Abstract
After decades of resistance there is now a genuine consensus that disease cannot be prevented or even successfully treated unless the role of stress is addressed alongside traditionally recognized factors such as genes and the environment. Measurement of allostatic load, which is quantified by the allostatic load score (ALS), is one of the most frequently used methods to assess the physiologic response to stress. Even though there is universal agreement that in the calculation of ALS, biomarkers from three categories should be included (cardiovascular, metabolic and immune), enormous variation exists in how ALS is calculated. Specifically, there is no consensus on which biomarkers to include or the method which should be used to determine whether the value of a biomarker represents high risk. In this Perspective, we outline the approach taken in 21 different NHANES studies.
Keywords: Allostatic Load Score, Stress, Biomarkers, Blood Pressure, A1C, C-Reactive Protein
PERSPECTIVE
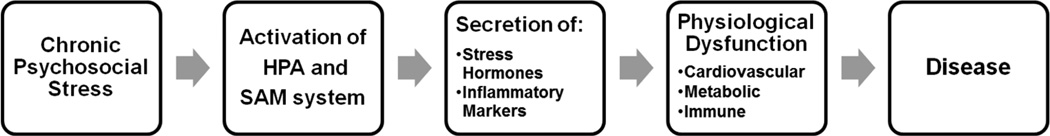
Chronic psychosocial stress activates both the hypothalamic-pituitary-adrenal axis (HPA) and the sympathetic-adrenal-medullary (SAM) system. The downstream result is the release of hormones and cytokines which exacerbate or promote cardiovascular, metabolic and immune disease (Figure) [1,2]. Measurement of allostatic load, which is quantified by the allostatic load score (ALS), is one of the most frequently used methods to assess the physiologic response to stress[1,2].
Figure 1. The Path from Psychosocial Stress to Disease.
HPA is an abbreviation for the hypothalamic-pituitary axis. SAM is the abbreviation for the sympathetic-adrenal medullary system.
This perspective on the calculation of ALS was written because we needed to evaluate the influence of stress on the metabolic health of African immigrants and rapidly recognized that guidelines on the calculation of ALS had not yet been established. In the absence of any consensus, and no previous publications on the calculation of ALS in African immigrants, we focused on publications which measured ALS using National Health and Nutrition and Examination Survey (NHANES) data. NHANES is a population-based, multiethnic cross-sectional survey conducted by the National Center for Health Statistics. We identified 13 publications. To determine whether these 13 publications were representative of how ALS was calculated using NHANES data, we did a PUBMED literature search on January 12, 2016 using the term “Allostatic Load Score and NHANES”. Twelve publications appeared. Of these 12 references, three did not use NHANES data and one was included in our original search. Therefore, this review on the calculation of ALS is based on 21 studies which used NHANES data in surveys of various lengths of time between 1988 and 2010[3–23].
Biomarkers included in the Allostatic Load Score
The 21 studies calculated ALS in 18 different ways using 26 different biomarkers (Tables 1 and 2). The number of biomarkers per ALS equation varied between 7 and 14 with at least one biomarker from three categories: cardiovascular, metabolic and immune. In the cardiovascular category, systolic and diastolic blood pressures were included in every equation except for one in which blood pressure was used as an outcome measure(Table 1)[23]. In the metabolic category, risk for diabetes was the primary focus and 16 of the18 equations used A1C to assess glycemic status. Of the two equations that did not use A1C, one equation used fasting glucose and the other did not include any measure of hyperglycemia[7,18]. In the immune category 17 out of the 18 equations used C-reactive protein (CRP) and one equation used WBC[12].
Table 1.
Frequency of 26 Biomarkers used in 18 Different Allostatic Load Score Equations
| Biomarkers | Frequency |
|---|---|
| Cardiovascular | |
| Systolic Blood Pressure | 17 |
| Diastolic Blood Pressure | 17 |
| Cholesterol | 15 |
| HDL | 15 |
| Triglycerides | 10 |
| Pulse | 7 |
| Homocysteine | 3 |
| Peak menstrual flow volume | 1 |
| Metabolic | |
| A1C | 16 |
| Albumin | 16 |
| Body Mass Index | 8 |
| eGFR | 7 |
| Waist to Hip Ratio | 7 |
| Waist Circumference | 4 |
| Creatinine | 3 |
| Fasting glucose | 2 |
| Alkaline phosphatase | 1 |
| Blood urea nitrogen | 1 |
| Cytomegalovirus optical density | 1 |
| Forced expiratory volume | 1 |
| HOMA-IR | 1 |
| Immune | |
| C-reactive protein | 17 |
| Asthma diagnosis | 1 |
| Fibrinogen | 1 |
| Herpes I & II antibodies | 1 |
| White blood cell count | 1 |
Table 2.
