Abstract
Context:
The level of awareness about osteoporosis in postmenopausal women who are the common sufferers.
Aims:
This study aims to evaluate the level of awareness in postmenopausal women using the Osteoporosis Health Belief Scale (OHBS).
Settings and Design:
Osteoporosis has emerged as a common health problem in geriatric population. A proactive role needs to be played for preventing its consequences. Before initiating any preventive measures, an evaluation of awareness level of the target population is necessary. The questionnaire-based study design was used for this study.
Subjects and Methods:
A questionnaire (OHBS)-based study in 100 postmenopausal women in Chandigarh was conducted. The bone mineral density (BMD) was measured in each case by dual energy X-ray absorptiometry. Height, weight, and body mass index (BMI) of the participants were noted.
Statistical Analysis Used:
Statistical analysis was conducted to evaluate any correlation between the various components of the OHBS and the BMD.
Results:
No statistically significant difference was noted in the seven component parameters of OHBS among the normal, osteopenic, and osteoporotic women suggesting that the health belief regarding susceptibility is not much different between the three groups of the study population. A statistically significant difference between the mean BMI of normal and osteoporotic population was noted.
Conclusions:
The results show that there is a great deficit in the awareness level of postmenopausal Indian women regarding osteoporosis. Most of the women were unaware of the condition and the means to prevent it. The study emphasizes that health care professionals have lot of ground to cover to decrease the incidence of osteoporosis and its associated health problem.
Key Words: Awareness, bone mineral density, dual energy X-ray absorptiometry, health belief, menopausal, osteoporosis
INTRODUCTION
Osteoporosis literally means “porous bones” and is characterized by a decreased mineral density of the bones. It is seen in aging population and is considered as a modern epidemic. Osteoporosis makes the bones weak and fragile, increasing the chances of them getting fractured even with trivial trauma. Such fractures may lead to pain, deformity, and disability.[1,2] The management of osteoporotic complications may consume a significant part of a nation's health-care resources in future as the number of geriatric patients is bound to increase with an increase in the average longevity. Osteoporosis renders significant morbidity among the geriatric population, especially in postmenopausal females. The basic requirement for managing any health disorder starts with the evaluation of the current awareness of the disorder among the target subjects residing in a region. The prevention and management of osteoporosis require understanding and commitment from the vulnerable population, i.e., postmenopausal women and elderly men. To assess the knowledge of osteoporosis among postmenopausal women in Chandigarh, we conducted the present study with a standard questionnaire-Osteoporosis Health Belief Scale (OHBS). Many methods of objective evaluation of bone mineral density (BMD) are available. The most widely used method is dual energy X-ray absorptiometry (DEXA) which is considered as the gold standard test[3] as it is cheap, easily available, and easy to use and provides a sufficiently accurate estimation of the BMD. In this study, we attempted to find out the relationship between various components of the OHBS which are indicators of awareness of osteoporosis in postmenopausal women and their BMD. By this, we attempted to assess whether there is any difference in the awareness level of women who had normal, osteopenic, or osteoporotic bone densities expecting to evaluate that women with normal densities may have better awareness than women with osteopenic or osteoporotic densities.
SUBJECTS AND METHODS
OHBS which was used in this study was developed by Kim et al.[4] on the basis of Rosenstock's Health Belief Model. It has two main subscales: Osteoporosis Health Belief Calcium Scale (OHBCS) and the Osteoporosis Health Belief Exercise Scale (OHBES). The OHBCS and OHBES have three parameters in common: Perceptions of osteoporosis regarding seriousness, susceptibility, and general health motivation. The parameters measuring the concepts of barriers and benefits are specific to calcium intake and exercise behavior and are different for both the subscales. There are 42 items in the scale as susceptibility (items 1–6), seriousness (items 7–12), benefits of exercises (items 13–18), benefits of calcium intake (items 19–24), barriers to exercise (items 25–30), barriers to calcium intake (items 31–36), and health motivation (items 37–42). Each item is rated using a 5 point Likert scale as 1 (strongly disagree), 2 (disagree), 3 (neutral), 4 (agree), and 5 (strongly agree). Test-retest reliability for the whole scale has been shown to be 0.90.[4]
The study was carried out among 100 postmenopausal women. The women included in the study were selected from localities of Chandigarh which is a union territory and capital city in the Northern India with multilingual and multicultural population, during public health check-up and awareness campaigns organized by our institution. Women who volunteered for the study were explained the questionnaire in their own vernacular language and the responses were recorded accordingly by trained health volunteers. As the questions were read out and explained, the problem with translation issues did not arise. Apart from the OHBS, other parameters such as the participants' height, weight, body mass index (BMI), dietary habits, and physical activity were recorded. All the participants underwent BMD assessment by DEXA using Hologic bone densitometer (SN86298, USA) installed in the Department of Radiodiagnosis of our institute. All the observations were recorded into an Excel spreadsheet. According to the “t” score of BMD assessment by DEXA, the patients were divided into three groups namely normal (t score ≥−1.0), osteopenic (t score between − 1.0 and − 2.5), and osteoporotic (t score ≤−2.5). The data so collected was analyzed using SPSS version 20 (IBM, USA).
