Abstract
Background
The contemporary characteristics and outcomes of cardiopulmonary resuscitation (CPR) in the neonatal intensive care unit (NICU) are poorly described. The objectives of this study were to determine the incidence, interventions, and outcomes of CPR in a quaternary referral NICU.
Methods
Retrospective observational study of infants who received chest compressions for resuscitation in the Children’s Hospital of Philadelphia NICU between April 1, 2011 and June 30, 2015. Patient, event, and survival characteristics were abstracted from the medical record and the hospital-wide resuscitation database. The primary outcome was survival to hospital discharge. Univariable and multivariable analyses were performed to identify patient and event factors associated with survival to discharge.
Results
There were 1.2 CPR events per 1,000 patient days. CPR was performed in 113 of 5,046 (2.2%) infants admitted to the NICU during the study period. The median duration of chest compressions was 2 minutes (interquartile range 1, 6 minutes). Adrenaline was administered in 34 (30%) CPR events. Of 113 infants with at least one CPR event, 69 (61%) survived to hospital discharge. Factors independently associated with decreased survival to hospital discharge were inotrope treatment prior to CPR (adjusted Odds Ratio [aOR] 0.14, 95% Confidence Interval [CI] 0.04, 0.54), and adrenaline administration during CPR (aOR 0.14, 95% CI 0.04, 0.50).
Conclusions
Although it was not uncommon, the incidence of CPR was low (<3%) among infants hospitalized in a quaternary referral NICU. Infants receiving inotropic therapy prior to CPR and adrenaline administration during CPR were less likely to survive to hospital discharge.
Keywords: newborn, cardiopulmonary resuscitation, cardiac arrest, chest compressions
Introduction
Little is known about the current practices and outcomes of cardiopulmonary resuscitation (CPR) in the neonatal intensive care unit (NICU). In historical studies, the reported incidence of CPR ranged from 1% to 6% of all infants admitted to the NICU,1–3 and was as high as 10% to 34% among extremely preterm infants.4–7 Between 49% to 100% of infants who received CPR in these studies died before hospital discharge, prompting some authors to question whether CPR in extremely preterm infants in the NICU is futile.4,6
However, many of these studies are over 15 years old and may not reflect current trends in CPR practice or outcomes in newborns. In addition, many of these early reports only included extremely preterm infants who received CPR in the first days after birth.2,5,6
With growing survival of extremely preterm newborns, complications of prematurity that require management at referral NICUs are increasing in prevalence.8 After surviving the initial neonatal periods with unstable fetal-neonatal transition and early neonatal cardiorespiratory disorders, these patients remain acutely ill throughout infancy and may suffer from acute cardiopulmonary instability requiring CPR. Characteristics and outcomes of CPR in the referral neonatal population are not well described. The objectives of this study were to determine the incidence, interventions, and outcomes of CPR events in a contemporary quaternary referral NICU.
Methods
Study design and population
This was a retrospective cohort study of all infants < 1 year of age who received CPR (defined as chest compressions for resuscitation) between April 1, 2011 and June 30, 2015 in the Children’s Hospital of Philadelphia (CHOP) NICU. This time period was selected because it encompasses the years when a hospital wide CPR database was in place. Delivery room CPR events were not captured in this database and were not evaluated in this analysis. The CHOP Institutional Review Board approved this study with a waiver of parental informed consent.
The CHOP NICU is a 96-bed level 4 referral NICU.9 The most common reasons for admission are surgery (38%), respiratory management (16%), neurologic problems (9%), and congenital anomalies (7%). Infants with complex congenital heart disease are not typically managed in the CHOP NICU in the immediate perioperative period but may be transferred to the NICU once their acute cardiac problems resolve. Approximately half of admitted infants are preterm (<37 weeks gestation); 14% have a gestational age < 29 weeks at birth, and 9% are of 29 to 33 weeks gestation at birth. At the time of admission, 42% of infants are greater than 2 weeks postnatal age. The baseline in-unit mortality is 5%.
All staff in the CHOP NICU are trained in the Neonatal Resuscitation Program (NRP) guidelines.10 CPR is initiated in infants with a heart rate <60 beats per minute after attempting to establish effective positive pressure ventilation. Chest compressions are performed with a backboard in place and are coordinated with ventilation in a 3:1 ratio.
