Abstract
There are over 35 million people worldwide infected with the Human Immunodeficiency Virus (HIV) and its progression to Acquired Immunodeficiency Syndrome (AIDS; WHO, 2014). With the advent of combined antiretroviral therapy (i.e., cART) in 1996, persons living with HIV/AIDS (PLWHA) now have much longer life expectancies. However, living with HIV remains challenging, as it is associated with a number of significant and recurrent (chronic) stressors including physical pain, side effects of cART, social stigma, and discrimination, among other social stressors. Presumably, as a result of these types of stressors, a disproportionately high number of PLWHA struggle with clinically-significant psychiatric symptoms and disorders. Although much scientific and clinical attention has focused on depressed mood and psychopathology among PLWHA, there has been comparably less focus on anxiety and its disorders. The paucity of work in this area is concerning from a public health perspective, as anxiety symptoms and disorders are the most common class of psychiatric disorders and often maintain a large negative impact on life functioning.
1. Introduction
Relatively little is known about the nature of the anxiety-HIV/AIDS relation. Drawing from extant empirical work and conceptual models, there is reason to theorize that anxiety symptoms and disorders may play a role in the engagement (or lack of engagement) in behaviors that increase risk for HIV/AIDS (i.e., unprotected sex, substance use), and the experience of living with HIV/AIDS may be related to anxiety psychopathology. The common comorbidity of anxiety and HIV/AIDS may suggest that integrated intervention strategies (prevention, treatment, and health promotion) for these conditions are needed. By better understanding the nature of the association between HIV/AIDS and anxiety problems, advances will be made in understanding the processes underlying comorbidity between multiple anxiety disorders and health disorders more generally (i.e., transdiagnostic processes).
Although there have been two attempts to summarize some aspects of the larger empirical literature on anxiety and HIV/AIDS (i.e., O’Cleirigh, Hart, & James, 2008; Rabkin, 1996), these overviews did not comprehensively seek to review the anxiety-HIV/AIDS co-occurrence. For instance, Rabkin (1996) examined prevalence rates of all mood disorders, and noted a distinct lack of empirical data regarding anxiety disorders at the time, where as O’Cleirigh et al. (2008) focused on providing an overview of studies largely dealing with the co-occurrence of posttraumatic stress and anxiety disorders among PLWHA. Here, it is noteworthy that certain populations, such as trauma-exposed samples, were disproportionately reviewed despite traumatic stress disorders not being formally being recognized as anxiety disorders in the most recent diagnostic system (APA, 2013). Also, because of the publication dates of these papers (i.e., 1996 and 2008, respectively), they do not contain coverage of work that has been completed after these time points (i.e., 2008–present); a period of time wherein there has been a great amount of growth in this literature, as documented in this review. Additionally, past summaries focused on linkages between anxiety symptoms and disorders and only a few clinical HIV/AIDS processes (e.g., medication adherence). Moreover, none addressed transdiagnostic individual difference factors that may undergird relations between anxiety and HIV/AIDS.
The current investigation was undertaken as an integrative literature review as opposed to a meta-analytic review. This decision was made primarily for two reasons. First, we believe that the former is better able to highlight the broad similarities across a literature that uses vastly different study methodologies, measurement techniques, and population samples. Second, given the dissimilarity of many of the samples and small number of studies focused on this topic, a meta-analytic review may be a premature research approach at the present time.
The purpose of the present paper is to review the available empirical literature on the relation between anxiety symptoms and disorders and HIV/AIDS. In the first section, we define our search strategy and offer operational definitions employed in the review. In the second section, we review empirical studies that document the comorbidity of HIV/AIDS and anxiety disorders. In the third section, we review studies addressing anxiety and its disorders in terms of clinical HIV/AIDS processes (e.g., quality of life, medication adherence). In the fourth section, we review studies addressing transdiagnostic individual difference factors that may underlie linkages between anxiety and HIV/AIDS. Finally, we propose an integrative theoretical model for understanding the role of anxiety in HIV/AIDS and conclude with several clinical and scientific implications that can be drawn from this approach.
2. Study selection criteria
PRIMSA guidelines for the literature search were used (see Fig. 1). We conducted a literature search utilizing electronic search engines (i.e., PsycINFO and PubMed) to examine databases using the following key word algorithms: HIV OR AIDS AND anxiety OR anxiety disorder. This search led to 82 articles that were relevant to the current review.
Fig. 1.
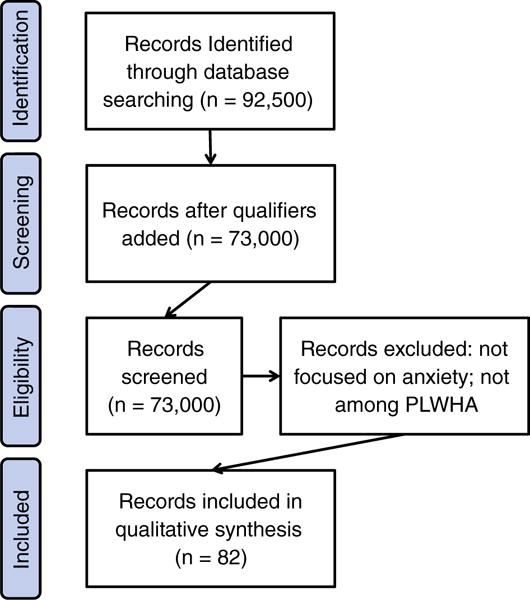
PRIMSA study selection guidelines.
3. Conceptual basis and definitions of key variables
3.1. HIV/AIDS
HIV is a retrovirus that is transmitted via exposure to contaminated bodily fluids. The recognition of HIV and its progression to AIDS is now widely recognized as a pandemic problem (World Health Organization WHO, 2014). Estimates suggest that 35 million individuals worldwide are currently infected with HIV and approximately 1.5 million people have died from AIDS within the last year (WHO, 2014). Although in the U.S. HIV/AIDS once primarily affected White, homosexual, and bisexual men (Kelly & Murphy, 1992), it is increasingly common among heterosexual men and women, children, and people of color (CDC, 2013). Although the number of diagnosed AIDS cases has remained stable from 2002 to 2006 (approximately 37,000 per year), the number of deaths due to AIDS has decreased by approximately 16,500 per year from 2002 to 2005 to approximately 14,000 deaths in 2006 (CDC, 2013). Thus, there has been a ‘shift’ to the management of HIV/AIDS as a chronic (vs. terminal) illness in the U.S. and other developed countries (Siegel & Lekas, 2002). This shift in the treatment landscape indicates the importance of presumed date of HIV infection, as those infected earlier may have a different experience with HIV than those infected more recently. Study publication date is therefore indicated for all studies and significant departures between data collection and publication date are noted accordingly.
3.2. Anxiety
According to the DSM-5 (APA, 2013), anxiety disorders share features of excessive fear (emotional response to real or perceived threat) and anxiety (anticipation of future threat) and include experience of one or more “anxiety states” (physiological activation, behavioral response, cognition). The anxiety disorders differ from one another in the types of objects or situations that elicit such emotions behaviors and cognition. Anxiety disorders differ from normative anxiety by being excessive, persistent (e.g., typically lasting 6 months or more), and life impairing. See Table 1 for DSM-5 defined anxiety disorders covered in the current review. It is important to note that the DSM-5 lists Post-Traumatic Stress Disorder as well as Obsessive Compulsive Disorder as categories separate from anxiety. As a result, these disorders are not covered in the current review.
Table 1.
DSM-5 anxiety disorders.
| Anxiety disorder | Distinguishing symptoms | 12-Month prevalence |
|---|---|---|
| Specific phobia | • Marked fear or anxiety about a specific object or situation | 7–9% of adults |
| Social anxiety disorder | • Marked fear or anxiety about one or more social situations in which the individual is exposed to possible scrutiny by others • Fear of negative evaluation |
2–7% of adults |
| Panic disorder | • Recurrent unexpected panic attacks • At least one panic attack followed by worry of future attacks or changes in behavior to avoid future attacks |
2–3% of adults |
| Agoraphobia | • Marked fear or anxiety about situations in which one may have a panic attack (e.g. being in open spaces, being outside of the home alone) • Avoidance of such situations because escape may not be available |
1.7% of adults |
| Generalized anxiety disorder | • Excessive anxiety and worry about a number of events or activities • Difficulty controlling worry |
0.4–3.6% of adults |
4. Anxiety disorders among the HIV/AIDS population
Existing studies examining prevalence of anxiety disorders among PLWHA were evaluated using two methodologies. First, each study was reviewed individually and important information (i.e., authors, study characteristics including sample size and sample population, inclusion of a control or comparison group, anxiety measurement technique utilized, and rates of anxiety disorders) was synthesized in a table format (please see Tables 2–4). Articles examining anxiety-HIV/AIDS comorbidity were grouped into three population sets: (1) the extent to which anxiety disorders are present among PLWHA in the U.S. and other developed countries (17 studies; see Table 2); (2) the extent to which anxiety disorders are present among PLWHA in developing countries or regions (11 studies; see Tables 2, 3); and (3) rates of HIV among anxiety-disordered persons (1 study; see Table 4). Second, in order to visually interpret prevalence of anxiety among PLWHA across these studies, box and whisker plots were constructed to indicate median prevalence rates, as well as first and third quartiles, and sample high and low prevalence values (see Figs. 2–5). Here, each study was weighed equally regardless of sample size. When examining the prevalence of anxiety disorders across studies, a number of discernable patterns emerge as well as a number of limitations to the extant literature.
Table 2.
Rates of anxiety disorders in developed countries (ordered chronologically).
| Authors | Study characteristics | Control group | Measurement of anxiety disorders | Rates of anxiety disorders |
|---|---|---|---|---|
| Sewell et al., 2000 | n = 183 homosexual HIV+ men who reported nonintravenous drug use | 84 seronegative nonintravenous drug using homosexual men; national comorbidity study as additional control group | Structured Clinical Interview for the DSM-IV Axis I (SCID-I4) | 19% of HIV+ participants met criteria for any anxiety disorder, compared to 18% in seronegative control group and 19% in the national comorbidity survey. There were no significant differences in rates of agoraphobia w/o panic, OCD, panic disorder, social phobia, or simple phobia. |
| Orlando et al., 2002 | n = 2864 selected from the HIV Cost and Services Utilization Study (HCSUS1) who were reached for reassessment | None | Composite International Diagnostic Interview – Short Form (CIDI-SF2) | At baseline assessment 47.9% of participants met criteria for any psychological disorder, 15.8% met criteria for GAD and 10.5% met criteria for panic disorder |
| Tucker, Burnam, Sherbourne, Kung, & Gifford, 2003 | n = 1910 participants selected from the HIV Cost and Services Utilization Study (HCSUS1) indicating medication adherence | None | Composite International Diagnostic Interview (CIDI3) for GAD and panic disorder | 3% of the total sample met criteria for GAD, and 13% for panic disorder |
| Mellins, Kang, Leu, Havens, & Chesney, 2003 | n = 128 HIV + females; 58% African American | None | Clinical Diagnostic Questionnaire (CDQ5) | 50% of participants met criteria for a current psychiatric disorder |
| Palmer, Salcedo, Miller, Winiarski, & Arno, 2003 | n = 107; 47% male, 63% Hispanic | None | SCID-I4 | 12% met criteria for panic disorder with and without agoraphobia; 0% met criteria for GAD |
| Ingersoll, 2004 | n = 120; 61.7% male, 83.3% African American, 47.5% disabled | None | CIDI-SF2 | 44.4% met criteria for any anxiety disorder, 26.1% for simple phobia, 14.8% for social phobia, 11.3% for panic attacks, and 9.6% for agoraphobia |
| Lambert, Keegan, & Petrak, 2005 | n = 82 HIV+ females; 75% African American, 63% unemployed | None | Hospital Anxiety and Depression Scale (HADS6) | 44% experienced moderate to severe anxiety, indicative of an anxiety disorder |
| Whetten et al., 2006 | n = 141; 55.7% male, 79.3% African American, 63.1% temporarily/permanently disabled | None | SCID-I4 | 29.8% of participants met criteria for PTSD, 9.22% met criteria for panic disorder |
| Pence, Miller, Whetten, Eron, & Gaynes, 2006 | n = 1125; 66.7% male, 62.6% African American | None | Substance Abuse and Mental Illness Symptom Screener (SAMISS7) | 20.3% of participants met criteria for any anxiety disorder, 5.4% for panic disorder, |
| Nurutdinova et al., 2012 | n = 9003; review of medical records for ICD-9-CM diagnostic codes | None | Psychiatric Disorder Diagnoses through VA healthcare system | 18% of HIV+ veterans met criteria for an anxiety disorder |
| Reif et al., 2012 | n = 40; 65% male, 80% African American, 62% over age 40 | None | Brief Symptom Inventory (BSI8) and Short Form-12 mental health index (SF-129) | scores indicated 33% had a “probably anxiety disorder” |
| Lopes et al., 2012 | n = 34,653 individuals taken from the National Epidemiologic Survey on Alcohol and Related Conditions, including 149 PLWHA | Non-HIV infected persons assessed during this survey | Alcohol Use Disorder and Associated Disabilities Interview Schedule – DSM-IV Version (AUDADIS-IV; Grant et al., 2003) | HIV+ men were four times as likely to meet criteria for an anxiety disorder compared to HIV− men (OR = 4.02; 33.43% met criteria for any anxiety disorder), while HIV+ women were only marginally more likely to meet criteria for an anxiety disorder compared to HIV− women (OR = 1.17; 23.74% met criteria for any anxiety disorder). |
| Parhami, Fong, Siani, Carlotti, & Khanlou, 2013 | n = review of 7834 medical records from HIV+ persons in California; mean age = 43.57, 88% male, 37% white | None | Diagnoses taken from medical records through AIDS Healthcare Foundation | 16% of sample met criteria for an anxiety disorder |
| Glémaud et al., 2014 | n = 96 HIV+ Haitian females, mean age = 74.6 | None | Primary Care Evaluation of Mental Disorders Patient Health Questionnaire (PRIME-MD10) | 42.7% of participants reported significant anxiety, and 2.1% reported panic-like symptoms |
| Robertson et al., 2014 | n = 2863 PLWHA, 61.7% male, mean age = 42.9 | None | HADS6 | 33.3% of sample met criteria for a “possible anxiety disorder” |
| Kosiba, Gonzalez, O’Cleirigh, & Safren, 2014 | n = 131 PLWHA in treatment for opioid use | None | MINI International Neuropsychiatric Interview (MINI15) | Among PLWHA 15.5% met criteria for GAD and 15.1% met criteria for PD. Among controls 4.3% met criteria for GAD, 6.5% met criteria for PD. All ps < 0.001 |
| O’Cleirigh, Magidson, Skeer, Mayer, & Safren, 2014 | n = 503 HIV infected gay/bisexual men | None | Medical Record Review | 22.3% of participants met criteria for social phobia, 9.5% met criteria for panic disorder, and 7.8% met criteria for GAD |
HIV Cost and Services Utilization Study (HCSUS; Bozzette et al., 1999);
Composite International Diagnostic Interview – Short Form (CIDI-SF; Kessler, Andrews, Mroczek, Ustun, & Wittchen, 1998b);
Composite International Diagnostic Interview (CIDI; Kessler, Andrews, Ustun, & Wittchen, 1998a);
Structured Clinical Interview for the DSM-IV Axis I (SCID-I; First, Gibbon, Spitzer, & Williams, 1995);
Clinical Diagnostic Questionnaire (CDQ; Aidala et al., 2004);
Hospital Anxiety and Depression Scale (HADS; Zigmond & Snaith, 1983);
Substance Abuse and Mental Illness Symptom Screener (SAMISS; Pence et al., 2005);
Brief Symptom Inventory (BSI, Derogatis & Melisaratos, 1983);
Short Form-12 mental health index (SF-12, Hurst, Kind, & Ruta, 1998);
Primary Care Evaluation of Mental Disorders Patient Health Questionnaire (PRIME-MD; Spitzer, Kroenke, & Williams, 1999);
Alcohol Use Disorder and Associated Disabilities Interview Schedule – DSM-IV Version (AUDADIS-IV; Grant et al., 2003);
Composite International Diagnostic Interview (CIDI; Kessler, et al., 1998b);
MINI International Neuropsychiatric Interview (MINI; Sheehan et al., 1998).
Table 4.
Rates of HIV among anxiety-disordered populations.
| Authors | Study characteristics | Control group | Measurement of anxiety disorders | Rates of anxiety disorders |
|---|---|---|---|---|
| Stoskopf, Kim, & Glover, 2001 | n = 378.710 individuals, 1775 HIV+ individuals | None | Data from a range of Hospitals in South Carolina was taken, ICD-91 diagnostic codes were used | People with mental illness were 1.44 times as likely to have HIV/AIDS than persons without a mental illness (p < 0.001) |
International Classification of Diseases-9; (ICD-9, US Department of Health and Human Services, 1980).
Table 3.
Rates of anxiety disorders in developing countries (ordered chronologically).
| Authors | Study characteristics | Control group | Measurement of anxiety disorders | Rates of anxiety disorders |
|---|---|---|---|---|
| Petrushkin, Boardman, & Ovuga, 2005 | n = 46 Ugandans, 52.2% female, mean age = 36.6 | None | MINI International Neuropsychiatric Interview (MINI1) | 32.6% met criteria for panic disorder, 23.9% met criteria for panic with agoraphobia, 10.9% for social anxiety disorder, and 4.3% for OCD |
| Olley, Seedat, Nei, & Stein, 2004 | n = 149 HIV+ individuals living in South Africa; 70% female, mean age = 30 | None | MINI1 | 14.8% of participants met criteria for PTSD, and 6.7% met criteria for GAD |
| Adewuya et al., 2007 | n = 88 HIV+ individuals living in Nigeria newly diagnosed with HIV (first seropositive test < 1 month prior) | 87 seronegative controls matched on age, sex, andsocioeconomic status | MINI1 | 34.1% of HIV+ participants met criteria for any anxiety disorder, compared to 12.5% of controls (Odds Ratio = 3.57; CI = 1.657.72) |
| Spies et al., 2009 | n = 429 HIV+ individuals living in South Africa; 67% Xhosa speaking, 25% Afrikaans speaking, 8% English speaking | None | K-102 and MINI1 | 15.3% met criteria for panic disorder, 18.4% agoraphobia, 12.3% social phobia, 21.5% PTSD, and 18.4% GAD |
| Marwick & Kaaya, 2010 | n = 220 HIV+ persons living in Tanzania, 74% female, mean age = 41 | None | Clinical Interview Schedule-Revised (CIS-R3) | 12.7% of participants met criteria for mixed anxiety and depression, 3.2% for a specific phobia, 1.8% for panic disorder, and 0.9% for OCD |
| Campos, Guimaraes, & Remien, 2010 | n = 293 HIV+ individuals living in Brazil; 65.9% male, 52.9% under age 35 | None | HADS4 | 35.8% of participants met criteria for moderate and severe anxiety, indicating an anxiety disorder |
| Sivasubramanian et al., 2011 | n = 150 HIV+ men who have sex with men in Mumbai, India | None | MINI1 | 24% met criteria for any anxiety disorder |
| Nebhinani, Mattoo, & Wanchu, 2011 | n = 100 HIV+ individuals living in India; 59% male, mean age = 33.6 | 40 patients with rheumatoid arthritis | Structured Clinical Interview for the DSM-IV Clinician Version (SCID-CV5) | 1% of participants with HIV met criteria for panic disorder; 2.5% of participants with RA met criteria for panic disorder |
| Hasanah, Zaliha, & Mahiran, 2011 | n = 271 PLWHA in Malaysia, 57.6% male, 60.1% between ages 30–39 | None | HADS4 | 29% of the sample met criteria for a “probable anxiety disorder” |
| Olagunju, Adeyemi, Ogbolu, & Campbell, 2012 | n = 300 HIV+ individuals living with HIV in Lagos, Nigeria; 38.7% male, mean age = 36.95 | None | Schedule for Clinical Assessment in Neuropsychiatry (SCAN6) | 21.7% of the sample met criteria for an anxiety disorder, including 4% for social anxiety disorder, 1.7% for panic disorder, and 6.2% for “anxiety disorder unspecified” |
| Breuer et al., 2014 | n = 366 HIV+ individuals living in South Africa; 71% female, mean age = 32.7 | None | Substance and Mental Illness Symptom Screener (SAMISS7) and Mini International Neuropsychiatric Interview (MINI1) | 3% of the sample met criteria for an anxiety disorder |
MINI International Neuropsychiatric Interview (MINI; Sheehan et al., 1998);
K-10, Kessler et al., 2002;
Clinical Interview Schedule-Revised (CIS-R; Lewis, Pelosi, Araya, Dunn, 1992);
Hospital Anxiety and Depression Scale (HADS; Zigmond & Snaith, 1983);
Structured Clinical Interview for the DSM-IV Clinician Version (SCID-CV; First, Spitzer, Gibbon, & Williams, 1997);
Schedule for Clinical Assessment in Neuropsychiatry (SCAN; World Health Organization, 1995);
Substance and Mental Illness Symptom Screener (SAMISS; Pence et al., 2005).
