Abstract
A move towards self-management is central to health strategy around chronic low back pain, but its concept and meaning for those involved are poorly understood. In the reported study, four distinct and shared viewpoints on self-management were identified among people with pain and healthcare providers using Q methodology. Each construes self-management in a distinctive manner and articulates a different vision of change. Identification of similarities and differences among the viewpoints holds potential for enhancing communication between patients and healthcare providers and for better understanding the complexities of self-management in practice.
Keywords: chronic illness, communication, critical health psychology, healthcare, health psychology, meaning, pain, pain acceptance, perception, qualitative methods
Introduction
Chronic low back pain (CLBP) is highly prevalent and costly in terms of personal impacts, disability, work-loss and healthcare expenditure (Hoy et al., 2010; Johannes et al., 2010). In the United Kingdom (Department of Health (DoH), 2001, 2005; Savigny et al., 2009) and internationally (Airaksinen et al., 2006; Institute of Medicine of the National Academics, 2011; Koes et al., 2010), there has been a move towards encouraging self-management as a strategy for reducing these impacts. The broad context to this strategy is the transition to an older population characterised by long-term health problems in a climate of rising healthcare costs and limited state funding (Bury et al., 2005; Dagenais et al., 2008; Freburger et al., 2009). This context has occasioned a shift from a ‘medical model’ towards the ‘empowerment’ of service users to control their own ways of living with illness (DoH, 2006, 2011; Glasgow et al., 2008). It is frequently observed among social scientists that the shift towards self-management is part of a socio-political context in which the balance of responsibility for health has shifted from the state to the individual (Clarke and Bennett, 2013).
A number of generic (Kennedy et al., 2007) and disease-specific (Lamb et al., 2010; Lorig, 2003; Van Hooff et al., 2012) self-management programmes have been developed to improve quality of life and independence for people with long-term conditions, and there is a trend towards online support and other digital resources. Healthcare providers are encouraged to support patients towards pro-active coping strategies and independent self-care. However, consistent patient engagement and achievement of effective self-management remains a challenge (De Silva, 2011; Rogers et al., 2008). Outcomes of interventions directed towards self-management can be disappointing (Du et al., 2011; Henschke et al., 2010; Oliveira et al., 2012; Williams et al., 2012), and degrees of engagement and confidence in self-management can vary considerably (Audulv, 2013; Carnes et al., 2012; Hibbard et al., 2007; Zufferey and Schulz, 2009).
Despite its strategic importance, there has been little research into the concept and meaning of self-management or how it is best achieved and supported in people with CLBP. Various obstacles to self-management have been identified, including patient and healthcare provider resistance, poor access to information and services and lack of knowledge among healthcare providers (Briggs et al., 2012; Corbett et al., 2009; Lawn et al., 2009). However, a more fundamental obstacle to effective implementation is the existence of divergent viewpoints on the nature and meaning of effective self-management on the part of different stakeholders (Cooper et al., 2009; Crowe et al., 2010; Kawi, 2014; Miles et al., 2011; Oliveira et al., 2012; Ong et al., 2014; Trappenburg et al., 2013). There is reason to expect divergent viewpoints on self-management related to different understandings and explanations of the nature, causes and consequences of CLBP (McParland et al., 2011; Risdon et al., 2003). In particular, if patients’ viewpoints do not correspond with those of healthcare providers (Busby et al., 1997; Eccleston et al., 1997), then this can compromise practices of self-management that expect people with pain to apply professional advice to the particularities of their own cases (Martin et al., 2014). Kenny (2004) writes in this context of a ‘communication chasm’, suggesting that medical explanations that invoke the psychological dimension can prove controversial with patients (Corbett et al., 2009; Peters et al., 1998; Toye and Barker, 2012). This study thus systematically explores the range of viewpoints on self-management held among stakeholders in CLBP care to inform service developments and enable more effective self-management for people with pain.
Method
Q methodology
Q methodology is a mixed-methods approach designed to explore the subjective dimension of any issue towards which different viewpoints can be expressed (Stenner and Stainton Rogers, 2004). It has a long tradition of successful applications in the field of health studies (Farrimond et al., 2010; Stainton Rogers, 1991; Stenner et al., 2003), and has been used to gain valuable insights in the study of chronic pain (Campbell, 2009; McParland et al., 2011; Risdon et al., 2003). Exploring viewpoints on self-management in CLBP from the perspectives of both people with pain and healthcare providers requires an appropriate methodology designed to detect differences of viewpoint while affording scope for their rigorous comparison. Q methodology permits participants to express their own viewpoint in a structured way as a ‘Q sort’ (Stenner et al., 2008). A Q sort is a collection of items (usually a set of statements of opinion) which are sorted by a participant according to a subjective dimension such as ‘agreement/disagreement’.
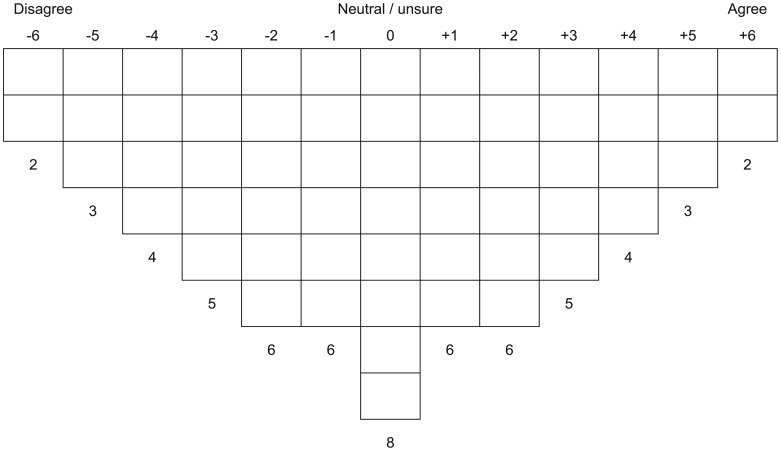
Each Q sort provides the researcher with a model of each participant’s viewpoint (see Figure 1), and the resulting numerical data can be analysed quantitatively to find patterns among the viewpoints. A by-person correlation and pattern analysis (typically factor analysis or principal component analysis) of the collected Q sorts enables the statistical identification of any shared viewpoints among the sample (Watts and Stenner, 2012). The result of a Q analysis is a set of factors each of which identifies a cluster of Q sorts which have been sorted in essentially the same way. A qualitative exegesis of the quantitative results yields an interpretation of the shared viewpoint which informs the distinctive way of Q sorting captured by each factor.