OBSERVATIONS AND RESULTS
The average age of the 100 enrolled women was 47.6 years (38–64 years). The average BMI was 26.6 ± 3.48. Of the 100 women, 18 women had a “t” score of − 2.5 and below and were osteoporotic, 55 women had “t” score − 1 to − 2.5 and were osteopenic and 27 women had “t” score − 1 to 1 and were considered normal. The mean scores were 18.30, 18.58, and 18.17 for normal, osteopenic, and osteoporotic individuals respectively (P value was 0.804 using ANOVA). There was no statistically significant difference between the mean susceptibility scores of the three groups (normal, osteopenic, and osteoporotic). Using ANOVA, the “P” values for other parameters such as seriousness, benefits of exercise, benefits of calcium intake, barriers to exercise, barriers to calcium intake, and health motivation were 0.520, 0.293, 0.329, 0.760, 0.953, and 0.859 respectively and so were not statistically significant. The minimum and maximum scores for each group for different questions are shown in Table 1.
Table 1.
Maximum and minimum scores for each of the questions of the Osteoporosis Health Belief Scale questionnaire
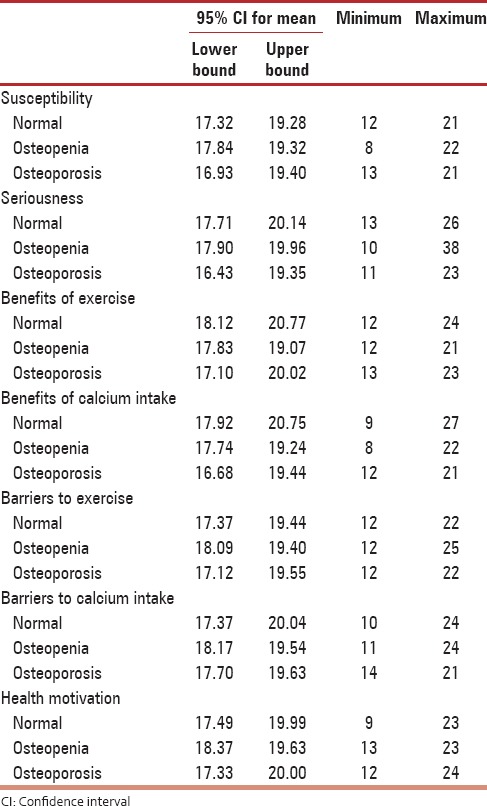
Pearson's correlation analysis was done, and the relation between the seven parameters was compared to each other, which was found to be significant. It can hence be inferred that the level of awareness regarding the component subsets of OHBS the same among the women, irrespective of the group they were classified into.
This was the same when spearman's rho analysis was used to analyze these variables.
Out of the 42 questions of the questionnaire, in only two questions the number of women answering as “agree” was high. In rest of the 40 questions, most of the responses were neutral. The two questions, “Regular exercise helps to build strong bones” (48% answered that they agreed) and “Exercising regularly makes you uncomfortable” (47% answered that they agreed) were contradictory to each other in terms of health belief, where one was benefit of exercise and the other was a barrier to exercise. One can infer that while the participants were aware that exercising was good for bones, most were reluctant to exercise.
The mean BMIs among the three groups were 28.2 ± 3.11, 26.2 ± 3.37, and 25.2 ± 3.65 for normal, osteopenic, and osteoporotic population [Figure 1]. On comparing this index using ANOVA, there was statistically significant difference between the mean BMI of the normal and osteoporotic population, whereas there was no statistically significant difference between normal and osteopenic women or osteopenic and osteoporotic population.
Figure 1.

