patient population as well as identify a bilingual staff member to act as an intermediary between patients and providers (see §330 of the Public Health Service Act for details). Despite the legislative guidance targeting services for LEP populations, there are no guarantees a given FQHC will have such resources on hand. Moreover, the acquisition of new or improved language resources at emerging destination FQHCs (ie, clinics within areas experiencing new growth in LEP Spanish speakers) may lag behind changing patient demographics.
Research Design
Audit Study Design
The primary experimental data were collected using an audit (simulated patient) methodology. The strength of an audit methodology lies in its ability to elicit real‐world behavior, rather than responses to the hypothetical situations of traditional survey methodology, which may be biased in various ways (eg, social desirability, recall, or non‐response biases). Additionally, audit designs can more effectively isolate the influence of particular factors (in this case LEP status) than observational studies.
Our audit study focused on adult primary care, with a sampling frame comprising FQHCs that provided such services and were located in 10 diverse states: Arkansas, Georgia, Iowa, Illinois, Massachusetts, Montana, New Jersey, Pennsylvania, Oregon, and Texas. The 10 states represent a purposive sample that provides a demographic and geographically diverse set of states. In addition, the states represent nearly 30% of the US population. The list of possible FQHCs was obtained from the Health Resources and Services Administration's (HRSA) public data files on FQHCs and FQHC “lookalike” facilities.46 Because the HRSA list may not be up‐to‐date (eg, if a facility has changed its service and/or patient population emphasis or is no longer in operation), our team verified the sampling frame using a nonexperimental call to each potential clinic identified from the current HRSA list. The nonexperimental calls confirmed the FQHC's existence (ie, not a closed or seasonal facility), correct contact information, and provision of adult primary care services. Of the 724 potential FQHCs identified in the HRSA list, 575 were confirmed and therefore included in the sampling frame. We then used tabulations of the 2000 and 2010 decennial Censuses obtained from the Pew Hispanic Center to classify the county associated with a given FQHC as either an emerging or traditional destination.47 Using similar criteria adapted from other published studies,25, 48, 49 we defined emerging and traditional destinations at the county level. Traditional destinations were counties with at least a 20% Latino population in 2010. Emerging destination counties were those with less than a 12% Latino population in 2010, at least 75% growth in the Latino population between 2000 and 2010, and a Latino population of at least 500 individuals in 2010. This methodology identified 107 FQHCs in emerging destinations and 156 FQHCs in traditional destinations across the full sample frame, which were then eligible for audit experimental calls. No FQHCs that met our selection criteria were located in Montana, which eliminated it from our study. Texas and Illinois had a disproportionate number of potentially eligible traditional destination clinics (76 and 59, respectively); thus, we took a random sample of 40 FQHCs located in traditional destinations from each of these 2 states to help balance the distribution of clinics across our 9 study states. Combining these randomly drawn subsamples with all traditional destination FQHCs from all other states gave us 100 clinic observations in total for the traditional group. Combined with the 107 FQHCs in emerging destinations, we identified 207 FQHCs in total.
Under the audit design, trained field staff called FQHCs posing as an English‐proficient relative (nephew or niece) of a Spanish‐speaking LEP adult seeking a primary care appointment. The audit scenario was kept consistent across callers: the person needing the appointment was reported to have poor English language skills, be of the opposite sex of the caller (and therefore would not want the caller to attend the visit), and be both uninsured and a legal resident of the United States (if asked). Audit callers requested the earliest available appointment at which the family member could be seen with any language accommodation, including a doctor, nurse practitioner, or other provider acting as a translator, another on‐site interpreter, or simultaneous phone translation. The first available appointment with interpreter services was accepted, regardless of the type of services available. Callers also asked clinics about the types of interpreter and language services available to accommodate LEP Spanish speakers, as well as other specific language services questions. If offered an appointment, the caller noted the date of the visit. For those appointments that could be affirmatively scheduled, the caller canceled the appointment at the end of the call. All calls were completed during the months of November and December 2014. Of the 207 unique FQHCs in the experimental sample, 197 were successfully contacted (7 were unable to be reached and 3, when called, stated they did not take uninsured patients).
While the audit experimental design can provide unbiased estimates of the appointment rates within each destination type (eg, traditional and emerging), it does not necessarily allow us to attribute any disparities in appointment rates across settings to language barriers for uninsured LEP Spanish speakers. Local environmental factors (eg, how busy the clinic is) could drive differential appointment rates for all types of patients, not just LEP Spanish speakers. In addition, appointment rates for the uninsured may be different than insured populations irrespective of LEP status. To directly address this, we leverage additional audit data that included English‐proficient uninsured and English‐proficient Medicaid experimental callers. The English‐proficient version was from a larger audit study conducted between June and September 2014 in which trained field staff posed as English‐proficient individuals seeking a primary care appointment for themselves. It is fully detailed in a recent paper.50 With the exception of the LEP elements embedded within the current study's audit design, the English‐proficient scenario closely paralleled the experimental procedure used here. We then mapped the experimental results for English‐proficient uninsured and English‐proficient Medicaid patients to the FQHCs identified and included in this study. Although there is not a perfect overlap between the two audit data sources, 147 of the 197 FQHCs called under the LEP study were also called in both the English‐proficient uninsured and English‐proficient Medicaid scenarios. Another 4 clinics called within this study received English‐proficient Medicaid calls as well. We then used this combined data source to determine if differences in access outcomes were unique to Spanish‐speaking LEP callers or common across all prospective patient groups. Going forward, we use the term “patient group” as shorthand for the 3 types of prospective patient groups.
Appointment Measures and Language Services
Our primary outcome, “Appointment,” is defined as a binary variable equal to one when the caller successfully received a specific appointment date to be seen and zero otherwise. Sometimes only an appointment range was made available to a caller. To accommodate these ambiguous cases, we created an alternative appointment rate measure. The alternative outcome, “Appointment with Range,” takes a value of one if the caller received a specific date or a range of potential dates and is zero otherwise. The second measure ensures that our results and inferences are not sensitive to the inclusion or exclusion of ambiguous cases. Among those receiving an appointment, “Days to Appointment” is calculated as the number of days from the date of the call to the date of the scheduled appointment and provides us with a measure of how soon an individual can ultimately receive care. This in turn offers insights into potential clinic capacity issues.