Figure 1.
The Q sort response grid.
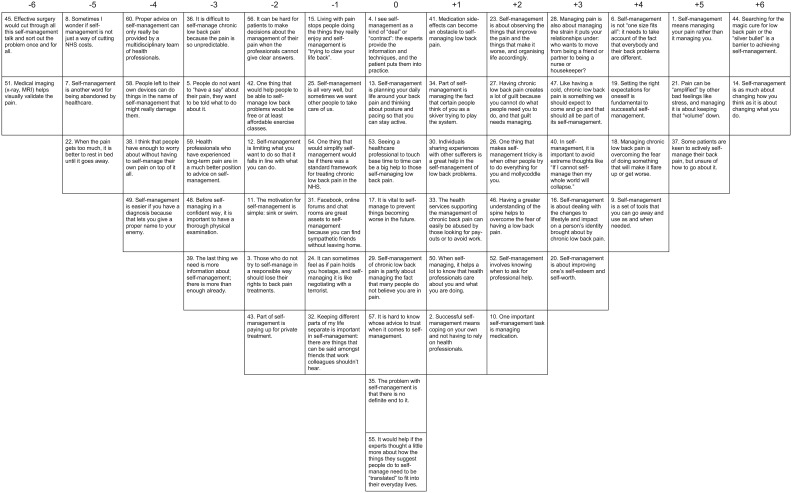
Generating the Q set
The first phase of Q methodology is the development of the items composing the Q set (the set of statements of opinion to be given to participants for Q sorting). The Q set items are statements which express the range of opinions, propositions and positions that are encountered in discussion around self-management of CLBP. To generate these statements, three sources were examined: (1) a review of relevant literature, (2) a series of discussions held by the project steering group (composed of researchers, clinicians and service user representatives) and (3) the analysis of seven focus groups run with people with varying levels of pain (as determined by Von Korff et al.’s (1992) chronic pain grade) and healthcare providers in the south east of England (including representatives from physiotherapy, clinical psychology, pain consultancy, general practice, orthopaedics, rheumatology, occupational health and practice management in primary, secondary and third sector care services). From these sources, 372 initial statements were generated and then divided into 10 themes, each containing several emergent categories. From these, a Q set of 60 statements was selected for piloting through a process of removing duplicates, synonyms and otherwise overlapping propositions, and – where redundancy of items within categories existed – selecting the most representative items while maintaining diversity and balance. The service user representatives on our steering group played an active role in selecting and refining the final item set. The pilot study involved steering group members, professional contacts and several participants from the focus groups. The final item set is shown in Figure 2.
Figure 2.
Factor array for factor 1.
Participant recruitment
Ethical approval was gained from the National Health Service (NHS) and host University Research Ethics Committees. People with pain and healthcare providers were recruited using emails and flyers targeted at relevant local healthcare services and providers in the south east of England. An invitation leaflet outlining the study and contact details were given to people meeting the inclusion criteria and considered to have an interest. Information sheets were provided as well as a verbal explanation of the study. Prior to obtaining written consent, participants were provided with information sheets, reassured that they could withdraw at any time and that data would be anonymous.
A total of 120 completed Q sorts were returned: 60 from patients with CLBP (age range from 23 to 81 years, of which 37 were female) and 60 from healthcare providers involved in managing individuals with CLBP (age range from 26 to 75 years, of which 39 were female, and several healthcare providers also had personal experience with CLBP).
Procedure
Participants received a Q sort pack by post or in person, including (1) a biographical questionnaire collecting socio-demographic data and information about CLBP care experience (to be completed first), (2) a complete set of instructions, (3) the 60-item Q set on numbered laminated cards, (4) a Q sort response grid sheet and (5) an open-ended response booklet inviting written comments on relevant items and sorting decisions. Each participant initially grouped the items into ‘agree’, ‘neutral/don’t know’ and ‘disagree’ piles. Participants then sorted these piles in a more fine-grained agree/disagree continuum according to the scale and matrix at the top of the response grid shown in Figure 1.
Participants were encouraged to adjust their Q sort until it felt representative of their viewpoint. Once completed, the item numbers were recorded in the appropriate boxes of the response grid shown as Figure 1. Participants were then asked to provide open-ended comments to explain the rationale of their sort, giving particular attention to items that best defined their own position. The Q sort process lasted approximately 60 minutes.
Results
Analysis
The 120 completed Q sorts were entered into SPSS (Version 20.0, IBM Corp., Armonk, NY) for statistical analysis using principal component analysis and varimax rotation with Kaiser normalisation. In a Q analysis, the loading of each Q sort on each extracted factor is expressed as a correlation with that factor. In a four-factor solution, all but three of the 120 Q sorts loaded significantly (at the p = 0.01 level) onto one of the four factors. This four-factor solution was accepted because (1) each factor had at least two ‘factor exemplar’ Q sorts loading significantly on it alone, (2) it satisfied the Kaiser–Guttman criterion which states that all extracted factors should have an eigenvalue greater than unity (λ > 1) (Brown, 1981; Guttman, 1954) and (3) each factor offered a clear, distinct and theoretically meaningful viewpoint on self-management (see below). For more details on criteria for factor solutions in Q methodology, (Watts and Stenner (2012).