Bar graph showing the means of body mass indices of the three study populations
DISCUSSION
With an increase in the life expectancy, the geriatric population of the developing countries like India is increasing and the impact of osteoporosis on the population and the nation is expected to increase.[5] Postmenopausal women, especially those with age more than 65 years are prone to develop complications of osteoporosis like fragility fractures.[6] Using effective bone sparing and bone formation promoting medications, osteoporosis can be managed effectively. Moreover, healthy lifestyle practices such as regular exercises and adequate calcium intake can promote the maintenance of BMD.[6,7] However, unfortunately, the majority of postmenopausal women who would actually benefit from such measures are not identified. Furthermore, the awareness on the part of such women with regards to osteoporosis and its management is considerably inadequate.[6,8] By being proactive orthopedic surgeons and allied health personnel can reduce the significant morbidity induced by hip and spine fractures among geriatric population.
For the Indian population, the exact figures on the prevalence of osteoporosis are not available, but the estimation is that more than 61 million Indians have osteoporosis with women accounting for 61% of them.[9,10] A previous study[11] attempted to determine the prevalence of osteoporosis in Indian women and reported that 106 of the studied 200 patients had low BMD (osteopenia and osteoporosis). The overall prevalence of osteoporosis has been reported to be higher in the Asian populations than their western counterparts.[12] This may be due to the racial factors and also to the fact that most of the Asian countries are less developed ones with the problems of poor nutritional status, frequent childbirth, poor socioeconomic status, poor educational levels among others contributing to low BMD and hence osteoporosis.[11] While detailed clinical practice guidelines on postmenopausal guidelines have been published by the Indian menopause society,[13] prevention of complications of postmenopausal osteoporosis cannot be done without the participation of the target population and hence an assessment of awareness of osteoporosis among postmenopausal women appears to be the logical first step in this process. A literature search failed to provide us with any study assessing the awareness among Indian population, and hence, we attempted to study the same in population in and around Chandigarh, India using a representative sample. Objective assessment of any condition or state needs a measurement tool and the OHBS developed in 1991 has been used in various studies as an effective tool for assessing osteoporosis awareness level. We did not face the problem of linguistic obstacles with OHBS as we had volunteers to translate the OHBS and note the responses in case the participating women were not aware of English.
The scores of all the seven parameters of OHBS was statistically not significantly among the normal, ostoepenic, and osteoporotic women, which means the health belief regarding susceptibility is not much different between the groups. In other words, the susceptible population actually lacks adequate knowledge about osteoporosis, and there is a strong need to educate them regarding the factors that predispose to osteoporosis. The osteoporotic population had comparatively lower seriousness than other two groups and almost equal mean scores in barriers to exercise, barriers to calcium intake and health motivation parameters of the OHBS in comparison to normal population [Figure 2].
Figure 2.
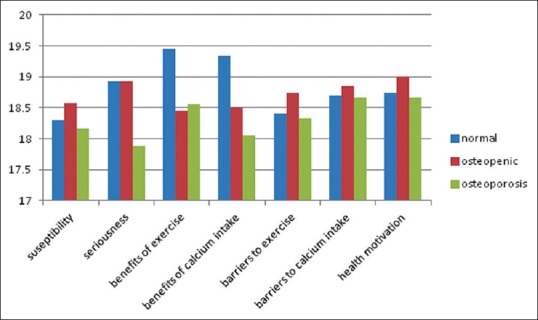
Bar graph showing means of seven parameters of Osteoporosis Health Belief Scale in three populations of this study
In a previous study by Gemalmaz and Oge,[14] they found that the women who reported having osteoporosis did not have a better knowledge than those who did not report having osteoporosis. In terms of seriousness, benefits of exercise and benefits of calcium intake, the scores were visibly lower in the osteoporotic group though all the seven parameters were not significantly different. Normal population group showed comparatively higher scores than other two groups in these two parameters only. Kim et al.[15] showed in their study that apart from barriers to exercise all other six parameters had no statistically significant difference among the three groups. The mean BMI of osteoporotic women was at borderline of the normal range in this study; signifying that underweight or lower BMI is a risk factor for osteoporosis. This is also supported by different studies.[16,17,18,19,20] Asomaning et al. stressed that the change in risk associated with a 1 unit change in BMI (approximately 5–8 lb) is of greater magnitude than most other modifiable risk factors.[21]
Load-bearing exercises are to be emphasized on because they have been shown to be more strongly associated with improvements in BMD when compared to non-weight-bearing exercises.[22]
Kasper et al.[23] showed that women's knowledge about adequate calcium intake and physical activity for prevention of osteoporosis did not influence their exercise or dietary behaviors. Marcus et al.[24] opined that even if most of the people know that physical activity is beneficial for health, a very few people actually participate in physical activity. Therefore, education programs should just not only be informative but very much participative and inclusive so that the women can practice the behaviors and include them in their daily routine.