We also examine differences in Spanish language and interpreter services across destinations through a series of questions that were asked during each audit call. “Phone Tree” indicates whether there was an automated message at the beginning of the call giving a Spanish language option (1 = yes, 0 = no). Nearly all clinics used phone trees as an initial means of fielding phone calls. “Spanish Access” is a hierarchical variable that records the highest level of Spanish‐language accommodation available for the first available appointment with language accommodation. In order, these options were (1) appointment with a Spanish‐speaking provider, including a physician, nurse practitioner, or physician assistant; (2) appointment with a non‐bilingual provider in which a bilingual staff member or interpreter would be physically in the room; and (3) appointment with a non‐bilingual provider assisted by remote translation technology (eg, telephone translator). These approaches represent a continuum, with greater resource investment generally involved in retaining bilingual providers or other staff. Only the highest response was recorded for each call. If none of these options were available, the caller recorded that no Spanish language accommodation was available. If callers recorded that a non‐clinical staff member would act as a translator, callers then ascertained the availability of the translator, assigning “Always Interpreter” a value of one if there is always/usually an interpreter available at the clinic and a value of zero if the interpreter is only available for specific days and/or hours. Callers also recorded whether they were asked if they could bring their own translator. “Own Translator” is coded with a one for “yes” and zero otherwise. Finally, callers asked whether their LEP aunt/uncle could speak to a Spanish‐speaker at the clinic if they had to call in advance of the appointment (1 = yes, 0 = no).
Empirical Analysis
We first examine descriptive differences in the aggregate appointment rates at FQHCs across patient groups and destinations. We then formally test for statistical differences between traditional and emerging destination appointment rates within a regression framework. This is accomplished with a linear probability model that includes a set of interactions for patient group and FQHC presence in an emerging destination. The regression specification is as follows:
| (1) |
For clinic i in patient group p, Yip represents the binary outcome of interest, Pip is a vector that represents the type of patient caller (eg, English‐proficient uninsured—the reference group, English‐proficient Medicaid, or LEP Spanish‐speaking uninsured), and Ei is a dichotomous variable that represents whether the FQHC is located in an emerging (1) or traditional (0) Latino‐immigrant destination. The interaction terms, Ei * Pip, capture any differential likelihood of receiving an appointment for patients contacting FQHCs within emerging communities. Any differential seen for uninsured LEP Spanish speakers in emerging destinations but not English‐proficient Medicaid patients in emerging destinations would be consistent with language barriers inhibiting access within the local safety net clinic. We ultimately estimate the specification twice, once with the full sample and once limiting the sample to FQHCs that were called under all 3 patient groups as a sensitivity check. The latter specification ensures that the non‐overlap in FQHCs called between the LEP Spanish‐speaking and English‐proficient versions do not influence the resulting estimates. As an additional sensitivity check, we conduct a series of re‐estimations that excludes observations from a single state. This approach helps ensure that state‐specific features or undetected relevant policies that go beyond federal statutes are not affecting our results and inferences. We also modify our main specification (Equation [1]) by including state fixed effects to generate our final robustness check. This analysis consequently compares appointment rates across patient groups within the same state. Throughout all regression analyses, we cluster our standard errors at the clinic level to reflect multiple calls to the same clinic.
We also examine the distribution of days until the appointment for patient groups across destinations to help determine if there are any unobserved differences influencing appointment availability. For example, if clinics within one setting disproportionately face greater demands for care (or possess more limited resources), we would expect to see longer wait times for patients receiving appointments, as well as lower appointment rates overall. To add further context to our appointment‐based results, we describe the type of Spanish language and interpreter services available at FQHCs within emerging and traditional destinations.
Lastly, an inability to receive care at a local FQHC in an emerging destination would likely necessitate a search for services elsewhere. To partly quantify this additional cost facing a given patient, we calculate the mean and median distance to both the next closest FQHC and the nearest “migrant health clinic” (as labeled in the HRSA data) for each of the 197 FQHCs called in our study. We identify 181 migrant health clinics from the same HRSA list used to construct the FQHC sample frame. To conduct this analysis, the FQHCs and the migrant health clinics are geographically plotted. The shortest “as the crow flies” distance between an FQHC and the next nearest facility is then calculated, which is likely an underestimate of the true travel time between facilities because it neglects the actual road route. We also note that the migrant health clinics are assumed to be operational and relevant (ie, they did not receive the pre‐experimental calls that the FQHCs did), but this may not be the case. Moreover, the geographically closest alternative clinic still may not be able to accommodate the patient and/or their full care needs, so this is an optimistic scenario from the patient's perspective. For these reasons, our ancillary analysis of distance to a primary care alternative is likely conservative and will understate the true burden facing many individuals denied access to their local safety net clinic.
Results
The FQHCs in this study are located in states whose counties vary widely in their Latino population. Six states contain FQHCs located in counties that fit our traditional Latino destination criterion (eg, Georgia, Iowa, Illinois, Massachusetts, New Jersey, and Texas), while all 9 states contain FQHCs in counties that meet our emerging destination criteria. Despite differences in the number of completed calls, the proportion of clinics in our sample located in emerging and traditional destinations does not vary by patient group (see Appendix Table A1 for a complete description).
Accessing Care
Figure 1 displays aggregate appointment rates for each patient group stratified by destination type. LEP Spanish‐speaking patients residing in emerging destinations are far less likely to receive an appointment relative to identical patients seeking care at FQHCs within traditional destinations. Less than 50% of LEP Spanish‐speaking callers receive an appointment in emerging destinations compared to more than 80% in traditional destinations. There is no similar difference across destinations in the appointment rates for English‐proficient Medicaid and English‐proficient uninsured patients. In fact, the rates are slightly higher in emerging destinations—opposite what is observed for LEP Spanish‐speakers.