In all, 74 Q sorts significantly loaded the first factor (which had an eigenvalue of 29.82 explaining 24.86% of the study variance), 21 ‘exemplars’ loaded the second (with an eigenvalue of 12.66 explaining 10.55% of the variance), 14 loaded the third (eigenvalue 11.13/9.27% of study variance), while the fourth factor had 8 significantly loading exemplars (eigenvalue 7.51/6.26% of study variance). To simplify interpretation, a single ‘factor exemplifying’ Q sort (known as a ‘factor array’) was created for each factor using the factor scores for each item (Watts and Stenner XXX, 2012). Each of the four factor arrays resembles a Q sort completed by a participant, but is in fact a ‘best estimate’ of the factor derived from data from all the Q sorts conforming to its pattern (Figure 2 shows the factor array for the first factor, others are available on request from the first author (P.S.)).
Factor interpretations
Interpretations of the factors draw upon all the ranking positions in the factor array and also on the open-ended comments from exemplar participants collected post-Q sort. In the interpretations below, these comments are indicated, where relevant, in italics, with P indicating a person with pain and HP a healthcare provider. Where the ranking position of an item is important to a section of interpretation, the relevant item is noted in brackets; hence (14: +6) would indicate that item 14 was ranked in the +6 position in the relevant factor array. Since there were no obvious associations between factor loadings and other data collected (such as employment status, chronic pain grade, duration of CLBP or disability status), these data will not be further discussed. The summaries below are condensed versions of full interpretations each of which was checked by a factor exemplar participant (who confirmed that the summary expresses a faithful version of their viewpoint).
Factor 1 summary: ‘I can change’ – a personal evolution
A total of 21 people with pain (12 females, age range 24–76) and 53 healthcare providers (33 females, age range 26–75) loaded onto the first factor. With 74 exemplars including 88 per cent of the service providers, this is very much the normative viewpoint. The main feature of this viewpoint was the idea that successful self-management of CLBP involves a significant change of ‘mind-set’ (14: +6). This change is a personal evolution: attitude is key. You have to get yourself out of the old mind-set (HP08); thinking affects what we do: it’s fundamental (HP14); the mainstay of treatment – I see this as absolutely vital (HP25); a positive attitude is crucial for motivation (P10); the only way to successfully self-manage is to address negative thoughts (P27); really important; power of the mind is great, so need a positive attitude to have most positive results (P28).
A changed mind-set equips individuals to live an active life with their pain (1: +5). Their way of thinking influences what people with pain do and how they feel, and so to move forward with self-management it is vital to adopt a positive, accepting and mindful attitude. This typically means a change of attitude, since many people find themselves ‘stuck’ in a mind-set which can make self-management difficult (16: +3): as self-management is about changing your thinking, searching for a magic bullet is simply tethering yourself to your old thinking (HP08). Pain, for example, can easily lead to negative thinking (40: +3). This in turn can lead to feelings of stress and anxiety which can actually make the pain worse (21: +5). Likewise, dwelling on worries and fears can make managing the pain more difficult (18: +4). Wishful thinking can also be a problem. For example, people in pain often quite understandably hope that a simple cure is waiting around the corner. They may devote their energies to a search for a magic bullet which may in fact never appear, and in this way, they can become ‘stuck’ in a waiting game, unable to go forward (44: +6): one of the first steps towards successful self-management is to accept there’s no magic cure (HP07).
In cases where a physical cure is unlikely, it is important to accept this and to learn to make the changes that are necessary to cope with CLBP, and to live with it (45: −6): The magic cure may not exist. ‘Looking at it’ may be ok, but not putting your life on hold until you found it (HP12). Managing pain is therefore much more than a medical matter (51: −6). It is about people understanding and managing their feelings and reactions to a life lived with pain, including the ways in which pain may influence relationships, the ability to work, ways of moving, self-esteem and sense of identity (20: +3, 28: +3): the interference of stress and other aspects of mental health (e.g. depression or anxiety) should not be underestimated! Practice of mindfulness meditation has the potential to be extremely beneficial! (HP06); depression and anxiety can exacerbate pain (HP10); stress can cause more pain and sleeplessness which in turn causes muscle to tighten (P18); stress can cause pain: mostly common in back, neck and shoulder (P19); yes. Fear is a huge barrier. With extensive education, reassurance, appropriate treatment the patient is no longer fearful of their CLBP. They can move forward (HP07).
Having the right mind-set will aid this process, and will allow individuals to stay in control of their pain rather than allowing the pain to control them: this to me is the key to self-management. Achieving function and goals despite of the pain (HP48); this is how I describe pain management programmes to the patients I refer to the course (HP58); I think this is vitally important. If you let pain get a grip over you it is very difficult to overcome (HP55); pain can take on its own identity which challenges your identity (HP08); you have to believe you can manage it!! And refuse to let it run your life (P03); it’s important to take control and do what you can do (P10); agree with this, about taking some control back in your life (P28); easier said than done but this is fundamentally what it is about (P27). Healthcare providers, for their part, can advise on tools and techniques which aid this process, helping to tailor advice and treatment to individual needs (6: +4). Good self-management is about professionals helping patients to regain control of their lives by changing their lives to cope better with their pain (19: +4, 9: +4).
Factor 2 summary: ‘Some things can change’ – practical action guided by accurate information
The Q sorts of 17 people with pain (10 females, age range 23–81) as well as 4 healthcare providers (3 females, age range 46–65) defined the second viewpoint in that they loaded significantly upon the second factor. Self-management of CLBP was perceived to require a pragmatic approach: know what works, what hinders, what hurts like hell! (P07); simple but true (P15). By carefully observing what works and what doesn’t (23: +6), the patient’s life can be organised to maximise their capabilities and minimise future flare-ups (12: +5). People with pain want to plan and organise their lives in accordance with their pain tolerance so that they can get on with their lives (17: +5, 15: +3). Staying active enables them to ‘claw back their lives’: Pain can worsen due to stiffness caused by inactivity and too much rest. We were designed to move and you have to keep the spine supple through gentle movement (P48). In order to successfully manage the pain, people need a good partnership with healthcare providers and it is helpful to receive a thorough physical examination and credible information (48: +5, 51: +4). Having a thorough physical examination, for instance, can be reassuring: you never know what would be behind the symptom (P12) and medical imaging can add confidence to diagnosis and so adds confidence to patient [sic] (P08). Good information and professional advice is vital because ill-informed self-management might be harmful (58: +3, 39: −5). That way, the person with pain can go away with confidence and put the healthcare providers’ advice into practice (4: +4). According to this problem-based perspective, the core of CLBP self-management lies in a well-informed understanding of the practicalities of staying active (13: +6). This has little or nothing to do with psychotherapy or social relationship management (29: −4, 28: −4, 40: −5). Psychology and relationships are a different life issue from CLBP problems and their solutions: self-management is not about self-esteem, [it] is about managing the pain (P31 to item 40); this is not pain management, this is relationship management. ‘In sickness and in health …’ this just adds guilt (P48 to item 28).