Involving the population in spreading knowledge and arranging exercise workshops where actually they can learn the exercises would be a good step in the educational programs. Kasper et al.[23] found that women prefer handouts, brochures, magazine articles, and short 5-min counseling sessions during medical office visits. However, we think in a country like ours where women may have less interest in reading books or magazines, pictorial brochures or small drama or skit-based knowledge transmission would have a greater impact. Ailinger et al. noticed that community health nurses who distribute osteoporosis information would have a positive impact on knowledge. Educational programs or workshops should have some osteoporotic people so that vulnerable population can be motivated to have a healthy lifestyle. One can expect that exposure to a person with osteoporosis would either motivate an individual to learn more about the disease or increases one's understanding of the problem.
The overall goal of health education is to ensure that the population understands the risk factors and their own current health status and can simultaneously make an informed decision regarding their health behavior to prevent such diseases. For this, all these barriers and benefits of exercises and calcium intake need to be explained to these women. However, more research is required to find out the different ways and types of intervention that can alter and positively affect the health beliefs of the population at risk.
Every study has its own set of limitations and shortcomings. The present study was only focused on perimenopausal women. Including men in the study would provide a greater picture regarding health belief of the population.
Out of 42 items in OHBS, responses for forty questions were neutral which create ambiguity whether the person agrees or not and can affect the results accordingly. Therefore, this scale can omit neutral response for more concrete responses. The person should be asked to commit whether he/she agrees or not.
In developing country like India, there are people who are ignorant to terms such as calcium and its definition. Therefore, an average intelligence of the population should be measured before this questionnaire though this was just not possible in this study being it was a community public health check-up.
CONCLUSIONS
The results show that there is a great deficit in the awareness level of postmenopausal Indian women regarding osteoporosis. Most of the women were unaware of the condition and the means to prevent it. The study emphasizes that health care professionals have lot of ground to cover to decrease the incidence of osteoporosis and its associated health problem.
Financial support and sponsorship
The study was funded by Department of Science and Technology, Chandigarh.
Conflicts of interest
There are no conflicts of interest.
Acknowledgment
The authors would like to thank The Department of Science and Technology, Chandigarh for supporting the study by providing a fund and all the patients who provided their consent for their inclusion in this study. The authors also want to express their gratitude toward the volunteers who help noting the responses from patients.
REFERENCES
- 1.NIH Consensus Development Panel on Osteoporosis Prevention, Diagnosis, and Therapy. Osteoporosis prevention, diagnosis, and therapy. JAMA. 2001;285:785–95. doi: 10.1001/jama.285.6.785. [DOI] [PubMed] [Google Scholar]
- 2.World Health Organisation. Assessment of Fracture Risk and Its Application to Screening for Postmenopausal Osteoporosis. Geneva: WHO; 1994. [PubMed] [Google Scholar]
- 3.U.S. Preventive Services Task Force. Screening for osteoporosis in postmenopausal women: Recommendations and rationale. Ann Intern Med. 2002;137:526–8. doi: 10.7326/0003-4819-137-6-200209170-00014. [DOI] [PubMed] [Google Scholar]
- 4.Kim KK, Horan ML, Gendler P, Patel MK. Development and evaluation of the osteoporosis health belief scale. Res Nurs Health. 1991;14:155–63. doi: 10.1002/nur.4770140210. [DOI] [PubMed] [Google Scholar]
- 5.Riggs BL, Melton LJ., 3rd The worldwide problem of osteoporosis: Insights afforded by epidemiology. Bone. 1995;17(5 Suppl):505S–11S. doi: 10.1016/8756-3282(95)00258-4. [DOI] [PubMed] [Google Scholar]
- 6.Cadarette SM, Beaton DE, Hawker GA. Osteoporosis health belief scale: Minor changes were required after telephone administration among women. J Clin Epidemiol. 2004;57:154–66. doi: 10.1016/j.jclinepi.2003.08.005. [DOI] [PubMed] [Google Scholar]