Fig. 2.
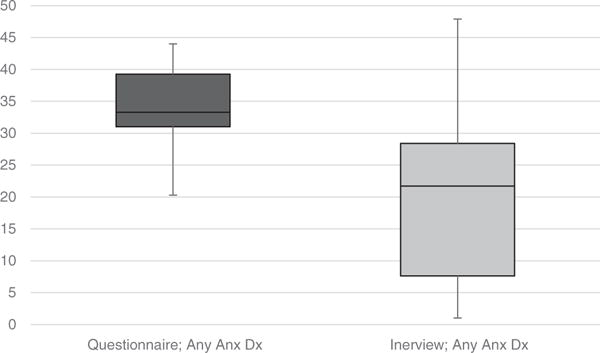
Rates of anxiety disorders as diagnosed by questionnaire compared to interview.
Fig. 5.
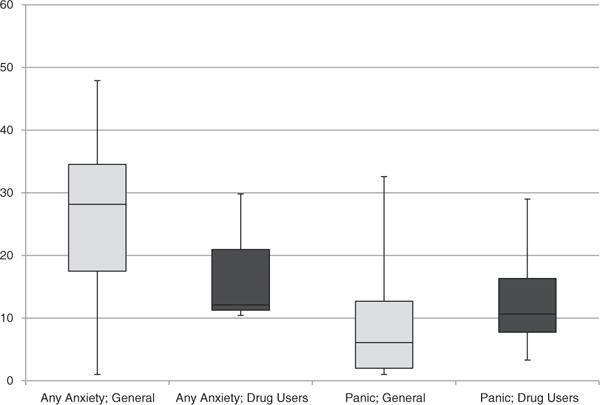
Rates of anxiety disorders in drug-using compared to non-drug using groups.
First, rates of anxiety disorders diagnoses were significantly higher when questionnaire-based assessments (median = 33.3%) as compared to a diagnostic interview (median = 22.85%; see Fig. 2) were employed. Second, when examining rates of anxiety disorder diagnoses among all studies utilizing diagnostic interview (i.e., developed and developing countries; n = 6–16; see Fig. 3), prevalence rates for anxiety disorders are notably higher among PLWHA than the general population. For instance, the median value of anxiety disorders among PLWHA in the reviewed studies was 22.85%, which is notably higher than the general population (18%; Kessler, Chiu, Demler, & Walters, 2005). When examining specific anxiety disorders individually, similar trends emerge for panic disorder (10.26% among PLWHA, compared to 3% for the general population), GAD (5.6% compared to 2.5%), and social anxiety disorder (9.1% compared to 6%). One disorder that does not follow this trend is specific phobia, where 3.85% of PLWHA meet criteria for this illness compared to approximately 8% in the general population. Although studies have found generally high rates of anxiety disorders among PLWHA (median prevalence rate across all studies = 27.9%; range 1% to 47.8%), control/comparison groups have rarely been employed in such work. Therefore, it is challenging to ascertain the nature of ‘true’ differences in base rates of anxiety disorders among PLWHA versus non-HIV+ samples.
Fig. 3.
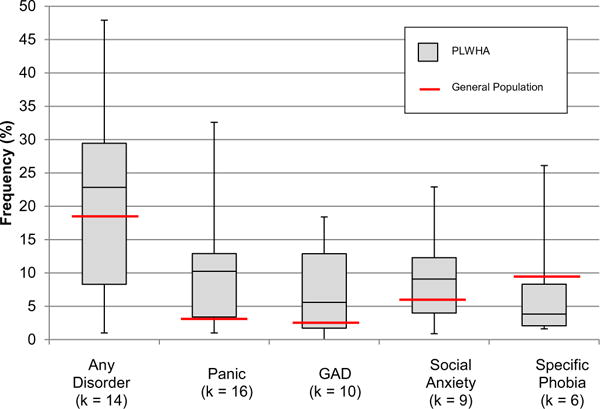
Rates of anxiety disorders among PLWHA using diagnostic interview.
Third, rates of anxiety disorders as diagnosed using diagnostic interview are higher among developed countries (median = 28.5%) compared to developing countries (median = 22.85%; see Fig. 4). The indication that PLWHA in developed countries present with anxiety disorders at higher rates than those found in developing countries may be due to a number of factors, including stigma and knowledge about mental health.
Fig. 4.
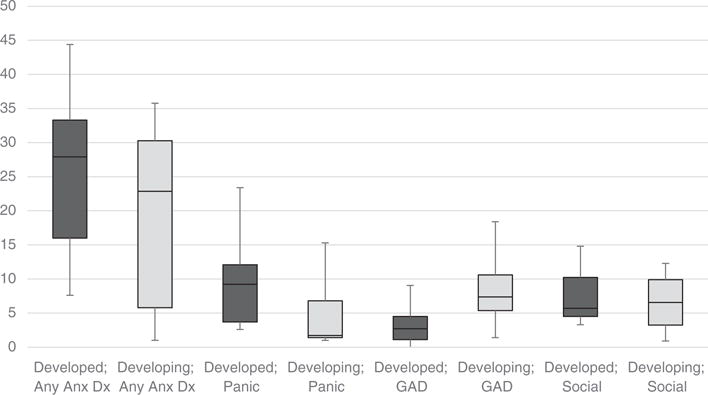
Rates of anxiety disorders in developed compared to developing countries.
Fourth, when examining rate of anxiety disorders among specific drug-using PLWHA compared to PLWHA who were not specifically selected for their drug-use status, rates of any anxiety disorder were notably higher among non-drug users compared to drug users (see Fig. 5). However, rates of panic disorder were higher among drug-users compared to non-drug users. This finding is in line with existing literature indicating that drug users may have a higher sensitivity to physical sensations, and may use drugs to escape these sensations, or be unable to quit using drugs because of withdrawal effects (Cox, Norton, Swinson, & Endler, 1990). However, a small number of samples limit the utility of this work, and additional research is needed to more fully understand these relations.
Fifth, it is important to note that one limiting factor of the existing literature is that there is limited work examining rates of anxiety disorders across different population groups with high rates of HIV infection. In particular, men who have sex with men (MSM) comprise over half of all HIV infections nationally (CDC, 2013). Future work examining rates of anxiety among this population specifically, as well as other groups indexing high rates of HIV infection (e.g., drug users, low SES women) more generally.
Sixth, it is yet not clear whether the strength of the observed associations between anxiety and HIV is attenuated when psychiatric comorbidity, particularly substance use disorders and other medical disorders, is controlled/adjusted. As predicted by syndemic models of health, because HIV and anxiety comorbidity may co-occur within a larger context of substance use and health behavior (e.g., O’Cleirigh et al., 2008), future work is needed to explore how such co-occurring processes (in combination) affect the observed relations.
Finally, across all reviewed work, none of the studies have employed an empirically-derived representative sample. Thus, it is not possible to rule out the role of systematic sampling biases across this body of work. For example, the vast majority of studies documenting HIV-anxiety co-occurrence have been conducted in samples seeking treatment for anxiety or anxiety-related issues. Alternatively, PLWHA engaged in care may represent a healthier sample that PLWHA not linked to care, or PLWHA unaware of their HIV status.
5. Anxiety and its disorders in relation to HIV/AIDS clinical processes
There is an emerging empirical literature aimed at exploring the role of anxiety and its disorders in terms of clinical features of HIV/AIDS. These studies demark a growth from earlier work that has been largely focused on prevalence and begin to shed empirical light on the nature of the distinct facets of anxiety to HIV/AIDS processes (e.g., disease progression, medication adherence). In this context, it is important to consider that multiple bi-directional processes are potentially applicable across various stages of disorder development. For example, HIV/AIDS may increase the risk for developing anxiety symptoms and disorders and at the same time anxiety states may influence the severity of HIV/AIDS. We have organized this section of the review around specific HIV/AIDS clinical processes that were most frequently cited in the extant literature, including disease progression, medication adherence, substance use, sexual risk taking, quality of life, suicidality, and cognitive functioning (see Table 5). Additionally, because the measures administered may affect reported rates of anxiety, this information is also presented in Table 5. To estimate the clinical significance of the observed effects, we standardized the effect sizes in the work reviewed and provided reference to these effects.
Table 5.
Anxiety and its disorders in relation to HIV/AIDS clinical processes (ordered chronologically by sub-category).
| Authors | Study characteristics | Clinical process | Outcome measured | Design | Main finding |
|---|---|---|---|---|---|
| Disease severity and progression | |||||
| Rabkin et al., 1991 | n = 124, 87% Caucasian, mean age = 38 | Hamilton Rating Scale for Anxiety (HAM-A2) | CD4 T-cell and lymphocyte subsets via blood testing | Cross-sectional; prospective | No significant relation between anxiety and CD4 T-cell decline or lymphocyte subsets cross-sectionally (ESU) or prospectively (r2 = 0.03) |
| Vassend, Eskld, & Halvorsen, 1997 | n = 65 PLWHA living in Oslo, Norway; mean age = 38 | Symptom Checklist-90 (SCL-903) | CD4 T-cell counts via blood testing | Prospective | Anxiety was not related to CD4 T-cell count (ESU) but was related to other possibly relevant factors, such as avoidant coping behavior (r2 = 0.12) |
| Thornton et al., 2000 | n = 161 PLWHA in London, 92.4% Caucasian, mean age = 40.4 | General Health Questionnaire 28 (GHQ-284) | CD4 T-cell count via blood testing | Prospective | “Anxiety and insomnia” as measured by the GHQ-28 was not significantly related to CD4 T-cell count (HR = 1.04) |
| Pence, Miller, Gaynes, & Eron (2007) | n = 198 cART naive PLWHA | 7 Substance Abuse and Mental Illness Symptom Screener (SAMISS; Pence et al., 2005) | 7 Substance Abuse and Mental Illness Symptom Screener (SAMISS; Pence et al., 2005) | Prospective | Participants with a higher predicted probability of mental illness and substance abuse took longer to achieve virologic suppression (adjusted hazard ration [aHR] = 0.86) and were quicker to demonstrate virologic failure (aHR = 1.22) |
| Fincham, Smit, Carey, Stein, & Seedat, 2008 | n = 456 PLWHA in South Africa, 72.4% Black, 67.3% Xhosa-speaking, 25% male | Anxiety disorder diagnosis (MINI1) | CD4 T-cell count via self-report | Cross-sectional | Anxiety disorder diagnosis was not predictive of CD4 T-cell count (Effect Size Unavailable [ESU]) |
| Nurutdinova et al., 2012 | n = 9003 Military Veterans, 98% male, 43% African American | ICD-95 anxiety disorder diagnoses via medical records review | CD4 T-cell count via medical record review | Prospective | Anxiety disorders were protective of all-cause mortality (OR = 0.80) and AIDS-defining illness (OR = 0.83) |
| HIV medication adherence | |||||
| Catz, Heckman, Kochman, & DiMarco, 2001 | n = 113 PLWHA, age 47–69 | Anxiety and somatization via the Symptom Checklist 90-Revised (SCL-90-R6) | Self-reported past-week HIV medication adherence | Cross-sectional | Patients reporting adhering to their medication had significantly lower levels of anxiety (r2 = 0.06) and somatization (r2 = 0.10) |
| Van Servellen, Chang, Garcia, & Lombardi, 2002 | n = 182, 56.93% male, 42.7% Hispanic, average age 38.15 | Hospital Anxiety and Depression Scale (HADS7) | Self-reported HIV medication adherence, confirmed with medical record review | Cross-sectional | HADS Anxiety scores significantly predicted self-reported HIV medication nonadherence (r2 = 0.05) |
| Mellins et al., 2002 | n = 128, 58% African American, mean age = 38 | Clinical Diagnostic Questionnaire (CDQ8) | self-report taken from the Adult AIDS Clinical Trials Group (AACTG9) | Cross-sectional | Presence of any psychiatric disorder (OR = 8.76) predicted missed HIV medication |
| Escobar, Venturelli, Escobar-Islas, & Hoyo-Vadillo, 2003 | n = 283, 68.6% male, mean age = 36 | State-Trait Anxiety Inventory (STAI10) | Percentage of prescriptions filled in the past 4–6 months | Cross-sectional | Medication nonadherent patients were more likely to score > 75% on the STAI state or trait anxiety scales (OR = 3.49) compared to medication adherent patients |
| Palmer et al., 2003 | n = 107 opioid-addicted PLWHA, 47% male, 63% Hispanic | Structured Clinical Interview for the DSM-IV Axis I (SCID-I13) | AACTG9 measurement of past 3 day adherence | Cross-sectional | Anxiety disorders were not significantly related to missed HIV medication (ESU) |
| Tucker et al., 2003 | n = 1910, 78% male, 32% African American | Composite International Diagnostic Interview – Short Form (CIDI-SF12) | Self-reported HIV medication adherence | Prospective | GAD (OR = 2.4) and Panic Disorder (OR = 2.0) significantly predicted nonadherence to HIV medication one year later |
| Carrieri et al., 2003 | n = 96 drug-injecting HIV infected persons, 68.8% men | Self-reported symptoms of anxiety | Self-report of adherence in the past week | Prospective | Anxiety-related somatic symptoms significantly predicted HIV medication non-adherence in the past week (OR = 2.7) six months later |
| Waldrop-Valverde & Valverde, 2005 | n = 58 HIV+ injection drug users, 25.9% homeless, 24.1% female | STAI10 | Self-reported one-day adherence | Cross-sectional | Anxiety was not significantly related to past-day adherence (ESU) |
| Schönnesson, Williams, Ross, Bratt, & Keel, 2007 | n = 193 PLWHA in Sweden, 100% Caucasian, 75% male, mean age = 43 | The Brief Symptom Inventory (BSI11) | Self-report confirmed with medical record review | Cross-sectional | Anxiety symptoms predicted sub-optimal HIV medication adherence (OR = 6.25) |
| Roux et al., 2009 | 4963 PLWHA in France | HADS7 | Self-reported adherence and virology data | Cross-sectional | Anxiety symptoms were associated with nonadherence to cART in men (OR = 1.5) but not women (ESU). |
| Campos et al., 2010 | n = 293 Brazilian PLWHA, 65.9% male | HADS7 | Semi-structured clinical interview measuring past 3 day adherence | Prospective | Severe symptoms of anxiety predicted HIV medication non-adherence (RH [Relative Hazard] = 2.28) |
| Nel & Kagee, 2013 | n = 107 HIV infected persons in South Africa, 82.2% female | Beck Anxiety Inventory (BAI14) | Self-report scale for medication adherence15 | Cross-sectional | No significant relation was found between anxiety and medication adherence (OR = 1.425) |
| Kosiba et al., 2014 | n = 131 PLWHA in treatment for opioid use | MINI International Neuropsychiatric Interview (MINI15) | Medication-Event-Monitoring-System (MEMS; AAR-DEX) | Cross-Sectional | Presence of panic disorder significantly predicted medication adherence (r2 = 0.05) |
| Substance use | |||||
| Comulada et al., 2010 | n = 936 PLWHA provided an HIV transmission prevention trial | STAI10 | Self-reported substance use | Cross-sectional and prospective | Lower rates of baseline anxiety were predictive of increasing alcohol and marijuana use over time (r2 = 0.05), as well as hard drug use over time (r2 = 0.11); prospectively, however, elevated anxiety symptoms were related to elevated alcohol and marijuana use (r2 = 0.003) and hard drug use (r2 = 0.01) |
| Ibanez, Purcell, Stall, Parsons, & Gomez, 2005 | n = 1168 HIV+ gay and bisexual men, 236 Injection Drug Users (IDU), 500 non-IDU, and 422 non-users | BSI11 | Self-reported use in the past 90-days | Cross-sectional | IDU participants reported significantly higher anxiety compared to non-IDU and non-using groups (F-test = 17.22, estimated effect size = 0.33) |
| Staton-Tindall et al., 2015 | n = 136 HIV+ females incarcerated for drug use | Global Appraisal of Individual Needs (GAIN-I16) | NM-Assist17 | Cross-sectional | Participants reporting anxiety reported higher rates of substance use (ESU) and participants reporting concurrent anxiety and substance use had significantly increased numbers of past-year male sexual partners (IRR = 1.03) |
| Garey et al., 2015 | n = 94 PLWHA, 88.3% male, 42.6% Caucasian | Inventory of Depression and Anxiety Symptoms (IDAS18) | Alcohol Use Disorders Identification Test (AUDIT19) | Cross-sectional | Hazardous alcohol use predicted higher rates of panic symptoms (r2 = 0.11) and social anxiety symptoms (r2 = 0.12) |
| Sexual risk taking behavior | |||||
| Kennedy et al., 1993 | n = 106 serodiscordant heterosexual couples | BSI | Self-reported condom use in the past month | Cross-sectional | Anxiety negatively predicted condom use among women, but not men in serodiscordant couples (ESU) |
| Kalichman, 1999 | n = 203 HIV+ men and 129 HIV+ women, mean age = 37.2, 67% African American | BSI | Self-report of past six-month anal and vaginal sexual intercourse instances, number of partners, condom use, and HIV status of partners | Cross-sectional | No differences were found between sexual low-risk and high-risk individuals in anxiety status (ESU) |
| O’Leary, Purcell, Remien, & Gomez, 2003 | n = 456 HIV+ men who have sex with men, average age = 37, 30% Caucasian | BSI | Self-report of past 90-day unprotected anal sex with | Cross-sectional | Anxiety mediated the relations between childhood sexual abuse and insertive and receptive anal intercourse (ESU) |
| Bancroft et al., 2003 | n = 589 HIV+ MSM, 87.5% white, 92% attended at least some college | STAI10 | Kinsey Institute Sexual Activity and Condom Use Questionnaire (KISACUQ; Bancroft et al., 2004); self-report of sexual partners and condom use | Cross-sectional | Higher train anxiety predicted greater likelihood of being in a high-risk sexual group (r2 = 0.10) |
| Roberts, Wechsberg, Zule, & Burroughs, 2003 | n = 355 African-American crack abusing HIV+ women | Drug Abuse Treatment for AIDS Risk Reduction, anxiety subscale (Simpson, 1990) | Risk Behavioral Assessment (RBA; Needle et al., 1995) | Cross-sectional | women with multiple sexual partners in the past month reported higher anxiety symptoms (ESU) |
| Comulada et al., 2010 | n = 936 PLWHA provided an HIV transmission prevention trial | STAI10 | Self-report of sex acts | Cross-sectional and Prospective | Cross-sectionally, increased anxiety predicted nonsignificant decreases in risk sexual acts (r2 = −0.44) and number of HIV-negative partners (r2 = −0.01); prospectively, increased anxiety predicted nonsignificant increases in risky sexual acts (r2 = 0.001) and significant increases in HIV-sexual partners (r2 = 0.005) |
| O’Cleirigh, Traeger, Mayer, Magidson, & Safren, 2013 | n = 503 HIV+ men, mean age = 41.9, 75% Caucasian | Mini Social Phobia Inventory (MINI SPIN21) and Patient Health Questionnaire (PHQ22) | Self-reported frequency of unprotected anal sex with HIV-negative or unknown partners in the past three months | Cross-sectional | Symptoms of social anxiety and panic did not significantly predict sexual risk taking behavior (ORs = 1.24, 1.02, respectively) |
| Cardoso & Malbergier, 2015 | n = 667 PLWHA in Brazil, 57.4% male, | BAI14 | Self-reported past six-month sexual behavior | Cross-sectional | Individuals reporting severe anxiety reported consistent condom use at half the rate of those indicating no anxiety (OR = 0.523) |
| Mimiaga et al., 2015 | n = 1210 sexually active men living with HIV/AIDS | PHQ22 | Self-reported past-month consistent condom use | Cross-sectional | Individuals reporting high anxiety were more likely to have had unprotected anal intercourse (OR = 1.7) and multiple unprotected anal intercourse partners (OR = 1.54) in the past six months. |