Factor 3: ‘Not sure what to/can change’ – managing the uncertainty and worried trust in healthcare providers
The third viewpoint was defined by the Q sorts of 11 people with pain (7 females, age range 27–81) and 3 female healthcare providers (age range 27–63). The main focus was on the uncertainty of how to manage the complex characteristics of CLBP in the context of what is perceived as the lack of clarity and understanding coming from service providers (56: +6): often a total lack of understanding (P41); too many different conditions that need too many different treatments (P20). There is a heavy reliance on the healthcare providers to take an advisory role (52: +3): patients need support from health professionals (P20). People with pain want clarity from healthcare providers and they want to be able to trust the advice they get: I do think that the professionals should be well prepared to give clear answers and advice to their patients otherwise they will not trust them which makes compliance with self-management difficult (P32). They value thorough examinations (48: +5) and proper diagnoses (49: +4), since these promise an end to anxious uncertainty: yes, it’s fear of the unknown that hampers how we cope (P41); some practitioners don’t give diagnosis so the patients don’t know what is wrong with them and they go back to pay more (P25 to 49). This is not so simple, however, and there is a perception that healthcare providers may not give clear answers and that the current health system lacks the kind of standardised framework that is needed to give people with pain consistent and effective help (60: +6, 54: +5): departments are too fragmented and isolated from each other (P41); ‘joined up thinking’ has to be beneficial – The whole picture is then considered (P38).
The result, from this viewpoint, was a lack of trust in professional advice and a sense of being misunderstood and of being sent away ill-equipped to self-manage (50: +4): being told to ‘go away and do this or that’ can be difficult to fit into your life (P20). They feel that managing pain is a complex affair that cannot be achieved by the patient alone (2: −6): health professionals should take an active role in self-management (HP26). They feel the need for regular contact with healthcare providers, and are reassured when they feel really cared for and empathised with (53: +4). They value a strong (ongoing) relationship of trust between person with pain and healthcare providers so that help can be accessed as and when needed. The professionals’ advice, however, needs to be easily transferable to people’s everyday lives (55: +5). Overall, there is a clear concern with trust and mutual understanding, which are evidently seen to be somewhat lacking: having faith and trusting health professionals is extremely important (HP26). This trust is vital given that people with pain often find their situation difficult to cope with, being ‘on the edge’ of extreme thoughts of crisis (40: +4) and forms of depression provoked by the pain: pain causes depression which can damage motivation (and the ability to deal) but realising that helps recovery (P20).
Factor 4: ‘The others need to change’ – questioning the politics and creating a mutual understanding of having CLBP
The fourth viewpoint was defined by the Q sorts of people with pain only (5 females, 3 males, age range 37–67). As with the third viewpoint, there was a strong feeling that pain management should not mean coping alone, and strong agreement that healthcare providers should be available for help, guidance and follow-up (52: +6, 53: +6): there is no human being who does not rely on anyone. We are social creatures, we cannot live in solitude (P60). Comments from participants expressed a clear preoccupation with the vital importance of knowing that health professionals are there to follow up how I’m doing well or not (P33), and with the sense that this need might be frustrated: it takes months to get an appointment (P59), perhaps not possible at current climate of NHS (P60). A distinctive feature of this perspective was a concern with how people with pain are portrayed and treated in society (33: −4): at work sometimes I am fine and wary that people think I’m lying (P58). Since pain is invisible, they find that others do not necessarily take it seriously or believe them (29: +5): I regularly experienced a culture of blame, disbelief and indifference from the medical profession (P59). They want to challenge the damaging perception that they are perhaps avoiding work or playing the system (34: +2). They also feel the need for expert proof of the validity of their pain. Medical imaging, for example, is valued partly because it can serve to prove the real existence of the pain (51: +5). The hope is that this validation might also lead to healthcare treatment that might cure the pain. Searching for this ‘magic bullet’ is not considered a barrier to achieving a good self-management (44: −4). This hope is a ‘double-edged sword’, however, since if no obvious physical causes are found, this can contribute to the climate of suspicion: unfortunately, visual evidence is the only way of fending off the suspicion of ‘feigning’ your pain (P59); It [a scan] helps, if anything is shown but augments the doubt towards health profession if nothing is shown (P60).
This viewpoint holds that people with pain are entitled to healthcare services in the NHS which should be freely accessible as and when needed (43: −5). In the context of cuts to these services, it can sometimes feel as though ‘self-management’ is a way to save on costs (8: +3, 4: −5): … ‘we can’t help anymore so here are some ideas to help you cope’ (P24). In this context, it becomes important to insist upon the rights of people with pain to treatment and the responsibilities of professionals to provide care (3: −6). It can be useful from this perspective to form alliances with those in similar positions, sharing experiences with other people with pain to get relevant information and knowledge (30: +4, 31: +4).
Those expressing this viewpoint first of all want their CLBP to be acknowledged (48: +4). They feel that self-management should not preclude the search for practical and effective treatments which cure the problem: Call a sniper [healthcare providers] and eliminate the terrorist [pain] with a sure shot (P60). They are aware, however, that this search is itself a way of coping with their situation (45: +3, 51: +5): You need to keep on looking because if a cure does come up you don’t want to miss it (P24); I don’t think it is a barrier, it can also be a goal for someone. Searching for latest ‘cure’ can provide means of coping for someone (P60).