Figure 1.
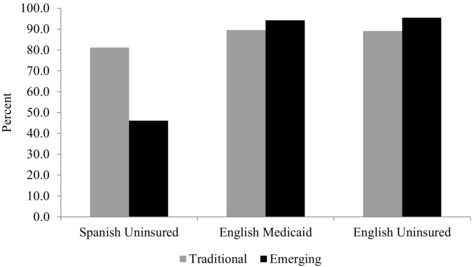
Percent of Patients Receiving an Appointment at an FQHC by Patient Language and Insurance Group and Destination Typea
a“Spanish Uninsured” are those in the LEP Spanish‐speaking patient group. “English Medicaid” and “English Uninsured” are those from the complementary English‐proficient audit study according to their respective insurance types. Traditional destination counties were defined as counties with at least a 20% Latino population in 2010. Emerging destination counties were defined as counties with less than a 12% Latino population in 2010, at least 75% growth in the Latino population between 2000 and 2010, and a Latino population of at least 500 individuals in 2010.
The multivariate results on the likelihood of receiving an appointment (Table 1) empirically test the differences in appointment availability across destinations seen in Figure 1. The “Spanish‐Emerging” interaction term confirms the large discrepancy seen in the descriptive results, indicating a 41 percentage points reduction in the probability of obtaining an appointment for uninsured LEP Spanish speakers in emerging destinations as compared to uninsured English‐proficient patients in traditional destinations (in the full sample specification, P<.001; = −.421 in the restricted sample limited to FQHCs that were called under all 3 patient groups). Similar results are also found under the alternative dependent variable (Appendix Table A2) and when excluding one state at a time or using state fixed effects (Appendix Tables A3 and A4, respectively). Meanwhile, the interaction for English‐proficient Medicaid patients and the non‐interacted “Emerging” (capturing English‐proficient uninsured callers within emerging destinations) coefficients suggest no differential access issues when seeking care from FQHCs in emerging areas. Neither is statistically significant.
Table 1.
Linear Probability Model Predicting the Likelihood of Receiving an Primary Care Appointment at an FQHCa
| Full Sampleb | Restricted Samplec | |||
|---|---|---|---|---|
| Covariate | Coefficient | P‐value | Coefficient | P‐value |
| Emerging | .064 | .176 | .064 | .177 |
| (.047) | (.047) | |||
| Spanish uninsured | −.080 | <.05 | −.060 | .155 |
| (.040) | (.038) | |||
| English Medicaid | .005 | .918 | .002 | .972 |
| (.047) | (.048) | |||
| Spanish‐emerging | −.414 | <.001 | −.421 | <.001 |
| (.068) | (.072) | |||
| Eng. Medicaid‐emerging | −.017 | .763 | −.001 | .986 |
| (.058) | (.057) | |||
| Constant | .891 | <.001 | .891 | <.001 |
| (.039) | (.039) | |||
| n | 463 | 409 | ||
“Spanish Uninsured” are those in the LEP Spanish‐speaking patient group. “English Medicaid” are those from the complementary English‐proficient Medicaid patient group. Standard errors are presented in parentheses.
Sample size varies by patient group. N = 197, 136, and 130 for LEP Spanish‐speaking uninsured, English‐proficient Medicaid, and English‐proficient uninsured, respectively.
The restricted sample is limited to clinics that were called under all 3 patient groups. Sample size varies by patient group. N = 147, 132, and 130 for LEP Spanish‐speaking uninsured, English‐proficient Medicaid, and English‐proficient uninsured, respectively.
There is no evidence to suggest clinician availability is driving the lower appointment rates of LEP Spanish‐speaking patients in emerging destinations (Table 2). On average, these patients wait nearly a week less than their counterparts in traditional destinations (9.0 vs. 15.6 days). The median wait time is also lower and the distribution tighter in emerging destinations. Additionally, the pattern of wait times is identical across all 3 patient groups—suggesting that so long as the FQHC is able to schedule an appointment for a LEP Spanish‐speaker, the patient does not face additional delays compared to other patient groups.
Table 2.
Days to Appointment with a Primary Care Physician at an FQHC by Patient Group and Destination Type
| Spanish Uninsured | English Medicaid | English Uninsured | ||||||
|---|---|---|---|---|---|---|---|---|
| Traditional | Emerging | P‐value | Traditional | Emerging | P‐value | Traditional | Emerging | |
| 25th percentile | 3 | 3 | – | 3 | 4 | – | 2.5 | 3 |
| Median | 12 | 7 | – | 8.5 | 7 | – | 8.5 | 7 |
| Mean | 15.6 | 9.0 | p<.01 | 15.3 | 10.5 | p<.1 | 13.1 | 10.6 |
| 75th percentile | 21 | 14 | – | 25 | 15 | – | 18.5 | 13 |
| n | 77 | 47 | 60 | 65 | 56 | 62 | ||
Language and Interpreter Services
Table 3 presents the Spanish language and interpreter services available for LEP Spanish‐speaking patients across the two destinations. Fewer FQHCs in emerging destinations offered a Spanish language option as part of the automated phone tree at the beginning of the call (P<.001). When asked for the highest level of Spanish language accommodation available, 43% of FQHCs in traditional destinations offered appointments with Spanish‐speaking clinicians while another 49% provided nonclinical bilingual staff as translators. In contrast, the proportions were 19% (P<.001) and 35% (P<.05), respectively, in emerging destinations. Additionally, more than one‐third of the FQHCs in emerging destinations offered no Spanish accommodation whatsoever, compared to 5% in traditional destinations (P<.001). Callers to these clinics were instead more likely to be asked if they could bring their own translator to the appointment. Even when a translator was available, the translator was less likely to always or usually be available at FQHCs in emerging destinations. Lastly, LEP Spanish speakers were less likely to be able to reach a Spanish‐speaker at an emerging destination FQHC if they needed to call prior to their appointment date. The divergence in language resources across the two destinations is consistent with the disparate appointment rates for LEP patients seen in Figure 1 and Table 1.