| Quality of life | |||||
| Hasanah et al., 2011 | n = 271, 57.6% male, 86.3% Malaysian ethnicity | HADS7 | Functional Assessment of Chronic Illness Therapy (FACIT27) | Cross-sectional | Anxiety significantly predicted poorer quality of life (adjusted regression coefficient = −36.41) |
| Psaros, O’Cleirigh, Bullis, Markowitz, & Safren, 2013 | n = 108 HIV+ intravenous drug users, 55.6% male, 48.1% Caucasian | BAI14 | AIDS Clinical Trials Group Short Form-21 (ACTG-SF-2128) including measurement of general health, physical functioning, role functioning, and pain | Cross-sectional | Anxiety was significantly related to general health (r2 = 0.13), physical functioning (r2 = 0.08), rule functioning (r2 = 0.14), and pain (r2 = 18) |
| Stanley, Sethuramalingam, & Sathia, 2014 | n = 309, 32.4% male | Depression Anxiety and Stress Scale (DASS23) | World Health Organization Quality of Life Questionnaire Brief version (WHOQOL-BREF24) | Cross-sectional | Results indicated that higher anxiety was significantly related to lower quality of life (r2 = 0.28) |
| Surah et al., 2013 | n = 55, 64% male, mean age = 37 | HADS7 | SF-3625 and EQ-5d26 | Cross-sectional | Higher rates of anxiety were significantly related to lower quality of life, regardless of health status (r2 = 0.21) |
| Zimpel & Fleck, 2014 | n = 308 PLWHA in Brazil, 60.4% male, 27.9% AIDS diagnosed | STAI10 | World Health Organization Quality of Life Questionnaire HIV version (WHOQOL-HIV24) | Cross-sectional | Trait anxiety significantly predicted total HIV-related quality of life (r2 = 0.03) |
| Suicidality | |||||
| Quintana-Ortiz, Gomez, Baez Feliciano, & Hunger-Mellado, 2008 | n = 714 PLWHA in Puerto Rico, 67.4% men | Self-report | Self-report | Prospective | Participants reporting episodes of anxiety “sometimes” and “frequently” reported significantly higher odds of suicide attempts one year later (OR = 7.41, 1.96, respectively) |
| Peng et al., 2010 | n = 535, mean age = 34.6 | Brief Symptom Rating Scale-5 (BSRS-529) | Two questions on lifetime suicidal thoughts/attempts | Cross-sectional | Past-week symptoms of anxiety or tension significantly predicted lifetime suicidal ideation (OR = 2.56) |
| Kinyanda, Hoskins, Nakku, Nawaz, & Patel, 2012 | n = 618 PLWHA living in Uganda, 27.3% male | MINI International Neuropsychiatric Interview MINI30 | (MINI30) | Cross-sectional | Results indicated that 0.81% (n = 5) of the sample met criteria for GAD, and 60% of those participants met criteria for current suicidality (OR = 18.9) |
| Passos, Souza, & Spessato, 2014 | n = 211, 47.9% male | HADS7 | MINI30 | Cross-sectional | Participants reporting anxiety had a significantly higher suicide risk compared to non-anxious individuals (relative risk = 2.43) |
| Cognitive impairment | |||||
| Woods et al., 2007 | n = 75 HIV+ persons, 94.7% male, 66.7% Caucasian, compared to 60 HIV− controls, 56.7% male, 56.7% Caucasian | Profile of Mood States (POMS33) | Prospective and Retrospective Memory Questionnaire (PRMQ34) | Cross-Sectional | “Tension/anxiety” and “fatigue” significantly predicted prospective memory complains among the HIV+ group (r2 values = 0.06, 0.10, respectively) |
| Au et al., 2008 | n = 90 PLWHA in Hong Kong, 82.2% male, mean age = 39.24 | STAI10 | Hong Kong List Learning Test (HKLLT31); Patients Assessment of Own Functioning Inventory (PAOF-Memory32) | Cross-Sectional | Self-reported trait anxiety did not predict total learning, 10-minute delayed recall, 30-minute delayed recall, or discrimination between stimuli (r2 values = 0.00 to 0.02, ns) but did predict patient’s assessment of own functioning (r2 = 0.11) |
| Malaspina et al., 2011 | n = 74 PLWHA | POMS33; CIDI12 | A combination of professionally-administered neurocognitive tests and self-report of cognitive complains used to measure successful cognitive ageing (SCA35) | Cross-sectional | Present of a DSM-IV defined anxiety disorder did not predict SCA (ESU), however, those endorsing SCA endorsed lower rates of tension-anxiety, and fatigue (ESU) |
| Micali, Zirilli, & Abbate, 2011 | n = 30 HIV+ men living in Sicily, mean age = 35.59 | POMS33 | Wechsler Adult Intelligence Scale (WAIS-R36) | Prospective | At 18-months post-baseline appointment, tension/anxiety significantly predicted cognitive decline (ESU) |
MINI International Neuropsychiatric Interview (MINI; Sheehan et al., 1998);
Hamilton Rating Scale for Anxiety (HAM-A; Hamilton, 1959);
Symptom Checklist 90 (SCL-90; Derogatis and Melisaratos, 1983);
General Health Questionnaire 28 (GHQ-18; Mulder, Antoni, Duivenvoorden, Kaufmann, & Goodkin, 1995);
International Classification of Diseases-9; (ICD-9, US Department of Health and Human Services, 1980);
Symptom Checklist 90-Revised (SCL-90-R; Derogatis and Melisaratos, 1983);
Hospital Anxiety and Depression Scale (HADS; Zigmond & Snaith, 1983);
Clinical Diagnostic Questionnaire (CDQ; Aidala et al., 2004);
Adult AIDS Clinical Trials Group (AACTG; Chesney et al., 2000);
State-Trait Anxiety Inventory (STAI, Spielberger, Gorsuch, & Lushene, 1970);
The Brief Symptom Inventory (BSI; Derogatis & Melisaratos, 1983);
Composite International Diagnostic Interview – Short Form (CIDI-SF; Kessler et al., 1998b);
Structured Clinical Interview for the DSM-IV Axis I (SCID-I; First, Gibbon, Spitzer, & Williams, 1995);
Beck Anxiety Inventory (BAI; Beck, Epstein, Brown, & Steer, 1988);
Self-report scale for medication adherence (Simoni et al., 2006);
Global Appraisal of Individual Needs (GAIN-I Version 5; Dennis, 1998);
NM-Assist (NIDA, 2009);
Inventory of Depression and Anxiety Symptoms (IDAS; Watson et al., 2007);
Alcohol Use Disorders Identification Test (AUDIT; Saunders, Aasland, Babor, de la Fuente & Grant, 1993);
Time Line Follow Back (TLFB; Sobell & Sobell, 1992);
Mini Social Phobia Inventory (MINI SPIN; Connor, Kobak, Churchill, Katzelnick, & Davidson, 2001);
Patient Health Questionnaire (PHQ, Spitzer, Kroenke, & Williams, 1999);
Depression Anxiety and Stress Scale (DASS; Lovibond & Lovibond, 1995);
World Health Organization Quality of Life Questionnaire Brief version (WHOQOL-BREF; Skevington, Sartoris, & Amir, 2004);
SF-36 (Brazier, Roberts, & Deverill, 2002);
EQ-5D (Gusi, Olivares, & Rajendram, 2010);
Functional Assessment of Chronic Illness Therapy (FACIT; Peterman, Cella, Mo, & McCain, 1997);
ACTG-SF-21 (Wu, Hays, Kelly, Malitz, & Bozzette, 1997);
Brief Symptom Rating Scale (BSRS-5; Lung & Lee, 2008);
MINI International Neuropsychiatric Interview (MINI; Sheehan et al., 1998);
Hong Kong List Learning Test (HKLLT; Chan & Kwok, 1999);
Patients Assessment of Own Functioning Inventory (PAOF-Memory; Chelune, Heaton, & Lehman, 1986);
Profile of Mood States (POMS; McNair, Lorr, & Droppleman, 1981);
Prospective and Retrospective Memory Questionnaire (PRMQ; Crawford et al., 2003);
Successful Cognitive Ageing (SCA; Antinori et al., 2007);
Wechsler Adult Intelligence Scale (WAIS-R; Wechsler, 1981).
5.1. Disease severity and progression (n = 6)
Two cross-sectional studies have been conducted utilizing retrospective reporting of disease severity/progression. Fincham et al. (2008) examined 456 South African’s living with HIV/AIDS and indicated that an anxiety disorder diagnosis was not associated with of CD4 T-cell count after controlling for prescription to cART. Rabkin et al. (1991) examined psychosocial stressors among 124 PLWHA both cross-sectionally and longitudinally and found no significant relation between anxiety and CD4 T-cell decline or lymphocyte subsets.
Three longitudinal studies have examined this relation to date, also indicating that there may not be a direct relation between anxiety and HIV progression. Vassend et al. (1997) examined 65 PLWHA and found that anxiety symptoms were not related to CD4 T-cell counts, even though the authors did not control for adherence to cART. However, anxiety symptoms were significantly related to subjective HIV-related somatic symptoms and coping style. Thornton et al. (2000) explored a number of personality, social, and psychological factors on CD4 T-cell count among 161 HIV+ persons recruited from a London clinic who were infected prior to January 1, 1988, and re-examined between 1993 and 1995. Results indicated that symptoms of “anxiety and insomnia” when examined concurrently with negative life events, employment, depression, and handedness, was not related to CD4 T-cell counts. Prescription to cART was entered as a control variable in this investigation. Pence, Miller, Gaynes, and Eron (2007) examined a group of 198 cART naïve HIV+ patients, discovering that the probability of mood/anxiety and substance use disorders predicted a slower rate of viral suppression and a faster rate of overall virologic failure after suppression. Alcohol and substance abuse/dependence also predicted faster overall virologic failure (Pence et al., 2007). Finally, one study conducted among 9003 HIV-infected military veterans indicated that anxiety was protective for ‘all-cause mortality.’ The authors theorized anxiety can serve to increase health behavior by promoting body vigilance (e.g., doctors’ visits, medication adherence; Nurutdinova et al., 2012). This type of perspective is consistent with other health behavior research (non-HIV/AIDS related) that has reported increased anxiety is related to more motivation to change negative health behaviors (e.g., smoking; Zvolensky et al., 2004). Given a major function of anxiety is ‘preparing an individual for dealing with potential threat’ (Barlow, 2002), anxiety states would be expected to have a positive influence (at certain levels) in terms of HIV disease severity and progression. Overall, of the six studies examining anxiety and disease severity/progression, four found no relation, one found a negative relation, and one found a positive relation. Before more confidence can be placed in the perspective that anxiety impacts HIV, further research is needed; specifically regarding independent replication and extension of the anxiety ‘protective factor’ role in HIV disease progression.
There are important caveats to this literature. First, each of the available studies examined anxiety in secondary analyses and none were oriented on anxiety disorders per se. Second, given some evidence that anxiety is related to emotion regulation and somatic complaints among PLHA (Vassend et al., 1997), it is possible that anxiety may indirectly relate to HIV disease severity/progression through other regulatory processes. Third, there is a need for more ‘fine-grained analyses’ of anxiety linkages to HIV disease progression via prospective methodologies. For example, there is a need for studies focused on specific anxiety states in relation to immune system response. Fourth, prescription or adherence to cART was not examined in some studies. Future work could examine treatment regimen in order to parse apart the unique effects of anxiety on medication adherence, as adherence to medication may be an explanatory variable in the relations between anxiety and disease progression and must be examined accordingly (see next section). Finally, the measurement of anxiety across existing studies has thus far been completed via a wide array of measures, with variable levels of psychometric performance.
5.2. HIV medication adherence (n = 13)
Catz et al. (2001) examined 113 older HIV+ persons and found that participants self-reporting medication adherence had lower levels of anxiety and somatization. Van Servellen et al. (2002) also found that among 182 PLWHA, anxiety symptoms were related to self-rated HIV medication adherence which was confirmed via medical record review (van Servellen et al., 2002). In line with these studies, Mellins et al. (2002) reported that among 128 HIV+ women, psychiatric disorders (including anxiety disorders) were associated with worse HIV self-reported medication adherence. Unfortunately, anxiety disorders were not separated from the other psychiatric disorders and therefore it is unclear how specific the findings are to anxiety versus other clinical psychiatric conditions. Escobar et al. (2003) examined 283 PLWHA and found that patients who did not fill their HIV medication prescriptions (indicating poor adherence) were more likely to index high state and/or trait anxiety. Another study (Schönnesson, Diamond, Ross, Williams, & Bratt, 2006) examined 193 HIV-infected Swedish persons and indicated that anxiety symptoms significantly predicted HIV medication self-reported nonadherence confirmed with patients’ medical records. A large cross-sectional study measuring anxiety symptoms among French HIV-infected individuals similarly indicated that anxiety symptoms predicted self-reported cART nonadherence among HIV+ men, but not women, taking anxiolytics (Roux et al., 2009). Finally, Kosiba et al. (2014) examined rates of panic disorder among 131 HIV-positive adults in treatment for opioid use, indicating that panic disorder status significantly predicted HIV medication adherence.
Tucker et al. (2003) prospectively examined 1910 HIV+ persons from the HIV Cost and Services Utilization Study. They reported that the presence of generalized anxiety disorder and panic disorder were related to self-reported HIV medication non-adherence one year later. Another prospective study examined 96 injection drug using French PLWHA, and found self-reported anxiety symptoms predicted self-reported non-adherence to HIV medications at 6-, 12-, and 18-months post-initial interview (Carrieri et al., 2003). Campos et al. (2010) prospectively measured anxiety symptoms and medication adherence via self-report, among 293 Brazilian PLWHA. Results of this study similarly indicated that symptoms of severe anxiety at the initiation of HIV medications were significant predictors of non-adherence.
A small number of studies suggest a modest association between anxiety and HIV medication adherence. For instance, Palmer et al. (2003) indicated that among 107 opioid-addicted PLWHA reporting at least one psychiatric diagnosis and at least one additional substance use disorder, anxiety disorders were not related to HIV medication non-adherence. Notably, by virtue of the study entry criteria, variability in anxiety states may have been truncated, limiting statistical power. In another cross-sectional study among 58 HIV+ homeless injection drug users, anxiety approached, but did not reach statistical significance in predicting self-reported HIV medication non-adherence (Waldrop-Valverde & Valverde, 2005). Due to the small sample size, limited statistical power is an important caveat to this study. In another secondary and cross-sectional analysis, Nel and Kagee (2013) found that among 101 South African PLWHA symptoms of anxiety did not significantly predict self-reported HIV medication adherence.
Together, of the 13 examining anxiety and HIV medication adherence, 10 suggested a relation between increased anxiety and HIV medication non-adherence. The three studies not reporting such a relation appear underpowered and may also have had a truncated range of variability. Importantly, almost all studies have utilized self-report indices of medication adherence. Future work is needed that incorporates biologic indicators of adherence (e.g., blood draw to detect presence of medication; Desmond, Moodley, Conolly, Castel, & Coovadia, 2015) in addition to self-report indices.
5.3. Substance use (n = 4)
Ibanez et al. (2005) examined a large sample (n = 1168) of HIV+ MSM split into three groups: injection drug users, non-injection drug users, and non-users. Results indicated that the injection drug using group had significantly higher rates of anxiety symptoms compared to the other groups. Results also indicated that injection drug use was significantly predictive of increased unprotected sexual acts with seronegative partners. More recently, Staton-Tindall et al. (2015) examined 136 HIV+ incarcerated substance-using women, indicating that anxiety symptoms were related to injection drug use. Additionally, women endorsing higher anxiety symptoms and higher substance use reported significantly more male sexual partners than those women with lesser anxiety symptoms. Another cross-sectional study conducted by Garey et al. (2015) found that among 94 PLWHA those reporting hazardous alcohol use reported significantly higher rates of panic and social anxiety symptoms compared to non-hazardous alcohol users.
One prospective study reported significant relations between anxiety and substance use behavior among PLWHA. In this study, Comulada et al. (2010) reported that among 936 PLWHA, lower rates of baseline trait level anxiety were related to higher rates of self-reported alcohol, marijuana, and hard drug use over time. However, when examining anxiety symptoms prospectively, increased anxiety symptoms were related to a non-significant increase in alcohol, marijuana, and drug use.