Data Sources
Infants were identified from a hospital-wide resuscitation database that captures all acute events for which the NICU emergency (code) alarm is activated. Per unit policy, a dedicated staff member records pre-specified data in real time into a resuscitation record during the resuscitation event. Basic demographic, resuscitation, and outcome data are subsequently entered into the resuscitation database (Supplemental File). We independently confirmed all resuscitation events using the infant’s primary medical record and abstracted detailed information about the resuscitation from the resuscitation database. Additional pre-specified demographic, medication, and laboratory data was abstracted from the medical record. We used administrative data to determine the baseline number of NICU admissions and patient days during the study period.
Study Definitions and Outcomes
CPR was defined as any event for which chest compressions were performed. If an infant had more than one CPR resuscitation event during his/her hospital admission, only the first event was included in this analysis. CPR events were sub-classified as either acute respiratory compromise (ARC) preceding cardiopulmonary arrest (CPA), or CPA alone, according to American Heart Association definitions.11 Briefly, ARC is defined as activation of a unit-based emergency response for absent, agonal or inadequate respiration that requires emergency assisted ventilation. CPA is defined as a cardiopulmonary resuscitation event requiring chest compressions and/or defibrillation.
The duration of chest compressions, inclusive of pauses for pulse checks or other interventions, was abstracted from the resuscitation record and recorded in whole minutes. Medications administered during the resuscitation were abstracted from the resuscitation record. Medications given prior to CPR were classified as any medication administered during the 24 hours prior to the event, as documented in the electronic medical record. Continuous capnography monitoring of intubated patients is not routinely used in the CHOP NICU, and monitoring tools such as arterial line waveforms during CPR were not recorded in the database.
The primary study outcome was survival to hospital discharge. Secondary outcomes were return of circulation (ROC), defined as no further need for chest compression within 20 minutes of the event, and survival for >24 hours after CPR.
Data Analysis
Descriptive summary statistics were generated for the interventions performed during resuscitation and the baseline characteristics and outcomes of infants who received CPR. We examined the association between in-hospital mortality and the following covariates: gestational age, post-natal age at event, primary diagnosis, inotropes prior to CPR (as an indicator of hypotension), systemic antibiotics prior to CPR (as an indicator for proven or suspected sepsis), primary CPA event, duration of chest compressions, and administration of adrenaline (epinephrine) during CPR. These potential risk factors were a priori selected because they were reported to be associated with mortality in previous studies of neonates or older children or were hypothesized to be significant contributors to in-hospital mortality in our population. 5,12,13 We explored the associations between these covariates and the study outcomes using chi-square or Fisher’s exact tests for dichotomous variables and Wilcoxon rank sum tests for continuous variables. A p-value <0.05 was considered statistically significant.
We used stepwise backwards logistic regression to identify patient and resuscitation characteristics that were independently associated with survival to hospital discharge. Variables associated with the primary outcome at p<0.1 in univariate analysis were included in the initial model. We then sequentially removed each variable from the model, using the likelihood ratio test to identify the most parsimonious model. We analyzed the data using Stata 14.0 (Statacorp, College Station TX).
Results
Infant characteristics and CPR events
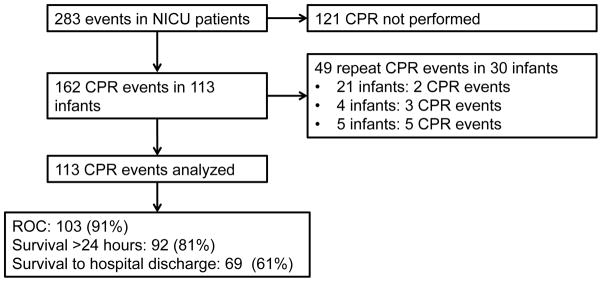
During the study period 5,046 infants were admitted to the CHOP NICU. There were 162 CPR events in 113 infants, representing 2.2% of infants admitted during the study period. Thirty infants had more than one CPR event (Figure 1). There were 1.2 CPR events per 1,000 patient days.
Figure 1.
Flow diagram of CPR events included in the analysis
Study infants had a median gestational age of 28 weeks, median birth weight of 950 grams, and median chronological age of 11 weeks at the time of the first CPR event (Table 1). Of 113 infants, 92 (81%) were receiving invasive mechanical ventilation at the time of the CPR event. Twenty-three infants (20%) were treated with inotropic support within 24 hours prior to CPR, and 63 (56%) received antibiotics for confirmed or suspected infection within 24 hours prior to the CPR event
Table 1.