Table 3.
Availability of Spanish Language and Interpreter Services at FQHCs for Spanish Speakers by Destination Typea
| Outcome | Traditional (%) | Emerging (%) | P‐value |
|---|---|---|---|
| Spanish language option available in phone tree at beginning of call | 0.61 | 0.36 | <.001 |
| Highest level of spanish language accommodation available | – | – | – |
| spanish speaking provider | 0.43 | 0.19 | <.001 |
| bilingual staff translator | 0.49 | 0.35 | <.05 |
| phone/other technology | 0.00 | 0.08 | <.01 |
| no spanish accommodation | 0.05 | 0.37 | <.001 |
| Unable to determine | 0.02 | 0.01 | .527 |
| Asked if could bring own translator | 0.03 | 0.20 | <.001 |
| Translator always availableb | 0.98 | 0.86 | <.1 |
| Spanish speaker available if need to call before appointmentc | 0.98 | 0.70 | <.001 |
| n | 95 | 102 |
For FQHCs called under the LEP Spanish‐speaking patient group.
Conditional on the highest level of accommodation available being a bilingual staff translator. N = 83.
Most clinics only answered this question conditional on scheduling an appointment. N = 146.
Distance to Next Nearest FQHC
Table 4 reports the mean and median crow flies distance in miles from all 197 successfully contacted clinics to the next‐closest FQHC and to the nearest migrant health clinic, by destination type. On average, the next‐nearest FQHC is 8.5 miles away for clinics located in traditional destination counties. In emerging destination counties, the average distance to the next‐nearest clinic is nearly 70% farther away (14.3 miles), a statistically significant difference (P<.01). When using median distance, the gap is accentuated with the next‐nearest FQHC more than 6 times farther away in emerging compared to traditional destinations (11.6 vs. 1.9 miles, P<.001). As previously mentioned, the actual travel time by vehicle may be longer, particularly for those reliant on public transportation (if even available). The differential distances are less pronounced when examining migrant health clinics; however, these facilities are far fewer and less accessible overall. As discussed earlier, we are unable to ascertain the operational status of these clinics—making them a less clear source of adult primary care in our data. For both clinic types, there is no guarantee that the closest alternative will have the resources and capacity to provide care for the uninsured LEP individual—in fact, our data suggest that they typically do not in emerging destinations. Therefore, the true access hurdles for LEP individuals in these areas is likely to be considerably higher.
Table 4.
Mean and Median Travel Distance from Closest FQHC to Next‐Closest FQHC and to Nearest Migrant Clinic
| Next‐Closest FQHC | Nearest Migrant Clinic | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| n | Mean (miles) | P‐value | Median (miles) | P‐value | Mean (miles) | P‐value | Median (miles) | P‐value | |
| Traditional | 95 | 8.46 | 1.87 | 83.67 | 43.9 | ||||
| Emerging | 102 | 14.26 | <.01 | 11.62 | <.001 | 78.93 | .605 | 77.93 | <.1 |
Discussion
Using an experimental audit methodology, our research examines differences in primary care access for uninsured LEP Spanish speakers across established and emerging Latino destinations, with a focus on FQHCs, since they serve as key access points for underserved populations.30, 31 Our empirical analysis reveals that uninsured LEP Spanish speakers residing in emerging destinations have greater difficulty in obtaining a primary care appointment relative to their counterparts in established areas. No comparable access differential is evident for English‐proficient patient groups seeking care, and the results related to wait times do not indicate any capacity constraints for emerging destination FQHCs. Instead, insufficient bilingual or translation resources appear to drive the lower appointment rates for LEP individuals within emerging areas. LEP patients who are unable to get an appointment with language accommodation are also likely to be further burdened with long travel distances to the next available safety net clinic—which may also be ill equipped for accommodating LEP Spanish speakers.
This research adds to the broader immigration literature and builds on Gresenz and colleagues (2012) by showing clear disparities in health care access for LEP Spanish speakers in emerging rather than traditional destinations.25 Moreover, the lower provision of language services available at emerging destination safety net clinics mirrors findings of fewer linguistic supports in the school setting,18, 20 suggesting a common problem for multiple social welfare initiatives. As emerging destinations are defined by a rapidly growing Latino population, the collective evidence highlights the potential for new and increasing language service needs within these communities.
For the public health safety net specifically, our data imply that the provision of interpreter services in emerging destinations may lag behind shifts in the underlying patient population. This issue could be especially severe given the limited health care alternatives open to uninsured immigrants and therefore should not be overlooked. Policymakers and public health programs should bear these issues in mind when allocating resources and designing future care delivery channels.
Several policy levers could augment access to interpreter services. The Department of Health and Human Services has the ability to award grants to eligible health centers with a substantial LEP population to facilitate the provision of translation and interpretation services.45 Evolving regulations could also increase provision of interpreter services. HHS’s finalized regulations on implementing the civil rights provision of the ACA (§Section 1557) require “free, accurate, and timely language” services as necessary to ensure equal opportunity of access as well as to prevent health care providers from relying on LEP patients to provide their own translation services (including an accompanying minor except in rare circumstances). In addition, the regulations require all eligible centers to publicly display a notice detailing the free availability of language assistance services in the 15 most common languages spoken within the state.51 Lastly, special programs could invest in training Spanish‐speaking clinicians and could provide incentives to Spanish‐speaking providers to move to high‐need areas. Providing face‐to‐face care, with services offered in the patient's own language, would likely enhance culturally competent care.52 Importantly, audit methods, such as those used in this study, can provide a useful tool for tracking progress in this care domain over the coming years.