Together, available empirical data suggests a consistent relation between anxiety symptoms and substance use behavior among PLWHA, with each of the four existing studies indicating significant relations. Yet, this body of work generally involves secondary analyses of data and has not been focused on the processes that may undergird these anxiety-substance use relations. There are apt to be multiple factors that may serve to explain these relations, including biologic (e.g., stress inflammation), behavioral (e.g., coping-oriented motives for substance use), cognitive (e.g., catastrophic thinking styles), environmental (e.g., trauma), and sociocultural factors (e.g., stress, discrimination). These explanatory candidate pathways have not thus far been empirically explored.
5.4. Sexual transmission risk behavior (n = 9)
Existing work has found significant relations between anxiety and sexual transmission risk behavior among PLWHA; however, measurement techniques have impacted these findings. For instance, studies using the anxiety subscale of the BSI have not shown reliable associations with HIV sexual risk behavior. One study found no association between BSI-reported anxiety symptoms and self-reported condomless sex among independently examined groups of 203 HIV+ men and 129 HIV+ women (Kalichman, 1999). Another study found a negative association between BSI-indexed anxiety and self-reported condomless sex among HIV+ women, but not among HIV+ men when examining 106 serodiscordant couples (Kennedy et al., 1993). Other studies have found a modest relation between scores on the BSI anxiety scale and sexual transmission risk behavior. For instance, O’Leary, Purcell, Remien, and Gomez (2003) found that BSI-indexed anxiety mediated the relations between childhood sexual abuse and self-reported condomless insertive and receptive anal intercourse in the past three months among 456 HIV+ MSM.
Some cross-sectional work using other measurements of anxiety have shown more consistent relations between anxiety and sexual transmission risk behavior. For instance, Roberts, Wechsberg, Zule, and Burroughs (2003) examined 355 African American crack-abusing women and found that women with multiple sexual partners in the past month reported higher anxiety symptoms. Cardoso and Malbergier (2015) examined 667 PLWHA in Brazil and found that individuals reporting severe anxiety reported condom use at half the rate of those with no anxiety symptoms. Another study by Mimiaga et al. (2015) found that among 1210 sexually men living with HIV/AIDS, anxiety symptoms predicted self-reported past 6-month sexual behavior of condomless anal intercourse and more than two anal intercourse partners.
However, other studies have not found statistical associations between anxiety symptoms and sexual transmission risk behavior. For instance, O’Cleirigh, Traeger, Mayer, Magidson, and Safren (2013) examined the effects of social anxiety symptoms and panic symptoms in relation to self-reported frequency of condomless anal sex with HIV-negative or unknown partners in the past three months among 503 HIV+ gay and bisexual men. Results indicated that social anxiety and panic symptoms did not significantly predict sexual transmission risk behavior, although the mean scores were in the expected direction. In another study, Comulada et al. (2010) found that among 936 PLWHA, lower rates of baseline anxiety were related to lower rates of self-reported risky sex acts over time when examined cross-sectionally. However, when examining anxiety symptoms prospectively, increases in anxiety produced a non-significant increase in risky sexual acts and HIV-negative sexual partners.
In summary, there is a burgeoning amount of work on anxiety and sexual risk taking among PLWHA. Of the nine studies examining these relations, five report a direct relation between anxiety symptoms and higher relative risk of sexual risk taking behavior, while two report no relations, and two more report negative relations. This work has not explored anxiety disorders per se, generally employing symptom indices for general (e.g. physical sensations) or specific types of anxiety (e.g., social anxiety). There also is little understanding of the mechanisms underlying anxiety-sexual risk taking behavior.
5.5. Quality of life (QuoL; n = 5)
At present, there is limited work examining the effects of anxiety on QuoL among PLWHA. However, available work suggests that there may be a clinically significant relation. For instance, Stanley, Sethuramalingam, and Sathia (2014) indicated via cross-sectional analyses that anxiety was related to poorer QuoL among 309 HIV-positive adults in India. Other international studies have found similar results. Among 55 HIV+ intravenous drug using participants living in Ireland, anxiety predicted lower quality of life irrespective of physical health (Surah et al., 2013). In another study, Hasanah et al. (2011) cross-sectionally examined the association of anxiety symptoms on QuoL among 271 HIV infected adults in Malaysia. Results indicated that anxiety symptoms significantly predicted a lower QuoL. Zimpel and Fleck (2014) found similar results when examining a cross-sectional sample of 308 PLWHA in Brazil wherein trait anxiety significantly predicted lower quality of life. A more recent study conducted in the US utilizing cross-sectional data from a larger trial indicated that anxiety symptoms predicted physical functioning and role functioning among a sample of 108 HIV+ intravenous drug uses (Psaros, O’Cleirigh, Bullis, Markowitz, & Safren, 2013).
All available studies suggest that anxiety symptoms are related to a lower QuoL among PLWHA (see Table 5). However, there are notable limitations to this body of work. First, each of the available studies examined the relationship between anxiety and QuoL via secondary analyses and cross-sectional research designs. The lack of prospective research examining this relationship represents a global need for future work on this topic, particularly when examining this relation as an a priori focus. Second, no research has been oriented on anxiety disorders per se, indicating a need for studies expressly oriented on anxiety psychopathology. Finally, the measurement of both anxiety and QuoL across these studies has been completed via a wide array of measures, making direct comparisons across studies challenging. Finally, given the consistent relation between anxiety symptoms and QuoL, there is a need to better understand the mechanisms underlying this association.
5.6. Suicidal thoughts, behaviors, and history (n = 4)
Some work suggests that suicide risk is significantly higher among PLWHA than among those with other chronic diseases as well as the general population (Keiser et al., 2010; Robertson, Parsons, Van Der Horst, & Hall, 2006). Existing cross-sectional work indicates a potential relationship between anxiety and suicidal thoughts, behaviors, and attempt history among PLWHA. For instance, one study examined 535 Taiwanese inmates (Peng et al., 2010) and indicated that psychological distress (including symptoms of anxiety or tension) predicted serious thoughts of suicide. Another cross-sectional study conducted by researchers in Uganda indicated that GAD was related to suicidal thoughts, plans, preparation, and previous attempts (coded together as a measure of overall suicidality) (Kinyanda, Hoskins, Nakku, Nawaz, & Patel, 2012). Passos, Souza, and Spessato (2014) indicated via cross-sectional analysis that among 211 HIV+ Brazilians, anxiety predicted suicide risk after controlling for a number of theoretically-relevant variables including gender, age, unemployment, depression, and substance use. To date, one study has prospectively examined the relationship between anxiety and suicidality among PLWHA. This study was conducted over a four-year period and included 714 HIV+ persons from Puerto Rico (Quintana-Ortiz, Gomez, Baez Feliciano, & Hunter-Mellado, 2008). Results indicated that self-reported “episodes of anxiety” were significantly related to increased self-reported suicide attempts at 1-, 2-, 3-, and 4-year follow-up assessments.
Together, there appears to be a consistent relation between anxiety and suicidal thoughts, behaviors, and history among PLWHA, as indexed by each of the four studies examining these relations. However, available studies examined the relationship between anxiety and suicide risk via secondary analysis, and three of the four studies utilized a cross-sectional design. Therefore, future prospective modeling of the role of anxiety symptoms and disorders in suicide risk among PLWHA is a key area for future study.
5.7. Cognitive impairment (n = 4)
Approximately 30–50% of PLWHA evidence neurocognitive impairment (Heaton et al., 2010), which is most commonly observed in the domains of executive functions and memory. Anxiety symptoms have been shown to affect cognitive impairment in the general population (Yates, Clare, & Woods, 2013); however, this relation has been understudied in the HIV+ population and there are mixed findings in the literature. For instance, one study examining secondary data found that anxiety did not predict performance on a test of memory among 90 HIV-infected individuals living in Hong Kong, although it did significantly predict self-reported cognitive symptoms (Au et al., 2008). Another study examining secondary data found that among 75 PLWHA tension/anxiety and fatigue did significantly predict increased frequency of prospective memory complaints (Woods et al., 2007). Malaspina et al. (2011) also examined factors that predicted successful cognitive ageing (SCA; a combination of neurocognitive tests and self-report of cognitive complaints) among 74 PLWHA and found an association with severity of anxiety symptoms but not anxiety disorder diagnoses.
To date, one prospective study has examined anxiety and its effect on cognitive decline among PLWHA longitudinally. In this study, Micali, Zirilli, and Abbate (2011) administered the Wechsler Adult Intelligence Scale (WAIS-R) and measures of anxiety symptoms to 30 PLWHA at a baseline appointment as well as 6- and 18-month followups. Results indicated that cognitive performance was significantly lower at 18-month follow-up for those with increased anxiety.
The literature examining the effect of HIV and anxiety in relation to cognitive impairment among PLWHA is growing, but still small in scope. Three of the four available studies examined this relationship via secondary analyses and using a cross-sectional design and there is little knowledge as to the mechanisms underlying anxiety-cognitive decline relations. Moreover, all studies have used self-report of cognitive complains, rather than comprehensive batteries of performance-based neurocognitive tasks, which may more accurately assess such impairment.
6. Transdiagnostic individual difference factors
To date, a number of transdiagnostic processes have been studied in the context of HIV/AIDS and anxiety psychopathology. These include anxiety sensitivity, distress tolerance, emotion dysregulation, avoidant coping, and to a lesser extent, personality factors. In this section, we review extant work in these domains.
6.1. Anxiety sensitivity
The anxiety sensitivity construct, defined as the extent to which individuals believe anxiety and anxiety-related sensations (e.g., racing heart) have harmful personal consequences (McNally, 2002; Reiss & McNally, 1985), is a relatively stable, but malleable, factor. The global anxiety sensitivity construct encompasses lower-order fears of physical, mental, and publicly observable experiences (Zinbarg, Barlow, & Brown, 1997). Theoretically, individuals higher in anxiety sensitivity are more likely to be frightened of harmless heart palpitations because they believe these sensations will lead to cardiac arrest or other feared outcomes, whereas individuals lower in anxiety sensitivity do not fear these sensations because they believe them to be benign. Empirically, anxiety sensitivity is distinguishable from the tendency to experience more frequent anxiety symptoms (trait anxiety) and other negative affect propensity variables (e.g., Rapee & Medoro, 1994; Zvolensky, Kotov, Antipova, & Schmidt, 2003).
There is strong and consistent evidence, across cultures and distinct national groups that anxiety sensitivity predisposes individuals to the development and maintenance of anxiety and mood psychopathology (Hayward, Killen, Kraemer, & Taylor, 2000; Li & Zinbarg, 2007; Maller & Reiss, 1992; Marshall, Miles, & Stewart, 2010; Schmidt et al., 2010; Schmidt, Lerew, & Jackson, 1999; Schmidt, Zvolensky, & Maner, 2006a). Such effects are not better explained by the broad-based tendency to experience negative affect or trait anxiety (Taylor, 1999).
To date, five studies have examined anxiety sensitivity on anxiety-related processes among PLWHA (please see Table 6). For instance, in a cross-sectional examination, Gonzalez, Zvolensky, Solomon, and Miller (2010) found that among 51 PLWHA (74.5% male, mean age = 45.53), anxiety sensitivity predicted overall anxiety and depression symptoms. Specifically, results indicated that global anxiety sensitivity predicted somatization, anxiety, and depression even when controlling for negative affectivity. Additionally, when examining the subscales independently, anxiety sensitivity physical concerns predicted somatization and anxiety sensitivity mental concerns significantly predicted anxiety symptoms. In a subsequent study, Schmidt, Richey, and Fitzpatrick, (2006b) examined anxiety sensitivity in relation to a wide array of aversive internal states among 164 PLWHA (82.9% male, 40.9% Caucasian). Results indicated that global anxiety sensitivity was significantly predictive of anxious arousal, bodily vigilance, interoceptive fear, and showed a trend relationship with HIV symptom distress. In a separate investigation utilizing the same sample of 164 PLWHA, Schmidt et al. (2006b) indicated that anxiety sensitivity independently predicted panic, social anxiety, and depression. Results indicated small to moderate effect sizes for anxiety sensitivity in relation to these outcome variables. Results also indicated that higher anxiety sensitivity, combined with high self-reported HIV symptom distress, predicted the greatest levels of panic, and social anxiety.
Table 6.
Transdiagnostic factors and anxiety (ordered chronologically by sub-category).
| Authors | Study characteristics | Measure of transdiagnostic process | Outcome measured | Design | Main finding |
|---|---|---|---|---|---|
| Anxiety sensitivity | |||||
| Gonalez, Zvolensky, Solomon, & Miller, 2010 | n = 51 PLWHA, 74.5% male, mean age = 45.53 | Anxiety Sensitivity Index-3 (ASI-31) | Symptom Checklist-90-Revised (SCL-90-R2) | Cross-sectional | Global anxiety sensitivity associated with somatization (AR = 0.13), anxiety (AR2 = 0.11), and depression (AR2 = 0.11); anxiety sensitivity physical concerns predicted somatization (p = 0.52), and anxiety sensitivity mental concerns significantly predicted anxiety (p = 0.29) |
| Gonzalez, Zvolensky, Grover and Parent, 2012a | n = 164 PLWHA, 82.9% male, 40.9% Caucasian | ASI-31 | Mood and Anxiety Symptoms Questionnaire (MASQ3) | Cross-sectional | Global anxiety sensitivity associated with anxious arousal (p = 0.34), bodily vigilance (p = 0.30), interoceptive fear (p = 0.24), and showed a trend relationship with HIV symptom distress (p = 0.15, p = 0.07) |
| Gonzalez, Zvolensky, Parent, et al., 2012b | n = 164 PLWHA, 82.9% male, 40.9% Caucasian | ASI-31 | Inventory of Depression and Anxiety Symptoms (IDAS4) | Cross-sectional | Global anxiety sensitivity associated with panic (r2 = 0.18), social anxiety (r2 = 0.27), and depression (r2 = 0.23) |
| Capron, Gonzalez, Parent, Zvolensky, & Schmidt, 2012 | n = 164 PLWHA, 82.9% male, 40.9% Caucasian | ASI-31 | Suicidality via the IDAS4 | Cross-sectional | Global anxiety sensitivity was not associated with suicidality among PLWHA (p = 0.05), but when examining the anxiety sensitivity subscales concurrently, physical and social concerns showed non-significant negative relations (p = −0.25 and p = −0.16 respectively), while cognitive concerns showed significant positive predictive value (p = 46) |
| Leyro, Vujanovic & Bonn-Miller, 2015 | n = 139 PLWHA, 75.5% male, average age = 48.2, 42% African American | ASI-31 | Barriers to cART Adherence Questionairre6 | Cross-sectional | Global anxiety sensitivity was shown to be significantly related to only HIV symptom severity, (p = 0.35) when examined concurrently with the other variables |
| Distress tolerance | |||||
| Brandt, Zvolensky, & Bonn-Miller, 2013 | n = 176 PLWHA, 78.4% male, 38.6% African American | Distress Tolerance Scale (DTS7) | IDAS4 | Cross-sectional | Distress tolerance was significantly negatively related to panic and social anxiety symptoms (r2 values = 12) |
| Emotion dysregulation | |||||
| Brandt, Zvolensky, & Bonn-Miller, 2013 | n = 176 PLWHA, 78.4% male, 38.6% African American | Difficulties in Emotion Regulation Scale (DERS9) | IDAS4 | Cross-sectional | Emotion Dysregulation was significantly related to panic and social anxiety symptoms (r2 = 0.19, 0.30, respectively). Emotion Dysregulation also mediated the relations between Distress Tolerance and panic and social anxiety symptoms |
| Avoidant coping | |||||
| Lutgendorf et al., 1997 | n = 39 HIV+ men, mean age = 36.75 years, 62.5% Caucasian | COPE10 | POMS11 | Prospective | Changes in denial coping during a coping intervention did not predict anxiety symptoms (r2 = 0.03) though increases in active coping were significantly related to decreased anxiety (r2 = 0.10) |
| Conley, Taylor, Kemeny, Cole, & Visscher, 1999 | n = 224 HIV+ men, mean age = 37.4 years, 91% Caucasian | Participants were asked if they had ever received an HIV test, and subsequently returned for the results. Those who were tested but did not receive results were termed avoidant of HIV serostatus | Two questions indexing concerns about developing AIDS; two questions indexing each individual’s perceived changes of getting HIV; POMS11 indexing depression. Anger, and anxiety as “mood disturbance” | Prospective | Those who avoided learning their HIV serostatus reported significantly higher rates of thought intrusions about AIDS, worry that physical symptoms signaled the onset of AIDS, and having a higher risk of developing AIDS (ESU) |
| Song & Ingram, 2002 | n = 116 African American’s living with HIV, 61.2% male, mean age = 37.9 | Coping Orientation to Problems Experienced (COPE10) | Profile of Mood States (POMS11) | Cross-sectional | Disengagement and Denial coping was significantly positively related to anxiety symptoms (r2 = 0.18) |
| Chan et al., 2006 | n = 118 PLWHA in Hong Kong | Responses to HIV Scale (RHS12) | Hospital Anxiety and Depression Scale (HADS13) | Cross-sectional | Avoidant coping was significantly positively related to anxiety symptoms (r2 = 0.10) |
| Kraaij et al., 2008 | n = 104 HIV+ homosexual and bisexual men, mean age = 50 years, 97% of Dutch nationality | Cognitive Emotion Regulation Questionnaire (CERQ14), COPE10 | HADS13 | Cross-sectional | Coping strategies related to avoidant coping including other-blame (r2 = 0.19) and substance use (r2 = 0.13) were not significantly related to anxiety symptoms. Active coping was also not related to anxiety symptoms (r2 = −0.04) |
| Gonzalez, Solomon, Zvolensky, & Miller, 2009 | n = 98 PLWHA, 68.4% male, mean age = 44.97, 85.7% Caucasian | The Response to Stress Questionnaire-HIV/AIDS Stigma (REQ15) | Beck Anxiety Inventory (BAI16) | Cross-sectional | Disengagement coping was significantly positively related to anxiety symptoms (r2 = 0.37) |
| Varni, Miller, McCuin, & Solomon, 2012 | n = 203 PLWHA, mean age = 43.18 | REQ15 | SCL-90-R2 | Cross-sectional | Enacted stigma, Concerns with public attitudes, Negative self-image, and disclosure concerns all interacted with disengagement (avoidant) coping to predict greater anxiety (r2 values = 0.24, 0.18, 0.17, and 0.29, respectively) |
| Hansen et al., 2013 | n = 307 older (age > 50) PLWHA | Ways of Coping Questionnaire (WCQ17); Coping with Illness Inventory (CWI18) and additional items measuring coping created for this study | BAI16 | Cross-sectional | Items from all coping measures used in this study were combined to create an index of avoidant coping. Avoidant coping was significantly related to anxiety symptoms (r2 = 0.14) |
| Personality | |||||
| Lockenhoff, Ironson, O’ Cleirigh, and Costa, 2009 | n = 112 PLWHA, mean age = 38.1, 67% female, 35% African American | Revised NEO Personality Inventory (NEO-PI-R17) | State Anxiety Scale (SCA18) | Cross-sectional | Neuroticism was significantly positively associated with anxiety (r2 = 0.14) whereas openness to experience (r2 = 0.06) and conscientiousness (r2 = 0.08) were significantly negatively associated with anxiety |
Anxiety Sensitivity Index-3 (ASI-3; Taylor et al., 2007);
Symptom Checklist-90-Revised (SCL-90-R; Derogatis, 1992);
Mood and Anxiety Symptoms Questionnaire (MASQ; Watson et al., 1995);
Inventory of Depression and Anxiety Symptoms (IDAS; Watson et al., 2007);
Posttraumatic Diagnostic Scale (PDS; Foa, 1995);
Barriers to cART Adherence Questionnaire (Chesney et al., 2000);
Distress Tolerance Scale (DTS; Simons & Gaher, 2005);
Discomfort Intolerance Scale (DIS; Schmidt et al., 2006b);
Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, 2004);
Coping Orientation to Problems Experienced (COPE; Carver, Scheier, & Weintraub, 1989);
Profile of Mood States (POMS; McNair, Lorr, & Droppleman, 1971);
Responses to HIV Scale (RHS; Reed, Kemeny, Taylor, Wang, & Visscher, 1994);
Hospital Anxiety and Depression Scale (HADS; Zigmond & Snaith, 1983);
Cognitive Emotion Regulation Questionnaire (CERQ; Garnefski, Kraaij, & Spinhoven, 2002);
The Response to Stress Questionnaire-HIV/AIDS Stigma (REQ; Connor-Smith, Compas, Wadsworth, Thomsen, & Saltzman, 2000).