Discussion
Four distinct viewpoints on self-management have been identified from 120 completed Q sorts. Each viewpoint is condensed into the pattern of a particular way of sorting the 60 statements (supported by open-ended comments), and these patterns have been interpreted and reported in qualitative detail. The first viewpoint is normative in the sense that most of our participants sorted according to this first pattern, including the vast majority (88%) of the service providers and 36 per cent of the service users. Having access to this ‘prototypical’ summary should be of significant value to future efforts to enhance self-management practice. The other viewpoints should not be neglected, however, since they are also coherent and feature aspects either peripheral to, or rejected by, the first viewpoint.
Two cross-cutting themes
Having these ‘snapshots’ of four distinct speaking positions provides a useful basis for exploring the evident scope both for agreement and tensions among self-management stakeholders. It is therefore of value to use this discussion section to bring out the key points of difference and similarity between the four viewpoints. The identification of points of difference which are sources of potential misunderstanding and even conflict is particularly valuable. Two themes can be identified which cut across the four viewpoints. These serve to highlight the key points of difference and similarity between the viewpoints, thus pointing to sources of potential misunderstanding which might interfere with self-management.
First theme: changing the self/resisting self-change
Consistent with previous findings (Eccleston et al., 1997; Martin et al., 2014), the relevance of what might be called the psychological dimension proves to be a key point of difference. However, while it is clear that explanations that invoke ‘psychology’ can be controversial, it is important not to assume a shared understanding of the meaning of ‘psychology’ since this notion appears to take on different significance from different viewpoints. The first factor places great importance on the need to change ‘mind-set’ and ‘attitudes’. This emphasis on mode of thought, however, ought not to be taken as indicating a set of psychological processes which exist in abstraction from the rest of the world. On the contrary, if ‘mind-set’ is important to this viewpoint, this is because it is tightly connected to action, to feeling and hence to physical wellbeing: thinking affects what we do: it’s fundamental (HP14). This explains the strong agreement with item 14 when compared to its ranking from the other three viewpoints, as indicated below:
| 14. Self-management is as much about changing how you think as it is about changing what you do | Factor 1+6 | Factor 2+1 | Factor 3+2 | Factor 40 |
The wording of this item is significant, since it does not suggest that ‘changing how you think’ is more important than ‘changing what you do’, but as important. The pragmatic focus of factor 2, by contrast, is concerned with changing what one does and not what one is. From this perspective, psychological themes of self-esteem or of managing negative feelings are actively rejected as issues not to be confused with self-management:
| 40. In self-management it is important to avoid extreme thoughts like ‘if I cannot self-manage then my whole world will collapse’ | Factor 1+3 | Factor 2−5 | Factor 3+4 | Factor 40 |
| 28. Managing pain is also about managing the strain it puts your relationships under: who wants to move from being a friend or partner to being a nurse or housekeeper? | +3 | −4 | 0 | +1 |
Despite this clear difference, it is interesting that feelings are welcomed as relevant by factor 2 in the much more practically relevant setting of overcoming fear of flare-ups which might hinder concrete activity:
| 18. Managing CLBP is overcoming the fear of doing something that will make it flare up or get worse | Factor 1+4 | Factor 2+3 | Factor 3−3 | Factor 4−2 |
A closely related dimension concerns the different meanings given to the ‘physicality’ associated with the search for underlying bio-medical factors explanatory of the pain. The different perspectives on this dimension are starkly illustrated by the rankings of item 44:
| 44. Searching for the magic cure for CLBP or the ‘silver bullet’ is a barrier to achieving self-management | Factor 1+6 | Factor 2−6 | Factor 3+3 | Factor 4−4 |
In short, a key part of the factor 1 project of ‘self-change’ is changing the (understandable) desire for a simple cure and accepting the need for ongoing self-management in the absence of a cure. Consistent with their stance on ‘the psychological’, factor 2 exemplars are unwilling to take this step of self-change prior to the availability of clear medical evidence, indicating the lack of a physical cause and possible cure: no. If I find the magic cure then this too will help improve my circumstances (HP01)); not in my experience. My silver bullets – Alexander Technique, massage, … physiotherapy exercises (P08); searching is fine till you get to #48 [thorough examination] + #49 [given a diagnosis].
Second theme: independence/isolation versus dependence/right to care
Factors 1 and 2 are broadly ‘in line’ with an agenda of self-management, with factor 2 taking a more narrowly focussed pragmatic position on the practicalities of how to do it (informed by expert knowledge). Both perspectives see that change is needed, but for factor 1, that change involves a more deep-seated change in mind-set rather than the adjustment of conduct that is the central concern of factor 2. Factors 3 and 4 are more complex in this respect. Factor 3 voices a profound uncertainty about how to proceed and about what can be changed, along with a critical sense of disappointment with the input of healthcare providers (who they both need to trust and fail to trust). Factor 4 voices a broader set of concerns. It is the societal perception and treatment of individuals with CLBP by others which needs to be changed, and this is sometimes associated with a cost-cutting governmental agenda which violates healthcare rights. The viewpoint of factor 3 is ‘irritated’, as it were, with a sense of misunderstanding, mistrust and even abandonment, while that of factor 4 is irritated by a sense of injustice and unfairness.