Despite the strong research design and unique application within immigrant health research, this study has several limitations. The experiment is of modest scale, and the results are not generalizable beyond the adult LEP Spanish‐speaking population seeking primary care appointments at safety net clinics located in 9 US states. However, FQHCs are highly relevant to this patient population and the chosen states are intentionally diverse, reflecting a blend of traditional and emerging destinations that is similar to the larger United States. The study is not able to differentiate the adult LEP Spanish‐speaking population by gender or country of origin, examine the experience of other language‐speakers with LEP, or address other barriers to care facing the adult LEP population. The study also does not address accessibility to the pediatric health care system for LEP Spanish‐speaking children, although some very recent work finds access to care and perceived quality to be largely similar between Latino children residing in emerging and traditional destinations.53 All of these topics are opportunities for future research. In addition, the 2 audits did not take place simultaneously, with the LEP Spanish‐speaking audit occurring 2 months after the conclusion of the English‐proficient version, though it is unlikely that this small temporal gap affects the results. Additionally, the study only focuses on new patient availability rather than ongoing care for existing patients, and it does not measure quality of care or whether language services are actually provided during a visit.
Conclusion
At this time, the larger US health care system risks a growing gap between the demand for and supply of medical services that can adapt to LEP Spanish‐speaking patient needs. Even traditional Latino areas are facing shortages in Spanish‐speaking providers.54 Our study suggests the safety net infrastructure is lacking Spanish‐speaking health care resources in areas witnessing the largest expansions in their Latino immigrant populations. Better accommodation within the public health system and social safety net will likely be key in the short run and can influence the long‐term health and well‐being of current and future generations of Spanish‐speaking immigrants within the United States.
Funding/Support
Funding for the study comes from the Center for Emergency Care Policy & Research at the University of Pennsylvania. The study additionally uses comparison data collected under grant #70160 from the Robert Wood Johnson Foundation.
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. No disclosures were reported.
Acknowledgment: The authors would like to acknowledge Daniel Polsky, Ari Friedman, and Simon Basseyn from the University of Pennsylvania and Genevieve M. Kenney, Douglas Wissoker, and Stephen Zuckerman from the Urban Institute for their helpful comments. They would also like to thank Martha Van Haitsma, Tiana Pyer‐Pereira, and the team of research assistants at the University of Chicago Survey Lab, as well as Alfredo Gonzalez, Geraldo Hernandez, Maria Rizzetto, and Huiting Xu for their excellent work in gathering the data.
Appendix Figure A1.

Predicted Probability of Patients Receiving an Appointment at an FQHC by Patient Language and Insurance Group and Destination Typea
aPredicted probabilities estimates derived from the linear probability model described in Table 1. “Spanish Uninsured” are those in the LEP Spanish‐speaking patient group. “English Medicaid” and “English Uninsured” are those from the complementary English‐proficient audit study according to their respective insurance types.
Table A1.
Count and State Location of FQHC Sample by Patient Group and Destination Type a
| Spanish Uninsured | English Medicaid | English Uninsured | ||||
|---|---|---|---|---|---|---|
| State | Traditional | Emerging | Traditional | Emerging | Traditional | Emerging |
| AR | 0 | 4 | 0 | 3 | 0 | 3 |
| GA | 5 | 28 | 5 | 18 | 5 | 18 |
| IA | 1 | 3 | 0 | 3 | 0 | 3 |
| IL | 36 | 9 | 29 | 8 | 28 | 7 |
| MA | 4 | 9 | 2 | 6 | 2 | 6 |
| NJ | 10 | 6 | 5 | 5 | 4 | 5 |
| OR | 0 | 5 | 0 | 4 | 0 | 4 |
| PA | 0 | 35 | 0 | 28 | 0 | 27 |
| TX | 39 | 3 | 32 | 3 | 32 | 3 |
| Percent | 0.48 | 0.52 | 0.48 | 0.52 | 0.48 | 0.52 |
| Total | 95 | 102 | 73 | 78 | 71 | 76 |
“Spanish Uninsured” are those in the LEP Spanish‐speaking patient group. “English Medicaid” and “English Uninsured” are those from the complementary English‐proficient audit study according to their respective insurance types.
Table A2.
Linear Probability Model Predicting the Likelihood of Receiving an Appointment with Range at an FQHC
| Full Sample a | Restricted Sample b | |||
|---|---|---|---|---|
| Covariate | Coefficient | P‐value | Coefficient | P‐value |
| Emerging | .057 | .179 | .057 | .180 |
| (.043) | (.043) | |||
| Spanish uninsured | −.028 | .468 | −.000 | 1.000 |
| (.038) | (.035) | |||
| English Medicaid | −.000 | 1.000 | −.003 | .950 |
| (.045) | (.046) | |||
| Spanish‐emerging | −.363 | <.001 | −.380 | <.001 |
| (.065) | (.069) | |||
| Eng. Medicaid‐emerging | −.012 | .831 | .003 | .949 |
| (.054) | (.053) | |||
| Constant | .901 | <.001 | .901 | <.001 |
| (.036) | (.036) | |||
| n | 488 | 434 | ||
Sample size varies by patient group. N = 197, 147, and 144 for LEP Spanish‐speaking uninsured, English‐proficient Medicaid, and English‐proficient uninsured, respectively. Standard errors are presented in parentheses.
The restricted sample is limited to clinics that were called under all 3 patient groups. Sample size varies by arm. N = 147, 143, and 144 for LEP Spanish‐speaking uninsured, English‐proficient Medicaid, and English‐proficient uninsured, respectively.
Table A3.