Beck Anxiety Inventory (BAI; Beck & Steer, 1993);
State Anxiety Scale (SA; Spielberger, Gorsuch, & Lushene, 1970).
Other work has implicated anxiety sensitivity in a number of other clinically-significant outcomes among PLWHA. For example, one investigation examined anxiety sensitivity in relation to suicidality among 164 PLWHA (82.9% male, 40.9% Caucasian; Capron et al., 2012). Results indicated that anxiety sensitivity cognitive concerns predicted suicidality incrementally above and beyond the effects of demographic and health-related covariates and negative affectivity. The most recent study, conducted by Leyro et al. (2015), cross-sectionally examined the predictive value of three transdiagnostic risk variables (anxiety sensitivity, emotion dysregulation, and distress tolerance) in predicting HIV symptom severity, barriers to HIV medication adherence, and viral load among 139 PLWHA (75.5% male, average age = 48.2, 42% African American). In this investigation anxiety sensitivity was shown to be significantly related to HIV symptom severity when examined concurrently with these other variables.
Together, available work from cross-sectional studies provides empirical evidence that anxiety sensitivity is related to anxiety and related negative mood symptoms as well as HIV symptoms and poorer medication adherence among PLWHA. This work is limited in that it is cross-sectional in nature, yet in most instances the effect of anxiety sensitivity appears to be clinically robust in that it is incremental, explaining variance above and beyond that accounted for by negative affectivity and other factors (see Table 6).
6.2. Distress tolerance
There have been two broad, conceptually distinct forms of distress tolerance characterized by the existing literature (Leyro, Zvolensky, & Bernstein, 2010): (a) the perceived capacity to withstand negative emotional and/or other aversive states (e.g., physical discomfort), and (b) the objective behavioral act of withstanding distressing internal states elicited by some type of stressor. Although nested conceptually within a broader network of risk and protective processes, distress tolerance is theorized to be related to, though conceptually distinct from, other variables (e.g., avoidant coping, emotion regulation, experiential avoidance; Leyro et al., 2010). Individuals with lower distress tolerance are prone to maladaptively respond to distress and distress-eliciting contexts, a common manifestation of which involves avoidance of negative emotions and/or related aversive states.
To date, only one study has examined cross-sectional associations between distress tolerance and anxiety among PLWHA. In this study, conducted by Brandt, Zvolensky, and Bonn-Miller (2013), the mediational effects of emotion regulation on the relations between perceived distress tolerance and anxiety and depressive symptoms among 176 PLWHA were examined. Results indicated that perceived distress tolerance significantly predicted depression symptoms, panic symptoms, and social anxiety symptoms, as measured by the IDAS. Results also indicated that emotion dysregulation mediated these findings; a topic area we return to in the subsequent section. Although existing work is limited in that it is cross-sectional in nature, the effect of distress tolerance appears to be clinically robust in that it is incremental, explaining variance above and beyond that accounted for by related secondary factors (see Table 6).
6.3. Emotion dysregulation
Contemporary perspectives denote that affect dysregulation reflects (1) difficulties in the self-regulation of affective states and (2) difficulties in self-control over affect-driven behaviors (Carver, Lawrence, & Scheier, 1996; Gross, 1998).
To date, only one study has explicitly examined the impact of emotion dysregulation on anxiety among PLHWA (see Table 6). In this study, Brandt, Gonzalez, et al. (2013) examined cross-sectional data from 176 PLWHA. Results indicated that emotion dysregulation explained the relations between distress tolerance and depressive symptoms, panic symptoms, and social anxiety symptoms. These findings were evident after adjusting for a number of covariates, including gender, ethnicity, education level, CD4 T-Cell counts, and cannabis use. Future work is needed to prospectively examine emotion dysregulation in relation to anxiety symptoms and disorders among PLWHA.
6.4. Avoidant coping
Coping processes are a subordinate category within the construct of affect regulation (Compas, Connor-Smith, Saltzman, Thomsen, & Wadsworth, 2001). Within this model, coping reflects conscious, voluntary attempts to manage internal or external stressors that an individual perceives as exceeding psychological-based resources. Importantly, such a definition excludes involuntary processes (e.g., rumination).
To date, eight cross-sectional studies have examined the effects of avoidant coping on anxiety among PLWHA. Song and Ingram (2002) examined 116 African Americans living with HIV. In this study, disengagement/denial coping significantly mediated the relations between multiple unsupportive social interactions (e.g., disconnecting, insensitivity) and anxiety symptoms. Another study examined relations between coping strategies and psychological distress among 118 PLWHA in Hong Kong (Chan et al., 2006). Results indicated that avoidant coping was significantly related to increased anxiety symptoms.
Another study (Kraaij et al., 2008) examined cognitive coping strategies and behavioral coping strategies in relation to anxiety symptoms among 104 HIV+ homosexual and bisexual men. Results indicated that avoidant coping was not significantly related to anxiety symptoms. Gonzalez, Solomon, Zvolensky, and Miller (2009) reported that disengagement coping significantly predicted anxiety symptoms among 98 PLWHA. Another study examined coping among 307 older (age > 50) adults living with HIV/AIDS (Hansen et al., 2013). Results indicated that avoidant coping significantly predicted anxiety symptoms. Finally, Varni, Miller, McCuin, and Solomon (2012) found that among 203 PLWHA, HIV stigma and disengagement (avoidant) coping significantly predicted anxiety symptoms.
There has been only one prospective study examining the effects of avoidant coping on anxiety among PLWHA. In this investigation, Conley, Taylor, Kemeny, Cole, and Visscher (1999) examined the psychological sequela of avoiding HIV-serostatus information among 224 men living with HIV/AIDS. Results indicated that those who avoided learning about their HIV status by not returning to receive results from an HIV test subsequently self-reported significantly higher rates of thought intrusions about developing AIDS as well as worries that physical symptoms they were having signaled the onset of AIDS compared to those who did receive their results.
Additionally, a growing corpus of work has begun to deliver interventions aimed at changing coping styles among PLWHA with the goal of reducing anxiety (and other negative emotional states). In one study, Lutgendorf et al. (1997) evaluated a cognitive coping skills intervention among 21 homosexual HIV+ men compared to a waitlist control group of 18 homosexual HIV+ men. Those receiving the active intervention reported no changes in denial coping and cross-sectional analyses did not indicate a relation between denial coping and anxiety. However, participants reported increased active coping reported significant decreases in anxiety symptoms.
Together, extant work suggests a relatively consistent relation between avoidant coping and anxiety symptoms among PLWHA. However, this work is limited as it typically has been a secondary analysis and researchers do not always clearly define coping processes in relation to specific stimuli. Theoretically, different stressors may require different coping strategies, and therefore, coping attempts may be differentially effective as a function of stressor type. Without a greater degree of precision, it is impossible to better understand the specific effects of coping in terms of various anxiety-related states among PLWHA (Compas et al., 2001).
6.5. Personality
Personality factors, reflecting individual differences in enduring psychological traits, have been the subject of sustained scholarly attention in terms of their role in psychopathology. Indeed, specific personality traits, such as neuroticism, are often associated with anxiety and depressive disorders (Clark, 2005).
Surprisingly, only one study has explicitly examined personality factors in relation to anxiety symptoms among PLWHA. In this study, Lockenhoff, Ironson, O’Cleirigh, and Costa (2009) examined personality traits and anxiety symptoms. Results indicated that neuroticism was significantly related to anxiety symptoms whereas openness and conscientiousness were significantly negatively related to anxiety symptoms among 112 PLWHA. These data suggest that there indeed may be merit to further exploration of personality dimensions in terms of anxiety psychopathology among PLWHA.
6.6. Summary
There is growing literature on transdiagnostic processes in relation to anxiety among PLWHA. Although there appears to be significant covariation between many of these transdiagnostic factors and anxiety among PLWHA, causal evidence for these processes as underlying mechanisms of anxiety and its disorders is lacking. Additional research conducted in naturalistic settings (perhaps using ecological momentary assessment), is necessary to establish the temporal precedence of these processes and the expression of anxiety symptoms and disorders. Yet, inspection of available work suggests that there is merit to a number of transdiagnostic processes in terms of better understanding anxiety among PLWHA.
7. A heuristic integrative model
Extant work suggests HIV/AIDS and anxiety symptoms and disorders often co-occur, indicating that perhaps both conditions share common underlying vulnerabilities. It is possible that the experience of living with HIV, and distressing HIV-related symptoms in particular, may represent a common pathophysiology between HIV/AIDS and anxiety symptoms. Drawing from available work, there is good reason to hypothesize that the experience of HIV/AIDS and anxiety vulnerability maintain bi-directional influences on one another (see Fig. 6). We posit that such affective disturbances can influence HIV/AIDS and vice versa via a number of different mechanisms, including biologic (e.g., chronic inflammation), behavioral (e.g., health behaviors), cognitive (e.g., distorted thinking styles), and social (e.g., stigma/discrimination) factors.
Fig. 6.
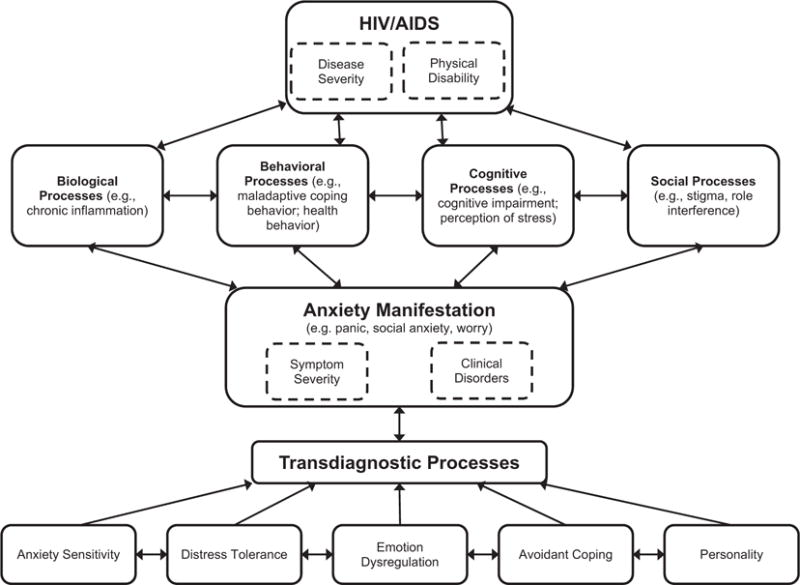
Model of HIV and anxiety relation.
To illustrate, it is generally accepted that biological stress pathways (e.g., Hypothalamic-Pituitary-Adrenal axis and Sympathetic-Adrenal-Medullary axis) are disrupted by HIV infection, and chronic anxiety, which uses these same pathways, may contribute to chronic inflammation and elevated anxiety symptoms over large periods of time (Danese et al., 2011; Leserman, 2003). Likewise, HIV/AIDS may be related to behavioral health practices, such as smoking, alcohol or drug use, or poor sleep hygiene that exacerbates or maintains anxiety symptoms (Niaura et al., 2000). Additionally, exaggerated cognitive biases for threat (e.g., exaggerated focus on bodily sensations) represented in interpretative, attention, or memory realms may contribute to elevations in anxiety symptoms (Schoth & Liossi, 2010). And finally, HIV/AIDS may be related to social factors such as stigma and discrimination (Bunn, Solomon, Miller, & Forehand, 2007), which are often linked to more severe anxiety symptoms (Okazaki, 2009). Factors such as disease severity or degree of life impairment from the illness may be important in understanding the degree or strength of the relation to mechanistic factors and expression of anxiety symptoms. Likewise, the manifestation of anxiety symptoms and disorders have well-established relations to many of the same biologic (e.g., chronic inflammation), behavioral (e.g., health behaviors), cognitive (e.g., distorted thinking styles), and social (e.g., discrimination) factors. Therefore, these mechanisms may serve to undergird the co-occurrence of HIV/AIDS and anxiety symptoms and disorders.
In the case of anxiety symptoms and disorders, it is also noteworthy that many of the manifestations of these appear to be driven by specific transdiagnostic factors, such as anxiety sensitivity, distress tolerance, emotion dysregulation, and personality factors (e.g., neuroticism). There are naturally many other putative transdiagnostic factors that could be related to the HIV/AIDS and anxiety co-occurrence, including genetic, pathophysiologic (e.g., heart rate variability), among other vulnerabilities. Future work is needed to not only isolate other transdiagnostic processes for anxiety in the context of HIV/AIDS, but also to focus a greater proportion of scientific efforts to programmatic work on such factors in this population. This approach is apt to facilitate more focused, theoretically-driven research efforts that can explicate how specific manifestations of anxiety related to specific features of HIV/AIDS and its clinical correlates. In this context, it may be especially valuable to characterize how individual transdiagnostic factors relate to one another in the context of anxiety symptoms and disorders, as there may well be synergistic or interactive types of effects.
Overall, the heuristic model predicts that the associations that exist between HIV/AIDS and anxiety symptoms and disorders are reciprocal and dynamic. Moreover, this model predicts that moderators (variables that influence the association between HIV/AIDS and anxiety symptoms and disorders) and mediators (variables that account for the relations between the two conditions) serve to qualify and explicate the nature of the observed co-occurrence. There is currently little work on moderators and mediators in HIV/AIDS and anxiety relations, but they represent a next “critical step” for the field. Although the model offered here is purposively general, it is presumed that there is, in fact, specificity between HIV/AIDS, moderators, mediators, and various forms of anxiety. That is, a specific aspect of HIV/AIDS (e.g., symptom severity) is linked to a particular type of problem (e.g., panic attacks) via a specified mediating process (e.g., impaired control over cognitive processes) in the context of certain moderating variables (e.g., high trait anxiety). The core idea being that the underlying mechanism between HIV/AIDS and anxiety in this hypothetical example may be quite different from that explaining other HIV/AIDS-anxiety relations.
8. Future research and clinical implications
We conclude our review with an abbreviated set of recommendations for advancing research and practice in the area of anxiety and HIV/AIDS comorbidity.
8.1. Prospective studies
Existing research is lacking in prospective studies examining the temporal order of HIV/anxiety relations, and subsequent effects of and on related processes. Indeed, the vast majority of existing studies are cross-sectional in design. Therefore, one clear recommendation for the future is to test prospective associations between anxiety factors and theoretically-relevant HIV/AIDS processes and outcomes and vice versa; these tests would be particularly informative when evaluated in relation to a broad sample of PLWHA. Studies examining long-term effects of HIV/anxiety at multiple time points may help to better understand HIV/anxiety associations and consequential outcomes. Importantly, these prospective tests are needed to clarify the temporal precedence of HIV/AIDS and anxiety onset and vice versa. Future studies would also benefit from examining trajectories of HIV symptoms and anxiety in greater resolution, especially when adjusting for the influence of potential third variables.
8.2. Experimental studies
Experimental models for testing anxiety as a factor that affects the experience of HIV/AIDS may be particularly innovative and offer a number of advantages, including: standardization of anxiety stimuli; reliable and valid measurement of sensory, cognitive, and affective aspects of the anxiety experience; systematic assessment and manipulation of hypothesized mediators/moderators; and the ability to demonstrate casual relations. Laboratory-based paradigms have the potential to uncover important theory-based mechanisms that may inform the development of targeted interventions for persons with comorbid HIV/AIDS and anxiety disorders. Future research examining the effects of anxiety on HIV/AIDS processes, such as symptom severity, could incorporate testing of anxiety modalities (e.g., social threat, physical threat) that are analogues to clinical anxiety conditions (e.g., social anxiety disorder, panic disorder) and be conducted across different subpopulations of HIV/AIDS samples, including those with preexisting anxiety conditions. Additionally, experimental tests that manipulate the acute impact of specific anxiety processes (e.g., anxiety sensitivity, perceived control) in the context of HIV/AIDS-relevant stimuli also would an important next step in further elucidating the interplay between these conditions.
8.3. Fear disorders vs. anxious-misery disorders
There have been multiple attempts at understanding psychopathology via underlying core traits as opposed to its’ manifestation as distinct disorders. One of these models – first discussed by Krueger (1999) – hypothesizes that anxiety and mood disorders can be conceptualized in the broad category of “internalizing disorders” and then divided into two subgroups: “anxious-misery” including MDD, dysthymia, and GAD, and “Fear” including social phobia, simple phobia, agoraphobia, and panic disorder. Because previous work has reviewed the depression literature among PLHIV, we chose to focus exclusively on anxiety disorders in the current review. However, future research may find added utility in examining psychopathology among PLWHA using this transdiagnostic theoretical framework.
8.4. Moderating and mediating processes
There are clear relations between HIV and anxiety-related processes, however, the examination of variables that may affect and/or explain this relation (e.g. moderators and mediators) is lacking. The field is now poised to move from tests of main effects to tests of moderating and mediating processes. A broader understanding of so-called “third variables” would allow researchers to further refine their understanding of this co-occurrence. Contextual variables (e.g., environmental variables such as socioeconomic status and race/ethnicity) that are related to both HIV/AIDS and anxiety may be at least partially responsible for the observed association. Likewise, there are numerous biopsychosocial factors that may contribute to the observed interrelationships between HIV/AIDS and anxiety (i.e., confounding or third variables). Future research should employ a strategic approach to the investigation of factors common to both HIV/AIDS and anxiety. Identifying the specific “third variables” in the HIV/AIDS-anxiety association provides critically important information that can be used for highly pragmatic reasons, such as guiding intervention planning.