Both of these perspectives (factors 3 and 4) strongly resist the implication that self-management should mean the withdrawal of professional healthcare. This means that what might be seen positively as ‘independence’ from the perspectives of factors 1 and 2 shows up negatively as ‘isolation’ and even as the threat of ‘abandonment’ for factors 3 and 4. Symmetrically, what might be seen negatively as ‘dependence on healthcare providers’ from the perspectives of factors 1 and 2 shows up as claiming a ‘right to health-care’ and being ‘properly treated’ for factors 3 and 4. These critical attitudes make it likely that, despite being relatively minoritarian (at least in the context of the present study), the perspectives of factors 3 and 4 are likely to be loudly and resiliently voiced, and hence to constitute a significant part of the debate and practice around self-management. This theme of ‘independence/isolation’ is brought out starkly in the following comparative rankings:
| 2. Successful self-management means coping on your own and not having to rely on health professionals | Factor 1+1 | Factor 2+2 | Factor 3−6 | Factor 4−5 |
| 52. Self-management involves knowing when to ask for professional help | +2 | 0 | +3 | +6 |
| 53. Seeing a healthcare professional to touch base from time to time can be a big help to those self-managing CLBP | 0 | +1 | +4 | +6 |
In this context, the wish for diagnoses, scans and physical examinations is associated with the sense of a right to treatment and the need to prove the reality of the pain to sceptics:
| 49. Self-management is easier if you have a diagnosis because that lets you give a proper name to your enemy. | Factor 1−4 | Factor 2+2 | Factor 3+4 | Factor 4+2 |
| 48. Before self-managing in a confident way it is important to have a thorough physical examination. | −3 | +5 | +5 | +4 |
| 51. Medical imaging (x-ray, MRI) helps visually validate the pain. | −6 | +4 | +3 | +5 |
Despite the similarities noted above, factors 3 and 4 are distinct in that factor 3 tends to be critical of healthcare professionals, while factor 4 is more preoccupied with negative societal perceptions of people with pain.
These four factors (and two themes) provide a more nuanced appreciation of what, in certain circumstances, can become a ‘communication chasm’ (Kenny, 2004) between people with pain and healthcare providers. The findings suggest that the social object of CLBP self-management is understood in distinctive ways from these four perspectives, and that key differences in meaning emerge around (1) the significance of implicating the psychological dimension and (2) of themes connoting independence and autonomy versus isolation and abandonment. Clear communication is likely to be challenged by the fact that each perspective assumes a very different construction of these issues, and that – especially for factors 3 and 4 – these constructions carry different ethical implications concerning the sense of justice, rights and obligations. Such obstacles to communication are likely to play a key role in the low uptake of psychologically based rehabilitation programmes despite evidence for their effectiveness. As Martin et al. (2014) suggest, if self-management is to be effective, there must be more consistent investment in explaining pain, especially since the anxiety created by unexplained symptoms can compound the symptoms. The present findings also suggest that the notion of a ‘communication chasm’ can be overstated (Salmon et al., 2004), since the majority of our participants with pain voiced views in line with current policy and in agreement with the majority of our healthcare providers.
This study is limited, however, in that it can only provide a static ‘snapshot’ of the range of viewpoints expressed using this item set by a strategically sampled but self-selected group of participants. Regarding the latter point, it is possible that those most sceptical about CLBP self-management opted out of participation, and this possibility should be followed up in future work. We would thus not claim that the debate on CLBP self-management is limited to the four viewpoints explicated in this study. Regarding the former point, future research should investigate whether and how these ‘snapshots’ relate to and play out in concrete real-time (i.e. temporally unfolding) communicative practices. The authors have made a start on this by inviting factor exemplars to participate in a Knowledge Translation Conference designed to facilitate the recognition of multiple perspectives on the part of CLBP service providers and service users. Although a formal analysis of this event remains work-in-progress, it is clear that during real-time communication (e.g. between a service provider identified with factor 1 and a person with pain identified with factor 3), the viewpoints informing discursive contributions are more fluid and variable. Nevertheless, points of difference and tension emerged at the junctures suggested above that were discernable only thanks to the ‘crystallisations’ provided by the four factors. It is thus important to avoid reifying the four viewpoints if the findings are to be of practical value as a guide for understanding the realities of actual communicative practice (including the practice of self-management). Embedded in this appropriate theoretical context (Stenner, 2015), the findings enhance our knowledge of the viewpoints at play and provide a basis for improving self-management and behaviour change, as well as professional and patient training. The four factors, for example, provide a focus for reflexive conversation and practice, within and between service users and providers, aimed at increasing the confidence of people with pain in their ability to self-manage. They provide a basis for a more nuanced and tailored approach to self-management that recognises that different modes of engagement with it are grounded in qualitatively distinct modes of understanding (Hibbard et al., 2009). Enhanced self-management could reduce the impact of persisting problems or recurrences while lessening the burden on healthcare providers by reducing the number of treatments needed.
Conclusion
The study provides valuable insight into the diversity of stakeholder viewpoints on self-management. The first and largest viewpoint might be taken as the normative prototype of self-management practice. The other viewpoints (predominantly voiced by people with pain) articulate either neglected concerns for future consideration, or points of potential tension between different taken-for-granted viewpoints. Tensions include the orientation towards the psychological dimension, the significance of autonomy and independence with respect to responsibility for self-management, the attitude towards possible cure and the role and nature of healthcare provider input in a challenging economic context. In drawing attention to these differences and tensions, the study provides an informed basis, not just for the collaborative development of particular self-management strategies but also for the articulation of an explicit and consensually agreed conceptualisation of self-management. The absence of such a conceptualisation is likely to prove an obstacle to the effective coordination of the activities of stakeholders in CLBP self-management.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: The research reported here was funded by a grant from the Research for Patient Benefit Programme of the UK National Institute for Health Research (PB-PG-0909-20039), entitled: An exploration of self-care in chronic low-back disorder from the perspective of practitioners and patients: a Q methodological study.