Baseline infant characteristics.
| Characteristic | n (%), N=113 |
|---|---|
| Gestational age (weeks), median (IQR) | 28 (26,34) |
| Birth weight (grams), median (IQR) | 950 (650, 2215) |
| Male sex | 66 (58%) |
| Age at CPR event (weeks), median (IQR) | 11 (4, 19) |
| Inotropes prior to CPR | 23 (20%) |
| Antibiotics prior to CPR | 63 (56%) |
| Invasive mechanical ventilation prior to CPR | 92 (81%) |
| Primary Diagnosis | |
| Prematurity | 27 (24%) |
| Chronic lung disease | 25 (22%) |
| Major surgical anomaly* | 14 (12%) |
| Genetic anomaly/Syndrome/Minor congenital anomalies | 18 (16%) |
| Necrotizing enterocolitis | 10 (9%) |
| Respiratory Failure (not RDS) | 6 (5%) |
| Other | 13 (12%) |
Abbreviations: CPR: cardiopulmonary resuscitation, IQR: Intraquartile range, RDS: respiratory distress syndrome
surgical anomalies include congenital diaphragmatic hernia (4), esophageal atresia/fistula (3) omphalocele (4), gastroschisis (1), lung lesion (1), pentology of Cantrell (1)
CPR Characteristics
The majority (77%) of CPR events were classified as ARC to CPA (Table 2). Endotracheal intubation was performed in 50 (44%) infants during CPR. Among these 50 infants, 42 (84%) were mechanically ventilated immediately prior to CPR. The indication for the intubations that occurred during CPR (e.g., confirmed unplanned extubation or elective change of the endotracheal tube) was not consistently documented in the resuscitation records.
Table 2.
Interventions performed during cardiopulmonary resuscitation
| Characteristic | n (%), N=113 |
|---|---|
| Duration of Chest Compressions (minutes), median (IQR) | 2 (1, 6) |
| Type of Event | |
| Acute Respiratory Compromise to Cardiopulmonary Arrest | 87 (77%) |
| Primary Cardiopulmonary Arrest | 23 (20%) |
| Not classified | 3 (3%) |
| Medications administered* | |
| Adrenaline | 34 (30%) |
| Opiates (fentanyl, morphine) | 34 (30%) |
| Sodium bicarbonate | 20 (18%) |
| Atropine | 18 (16%) |
| Sodium chloride fluid bolus | 16 (14%) |
| Calcium gluconate | 16 (14%) |
| Neuromuscular blockade | 16 (14%) |
only medications administered to ≥5% of infants presented
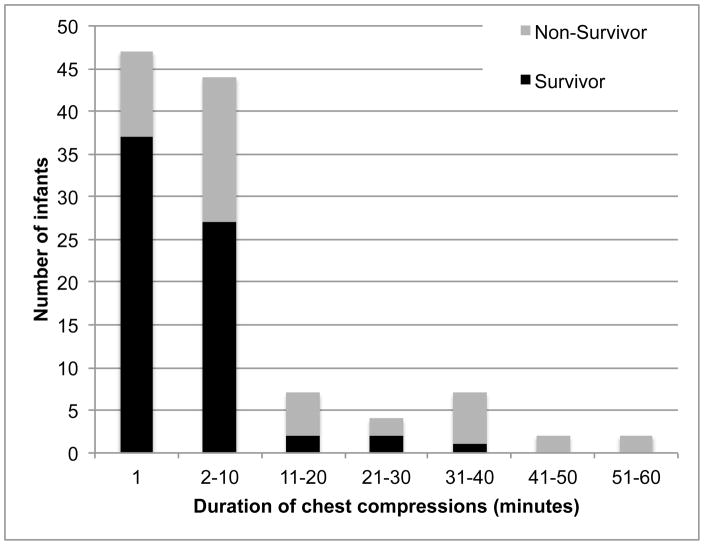
The median duration of chest compressions was 2 minutes (Interquartile range [IQR] 1–6 minutes). Chest compressions were performed for one minute or less in 47 (42%) events, and were performed for longer than 10 minutes in 22 (19%) CPR events (Figure 2).
Figure 2.