8.5. Methodological advancements
There has been an emphasis on only a limited number of methodological approaches to studying HIV/AIDS-anxiety associations. For example, there have been no laboratory-based studies of these associations or studies using time sampling techniques. Without broadening the methodological approaches used in this area of study to tap theoretically relevant processes, it will be difficult to document the nature of these processes across and between levels of analysis (e.g., cognitive and physiological systems); an approach consistent with RDoC initiatives. Furthermore, the studies reviewed often relied on self-report for obtaining an anxiety diagnosis and to assess anxiety symptoms. Multimethod assessment techniques for both HIV/AIDS and anxiety assessment will decrease any potential problems due to shared method variance as well as lend greater validity to clinical diagnoses.
8.6. Intervention programming
Despite a relatively large corpus of work examining the effect of anxiety on HIV/AIDS, there have been few studies that have aimed at developing novel treatments specifically for this population. Although researchers have attempted to understand the utility of integrating cognitive-behavioral treatment of depression into HIV treatment (for a review, see Spies, Asmal, & Seedat, 2013), no research has directly targeted anxiety vulnerability factors in HIV/AIDS care (i.e., medication adherence). At the same time, there is little work addressing HIV in the persons seeking care for anxiety disorders. Given consistent empirical evidence of bi-directional associations between these behavioral problems, it is important to develop specialized treatments, as broad-based interventions may not target the affective vulnerability processes apparent in this population.
8.7. HIV/AIDS practitioner education
It remains unclear the extent to which HIV service providers are aware that anxiety symptoms and disorders affect HIV/AIDS severity and clinical correlates. In addition, it is unknown how frequently the HIV service providers give information to their patients about such affective disturbances. It is unlikely that patients are aware of the specific problems of anxiety with HIV/AIDS beyond the general understanding of existential experiences with ‘stress.’ There is clear need to develop empirical knowledge and understanding about the extent of knowledge and skills sets for anxiety symptoms and disorders among HIV/AIDS service providers and the degree of training/education in evidenced-based care for anxiety.
9. Summary of review
The public health impact of HIV/AIDS and anxiety symptoms and disorders is substantial and warrants the financial and social investment in research to better understand their etiology, maintenance, and treatment. Moreover, the empirical evidence of significant comorbidity between the conditions, although producing a combined burden upon individuals and systems, also offers insight into the mechanisms underlying their etiology, progression, and maintenance. Ultimately, clinical research efforts in these areas may aid in the development of targeted interventions for the respective and combined conditions. We presented a heuristic model, which posits that HIV/AIDS and anxiety may, in fact, exacerbate each other via a number of distinct mechanisms. Future research in this emerging area has the potential to refine both theory and application with respect to HIV/AIDS, anxiety, and their comorbid presentation.
HIGHLIGHTS.
A review of the rates and impact of clinically-significant anxiety among persons living with HIV/AIDS (PLWHA) is presented.
Anxiety disorders and clinically-relevant symptoms have negative physical and emotional effects on PLWHA.
Certain transdiagnostic variables may impact the rates and impact of anxiety among PLWHA.
A heuristic model is proposed outlining the interrelations of anxiety and poor physical and psychological symptoms.
References
- Adewuya AO, Afolabi MO, Ola BA, Ogundele OA, Ajibare AO, Oladipo BF. Psychiatric disorders among the HIV-positive population in Nigeria: A control study. Journal Of Psychosomatic Research. 2007;63(2):203–206. doi: 10.1016/j.jpsychores.2007.03.006. http://dx.doi.org/10.1016/j.jpsychores.2007.03.006. [DOI] [PubMed] [Google Scholar]
- Aidala A, Havens J, Mellins CA, Dodds S, Whetten K, Martin D, Ko P. Development and validation of the Client Diagnostic Questionnaire (CDQ): A mental health screening tool for use in HIV service settings. Psychology, Health & Medicine. 2004;9(3):371–388. [Google Scholar]
- Antinori A, Arendt G, Becker JT, Brew BJ, Byrd DA, Cherner M, Wojna VE. Updated research nosology for HIV-associated neurocognitive disorders. Neurology. 2007;69(18):1789–1799. doi: 10.1212/01.WNL.0000287431.88658.8b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- APA. Diagnostic and Statistical Manual of Mental Disorders. 5th. Arlington, VA: American Psychiatric Association; 2013. [Google Scholar]
- Au A, Cheng C, Chan I, Leung P, Li P, Heaton RK. Subjective memory complaints, mood, and memory deficits among HIV/AIDS patients in Hong Kong. Journal of Clinical and Experimental Neuropsychology. 2008;30(3):338–348. doi: 10.1080/13803390701416189. http://dx.doi.org/10.1080/13803390701416189. [DOI] [PubMed] [Google Scholar]
- Bancroft J, Janssen E, Strong D, Carnes L, Vukadinovic Z, Long JS. Sexual risk-taking in gay men: The relevance of sexual arousability, mood, and sensation seeking. Archives of Sexual Behavior. 2003;32(6):555–572. doi: 10.1023/a:1026041628364. [DOI] [PubMed] [Google Scholar]
- Barlow DH. Anxiety and its disorders: The nature and treatment of anxiety and panic. 2nd. New York, NY, US: Guilford Press; 2002. [Google Scholar]
- Beck AT, Steer RA. Beck Anxiety Inventory (BAI): Manual. Ney York, NY: The Psychological Corporation; 1993. [Google Scholar]
- Beck AT, Epstein N, Brown G, Steer RA. An inventory for measuring clinical anxiety: psychometric properties. Journal of Consulting and Clinical Psychology. 1988;56(6):893. doi: 10.1037//0022-006x.56.6.893. [DOI] [PubMed] [Google Scholar]
- Bozzette SA, Berry SH, Duan N, Frankel M, Leibowitz A, Lefkowitz D, Shapiro MF. Caring for HIV Patients 1999 [Google Scholar]
- Brandt CP, Gonzalez A, Grover KW, Zvolensky MJ. The relation between emotional dysregulation and anxiety and depressive symptoms, pain-related anxiety, and HIV-symptom distress among adults with HIV/AIDS. Journal of Psychopathology and Behavioral Assessment. 2013a;35(2):197–204. http://dx.doi.org/10.1007/s10862-012-9329-y. [Google Scholar]
- Brandt CP, Zvolensky MJ, Bonn-Miller MO. Distress tolerance, emotion dysregulation, and anxiety and depressive symptoms among HIV+ individuals. Cognitive Therapy and Research. 2013b;37(3):446–455. http://dx.doi.org/10.1007/s10608-012-9497-9. [Google Scholar]
- Brazier J, Roberts J, Deverill M. The estimation of a preference-based measure of health from the SF-36. Journal of Health Economics. 2002;21(2):271–292. doi: 10.1016/s0167-6296(01)00130-8. [DOI] [PubMed] [Google Scholar]
- Breuer E, Stoloff K, Myer L, Seedat S, Stein DJ, Joska JA. The validity of the Substance Abuse and Mental Illness Symptom Screener (SAMISS) in people living with HIV/AIDS in primary HIV care in Cape Town, South Africa. AIDS and Behavior. 2014;18(6):1133–1141. doi: 10.1007/s10461-014-0698-y. http://dx.doi.org/10.1007/s10461-014-0698-y. [DOI] [PubMed] [Google Scholar]
- Bunn JY, Solomon SE, Miller C, Forehand R. Measurement of stigma in people with HIV: A reexamination of the HIV stigma scale. AIDS Education and Prevention. 2007;19(3):198–208. doi: 10.1521/aeap.2007.19.3.198. http://dx.doi.org/10.1521/aeap.2007.19.3.198. [DOI] [PubMed] [Google Scholar]
- Campos LN, Guimaraes MD, Remien RH. Anxiety and depression symptoms as risk factors for non-adherence to antiretroviral therapy in Brazil. AIDS and Behavior. 2010;14(2):289–299. doi: 10.1007/s10461-008-9435-8. http://dx.doi.org/10.1007/s10461-008-9435-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Capron DW, Gonzalez A, Parent J, Zvolensky MJ, Schmidt NB. Suicidality and anxiety sensitivity in adults with HIV. AIDS Patient Care and STDs. 2012;26(5):298–303. doi: 10.1089/apc.2011.0429. http://dx.doi.org/10.1089/apc.2011.0429. [DOI] [PubMed] [Google Scholar]
- Cardoso LD, Malbergier A. Who is not using condoms among HIV-positive patients in treatment in the largest city in Brazil? AIDS Care. 2015;27(5):629–636. doi: 10.1080/09540121.2014.986047. http://dx.doi.org/10.1080/09540121.2014.986047. [DOI] [PubMed] [Google Scholar]
- Carrieri MP, Chesney MA, Spire B, Loundou A, Sobel A, Lepeu G, Vlahov D. Failure to maintain adherence to HAART in a cohort of French HIV-positive injecting drug users. International Journal of Behavioral Medicine. 2003;10(1):1–14. doi: 10.1207/s15327558ijbm1001_01. http://dx.doi.org/10.1207/S15327558IJBM1001_01. [DOI] [PubMed] [Google Scholar]
- Carver CS, Lawrence JW, Scheier MF. A control-process perspective on the origins of affect. In: Martin LL, Tesser A, Martin LL, Tesser A, editors. Striving and feeling: Interactions among goals, affect, and self-regulation. Hillsdale, NJ, England: Lawrence Erlbaum Associates, Inc; 1996. pp. 11–52. [Google Scholar]
- Carver CS, Scheier MF, Weintraub JK. Assessing coping strategies: A theoretically based approach. Journal of Personality and Social Psychology. 1989;56(2):267–283. doi: 10.1037//0022-3514.56.2.267. [DOI] [PubMed] [Google Scholar]
- Catz SL, Heckman TG, Kochman A, DiMarco M. Rates and correlates of HIV treatment adherence among late middle-aged and older adults living with HIV disease. Psychology, Health & Medicine. 2001;6(1):47–58. http://dx.doi.org/10.1080/13548500020021919. [Google Scholar]
- CDC. HIV incidence. 2013 from http://www.cdc.gov/hiv/statistics/surveillance/incidence/index.html.
- Chan AS, Kwok I. Hong Kong List Learning Test: Manual and preliminary norm. Hong Kong: The Chinese University of Hong Kong; 1999. [Google Scholar]
- Chan I, Au A, Li P, Chung R, Lee MP, Yu P. Illness-related factors, stress and coping strategies in relation to psychological distress in HIV-infected persons in Hong Kong. AIDS Care. 2006;18(8):977–982. doi: 10.1080/09540120500490093. http://dx.doi.org/10.1080/09540120500490093. [DOI] [PubMed] [Google Scholar]
- Chelune GJ, Heaton RK, Lehman RA. Advances in clinical neuropsychology. US: Springer; 1986. Neuropsychological and personality correlates of patients‘ complaints of disability; pp. 95–126. [Google Scholar]
- Chesney MA, Ickovics JR, Chambers DB, Gifford AL, Neidig J, Zwickl B, Wu AW. Self-reported adherence to antiretroviral medications among participants in HIV clinical trials: The AACTG adherence instruments. AIDS Care. 2000;12(3):255–266. doi: 10.1080/09540120050042891. [DOI] [PubMed] [Google Scholar]
- Clark LA. Temperament as a unifying basis for personality and psychopathology. Journal of Abnormal Psychology. 2005;114(4):505–521. doi: 10.1037/0021-843X.114.4.505. http://dx.doi.org/10.1037/0021-843x.114.4.505. [DOI] [PubMed] [Google Scholar]
- Compas BE, Connor-Smith JK, Saltzman H, Thomsen AH, Wadsworth ME. Coping with stress during childhood and adolescence: Problems, progress, and potential in theory and research. Psychological Bulletin. 2001;127(1):87–127. [PubMed] [Google Scholar]
- Comulada WS, Rotheram-Borus MJ, Pequegnat W, Weiss RE, Desmond KA, Arnold EM, Chesney MA. Relationships over time between mental health symptoms and transmission risk among persons living with HIV. Psychology of Addictive Behaviors. 2010;24(1):109–118. doi: 10.1037/a0018190. http://dx.doi.org/10.1037/a0018190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conley TD, Taylor SE, Kemeny ME, Cole SW, Visscher B. Psychological sequelae of avoiding HIV-serostatus information. Basic and Applied Social Psychology. 1999;21(2):81–90. [Google Scholar]
- Connor KM, Kobak KA, Churchill LE, Katzelnick D, Davidson JR. Mini-SPIN: A brief screening assessment for generalized social anxiety disorder. Depression and Anxiety. 2001;14(2):137–140. doi: 10.1002/da.1055. [DOI] [PubMed] [Google Scholar]
- Connor-Smith JK, Compas BE, Wadsworth ME, Thomsen AH, Saltzman H. Responses to stress in adolescence: Measurement of coping and involuntary stress responses. Journal of Consulting and Clinical Psychology. 2000;68(6):976–992. [PubMed] [Google Scholar]
- Cox BJ, Norton GR, Swinson RP, Endler NS. Substance abuse and panic-related anxiety: A critical review. Behaviour Research and Therapy. 1990;28(5):385–393. doi: 10.1016/0005-7967(90)90157-e. http://dx.doi.org/10.1016/0005-7967(90)90157-E. [DOI] [PubMed] [Google Scholar]
- Crawford J, Smith G, Maylor E, Della Sala S, Logie R. The Prospective and Retrospective Memory Questionnaire (PRMQ): Normative data and latent structure in a large non-clinical sample. Memory. 2003;11(3):261–275. doi: 10.1080/09658210244000027. [DOI] [PubMed] [Google Scholar]
- Danese A, Caspi A, Williams B, Ambler A, Sugden K, Mika J, Arseneault L. Biological embedding of stress through inflammation processes in childhood. Molecular Psychiatry. 2011;16(3):244–246. doi: 10.1038/mp.2010.5. http://dx.doi.org/10.1038/mp.2010.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dennis ML. Global Appraisal of Individual Needs (GAIN) Bloomington, IL: Chestnut Healthcare Systems; 1998. [Google Scholar]
- Derogatis LR. SCL-90-R: Administration, scoring & procedures manual-II for the R (evised) version and other instruments of the psychopathology rating scale series. Clinical psychometric research, Incorporated; 1992. [Google Scholar]
- Derogatis LR, Melisaratos N. The Brief Symptom Inventory: An introductory report. Psychological Medicine. 1983;13(3):595–605. [PubMed] [Google Scholar]
- Desmond AC, Moodley D, Conolly CA, Castel SA, Coovadia HM. Evaluation of adherence measures of antiretroviral prophylaxis in HIV exposed infants in the first 6 weeks of life. BMC Pediatrics. 2015;15:23. doi: 10.1186/s12887-015-0340-9. http://dx.doi.org/10.1186/s12887-015-0340-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Escobar Y, Venturelli CR, Escobar-Islas E, Hoyo-Vadillo C. Pharmacokinetics of stavudine by oral administration to healthy Mexican volunteers. Paper presented at the Proceedings-Western Pharmacology Society. 2003 [PubMed] [Google Scholar]
- Fincham D, Smit J, Carey P, Stein DJ, Seedat S. The relationship between behavioural inhibition, anxiety disorders, depression and CD4 counts in HIV-positive adults: A cross-sectional controlled study. AIDS Care. 2008;20(10):1279–1283. doi: 10.1080/09540120801927025. http://dx.doi.org/10.1080/09540120801927025. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. Structured clinical interview for DSM-IV axis I disorders. New York: New York State Psychiatric Institute; 1995. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JB. User’s guide for the Structured clinical interview for DSM-IV axis I disorders SCID-I: clinician version. American Psychiatric Pub; 1997. [Google Scholar]
- Foa EB. Posttraumatic stress diagnostic scale. National Computer Systems; 1995. [Google Scholar]
- Garey L, Bakhshaie J, Sharp C, Neighbors C, Zvolensky MJ, Gonzalez A. Anxiety, depression, and HIV symptoms among persons living with HIV/AIDS: The role of hazardous drinking. AIDS Care. 2015;27(1):80–85. doi: 10.1080/09540121.2014.956042. http://dx.doi.org/10.1080/09540121.2014.956042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garnefski N, Kraaij V, Spinhoven P. Manual for the use of the Cognitive Emotion Regulation Questionnaire. Leiderdorp, The Netherlands: DATEC; 2002. [Google Scholar]
- Glémaud M, Illa L, Echenique M, Bustamente-Avellaneda V, Gazabon S, Villar-Loubet O, Kolber MA. Abuse and mental health concerns among HIV-infected Haitian women living in the United States. JANAC: Journal of The Association Of Nurses In AIDS Care. 2014;25(1, Suppl):S62–S69. doi: 10.1016/j.jana.2013.06.005. http://dx.doi.org/10.1016/j.jana.2013.06.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez A, Zvolensky MJ, Grover KW, Parent J. The role of anxiety sensitivity and mindful attention in anxiety and worry about bodily sensations among adults living with HIV/AIDS. Behavior Therapy. 2012a;43(4):768–778. doi: 10.1016/j.beth.2012.04.001. [DOI] [PubMed] [Google Scholar]
- Gonzalez A, Zvolensky MJ, Parent J, Grover KW, Hickey M. HIV symptom distress and anxiety sensitivity in relation to panic, social anxiety, and depression symptoms among HIV-positive adults. AIDS Patient Care and STDs. 2012b;26(3):156–164. doi: 10.1089/apc.2011.0309. [DOI] [PubMed] [Google Scholar]
- Gonzalez A, Solomon SE, Zvolensky MJ, Miller CT. The interaction of mindful-based attention and awareness and disengagement coping with HIV/AIDS-related stigma in regard to concurrent anxiety and depressive symptoms among adults with HIV/AIDS. Journal of Health Psychology. 2009;14(3):403–413. doi: 10.1177/1359105309102193. http://dx.doi.org/10.1177/1359105309102193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gonzalez A, Zvolensky MJ, Solomon SE, Miller CT. Exploration of the relevance of anxiety sensitivity among adults living with HIV/AIDS for understanding anxiety vulnerability. Journal of Health Psychology. 2010;15(1):138–146. doi: 10.1177/1359105309344898. http://dx.doi.org/10.1177/1359105309344898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou PS, Kay W, Pickering R. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug and Alcohol Dependence. 2003;71(1):7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- Gratz KL, Roemer L. Multidimensional assessment of emotion regulation and dysregulation: Development, factor structure, and initial validation of the difficulties in emotion regulation scale. Journal of Psychopathology and Behavioral Assessment. 2004;26(1):41–54. http://dx.doi.org/10.1023/B:JOBA.0000007455.08539.94. [Google Scholar]