References
- Airaksinen O, Brox JI, Cedraschi C, et al. (2006) Chapter 4: European guidelines for the management of chronic non-specific low back pain. European Spine Journal 15(S2): S192–S300. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Audulv A. (2013) The over time development of chronic illness self-management patterns: A longitudinal qualitative study. BMC Public Health 13: 452–466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Briggs AM, Slater H, Bunzli S, et al. (2012) Consumers’ experiences of back pain in rural Western Australia: Access to information and services, and self-management behaviours. BMC Health Services Research 12: 357–370. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown SR. (1981) Intensive analysis. In: Nimms D, Sanders KR. (eds) Handbook of Political Communication. Beverly Hills, CA: SAGE, pp. 627–649. [Google Scholar]
- Bury M, Newbould J, Taylor D. (2005) A Rapid Review of the Current State of Knowledge Regarding Lay-Led Self-Management of Chronic Illness: Evidence Review. London: NICE. [Google Scholar]
- Busby H, Williams G, Rogers A. (1997) 3. Bodies of knowledge: Lay and biomedical understandings of musculoskeletal disorders. Sociology of Health & Illness 19(19B): 79–99. [Google Scholar]
- Campbell C. (2009) A Q-methodological study to explore the low back pain beliefs and attitudes of low back pain health professionals. Journal of Pain Management 2(2): 91–111. [Google Scholar]
- Carnes D, Homer KE, Miles CL, et al. (2012) Effective delivery styles and content for self-management interventions for chronic musculoskeletal pain: A systematic literature review. Clinical Journal of Pain 28(4): 344–354. [DOI] [PubMed] [Google Scholar]
- Clarke L.H., Bennett E.V. (2013) Constructing the moral body: self-care among older adults with multiple chronic conditions. Health 17(3): 211–28. [DOI] [PubMed] [Google Scholar]
- Cooper K, Smith BH, Hancock E. (2009) Patients’ perceptions of self-management of chronic low back pain: Evidence for enhancing patient education and support. Physiotherapy 95(1): 43–50. [DOI] [PubMed] [Google Scholar]
- Corbett M, Foster N, Ong BN. (2009) GP attitudes and self-reported behaviour in primary care consultations for low back pain. Family Practice 26(5): 359–364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crowe M, Whitehead L, Gagan MJ, et al. (2010) Self-management and chronic low back pain: A qualitative study. Journal of Advanced Nursing 66(7): 1478–1486. [DOI] [PubMed] [Google Scholar]
- Dagenais S, Caro J, Haldeman S. (2008) A systematic review of low back pain cost of illness studies in the United States and internationally. Spine Journal 8(1): 8–20. [DOI] [PubMed] [Google Scholar]
- Department of Health (DoH) (2001) The Expert Patient: A New Approach to Chronic Disease Management for the 21st Century. London: DoH. [Google Scholar]
- Department of Health (DoH) (2005) Self Care – A Real Choice: Self Care Support – A Practical Option. London: DoH. [Google Scholar]
- Department of Health (DoH) (2006) The Musculoskeletal Services Framework – A Joint Responsibility: Doing it Differently. London: DoH. [Google Scholar]
- Department of Health (DoH) (2011) The NHS Outcomes Framework 2012/13. London: DoH. [Google Scholar]
- De Silva D. (2011) Evidence: Helping People Help Themselves – A Review of the Evidence Considering Whether It Is Worthwhile to Support Self-Management. London: The Health Foundation. [Google Scholar]
- Du S, Yuan C, Xiao X, et al. (2011) Self-management programs for chronic musculoskeletal pain conditions: A systematic review and meta-analysis. Patient Education and Counseling 85(3): e299–e310. [DOI] [PubMed] [Google Scholar]
- Eccleston C, Williams AC, Rogers WS. (1997) Patients’ and professionals’ understandings of the causes of chronic pain: Blame, responsibility and identity protection. Social Science & Medicine 45(5): 699–709. [DOI] [PubMed] [Google Scholar]
- Farrimond H, Joffe H, Stenner P. (2010) A Q-methodological study of smoking identities. Psychology & Health 25(8): 979–998. [DOI] [PubMed] [Google Scholar]
- Freburger JK, Holmes GM, Agans RP, et al. (2009) The rising prevalence of chronic low back pain. Archives of Internal Medicine 169(3): 251–258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow NJ, Jeon YH, Kraus SG, et al. (2008) Chronic disease self-management support: The way forward for Australia. Medical Journal of Australia 189(10): S14–S16. [DOI] [PubMed] [Google Scholar]
- Guttman L. (1954) Some necessary conditions for common-factor analysis. Psychometrika 19(2): 149–161. [Google Scholar]
- Henschke N, Ostelo RWJG, van Tulder MW, et al. (2010) Behavioural treatment for chronic low-back pain. Cochrane Database of Systematic Reviews 7: CD002014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hibbard JH, Greene J, Tusler M. (2009) Improving the outcomes of disease management by tailoring care to the patient’s level of activation. American Journal of Managed Care 15(6): 353–360. [PubMed] [Google Scholar]
- Hibbard JH, Mahoney ER, Stock R, et al. (2007) Do increases in patient activation result in improved self-management behaviors? Health Services Research 42(4): 1443–1463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hoy D, March L, Brooks P, et al. (2010) Measuring the global burden of low back pain. Best Practice & Research in Clinical Rheumatology 24(2): 155–165. [DOI] [PubMed] [Google Scholar]
- Institute of Medicine of the National Academics (2011) Relieving Pain in America: A Blueprint for Transforming Prevention, Care, Education, and Research. Washington, DC: The National Academies Press. [PubMed] [Google Scholar]
- Johannes CB, Le TK, Zhou XL, et al. (2010) The prevalence of chronic pain in United States adults: Results of an internet-based survey. Journal of Pain 11(11): 1230–1239. [DOI] [PubMed] [Google Scholar]
- Kawi J. (2014) Chronic low back pain patients’ perceptions on self-management, self-management support, and functional ability. Pain Management Nursing 15(1): 258–264. [DOI] [PubMed] [Google Scholar]