- 7.Sambrook PN, Seeman E, Phillips SR, Ebeling PR. Osteoporosis Australia; National Prescribing Service. Preventing osteoporosis: Outcomes of the Australian fracture prevention summit. Med J Aust. 2002;176(8 Suppl):S1–16. doi: 10.5694/j.1326-5377.2002.tb04475.x. [DOI] [PubMed] [Google Scholar]
- 8.Jaglal SB, Carroll J, Hawker G, McIsaac WJ, Jaakkimainen L, Cadarette SM, et al. How are family physicians managing osteoporosis? Qualitative study of their experiences and educational needs. Can Fam Physician. 2003;49:462–8. [PMC free article] [PubMed] [Google Scholar]
- 9.Joshi VR, Mangat G, Balakrishnan C, Mittal G. Osteoporosis – Approach in Indian scenario. J Assoc Physicians India. 1998;46:965–7. [PubMed] [Google Scholar]
- 10.Rao H, Rao N, Sharma LR. A clinical study of bone mineral density using heel ultra-densitometer in Southern Maharashtra. Indian J Orthop. 2003;37:9. [Google Scholar]
- 11.Aggarwal N, Raveendran A, Khandelwal N, Sen RK, Thakur JS, Dhaliwal LK, et al. Prevalence and related risk factors of osteoporosis in peri- and postmenopausal Indian women. J Midlife Health. 2011;2:81–5. doi: 10.4103/0976-7800.92537. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Melton LJ., 3rd Epidemiology worldwide. (v).Endocrinol Metab Clin North Am. 2003;32:1–13. doi: 10.1016/s0889-8529(02)00061-0. [DOI] [PubMed] [Google Scholar]
- 13.Harinarayan CV, Marwah R, Sahay R, Kalra S, Babhulkar S. Clinical practice guidelines on postmenopausal osteoporosis: An executive summary and recommendations. Journal of Mid-Life Health. 2013;4:107–26. doi: 10.4103/0976-7800.115293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gemalmaz A, Oge A. Knowledge and awareness about osteoporosis and its related factors among rural Turkish women. Clin Rheumatol. 2008;27:723–8. doi: 10.1007/s10067-007-0777-9. [DOI] [PubMed] [Google Scholar]
- 15.Kim TH, Lee YS, Byun DW, Jang S, Jeon DS, Lee HH. Evaluation of the osteoporosis health belief scale in Korean women. J Bone Metab. 2013;20:25–30. doi: 10.11005/jbm.2013.20.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Iqbal SI, Mørch LS, Rosenzweig M, Dela F. The outcome of bone mineral density measurements on patients referred from general practice. J Clin Densitom. 2005;8:178–82. doi: 10.1385/jcd:8:2:178. [DOI] [PubMed] [Google Scholar]
- 17.Felson DT, Zhang Y, Hannan MT, Anderson JJ. Effects of weight and body mass index on bone mineral density in men and women: The Framingham study. J Bone Miner Res. 1993;8:567–73. doi: 10.1002/jbmr.5650080507. [DOI] [PubMed] [Google Scholar]
- 18.Nguyen TV, Center JR, Eisman JA. Osteoporosis in elderly men and women: Effects of dietary calcium, physical activity, and body mass index. J Bone Miner Res. 2000;15:322–31. doi: 10.1359/jbmr.2000.15.2.322. [DOI] [PubMed] [Google Scholar]
- 19.Baheiraei A, Pocock NA, Eisman JA, Nguyen ND, Nguyen TV. Bone mineral density, body mass index and cigarette smoking among Iranian women: Implications for prevention. BMC Musculoskelet Disord. 2005;6:34. doi: 10.1186/1471-2474-6-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Salamat MR, Salamat AH, Abedi I, Janghorbani M. Relationship between weight, body mass index, and bone mineral density in men referred for dual-energy x-ray absorptiometry scan in Isfahan, Iran. J Osteoporos. 2013;2013:205963. doi: 10.1155/2013/205963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Asomaning K, Bertone-Johnson ER, Nasca PC, Hooven F, Pekow PS. The association between body mass index and osteoporosis in patients referred for a bone mineral density examination. J Womens Health (Larchmt) 2006;15:1028–34. doi: 10.1089/jwh.2006.15.1028. [DOI] [PubMed] [Google Scholar]
- 22.Ulrich CM, Georgiou CC, Gillis DE, Snow CM. Lifetime physical activity is associated with bone mineral density in premenopausal women. J Womens Health. 1999;8:365–75. doi: 10.1089/jwh.1999.8.365. [DOI] [PubMed] [Google Scholar]
- 23.Kasper MJ, Peterson GE, Allegrante JP. The need for comprehensive educational osteoporosis prevention programs for young women: Results from a second osteoporosis prevention survey. Arthritis Care Res. 2001;45:28–34. doi: 10.1002/1529-0131(200102)45:1<28::AID-ANR80>3.0.CO;2-G. [DOI] [PubMed] [Google Scholar]
- 24.Marcus BH, Banspach SW, Lefebvre RC, Rossi JS, Carleton RA, Abrams DB. Using the stages of change model to increase the adoption of physical activity among community participants. Am J Health Promot. 1992;6:424–9. doi: 10.4278/0890-1171-6.6.424. [DOI] [PubMed] [Google Scholar]