Distribution of duration of chest compressions (in minutes) during CPR, according to survival to hospital discharge.
Adrenaline was administered during 34 (30%) CPR events, with a median of 3 doses (IQR 2, 4 doses). The most common other medications administered during resuscitation were opiates (30%), sodium bicarbonate (18%), and atropine (16%) (Table 2).
Outcomes
Among 113 infants who received CPR in this study, 69 (61%) survived to hospital discharge (Figure 1). ROC was achieved in 103 (91%) infants, and 92 (81%) infants survived for at least 24 hours after CPR.
In univariable analysis, infants who survived to discharge had a lower median gestational age at birth (28 weeks vs. 30 weeks, p=0.037) and were less likely to have a primary CPA event (6% vs. 43%, p<0.001). In addition, infants who survived to discharge were less often treated with inotropes (7% vs. 41%, p<0.001) and antibiotics (48% vs. 68%, p=0.034) during the 24 hours prior to CPR. The primary diagnosis was not associated with survival to discharge
The CPR characteristics associated with survival to discharge were duration of chest compressions (median 1 minute [IQR 1, 4 minutes] for survivors vs. 5 minutes [IQR 2, 24 minutes] for non-survivors, p<0.001) and adrenaline administration during CPR (10% survivors vs. 61% non-survivors, p<0.001) (Table 3). The proportion of infants who survived at least 24 hours after CPR event and subsequently had another CPR event did not significantly differ between survivors (39%) and non-survivors (29%) (p=0.36).
Table 3.
Univariable analysis of infant and resuscitation characteristics associated with survival to hospital discharge
| Characteristic | Survivors (n=69) | Non- survivors (n=44) | p value |
|---|---|---|---|
| Gestational age (weeks), median (IQR) | 28 (25, 32) | 30 (26, 37) | 0.037 |
| Age at event (weeks), median (IQR) | 13 (7, 19) | 7 (3, 16) | 0.051 |
| Inotropes prior to CPR | 5 (7%) | 18 (41%) | <0.001 |
| Antibiotics prior to CPR | 33 (48%) | 30 (68%) | 0.034 |
| Invasive ventilation prior to CPR | 58 (84%) | 34 (77%) | 0.37 |
| Primary CPA event* | 4 (6%) | 19 (43%) | <0.001 |
| Duration of chest compressions (minutes), median (IQR) | 1 (1, 4) | 5 (2, 24) | 0.0001 |
| Adrenaline administered | 7 (10%) | 27 (61%) | <0.001 |
| Primary Diagnosis | 0.29 | ||
| Prematurity | 19 (28%) | 8 (18%) | |
| Chronic lung disease | 18 (26%) | 7 (16%) | |
| Major surgical anomaly* | 7 (10%) | 7 (16%) | |
| Genetic anomaly/Syndrome/Minor congenital anomalies | 11 (16%) | 7 (16%) | |
| Necrotizing enterocolitis | 3 (4%) | 7 (16%) | |
| Respiratory Failure (not RDS) | 3 (4%) | 3 (7%) | |
| Other | 8 (12%) | 5 (11%) | |
calculated with Fisher’s exact test
The final multivariable model included the following covariates: gestational age, post-natal age, inotrope treatment prior to CPR, primary CPA, and adrenaline administration during CPR. Factors that were independently associated with decreased survival to hospital discharge were inotrope treatment prior to CPR (adjusted Odds Ratio [aOR] 0.14, 95% Confidence Interval [CI] 0.04, 0.54), and adrenaline administration during CPR (aOR 0.14, 95% CI 0.04, 0.50).
Discussion
We conducted the present study to describe the incidence, characteristics, and outcomes of CPR in a contemporary, quaternary referral NICU. CPR was performed in 2.2% of infants. Most CPR events started as an acute respiratory compromise that progressed to cardiopulmonary arrest. Most events were also brief. Chest compressions were performed for ≤10 minutes in 81% of CPR events. Sixty-one percent of infants receiving CPR survived to hospital discharge. Factors that were independently associated with decreased survival to discharge were treatment with inotropes prior to CPR and adrenaline administration during CPR.