Linear Probability Model Predicting the Likelihood of Receiving an Appointment at an FQHC, by State Exclusiona
| No AR | No GA | No IA | No IL | No MA | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Covariate | Coefficient | P‐value | Coefficient | P‐value | Coefficient | P‐value | Coefficient | P‐value | Coefficient | P‐value |
| Emerging | .062 | .199 | .076 | .138 | .062 | .199 | .030 | .571 | .047 | .314 |
| (.048) | (.051) | (.048) | (.052) | (.046) | ||||||
| Spanish | −.060 | .115 | −.050 | .186 | −.060 | .115 | −.061 | .264 | −.064 | <.1 |
| uninsured | (.038) | (.038) | (.038) | (.054) | (.038) | |||||
| English | .002 | .972 | −.000 | 1.000 | .002 | .972 | .002 | .968 | .016 | .738 |
| Medicaid | (.048) | (.052) | (.048) | (.051) | (.047) | |||||
| Spanish‐ | −.413 | <.001 | −.392 | <.001 | −.441 | <.001 | −.412 | <.001 | −.402 | <.001 |
| emerging | (.073) | (.076) | (.073) | (.085) | (.075) | |||||
| Eng. | −.001 | .987 | −.020 | .745 | −.001 | .987 | −.001 | .984 | .001 | .989 |
| Medicaid‐ | (.058) | (.063) | (.058) | (.060) | (.055) | |||||
| emerging | ||||||||||
| Constant | .891 | <.001 | .883 | <.001 | .891 | <.001 | .921 | <.001 | .905 | <.001 |
| (.039) | (.042) | (.039) | (.044) | (.037) | ||||||
| n | 400 | 342 | 400 | 312 | 390 | |||||
| No NJ | No OR | No PA | No TX | |||||
|---|---|---|---|---|---|---|---|---|
| Covariate | Coefficient | P‐value | Coefficient | P‐value | Coefficient | P‐value | Coefficient | P‐value |
| Emerging | .068 | .175 | .061 | .207 | .086 | <.1 | .095 | .150 |
| (.050) | (.048) | (.046) | (.066) | |||||
| Spanish uninsured | −.062 | .121 | −.060 | .115 | −.060 | .116 | −.062 | .152 |
| (.040) | (.038) | (.038) | (.043) | |||||
| English Medicaid | .002 | .970 | .002 | .972 | .002 | .972 | −.019 | .789 |
| (.051) | (.048) | (.048) | (.072) | |||||
| Spanish‐emerging | −.424 | <.001 | −.448 | <.001 | −.427 | <.001 | −.424 | <.001 |
| (.075) | (.074) | (.087) | (.077) | |||||
| Eng. Medicaid‐emerging | −.001 | .985 | .015 | .788 | −.024 | .703 | .020 | .799 |
| (.061) | (.056) | (.063) | (.079) | |||||
| Constant | .883 | <.001 | .891 | <.001 | .891 | <.001 | .857 | <.001 |
| (.042) | (.039) | (.039) | (.060) | |||||
| n | 384 | 397 | 336 | 311 | ||||
Each Model excludes all FQHCs located in one state. Standard errors are presented in parentheses.
Table A4.
Linear Probability Model Predicting the Likelihood of Receiving an Appointment at an FQHC, with State Fixed Effects
| Full Sample a | Restricted Sample b | |||
|---|---|---|---|---|
| Covariate | Coefficient | P‐value | Coefficient | P‐value |
| Emerging | .105 | <.1 | .106 | <.1 |
| (.058) | (.061) | |||
| Spanish | −.077 | <.05 | −.056 | .150 |
| uninsured | (.039) | (.038) | ||
| English | .011 | .817 | .008 | .872 |
| Medicaid | (.047) | (.048) | ||
| Spanish‐ | −0.401 | <.001 | −.419 | <.001 |
| emerging | (.067) | (.072) | ||
| Eng. | −.023 | .691 | −.007 | .904 |
| Medicaid‐ | (.057) | (.056) | ||
| emerging | ||||
| Georgia | .059 | .572 | .008 | .933 |
| (.103) | (.099) | |||
| Iowa | .270 | <.01 | .222 | <.05 |
| (.096) | (.093) | |||
| Illinois | .043 | .703 | .015 | .897 |
| (.112) | (.112) | |||
| Massachusetts | −.254 | <.1 | −.227 | .181 |
| (.153) | (.169) | |||
| New Jersey | .215 | <.1 | .138 | .211 |
| (.111) | (.110) | |||
| Oregon | .216 | <.1 | .139 | .242 |
| (.122) | (.118) | |||
| Pennsylvania | .032 | .769 | −.007 | .948 |
| (.110) | (.106) | |||
| Texas | .155 | .163 | .110 | .320 |
| (.111) | (.110) | |||
| Constant | .790 | <.001 | .829 | <.001 |
| (.122) | (.111) | |||
| n | 463 | 409 | ||
Sample size varies by patient group. N = 197, 136, and 130 for LEP Spanish‐speaking uninsured, English‐proficient Medicaid, and English‐proficient uninsured, respectively. Standard errors are presented in parentheses.
Sample size varies by patient group. N = 147, 132, and 130 for LEP Spanish‐speaking uninsured, English‐proficient Medicaid, and English‐proficient uninsured, respectively.
References
- 1. Zong J, Batalova J. The limited English proficient population of the United States. Migration Policy Institute website. http://www.migrationpolicy.org/article/limited-english-proficient-population-united-states/#13. Published July 8, 2015. Accessed March 31, 2015.
- 2. Zong J, Batalova J. Frequently requested statistics on immigrants and immigration in the United States. Migration Policy Institute website. http://www.migrationpolicy.org/article/frequently-requested-statistics-immigrants-and-immigration-united-states#Immigrant%20Population%20Change. Updated April 27, 2016. Accessed March 31, 2015.