- Kennedy A, Reeves D, Bower P, et al. (2007) The effectiveness and cost effectiveness of a national lay-led self care support programme for patients with long-term conditions: A pragmatic randomised controlled trial. Journal of Epidemiology and Community Health 61(3): 254–261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kenny DT. (2004) Constructions of chronic pain in doctor-patient relationships: Bridging the communication chasm. Patient Education and Counseling 52(3): 297–305. [DOI] [PubMed] [Google Scholar]
- Koes BW, van Tulder M, Lin CW, et al. (2010) An updated overview of clinical guidelines for the management of non-specific low back pain in primary care. European Spine Journal 19(12): 2075–2094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lamb SE, Hansen Z, Lall R, et al. (2010) Group cognitive behavioural treatment for low-back pain in primary care: A randomised controlled trial and cost-effectiveness analysis. Lancet 375(9718): 916–923. [DOI] [PubMed] [Google Scholar]
- Lawn S, Battersby M, Lindner H, et al. (2009) What skills do primary health care professionals need to provide effective self-management support? Seeking consumer perspectives. Australian Journal of Primary Health 15(1): 37–44. [Google Scholar]
- Lorig K. (2003) Self-management education: More than a nice extra. Medical Care 41(6): 699–701. [DOI] [PubMed] [Google Scholar]
- McParland J, Hezseltine L, Serpell M, et al. (2011) An investigation of constructions of justice and injustice in chronic pain: A Q-methodology approach. Journal of Health Psychology 16(6): 873–883. [DOI] [PubMed] [Google Scholar]
- Martin S, Daniel C, Williams AC. (2014) How do people understand their neuropathic pain? A Q-study. Pain 155(2): 349–355. [DOI] [PubMed] [Google Scholar]
- Miles CL, Pincus T, Carnes D, et al. (2011) Can we identify how programmes aimed at promoting self-management in musculoskeletal pain work and who benefits? A systematic review of sub-group analysis within RCTs. European Journal of Pain 15(8): 775.e1–775.e11. [DOI] [PubMed] [Google Scholar]
- Oliveira VC, Ferreira PH, Maher CG, et al. (2012) Effectiveness of self-management of low back pain: Systematic review with meta-analysis. Arthritis Care and Research 64(11): 1739–1748. [DOI] [PubMed] [Google Scholar]
- Ong BN, Rogers A, Kennedy A, et al. (2014) Behaviour change and social blinkers? The role of sociology in trials of self-management behaviour in chronic conditions. Sociology of Health & Illness 36(2): 226–238. [DOI] [PubMed] [Google Scholar]
- Peters S, Stanley I, Rose M, et al. (1998) Patients with medically unexplained symptoms: Sources of patients’ authority and implications for demands on medical care. Social Science & Medicine 46(4–5): 559–565. [DOI] [PubMed] [Google Scholar]
- Risdon A, Eccleston C, Crombez G, et al. (2003) How can we learn to live with pain? A Q-methodological analysis of the diverse understandings of acceptance of chronic pain. Social Science & Medicine 56(2): 375–386. [DOI] [PubMed] [Google Scholar]
- Rogers A, Kennedy A, Bower P, et al. (2008) The United Kingdom Expert Patients Programme: Results and implications from a national evaluation. Medical Journal of Australia 189(10): S21–S24. [DOI] [PubMed] [Google Scholar]
- Salmon P, Dowrick CF, Ring A, et al. (2004) Voiced but unheard agendas: Qualitative analysis of the psychosocial cues that patients with unexplained symptoms present to general practitioners. British Journal of General Practice 54(500): 171–176. [PMC free article] [PubMed] [Google Scholar]
- Savigny P, Watson P, Underwood M, et al. (2009) Guidelines: Early management of persistent non-specific low back pain: Summary of NICE guidance. British Medical Journal 338: b1805. [DOI] [PubMed] [Google Scholar]
- Stainton Rogers W. (1991) Explaining Health and Illness: An Exploration of Diversity. New York; London: Harvester Wheatsheaf. [Google Scholar]
- Stenner P. (2015) A transdisciplinary psychosocial approach. In: Slaney K, Martin J, Sugarman J. (eds) The Wiley Handbook of Theoretical and Philosophical Psychology: Methods, Approaches and New Directions for Social Science. New York: Wiley, pp. 308–354. [Google Scholar]
- Stenner P, Stainton R. (2004) Q methodology and qualiquantology: The example of discriminating between emotions. In: Todd Z, Nerlich B, McKeown S, Clarke DD. (eds) Mixing Methods in Psychology: The Integration of Qualitative and Quantitative Methods in Theory and Practice. New York: Psychology Press. [Google Scholar]
- Stenner P, Watts S, Worrell M. (2008) Q methodology. In: Willig C, Stainton W. (eds) The Sage Handbook of Qualitative Research in Psychology. London: SAGE, pp. 215–239. [Google Scholar]
- Stenner PHD, Cooper D, Skevington SM. (2003) Putting the Q into quality of life; the identification of subjective constructions of health-related quality of life using Q methodology. Social Science & Medicine 57(11): 2161–2172. [DOI] [PubMed] [Google Scholar]
- Toye F, Barker K. (2012) ‘I can’t see any reason for stopping doing anything, but I might have to do it differently’ – Restoring hope to patients with persistent non-specific low back pain – A qualitative study. Disability and Rehabilitation 34(11): 894–903. [DOI] [PubMed] [Google Scholar]
- Trappenburg J, Jonkman N, Jaarsma T, et al. (2013) Self-management: One size does not fit all. Patient Education and Counseling 92(1): 134–137. [DOI] [PubMed] [Google Scholar]
- Van Hooff ML, Ter Avest W, Horsting PP, et al. (2012) A short, intensive cognitive behavioral pain management program reduces health-care use in patients with chronic low back pain: Two-year follow-up results of a prospective cohort. European Spine Journal 21(7): 1257–1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Von Korff M, Ormel J, Keefe FJ, et al. (1992) Grading the severity of chronic pain. Pain 50(2): 133–149. [DOI] [PubMed] [Google Scholar]
- Watts S, Stenner P. (2012) Doing Q-Methodological Research: Theory, Method and Interpretation. London: SAGE. [Google Scholar]
- Williams AC, Eccleston C, Morley S. (2012) Psychological therapies for the management of chronic pain (excluding headache) in adults. Cochrane Database of Systematic Reviews 11: Cd007407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zufferey MC, Schulz PJ. (2009) Self-management of chronic low back pain: An exploration of the impact of a patient-centered website. Patient Education and Counseling 77(1): 27–32. [DOI] [PubMed] [Google Scholar]