The incidence of CPR in the present study was lower than described in several previous studies.5,6 However, many prior reports focused on extremely preterm infants who received CPR early in life.4–6 Our population consists largely of former extremely preterm infants who continue require hospitalization due to complex medical needs as well as full term infants with congenital anomalies. The incidence of CPR in our unit was comparable to that reported by Barr and colleagues,3 who found that CPR was performed in 1% of infants admitted to a referral NICU that provides care for diverse medical and surgical diagnoses. This result is also similar to reports from pediatric intensive care units, where 1–2% of admitted patients receive CPR.14,15
The proportion of infants who survived to discharge was higher in our cohort than previous neonatal studies 2,4–6 Similar to the lower incidence of CPR, this finding may also reflect inherent differences in the baseline characteristics of the study populations. The infants we described were generally older at the time of CPR and had more diverse underlying conditions than infants found in many previous studies. There may also be an inherent selection bias in our cohort as some critically ill infants likely died prior to desired transport to our center
Most of the CPR events in this study progressed from an initial acute respiratory compromise. Neonates and infants are especially susceptible to CPA following acute respiratory decompensation.16 Continuous capnography monitoring in NICU patients permits identification of elevated CO2 levels, 17 and capnography permits rapid identification of endotracheal tube dislodgement in intubated patients.18 Enhanced respiratory monitoring with continuous capnography may therefore help providers recognize and prevent ARC, averting some cases of CPA in the NICU.
Consistent with previous studies, 2,5 inotropic therapy prior to CPR was independently associated with decreased survival, suggesting that antecedent cardiovascular compromise portends a poor outcome. In addition, we found that adrenaline administration during CPR was associated with decreased survival. Strategies to improve survival in infants with these characteristics are needed. Moreover, interventions that improve CPR performance, such as real-time feedback during CPR and interdisciplinary team debriefings after CPR, have been shown to improve the quality and outcomes of CPR in the pediatric intensive care setting.19,20 These interventions merit further investigation to improve CPR in the NICU.
We acknowledge study limitations. The CHOP NICU is a referral setting, and study results may not generalize to an inborn NICU population. Reliable information about the cardiac rhythm immediately before or during CPR was not recorded. Infants who received CPR were not consistently seen in the CHOP follow-up program, preventing assessment of neurodevelopmental outcomes in survivors.
Study strengths include the analysis of data that were recorded in real-time during resuscitation events. In addition, we were able to characterize the incidence of CPR in our population, which is not possible using CPR registries.
Conclusions
Although it was not uncommon, the incidence of CPR was low (<3%) among infants hospitalized in a quaternary referral NICU. Most CPR events progressed from acute respiratory compromise. Survival following CPR in the present study was higher than in prior reports of extremely preterm infants. Among this referral population, inotropic therapy prior to CPR and adrenaline administration during CPR were associated with decreased survival to hospital discharge. Future studies in the tertiary neonatal population should focus on methods to improve outcomes in infants with these risk factors.
Supplementary Material
Acknowledgments
Dr. Foglia is supported by a NIH Career Development Award, 1K23HD084727-01A1. No study sponsors were involved in the study design, data analysis and interpretation, or decision to submit this manuscript for publication. We would like to thank our colleagues who maintain the CHOP resuscitation database.