- Gross JJ. Antecedent- and response-focused emotion regulation: Divergent consequences for experience, expression, and physiology. Journal of Personality and Social Psychology. 1998;74(1):224–237. doi: 10.1037//0022-3514.74.1.224. http://dx.doi.org/10.1037/0022-3514.74.1.224. [DOI] [PubMed] [Google Scholar]
- Gusi N, Olivares PR, Rajendram R. The EQ-5D health-related quality of life questionnaire. In: Preedy V, Watson R, editors. Handbook of disease burdens and quality of life measures. New York: Springer; 2010. pp. 87–99. [Google Scholar]
- Hamilton M. The assessment of anxiety states by rating. The British Journal of Medical Psychology. 1959;32(1):50–55. doi: 10.1111/j.2044-8341.1959.tb00467.x. [DOI] [PubMed] [Google Scholar]
- Hansen NB, Harrison B, Fambro S, Bodnar S, Heckman TG, Sikkema KJ. The structure of coping among older adults living with HIV/AIDS and depressive symptoms. Journal of Health Psychology. 2013;18(2):198–211. doi: 10.1177/1359105312440299. http://dx.doi.org/10.1177/1359105312440299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasanah CI, Zaliha AR, Mahiran M. Factors influencing the quality of life in patients with HIV in Malaysia. Quality of Life Research: An International Journal Of Quality Of Life Aspects Of Treatment, Care & Rehabilitation. 2011;20(1):91–100. doi: 10.1007/s11136-010-9729-y. http://dx.doi.org/10.1007/s11136-010-9729-y. [DOI] [PubMed] [Google Scholar]
- Hayward C, Killen JD, Kraemer HC, Taylor CB. Predictors of panic attacks in adolescents. Journal of the American Academy of Child and Adolescent Psychiatry. 2000;39(2):207–214. doi: 10.1097/00004583-200002000-00021. http://dx.doi.org/10.1097/00004583-200002000-00021. [DOI] [PubMed] [Google Scholar]
- Heaton RK, Clifford DB, Franklin DR, Jr, Woods SP, Ake C, Vaida F, Grant I. HIV-associated neurocognitive disorders persist in the era of potent antiretroviral therapy: Charter study. Neurology. 2010;75(23):2087–2096. doi: 10.1212/WNL.0b013e318200d727. http://dx.doi.org/10.1212/WNL.0b013e318200d727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hurst NP, Kind P, Ruta D. Comparison of the MOS short form-12 (SF12) health status questionnaire with the SF 36 in patients with rheumatoid arthritis. British Journal of Rheumatology. 1998;37(8):862–869. doi: 10.1093/rheumatology/37.8.862. [DOI] [PubMed] [Google Scholar]
- Ibanez GE, Purcell DW, Stall R, Parsons JT, Gomez CA. Sexual risk, substance use, and psychological distress in HIV-positive gay and bisexual men who. 2005 doi: 10.1097/01.aids.0000167351.00503.92. [DOI] [PubMed] [Google Scholar]
- Ingersoll K. The impact of psychiatric symptoms, drug use, and medication regimen on nonadherence to HIV treatment. AIDS Care. 2004;16(2):199–211. doi: 10.1080/09540120410001641048. http://dx.doi.org/10.1080/09540120410001641048. [DOI] [PubMed] [Google Scholar]
- Kalichman SC. Psychological and social correlates of high-risk sexual behaviour among men and women living with HIV/AIDS. AIDS Care. 1999;11(4):415–427. doi: 10.1080/09540129947794. http://dx.doi.org/10.1080/09540129947794. [DOI] [PubMed] [Google Scholar]
- Keiser O, Spoerri A, Brinkhof MWG, Hasse B, Gayet-Ageron A, Tissot F, Egger M. Suicide in HIV-infected individuals and the general population in Switzerland, 1988–2008. The American Journal of Psychiatry. 2010;167(2):143–150. doi: 10.1176/appi.ajp.2009.09050651. http://dx.doi.org/10.1176/appi.ajp.2009.09050651. [DOI] [PubMed] [Google Scholar]
- Kelly JA, Murphy DA. Psychological interventions with AIDS and HIV: Prevention and treatment. Journal of Consulting and Clinical Psychology. 1992;60(4):576–585. doi: 10.1037//0022-006x.60.4.576. [DOI] [PubMed] [Google Scholar]
- Kennedy CA, Skurnick J, Wan JY, Quattrone G, Sheffet A, Quinones M, Louria DB. Psychological distress, drug and alcohol use as correlates on condom use in HIV-serodiscordant heterosexual couples. AIDS. 1993;7(11):1493–1499. doi: 10.1097/00002030-199311000-00014. http://dx.doi.org/10.1097/00002030-199311000-00014. [DOI] [PubMed] [Google Scholar]
- Kessler R, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SL, Zaslavsky AM. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine. 2002;32(6):959–976. doi: 10.1017/s0033291702006074. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Andrews M, Ustun, Wittchen The world health organization composite international diagnostic interview short-form (CIDI-SF) International Journal of Methods in Psychiatric Research. 1998a;7(4):171–185. doi: 10.1002/mpr.168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kessler RC, Andrews G, Mroczek D, Ustun B, Wittchen HU. The world health organization composite international diagnostic interview short-form (cidisf) International Journal of Methods in Psychiatric Research. 1998b;7(4):171–185. [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kinyanda E, Hoskins S, Nakku J, Nawaz S, Patel V. The prevalence and characteristics of suicidality in HIV/AIDS as seen in an African population in Entebbe district, Uganda. BMC Psychiatry. 2012;12:63. doi: 10.1186/1471-244X-12-63. http://dx.doi.org/10.1186/1471-244x-12-63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kosiba JD, Gonzalez A, O’Cleirigh C, Safren SA. Medication adherence and HIV symptom distress in relation to panic disorder among HIV-positive adults managing opioid dependence. Cognitive Therapy and Research. 2014;38(4):458–464. doi: 10.1007/s10608-014-9608-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraaij V, van der Veek SM, Garnefski N, Schroevers M, Witlox R, Maes S. Coping, goal adjustment, and psychological well-being in HIV-infected men who have sex with men. AIDS Patient Care and STDs. 2008;22(5):395–402. doi: 10.1089/apc.2007.0145. http://dx.doi.org/10.1089/apc.2007.0145. [DOI] [PubMed] [Google Scholar]
- Krueger RF. The structure of common mental disorders. Archives of General Psychiatry. 1999;56(10):921–926. doi: 10.1001/archpsyc.56.10.921. [DOI] [PubMed] [Google Scholar]
- Lambert S, Keegan A, Petrak J. Sex and relationships for HIV positive women since HAART: A quantitative study. Sexually Transmitted Infections. 2005;81(4):333–337. doi: 10.1136/sti.2004.013516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leserman J. HIV disease progression: Depression, stress, and possible mechanisms. Biological Psychiatry. 2003;54(3):295–306. doi: 10.1016/s0006-3223(03)00323-8. [DOI] [PubMed] [Google Scholar]
- Lewis G, Pelosi AJ, Araya R, Dunn G. Measuring psychiatric disorder in the community: a standardized assessment for use by lay interviewers. Psychological Medicine. 1992;22(02):465–486. doi: 10.1017/s0033291700030415. [DOI] [PubMed] [Google Scholar]
- Leyro TM, Vujanovic AA, Bonn-Miller MO. Examining associations between cognitive-affective vulnerability and HIV symptom severity, perceived barriers to treatment adherence, and viral load among HIV-positive adults. International Journal of Behavioral Medicine. 2015;22(1):139–148. doi: 10.1007/s12529-014-9404-8. http://dx.doi.org/10.1007/s12529-014-9404-8. [DOI] [PubMed] [Google Scholar]
- Leyro TM, Zvolensky MJ, Bernstein A. Distress tolerance and psychopathological symptoms and disorders: A review of the empirical literature among adults. Psychological Bulletin. 2010;136(4):576–600. doi: 10.1037/a0019712. http://dx.doi.org/10.1037/a0019712. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Li W, Zinbarg RE. Anxiety sensitivity and panic attacks: A 1-year longitudinal study. Behavior Modification. 2007;31(2):145–161. doi: 10.1177/0145445506296969. http://dx.doi.org/10.1177/0145445506296969. [DOI] [PubMed] [Google Scholar]
- Lockenhoff CE, Ironson GH, O’Cleirigh C, Costa PT., Jr Five-factor model personality traits, spirituality/religiousness, and mental health among people living with HIV. Journal of Personality. 2009;77(5):1411–1436. doi: 10.1111/j.1467-6494.2009.00587.x. http://dx.doi.org/10.1111/j.1467-6494.2009.00587.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lopes M, Olfson M, Rabkin J, Hasin DS, Alegría AA, Lin K, Blanco C. Gender, HIV status, and psychiatric disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions. Journal of Clinical Psychiatry. 2012;73(3):384–391. doi: 10.4088/JCP.10m06304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lovibond PF, Lovibond SH. The structure of negative emotional states: Comparison of the Depression Anxiety Stress Scales (DASS) with the Beck Depression and Anxiety Inventories. Behaviour Research and Therapy. 1995;33(3):335–343. doi: 10.1016/0005-7967(94)00075-u. [DOI] [PubMed] [Google Scholar]
- Lung F-W, Lee M-B. The five-item Brief-Symptom Rating Scale as a suicide ideation screening instrument for psychiatric inpatients and community residents. BMC Psychiatry. 2008;8 doi: 10.1186/1471-244X-8-53. http://dx.doi.org/10.1186/1471-244X-8-53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lutgendorf SK, Antoni MH, Ironson G, Klimas N, Kumar M, Starr K, Schneiderman N. Cognitive–behavioral stress management decreases dysphoric mood and herpes simplex virus-type 2 antibody titers in symptomatic HIV-seropositive gay men. Journal of Consulting and Clinical Psychology. 1997;65(1):31–43. doi: 10.1037//0022-006x.65.1.31. http://dx.doi.org/10.1037/0022-006X.65.1.31. [DOI] [PubMed] [Google Scholar]
- Malaspina L, Woods SP, Moore DJ, Depp C, Letendre SL, Jeste D, Grant I. Successful cognitive aging in persons living with HIV infection. Journal of Neurovirology. 2011;17(1):110–119. doi: 10.1007/s13365-010-0008-z. http://dx.doi.org/10.1007/s13365-010-0008-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maller RG, Reiss S. Anxiety sensitivity in 1984 and panic attacks in 1987. Journal of Anxiety Disorders. 1992;6(3):241–247. [Google Scholar]
- Marshall GN, Miles JN, Stewart SH. Anxiety sensitivity and PTSD symptom severity are reciprocally related: Evidence from a longitudinal study of physical trauma survivors. Journal of Abnormal Psychology. 2010;119(1):143–150. doi: 10.1037/a0018009. http://dx.doi.org/10.1037/a0018009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marwick KM, Kaaya SF. Prevalence of depression and anxiety disorders in HIV-positive outpatients in rural Tanzania. AIDS Care. 2010;22(4):415–419. doi: 10.1080/09540120903253981. http://dx.doi.org/10.1080/09540120903253981. [DOI] [PubMed] [Google Scholar]
- McNair DM, Lorr M, Droppleman LF. Profile of mood states: Univ 1971 [Google Scholar]
- McNair DM, Lorr M, Droppleman LF. Profile of mood states. San Diego, CA: Educational and Industrial Testing Service; 1981. pp. 1–29. [Google Scholar]
- McNally RJ. Anxiety sensitivity and panic disorder. Biological Psychiatry. 2002;52(10):938–946. doi: 10.1016/s0006-3223(02)01475-0. http://dx.doi.org/10.1016/S0006-3223(02)01475-0. [DOI] [PubMed] [Google Scholar]
- Mellins CA, Havens JF, McCaskill EO, Leu CS, Brudney K, Chesney MA. Mental health, substance use and disclosure are significantly associated with the medical treatment adherence of HIV-infected mothers. Psychology, Health & Medicine. 2002;7(4):451–460. [Google Scholar]
- Mellins CA, Kang E, Leu CS, Havens JF, Chesney MA. Longitudinal study of mental health and psychosocial predictors of medical treatment adherence in mothers living with HIV disease. AIDS Patient Care & STDS. 2003;17(8):407–416. doi: 10.1089/108729103322277420. [DOI] [PubMed] [Google Scholar]
- Micali E, Zirilli A, Abbate C. Minor cognitive deficits and mood states in HIV-1 infected men. Illness, Crisis, & Loss. 2011;19(4):363–377. http://dx.doi.org/10.2190/IL.19.4.e. [Google Scholar]
- Mimiaga MJ, Biello K, Reisner SL, Crane HM, Wilson J, Grasso C, Safren SA. Latent class profiles of internalizing and externalizing psychosocial health indicators are differentially associated with sexual transmission risk: Findings from the CFAR Network of Integrated Clinical Systems (CNICS) cohort study of HIV-infected men engaged in primary care in the United States. Health Psychology. 2015 doi: 10.1037/hea0000189. http://dx.doi.org/10.1037/hea0000189. [DOI] [PMC free article] [PubMed]
- Mulder CL, Antoni MH, Duivenvoorden HJ, Kauffmann RH, Goodkin K. Active confrontational coping predicts decreased clinical progression over a one-year period in HIV-infected homosexual men. Journal of Psychosomatic Research. 1995;39(8):957–965. doi: 10.1016/0022-3999(95)00062-3. [DOI] [PubMed] [Google Scholar]
- Nebhinani N, Mattoo SK, Wanchu A. Psychiatric morbidity in HIV-positive subjects: A study from India. Journal of Psychosomatic Research. 2011;70(5):449–454. doi: 10.1016/j.jpsychores.2010.09.021. http://dx.doi.org/10.1016/j.jpsychores.2010.09.021. [DOI] [PubMed] [Google Scholar]
- Nel A, Kagee A. The relationship between depression, anxiety and medication adherence among patients receiving antiretroviral treatment in South Africa. AIDS Care. 2013;25(8):948–955. doi: 10.1080/09540121.2012.748867. http://dx.doi.org/10.1080/09540121.2012.748867. [DOI] [PubMed] [Google Scholar]
- Niaura R, Shadel WG, Morrow K, Tashima K, Flanigan T, Abrams DB. Human immunodeficiency virus infection, AIDS, and smoking cessation: The time is now. Clinical Infectious Diseases. 2000;31(3):808–812. doi: 10.1086/314048. [DOI] [PubMed] [Google Scholar]
- NIDA. NIDA modified-ASSIST. 2009 (from) http://www.drugabuse.gov/nidamed/screening/
- Nurutdinova D, Chrusciel T, Zeringue A, Scherrer JF, Al-Aly Z, McDonald JR, Overton ET. Mental health disorders and the risk of AIDS-defining illness and death in HIV-infected veterans. AIDS. 2012;26(2):229–234. doi: 10.1097/QAD.0b013e32834e1404. http://dx.doi.org/10.1097/QAD.0b013e32834e1404. [DOI] [PubMed] [Google Scholar]
- O’Cleirigh C, Hart TA, James CA. HIV and anxiety. In: Zvolensky MJ, Smits JAJ, Zvolensky MJ, Smits JAJ, editors. Anxiety in health behaviors and physical illness. New York, NY, US: Springer Science + Business Media; 2008. pp. 317–340. [Google Scholar]
- O’Cleirigh C, Magidson JF, Skeer MR, Mayer KH, Safren SA. Prevalence of psychiatric and substance abuse symptomatology among HIV-infected gay and bisexual men in HIV primary care. Psychosomatics. 2014 doi: 10.1016/j.psym.2014.08.004. http://dx.doi.org/10.1016/j.psym.2014.08.004. [DOI] [PMC free article] [PubMed]
- O’Cleirigh C, Traeger L, Mayer KH, Magidson JF, Safren SA. Anxiety specific pathways to HIV sexual transmission risk behavior among young gay and bisexual men. Journal Gay Lesbian Mental Health. 2013;17(3):314–326. doi: 10.1080/19359705.2012.755142. http://dx.doi.org/10.1080/19359705.2012.755142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okazaki S. Impact of racism on ethnic minority mental health. Perspectives on Psychological Science. 2009;4(1):103–107. doi: 10.1111/j.1745-6924.2009.01099.x. [DOI] [PubMed] [Google Scholar]
- Olagunju AT, Adeyemi JD, Ogbolu RE, Campbell EA. A study on epidemiological profile of anxiety disorders among people living with HIV/AIDS in a sub-Saharan Africa HIV clinic. AIDS and Behavior. 2012;16(8):2192–2197. doi: 10.1007/s10461-012-0250-x. http://dx.doi.org/10.1007/s10461-012-0250-x. [DOI] [PubMed] [Google Scholar]
- O’Leary A, Purcell D, Remien RH, Gomez C. Childhood sexual abuse and sexual transmission risk behaviour among HIV-positive men who have sex with men. AIDS Care. 2003;15(1):17–26. doi: 10.1080/0954012021000039725. [DOI] [PubMed] [Google Scholar]
- Olley BO, Seedat S, Nei DG, Stein DJ. Predictors of major depression in recently diagnosed patients with HIV/AIDS in South Africa. AIDS Patient Care And Stds. 2004;18(8):481–487. doi: 10.1089/1087291041703700. http://dx.doi.org/10.1089/1087291041703700. [DOI] [PubMed] [Google Scholar]
- Orlando M, Burnam MA, Beckman R, Morton SC, London AS, Bing EG, Fleishman JA. Re-estimating the prevalence of psychiatric disorders in a nationally representative sample of persons receiving care for HIV: Results from the HIV Cost and Services Utilization Study. International Journal of Methods in Psychiatric Research. 2002;11(2):75–82. doi: 10.1002/mpr.125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Palmer NB, Salcedo J, Miller AL, Winiarski M, Arno P. Psychiatric and social barriers to HIV medication adherence in a triply diagnosed methadone population. AIDS Patient Care and STDs. 2003;17(12):635–644. doi: 10.1089/108729103771928690. http://dx.doi.org/10.1089/108729103771928690. [DOI] [PubMed] [Google Scholar]
- Parhami I, Fong TW, Siani A, Carlotti C, Khanlou H. Documentation of psychiatric disorders and related factors in a large sample population of HIV-positive patients in California. AIDS and Behavior. 2013;17(8):2792–2801. doi: 10.1007/s10461-012-0386-8. http://dx.doi.org/10.1007/s10461-012-0386-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Passos SM, Souza LD, Spessato BC. High prevalence of suicide risk in people living with HIV: Who is at higher risk? AIDS Care. 2014;26(11):1379–1382. doi: 10.1080/09540121.2014.913767. http://dx.doi.org/10.1080/09540121.2014.913767. [DOI] [PubMed] [Google Scholar]
- Pence BW, Miller WC, Gaynes BN, Eron JJ., Jr Psychiatric illness and virologic response in patients initiating highly active antiretroviral therapy. Journal of Acquired Immune Deficiency Syndromes. 2007;44(2):159–166. doi: 10.1097/QAI.0b013e31802c2f51. http://dx.doi.org/10.1097/QAI.0b013e31802c2f51. [DOI] [PubMed] [Google Scholar]