- 3. Gambino CP, Acosta YD, Grieco, EM . English‐Speaking Ability of the Foreign‐Born Population in the United States: 2012. American Community Survey Reports, ACS‐26. Washington, DC: U.S. Census Bureau; June 2014. https://www.census.gov/content/dam/Census/library/publications/2014/acs/acs-26.pdf. Accessed May 1, 2016. [Google Scholar]
- 4. Lichter DT, Johnson KM. Immigrant gateways and Hispanic migration to new destinations. Int Migration Rev. 2009;43(3):496‐518. [Google Scholar]
- 5. Massey DS. New Faces in New Places: The Changing Geography of American Immigration. New York: Russell Sage Foundation; 2008. [Google Scholar]
- 6. Portes A, Rumbaut RG. Immigrant America: A Portrait. Berkeley: University of California Press; 2006. [Google Scholar]
- 7. Terrazas A. Immigrants in new‐destination states. Migration Policy Institute website. http://www.migrationpolicy.org/article/immigrants-new-destination-states. Published February 8, 2011. Accessed May 2, 2016. [Google Scholar]
- 8. Fischer MJ, Tienda M. Redrawing spatial color lines: Hispanic metropolitan dispersal, segregation, and economic opportunity In: Tienda M, Mitchell F, eds. Hispanics and the Future of America. Washington, DC: National Academies Press; 2006:100‐137. [PubMed] [Google Scholar]
- 9. Hall M. Residential integration on the new frontier: immigrant segregation in established and new destinations. Demography. 2013;50(5):1873‐1896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Iceland J, Scopilliti M. Immigrant residential segregation in U.S. metropolitan areas, 1990‐2000. Demography. 2008;45(1):79‐94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lichter DT, Parisi D, Taquino MC, Grice SM. Residential segregation in new Hispanic destinations: cities, suburbs, and rural communities compared. Soc Sci Res. 2010;39(2):215‐230. [Google Scholar]
- 12. Lichter DT, Sanders SR, Johnson KM. Hispanics at the starting line: poverty among newborn infants in established gateways and new destinations. Soc Forces. 2015;94(1):209‐235. [Google Scholar]
- 13. Park J, Iceland J. Residential segregation in metropolitan established immigrant gateways and new destinations, 1990‐2000. Soc Sci Res. 2011;40(3):811‐821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Tienda M, Fuentes N. Hispanics in metropolitan America: new realities and old debates. Annu Rev Sociol. 2014;40:499‐520. [Google Scholar]
- 15. Smith H, Furuseth O, eds. Latinos in the New South: Transformations of Place. Burlington, VT: Ashgate Publishing Company; 2006. [Google Scholar]
- 16. Zuniga V, Hernandez‐Leon R, eds. New Destinations: Mexican Immigration in the United States. New York: Russell Sage Foundation; 2005. [Google Scholar]
- 17. Clotfelter CT, Ladd HF, Vigdor JL. New destinations, new trajectories? The educational progress of Hispanic youth in North Carolina. Child Dev. 2012;83(5):1608‐1622. [DOI] [PubMed] [Google Scholar]
- 18. Dondero M, Muller C. School stratification in new and established Latino destinations. Soc Forces. 2012;91(2):477‐502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Fischer MJ. Immigrant educational outcomes in new destinations: an exploration of high school attrition. Soc Sci Res. 2010;39(4):627‐641. [Google Scholar]
- 20. Bohon SA, MacPherson H, Atiles JH. Educational barriers for new Latinos in Georgia. J Latinos Educ. 2005;4(1):43‐58. [Google Scholar]
- 21. Stamps K, Bohon SA. Educational attainment in new and established Latino metropolitan destinations. Soc Sci Q. 2006;87(5):1225‐1240. [Google Scholar]
- 22. Blewett LA, Smaida SA, Fuentes C, Zuehlke EU. Health care needs of the growing Latino population in rural America: focus group findings in one midwestern state. J Rural Health. 2003;19(1):33‐41. [DOI] [PubMed] [Google Scholar]
- 23. Casey MM, Blewett LA, Call KT. Providing health care to Latino immigrants: community‐based efforts in the rural Midwest. Am J Public Health. 2004;94(10):1709‐1711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Harari N, Davis M, Heisler M. Strangers in a strange land: health care experiences for recent Latino immigrants in Midwest communities. J Health Care Poor Underserved. 2008;19(4):1350‐1367. [DOI] [PubMed] [Google Scholar]
- 25. Gresenz CR, Derose KP, Ruder T, Escarce JJ. Health care experiences of Hispanics in new and traditional U.S. destinations. Med Care Res Rev. 2012;69(6):663‐678. [DOI] [PubMed] [Google Scholar]
- 26. Agency for Healthcare Research and Quality Disparities in Healthcare Quality Among Racial and Ethnic Groups: Selected Findings from the 2011 National Healthcare Quality and Disparities Reports. Washington DC: Agency for Healthcare Research and Quality; September 2012. http://archive.ahrq.gov/research/findings/nhqrdr/nhqrdr11/minority.pdf. Accessed August 19, 2016. [Google Scholar]
- 27. Smith DL. Health care disparities for persons with limited English proficiency: relationships from the 2006 Medial Expenditure Panel Survey (MEPS). J Health Disparities Res Pract. 2009;3(3):57‐67. [Google Scholar]
- 28. Flores G, Abreu M, Tomany‐Korman SC. Limited English proficiency, primary language at home, and disparities in children's health care: how language barriers are measured matters. Public Health Rep. 2005;120(4):418‐430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Derose KP, Baker DW. Limited English proficiency and Latinos’ use of physician services. Med Care Res Rev. 2000;57(1):76‐91. [DOI] [PubMed] [Google Scholar]
- 30. Richards MR, Saloner B, Kenney GM, Rhodes K, Polsky D. Access points for the underserved: primary care appointment availability at federally qualified health centers in 10 states. Med Care. 2014;52(9):818‐825. [DOI] [PubMed] [Google Scholar]
- 31. Saloner B, Kenney GM, Polsky D, Rhodes K, Wissoker D, Zuckerman S. The Availability of New Patient Appointments for Primary Care at Federally Qualified Health Centers: Findings From an Audit Study. Washington, DC: Urban Institute; April 7, 2014. http://www.urban.org/sites/default/files/alfresco/publication-pdfs/413088-the-availability-of-new-patient-appointments-for-primary-care-at-federally-qualified-health-centers-findings-from-an-audit-study.pdf. Accessed August 19, 2016. [Google Scholar]
- 32. National Association of Community Health Centers America's Health Centers. Fact Sheet. Bethesda, MD: National Association of Community Health Centers; March 2016. http://nachc.org/wp-content/uploads/2015/06/Americas-Health-Centers-March-2016.pdf. Accessed July 22, 2015. [Google Scholar]
- 33. Cordasco KM, Ponce NA, Gatchell MS, Traudt B, Escarce JJ. English language proficiency and geographical proximity to a safety net clinic as a predictor of health care access. J Immigr Minor Health. 2011;13(2):260‐267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Gonzales G. State Estimates of Limited English Proficiency (LEP) by Health Insurance Status. Issue Brief 40. Minneapolis, MN: State Health Access Data Assistance Center, University of Minnesota; May 2014. http://www.rwjf.org/content/dam/farm/reports/issue_briefs/2014/rwjf414189. Accessed March 31, 2015. [Google Scholar]
- 35. Tavernise S, Gebeloff R. Immigrants, the poor and minorities gain sharply under Affordable Care Act. New York Times. April 17, 2016. http://www.nytimes.com/2016/04/18/health/immigrants-the-poor-and-minorities-gain-sharply-under-health-act.html?_r=0. Accessed August 19, 2016. [Google Scholar]
- 36. Wilson JH. Investing in English Skills: The Limited English Proficient Workforce in U.S. Metropolitan Areas. Washington, DC: Metropolitan Policy Program, Brookings Institution; September 2014. http://www.brookings.edu/~/media/Research/Files/Reports/2014/09/english-skills/Srvy_EnglishSkills_Sep22.pdf?la=en. Accessed April 10, 2016. [Google Scholar]
- 37. HR 3590 (111th) : Patient Protection and Affordable Care Act. GovTrack website. https://www.govtrack.us/congress/bills/111/hr3590. Updated March 22, 2010. Accessed November 8, 2015.