Footnotes
Conflicts of Interest
The authors have no conflicts of interest to disclose.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Chamnanvanakij S, Perlman JM. Outcome following cardiopulmonary resuscitation in the neonate requiring ventilatory assistance. Resuscitation. 2000;45:173–80. doi: 10.1016/s0300-9572(00)00184-2. [DOI] [PubMed] [Google Scholar]
- 2.Willett LD, Nelson RM. Outcome of cardiopulmonary resuscitation in the neonatal intensive care unit. Crit Care Med. 1986;14:773–6. doi: 10.1097/00003246-198609000-00003. [DOI] [PubMed] [Google Scholar]
- 3.Barr P, Courtman SP. Cardiopulmonary resuscitation in the newborn intensive care unit. J Paediatr Child Health. 1998;34:503–7. doi: 10.1046/j.1440-1754.1998.00294.x. [DOI] [PubMed] [Google Scholar]
- 4.Campbell ME, Byrne PJ. Cardiopulmonary resuscitation and epinephrine infusion in extremely low birth weight infants in the neonatal intensive care unit. J Perinatol. 2004;24:691–5. doi: 10.1038/sj.jp.7211174. [DOI] [PubMed] [Google Scholar]
- 5.Sood S, Giacoia GP. Cardiopulmonary resuscitation in very low birthweight infants. Am J Perinatol. 1992;9:130–3. doi: 10.1055/s-2007-994686. [DOI] [PubMed] [Google Scholar]
- 6.Lantos JD, Miles SH, Silverstein MD, Stocking CB. Survival after cardiopulmonary resuscitation in babies of very low birth weight. Is CPR futile therapy? N Engl J Med. 1988;318:91–5. doi: 10.1056/NEJM198801143180206. [DOI] [PubMed] [Google Scholar]
- 7.Kostelanetz AS, Dhanireddy R. Survival of the very-low-birth-weight infants after cardiopulmonary resuscitation in neonatal intensive care unit. J Perinatol. 2004;24:279–83. doi: 10.1038/sj.jp.7211054. [DOI] [PubMed] [Google Scholar]
- 8.Murthy K, Dykes FD, Padula MA, et al. The Children’s Hospitals Neonatal Database: an overview of patient complexity, outcomes and variation in care. J Perinatol. 2014;34:582–6. doi: 10.1038/jp.2014.26. [DOI] [PubMed] [Google Scholar]
- 9.American Academy of Pediatrics Committee on Fetus And Newborn. Levels of neonatal care. Pediatrics. 2012;130:587–97. doi: 10.1542/peds.2012-1999. [DOI] [PubMed] [Google Scholar]
- 10.Wyckoff MH, Aziz K, Escobedo MB, et al. Part 13: Neonatal Resuscitation: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation. 2015;132:S543–60. doi: 10.1161/CIR.0000000000000267. [DOI] [PubMed] [Google Scholar]
- 11.Get With the Guidelines- Resuscitation. American Heart Association; [Accessed 23 June 2016]. at www.heart.org/resuscitation. [Google Scholar]
- 12.Del Castillo J, López-Herce J, Cañadas S, et al. Cardiac arrest and resuscitation in the pediatric intensive care unit: a prospective multicenter multinational study. Resuscitation. 2014;85:1380–6. doi: 10.1016/j.resuscitation.2014.06.024. [DOI] [PubMed] [Google Scholar]
- 13.Meaney PA, Nadkarni VM, Cook EF, et al. Higher survival rates among younger patients after pediatric intensive care unit cardiac arrests. Pediatrics. 2006;118:2424–33. doi: 10.1542/peds.2006-1724. [DOI] [PubMed] [Google Scholar]
- 14.Berg RA, Nadkarni VM, Clark AE, et al. Incidence and Outcomes of Cardiopulmonary Resuscitation in PICUs. Crit Care Med. 2016;44:798–808. doi: 10.1097/CCM.0000000000001484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.de Mos N, van Litsenburg RRL, McCrindle B, et al. Pediatric in-intensive-care-unit cardiac arrest: incidence, survival, and predictive factors. Crit Care Med. 2006;34:1209–15. doi: 10.1097/01.CCM.0000208440.66756.C2. [DOI] [PubMed] [Google Scholar]
- 16.Klugman D, Berger JT, Spaeder MC, Wright A, Pastor W, Stockwell DC. Intensive Care Med. Intensive Care Med. 2013;39:1333–4. doi: 10.1007/s00134-013-2932-x. [DOI] [PubMed] [Google Scholar]
- 17.Kugelman A, Golan A, Riskin A, et al. Impact of Continuous Capnography in Ventilated Neonates: A Randomized, Multicenter Study. J Pediatr. 2016;168:56–61. doi: 10.1016/j.jpeds.2015.09.051. [DOI] [PubMed] [Google Scholar]
- 18.Cheifetz IM, Myers TR. Respiratory therapies in the critical care setting. Should every mechanically ventilated patient be monitored with capnography from intubation to extubation? Respir Care. 2007;52:423–38. [PubMed] [Google Scholar]
- 19.Sutton RM, Niles D, French B, et al. First quantitative analysis of cardiopulmonary resuscitation quality during in-hospital cardiac arrests of young children. Resuscitation. 2014;85:70–4. doi: 10.1016/j.resuscitation.2013.08.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Wolfe H, Zebuhr C, Topjian AA, et al. Interdisciplinary ICU cardiac arrest debriefing improves survival outcomes. Crit Care Med. 2014;42:1688–95. doi: 10.1097/CCM.0000000000000327. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.