- Pence BW, Miller WC, Whetten K, Eron JJ, Gaynes BN. Prevalence of DSM-IV-defined mood, anxiety, and substance use disorders in an HIV clinic in the southeastern United States. JAIDS Journal of Acquired Immune Deficiency Syndromes. 2006;42(3):298–306. doi: 10.1097/01.qai.0000219773.82055.aa. http://dx.doi.org/10.1097/01.qai.0000219773.82055.aa. [DOI] [PubMed] [Google Scholar]
- Pence BW, Gaynes BN, Whetten K, Eron JJ, Ryder RW, Miller WC. Validation of a brief screening instrument for substance abuse and mental illness in HIV/patients. Journal of Acquired Immunodeficiency Syndromes. 2005;40:434444. doi: 10.1097/01.qai.0000177512.30576.9c. [DOI] [PubMed] [Google Scholar]
- Peng EY-C, Yeh C-Y, Lyu S-Y, Morisky DE, Chen Y-MA, Lee M-B, Malow RM. Prevalence and correlates of lifetime suicidal ideation among HIV-infected male inmates in Taiwan. AIDS Care. 2010;22(10):1212–1220. doi: 10.1080/09540121003623701. http://dx.doi.org/10.1080/09540121003623701. [DOI] [PubMed] [Google Scholar]
- Peterman AH, Cella D, Mo F, McCain N. Psychometric validation of the revised Functional Assessment of Human Immunodeficiency Virus Infection (FAHI) quality of life instrument. Quality of Life Research. 1997;6(6):572–584. doi: 10.1023/a:1018416317546. [DOI] [PubMed] [Google Scholar]
- Petrushkin H, Boardman J, Ovuga E. Psychiatric disorders in HIV-positive individuals in urban Uganda. Psychiatric Bulletin. 2005;29(12):455–458. http://dx.doi.org/10.1192/pb.29.12.455. [Google Scholar]
- Psaros C, O’Cleirigh C, Bullis JR, Markowitz SM, Safren SA. The influence of psychological variables on health-related quality of life among HIV-positive individuals with a history of intravenous drug use. Journal of Psychoactive Drugs. 2013;45(4):304–312. doi: 10.1080/02791072.2013.825030. http://dx.doi.org/10.1080/02791072.2013.825030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Quintana-Ortiz RA, Gomez MA, Baez Feliciano DV, Hunter-Mellado RF. Suicide attempts among Puerto Rican men and women with HIV/AIDS: A study of prevalence and risk factors. Ethnicity and Disease. 2008;18(2 Suppl 2):S2-219–224. [PubMed] [Google Scholar]
- Rabkin JG. Prevalence of psychiatric disorders in HIV illness. International Review of Psychiatry. 1996;8(2–3):157–166. http://dx.doi.org/10.3109/09540269609046300. [Google Scholar]
- Rabkin JG, Williams JB, Remien RH, Goetz R, Kertzner R, Gorman JM. Depression, distress, lymphocyte subsets, and human immunodeficiency virus symptoms on two occasions in HIV-positive homosexual men. Archives of General Psychiatry. 1991;48(2):111–119. doi: 10.1001/archpsyc.1991.01810260019002. [DOI] [PubMed] [Google Scholar]
- Rapee RM, Medoro L. Fear of physical sensations and trait anxiety as mediators of the response to hyperventilation in nonclinical subjects. Journal of Abnormal Psychology. 1994;103(4):693–699. doi: 10.1037//0021-843x.103.4.693. [DOI] [PubMed] [Google Scholar]
- Reed GM, Kemeny ME, Taylor SE, Wang HY, Visscher BR. Realistic acceptance as a predictor of decreased survival time in gay men with AIDS. Health Psychology. 1994;13(4):299–307. doi: 10.1037//0278-6133.13.4.299. [DOI] [PubMed] [Google Scholar]
- Reif SS, Pence BW, LeGrand S, Wilson ES, Swartz M, Ellington T, Whetten K. In-home mental health treatment for individuals with HIV. AIDS Patient Care and STDs. 2012;26(11):655–661. doi: 10.1089/apc.2012.0242. http://dx.doi.org/10.1089/apc.2012.0242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reiss S, McNally RJ. Expectancy model of fear. In: Reiss S, Bootzin RR, editors. Theoretical issues in behavior therapy. San Diego, CA: Academic Press; 1985. [Google Scholar]
- Roberts AC, Wechsberg WM, Zule W, Burroughs AR. Contextual factors and other correlates of sexual risk of HIV among African-American crack-abusing women. Addictive Behaviors. 2003;28(3):523–536. doi: 10.1016/s0306-4603(01)00255-6. http://dx.doi.org/10.1016/S0306-4603(01)00255-6. [DOI] [PubMed] [Google Scholar]
- Robertson K, Bayon C, Molina J, McNamara P, Resch C, Muñoz-Moreno JA, van Wyk J. Screening for neurocognitive impairment, depression, and anxiety in HIV-infected patients in Western Europe and Canada. AIDS Care. 2014;26(12):1555–1561. doi: 10.1080/09540121.2014.936813. http://dx.doi.org/10.1080/09540121.2014.936813. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robertson K, Parsons TD, Van Der Horst C, Hall C. Thoughts of death and suicidal ideation in nonpsychiatric human immunodeficiency virus seropositive individuals. Death Studies. 2006;30(5):455–469. doi: 10.1080/07481180600614435. http://dx.doi.org/10.1080/07481180600614435. [DOI] [PubMed] [Google Scholar]
- Roux P, Carrieri MP, Michel L, Fugon L, Marcellin F, Obadia Y, Spire B. Effect of anxiety symptoms on adherence to highly active antiretroviral therapy in HIV-infected women. Journal of Clinical Psychiatry. 2009;70(9):1328–1329. doi: 10.4088/JCP.08l04885. http://dx.doi.org/10.4088/JCP.08l04885. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO Collaborative Project on Early Detection of Persons with Harmful Alcohol Consumption–II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Keough ME, Mitchell MA, Reynolds EK, Macpherson L, Zvolensky MJ, Lejuez CW. Anxiety sensitivity: Prospective prediction of anxiety among early adolescents. Journal of Anxiety Disorders. 2010;24(5):503–508. doi: 10.1016/j.janxdis.2010.03.007. http://dx.doi.org/10.1016/j.janxdis.2010.03.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schmidt NB, Lerew DR, Jackson RJ. Prospective evaluation of anxiety sensitivity in the pathogenesis of panic: Replication and extension. Journal of Abnormal Psychology. 1999;108(3):532–537. doi: 10.1037//0021-843x.108.3.532. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Zvolensky MJ, Maner JK. Anxiety sensitivity: Prospective prediction of panic attacks and Axis I pathology. Journal of Psychiatric Research. 2006a;40(8):691–699. doi: 10.1016/j.jpsychires.2006.07.009. http://dx.doi.org/10.1016/j.jpsychires.2006.07.009. [DOI] [PubMed] [Google Scholar]
- Schmidt NB, Richey JA, Fitzpatrick KK. Discomfort intolerance: Development of a construct and measure relevant to panic disorder. Journal of Anxiety Disorders. 2006b;20(3):263–280. doi: 10.1016/j.janxdis.2005.02.002. http://dx.doi.org/10.1016/j.janxdis.2005.02.002. [DOI] [PubMed] [Google Scholar]
- Schönnesson LN, Diamond PM, Ross MW, Williams M, Bratt G. ‘Baseline predictors of three types of antiretroviral therapy (ART) adherence: A 2-year followup‘: Erratum. AIDS Care. 2006;18(4):406–414. doi: 10.1080/09540120500456631a. [DOI] [PubMed] [Google Scholar]
- Schönnesson LN, Williams ML, Ross MW, Bratt G, Keel B. Factors associated with suboptimal antiretroviral therapy adherence to dose, schedule, and dietary instructions. AIDS and Behavior. 2007;11(2):175–183. doi: 10.1007/s10461-006-9160-0. [DOI] [PubMed] [Google Scholar]
- Schoth DE, Liossi C. Attentional bias toward pictorial representations of pain in individuals with chronic headache. The Clinical Journal of Pain. 2010;26(3):244–250. doi: 10.1097/AJP.0b013e3181bed0f9. [DOI] [PubMed] [Google Scholar]
- Sewell MC, Goggin KJ, Rabkin JG, Ferrando SJ, McElhiney MC, Evans S. Anxiety syndromes and symptoms among men with AIDS: A longitudinal controlled study. Psychosomatics. 2000;41(4):294–300. doi: 10.1176/appi.psy.41.4.294. http://dx.doi.org/10.1176/appi.psy.41.4.294. [DOI] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Dunbar GC. The Mini-International Neuropsychiatric Interview (M.I.N.I.): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. The Journal of Clinical Psychiatry. 1998;59(Suppl. 20):22–33. (quiz 34–57) [PubMed] [Google Scholar]
- Siegel K, Lekas HM. AIDS as a chronic illness: Psychosocial implications. AIDS. 2002;16(Suppl. 4):S69–S76. doi: 10.1097/00002030-200216004-00010. [DOI] [PubMed] [Google Scholar]
- Simoni JM, Frick PA, Huang B. A longitudinal evaluation of a social support model of medication adherence among HIV-positive men and women on antiretroviral therapy. Health Psychology. 2006;25(1):74. doi: 10.1037/0278-6133.25.1.74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons JS, Gaher RM. The Distress Tolerance Scale: Development and validation of a self-report measure. Motivation and Emotion. 2005;29(2):83–102. http://dx.doi.org/10.1007/s11031-005-7955-3. [Google Scholar]
- Simpson D. Drug abuse treatment for AIDS risk reduction (DATAR): Forms manual. Fort Worth, TX: Texas Christian University; 1990. [Google Scholar]
- Sivasubramanian M, Mimiaga MJ, Mayer KH, Anand VR, Johnson CV, Prabhugate P, Safren SA. Suicidality, clinical depression, and anxiety disorders are highly prevalent in men who have sex with men in Mumbai, India: Findings from a community-recruited sample. Psychology Health & Medicine. 2011;16(4):450–462. doi: 10.1080/13548506.2011.554645. http://dx.doi.org/10.1080/13548506.2011.554645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skevington SM, Sartorius N, Amir M. Developing methods for assessing quality of life in different cultural settings. Social Psychiatry and Psychiatric Epidemiology. 2004;39(1):1–8. doi: 10.1007/s00127-004-0700-5. [DOI] [PubMed] [Google Scholar]
- Sobell LC, Sobell MB. Timeline Followback: A technique for assessing self-reported alcohol consumption. In: Litten RZ, Allen J, editors. Measuring alcohol consumption: Psychosocial and biological methods. Towota, NJ: Humana Press; 1992. pp. 41–72. [Google Scholar]
- Song YS, Ingram KM. Unsupportive social interactions, availability of social support, and coping: Their relationship to mood disturbance among African Americans living with HIV. Journal of Social and Personal Relationships. 2002;19(1):67–86. http://dx.doi.org/10.1177/0265407502191004. [Google Scholar]
- Spielberger R, Gorsuch R, Lushene R. STAI manual for the State-Trait Anxiety Inventory 1970. Palo Alto, CA: Consulting Psychologists; 1970. [Google Scholar]
- Spies G, Asmal L, Seedat S. Cognitive-behavioural interventions for mood and anxiety disorders in HIV: A systematic review. Journal of Affective Disorders. 2013;150(2):171–180. doi: 10.1016/j.jad.2013.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spies G, Kader K, Kidd M, Smit J, Myer L, Stein DJ, Seedat S. Validity of the K-10 in detecting DSM-IV-defined depression and anxiety disorders among HIV-infected individuals. AIDS Care. 2009;21(9):1163–1168. doi: 10.1080/09540120902729965. http://dx.doi.org/10.1080/09540120902729965. [DOI] [PubMed] [Google Scholar]
- Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: The PHQ primary care study. Primary care evaluation of mental disorders. Patient health questionnaire. JAMA. 1999;282(18):1737–1744. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- Stanley S, Sethuramalingam V, Sathia S. Quality of life correlates in HIV-positive people in a city in South India. Journal of HIV/AIDS & Social Services. 2014;13(4):337–352. [Google Scholar]
- Staton-Tindall M, Harp KL, Minieri A, Oser C, Webster JM, Havens J, Leukefeld C. An exploratory study of mental health and HIV risk behavior among drug-using rural women in jail. Psychiatric Rehabilitation Journal. 2015;38(1):45–54. doi: 10.1037/prj0000107. http://dx.doi.org/10.1037/prj0000107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoskopf CH, Kim YK, Glover SH. Dual diagnosis: HIV and mental illness, a population-based study. Community Mental Health Journal. 2001;37(6):469–479. doi: 10.1023/a:1017577827658. http://dx.doi.org/10.1023/A:1017577827658. [DOI] [PubMed] [Google Scholar]
- Surah S, Adams R, Townsend L, Reynolds I, Kinahan JC, Keating S, Lyons F. Health-related quality of life of HIV-infected intravenous drug users. International Journal of STD & AIDS. 2013;24(11):867–874. doi: 10.1177/0956462413486454. http://dx.doi.org/10.1177/0956462413486454. [DOI] [PubMed] [Google Scholar]
- Taylor S. Anxiety sensitivity: Theory, research, and treatment of the fear of anxiety. Mahwah, NJ, US: Lawrence Erlbaum Associates Publishers; 1999. [Google Scholar]
- Taylor S, Zvolensky MJ, Cox BJ, Deacon B, Heimberg RG, Ledley DR, Cardenas SJ. Robust dimensions of anxiety sensitivity: Development and initial validation of the Anxiety Sensitivity Index-3. Psychological Assessment. 2007;19(2):176–188. doi: 10.1037/1040-3590.19.2.176. http://dx.doi.org/10.1037/1040-3590.19.2.176. [DOI] [PubMed] [Google Scholar]
- Thornton S, Troop M, Burgess AP, Button J, Goodall R, Flynn R, Easterbrook PJ. The relationship of psychological variables and disease progression among long-term HIV-infected men. International Journal of STD & AIDS. 2000;11(11):734–742. doi: 10.1258/0956462001915165. http://dx.doi.org/10.1258/0956462001915165. [DOI] [PubMed] [Google Scholar]
- Tucker JS, Burnam MA, Sherbourne CD, Kung FY, Gifford AL. Substance use and mental health correlates of nonadherence to antiretroviral medications in a sample of patients with human immunodeficiency virus infection. The American Journal of Medicine. 2003;114(7):573–580. doi: 10.1016/s0002-9343(03)00093-7. [DOI] [PubMed] [Google Scholar]
- US Department of Health and Human Services. International Classification of Disease and Related Problems. (10th) 1980 (Retrieved from ftp://ftp.cdc.gov/pub/Health_Statistics/NCHS/Publications/ICD-9/ucod.txt.)
- Van Servellen G, Chang B, Garcia L, Lombardi E. Individual and system level factors associated with treatment nonadherence in human immunodeficiency virus-infected men and women. AIDS Patient Care and STDs. 2002;16(6):269–281. doi: 10.1089/10872910260066705. http://dx.doi.org/10.1089/10872910260066705. [DOI] [PubMed] [Google Scholar]
- Varni SE, Miller CT, McCuin T, Solomon SE. Disengagement and engagement coping with HIV/AIDS stigma and psychological well-being of people with HIV/AIDS. Journal of Social and Clinical Psychology. 2012;31(2):123–150. doi: 10.1521/jscp.2012.31.2.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vassend O, Eskld A, Halvorsen R. Negative affectivity, coping, immune status, and disease progression in HIV iwected individuals. Psychology and Health. 1997;12(3):375–388. [Google Scholar]
- Waldrop-Valverde D, Valverde E. Homelessness and psychological distress as contributors to antiretroviral nonadherence in HIV-positive injecting drug users. AIDS Patient Care and STDs. 2005;19(5):326–334. doi: 10.1089/apc.2005.19.326. http://dx.doi.org/10.1089/apc.2005.19.326. [DOI] [PubMed] [Google Scholar]
- Watson D, O’Hara MW, Simms LJ, Kotov R, Chmielewski M, McDade-Montez EA, Stuart S. Development and validation of the Inventory of Depression and Anxiety Symptoms (IDAS) Psychological Assessment. 2007;19(3):253–268. doi: 10.1037/1040-3590.19.3.253. http://dx.doi.org/10.1037/1040-3590.19.3.253. [DOI] [PubMed] [Google Scholar]
- Watson D, Weber K, Assenheimer JS, Clark LA, Strauss ME, McCormick RA. Testing a tripartite model: I. Evaluating the convergent and discriminant validity of anxiety and depression symptom scales. Journal of abnormal psychology. 1995;104(1):3. doi: 10.1037//0021-843x.104.1.3. [DOI] [PubMed] [Google Scholar]
- Wechsler D. Manual of the Wechsler Adult Intelligence Scale–Revised (WAIS-R) New York: Psychological Corporation; 1981. [Google Scholar]
- Whetten K, Reif S, Ostermann J, Pence BW, Swartz M, Whetten R, Eron J. Improving health outcomes among individuals with HIV, mental illness, and substance use disorders in the Southeast. AIDS Care. 2006;1(18 Suppl):S18–S26. doi: 10.1080/09540120600839330. [DOI] [PubMed] [Google Scholar]
- WHO. Global summary of the AIDS epidemic, 2013. 2014 Retrieved June 24, 2015, 2014, from http://www.who.int/hiv/data/epi_core_dec2014.png?ua=1.
- World Health Organization. Schedules for clinical assessment in neuropsychiatry. In: van Gülick-Bailer M, editor. SCAN. Huber; 1995. [Google Scholar]
- Woods SP, Carey CL, Moran LM, Dawson MS, Letendre SL, Grant I. Frequency and predictors of self-reported prospective memory complaints in individuals infected with HIV. Archives of Clinical Neuropsychology. 2007;22(2):187–195. doi: 10.1016/j.acn.2006.12.006. http://dx.doi.org/10.1016/j.acn.2006.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu AW, Hays RD, Kelly S, Malitz F, Bozzette SA. Applications of the Medical Outcomes Study health-related quality of life measures in HIV/AIDS. Quality of Life Research. 1997;6(6):531–554. doi: 10.1023/a:1018460132567. [DOI] [PubMed] [Google Scholar]
- Yates JA, Clare L, Woods RT. Mild cognitive impairment and mood: A systematic review. Reviews in Clinical Gerontology. 2013;23(04):317–356. [Google Scholar]
- Zigmond AS, Snaith RP. The Hospital Anxiety and Depression Scale. Acta Psychiatrica Scandinavica. 1983;67(6):361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. http://dx.doi.org/10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- Zimpel RR, Fleck MP. Depression as a major impact on the quality of life of HIV-positive Brazilians. Psychology, Health & Medicine. 2014;19(1):47–58. doi: 10.1080/13548506.2013.772302. http://dx.doi.org/10.1080/13548506.2013.772302. [DOI] [PubMed] [Google Scholar]
- Zinbarg RE, Barlow DH, Brown TA. Hierarchical structure and general factor saturation of the Anxiety Sensitivity Index: Evidence and implications. Psychological Assessment. 1997;9(3):277. [Google Scholar]
- Zvolensky MJ, Baker KM, Leen-Feldner E, Bonn-Miller MO, Feldner MT, Brown RA. Anxiety sensitivity: Association with intensity of retrospectively-rated smoking-related withdrawal symptoms and motivation to quit. Cognitive Behaviour Therapy. 2004;33(3):114–125. doi: 10.1080/16506070310016969. [DOI] [PubMed] [Google Scholar]
- Zvolensky MJ, Kotov R, Antipova AV, Schmidt NB. Cross cultural evaluation of smokers risk for panic and anxiety pathology: A test in a Russian epidemiological sample. Behaviour Research and Therapy. 2003;41(10):1199–1215. doi: 10.1016/s0005-7967(03)00031-7. [DOI] [PubMed] [Google Scholar]