- 38. Joseph, TD. What health care reform means for immigrants: comparing the Affordable Care Act and Massachusetts health reforms. J Health Polit Policy Law. 2016;41(1):101‐116. [DOI] [PubMed] [Google Scholar]
- 39. Currier E, Key C, Biernacka‐Lievestro J, et al. The Precarious State of Family Balance Sheets. Philadelphia, PA: Pew Charitable Trusts; January 2015. http://www.pewtrusts.org/~/media/Assets/2015/01/FSM_Balance_Sheet_Report.pdf. Accessed March 31, 2015. [Google Scholar]
- 40. Pippins JR, Alegria M, Haas JS. Association between language proficiency and the quality of primary care among a national sample of insured Latinos. Med Care. 2007;45(11):1020‐1025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Hadler MW, Chen X, Gonzalez E, Roby DH. Limited English Proficient HMO Enrollees Remain Vulnerable to Communication Barriers Despite Language Assistance Regulations. Policy Brief. Los Angeles, CA: UCLA Center for Health Policy Research; February 2013. http://www.ncbi.nlm.nih.gov/pubmed/23550321. Accessed March 31, 2015. [PubMed] [Google Scholar]
- 42. Flores G. The impact of medical interpreter services on the quality of health care: a systematic review. Med Care Res Rev. 2005;62(3):255‐299. [DOI] [PubMed] [Google Scholar]
- 43. Karliner LS, Jacobs EA, Chen AH, Mutha S. Do professional interpreters improve clinical care for patients with limited English proficiency? A systematic review of the literature. Health Serv Res. 2007;42(2):727‐754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Office for Civil Rights . Guidance to Federal Financial Assistance Recipients Regarding Title VI Prohibition Against National Origin Discrimination Affecting Limited English Proficient Persons. Washington, DC: U.S. Department of Health & Human Services; October 4, 2006. http://www.hhs.gov/sites/default/files/ocr/civilrights/resources/specialtopics/lep/lepguidance.pdf. Accessed August 19, 2016. [Google Scholar]
- 45. Public Health Service Act . 42 USC §254b. 1944. https://www.law.cornell.edu/uscode/text/42/254b. Accessed March 31, 2015.
- 46. Health Resources and Services Administration . Health Center Data Uniform Data System. http://bphc.hrsa.gov/datareporting/. 2014. Accessed July 2013.
- 47. Census 2010. Pew Research Center Hispanic Trends website. http://www.pewhispanic.org/census-2010. Accessed September 15, 2014.
- 48. Johnson KM, Lichter DT. Natural increase: a new source of population growth in emerging Hispanic destinations in the United States. Popul Dev Rev. 2008;34(2):327‐346. [Google Scholar]
- 49. Kandel WA, Cromartie J. New Patterns of Hispanic Settlement in Rural America. Rural Development Research Report 99. Washington, DC: Economic Research Service, U.S. Department of Agriculture; May 2004. http://www.ers.usda.gov/publications/rdrr-rural-development-research-report/rdrr99.aspx. Updated May 27, 2012. Accessed August 27, 2015. [Google Scholar]
- 50. Polsky D, Richards M, Basseyn S, et al. Appointment availability after increases in Medicaid payments for primary care. N Eng J Med. 2015;372(6):537‐545. [DOI] [PubMed] [Google Scholar]
- 51. Cornachione E, Musemici MB, and Artiga S. Summary of HHS's Final Rule on Nondiscrimination in Health Programs and Activities. Kaiser Family Foundation website. http://kff.org/disparities-policy/issue-brief/summary-of-hhss-final-rule-on-nondiscrimination-in-health-programs-and-activities. Published July 14, 2016. Accessed August 19, 2016.
- 52. Betancourt JR, Green AR, and Carrillo JE. Cultural Competence in Health Care: Emerging Frameworks and Practical Approaches. Washington, DC: Commonwealth Fund; October 2002. http://www.commonwealthfund.org/usr_doc/betancourt_culturalcompetence_576.pdf. Accessed May 11, 2016. [Google Scholar]
- 53. Saloner B, Gresenz CR. Health care experiences of latino children in emerging and traditional destinations. Med Care. 2016;54(5):442‐448. [DOI] [PubMed] [Google Scholar]
- 54. Sanchez G, Nevares T, Schink W, Hayes‐Bautista D. Latino physicians in the United States, 1980–2010: A thirty‐year overview from the Censuses. Acad Med. 2015;90(7):906‐912. [DOI] [PubMed] [Google Scholar]