Eighteen ALS Equations from 21 NHANES Studies
| Equation Number |
Number of Bio- markers |
Biomarkersa | Authors | Survey Period (years) |
N | Age | % Male |
Race | Main Finding |
|---|---|---|---|---|---|---|---|---|---|
| A. High Risk for Each Biomarker Determined by Clinical Guidelines | |||||||||
|
1 |
14 |
CV: SBP, DBP, HDL,
pulse, total cholesterol, TG Metabolic: albumin, WHR, A1C, BMI, creatinine Immune: CRP, herpes simplex virus I & II |
Frei et al.b Reference 9 |
1988–1994 |
4620 |
≥20y |
49% |
White: 43% Black: 26% Mexican: 27% Other: 4% |
Even after adjustment for biological, socioeconomic, lifestyle and health variables, low vitamin D concentrations are associated with high ALS. |
|
2 |
9 |
CV: SBP, DBP, HDL,
pulse, total cholesterol Metabolic: Albumin, WHR, A1C Immune: CRP |
Frei et al.b Reference 9 |
1988–1994 |
14213 |
≥20y |
47% |
White: 43% Black: 26% Mexican: 27% Other: 4% |
Even after adjustment for biological, socioeconomic, lifestyle and health variables, low vitamin D concentrations are associated with high ALS. |
|
3 |
9 |
CV: SBP, DBP, HDL,
pulse, total cholesterol Metabolic: Albumin, WHR, A1C Immune: CRP |
Borrell et al. Reference 4 |
1988–1994 |
13715 |
≥25y |
48% |
Distribution by Race/Ethnicity not provided |
High ALS is associated with as increased risk of all-cause mortality. |
|
Merkin et al. Reference 14 |
1988–1994 |
13199 |
≥20y |
N/A |
White: 40% Black: 30% Mexican: 30% |
Blacks living in low
socioeconomic neighborhoods are consistently found to have high ALS and adverse biological risk profiles. |
|||
|
Rosenberg et al. Reference 17 |
1988–1994 |
3387 |
45–64y |
48% |
Distribution
by Race/Ethnicity not provided |
Low serum β-carotene concentrations are associated with high ALS. |
|||
|
Seeman et al. Reference 19 |
1988–1994 |
15578 |
≥20y |
49% |
White: 77% Black: 10% Mexican: 5% Other: 8% |
Low education and income are associated with high ALS. |
|||
|
4 |
9 |
CV: SBP, DBP, HDL,
pulse, total cholesterol Metabolic: BMI, A1C, Albumin Immune: CRP |
Chen et al. Reference 5 |
2005–2008 |
3330 |
≥18y |
53% |
White: 48% Black: 21% Mexican: 19% Other: 12% |
High ALS is associated with sleep apnea, insomnia, short sleep duration, and sleep disorders. |
|
Parente et al. Reference 15 |
1999–2008 |
4875 |
35–85y |
0% |
White: 75% Black: 25% |
Even after adjusting for demographic, behavorial and co-morbidities, breast cancer increases ALS in black women but not white women. |
|||
|
5 |
7 |
CV: SBP + DBP, HDL,
TG Metabolic: WC, fasting glucose Immune: CRP, fibrinogen |
Sabbah et al. Reference 18 |
1988–1994 |
6847 |
≥17y |
N/A |
Distribution by Race/Ethnicity not provided |
Higher allostatic load is associated with ischemic heart disease and periodontal disease. |
| B. High Risk for Each
Biomarker by Quartile
Analyses: (≥75th percentile for all variables except albumin, HDL and eGFR≤25th percentile) |
|||||||||
|
6 |
14 |
CV: SBP, DBP, HDL,
pulse, total cholesterol, TG Metabolic: albumin, WHR, A1C, BMI, creatinine Immune: CRP, herpes simplex virus I & II |
Frei et al.b Reference 9 |
1988–1994 |
4620 |
≥20y |
49% |
White: 43% Black: 26% Mexican: 27% Other: 4% |
Even after adjustment for biological, socioeconomic, lifestyle and health variables, low vitamin D concentrations are associated with high ALS. |
|
7 |
11 |
CV: SBP, DBP, HDL, TG,
total cholesterol, peak menstrual flow Metabolic: A1C, BMI, eGFR, albumin Immune: CRP |
Allsworth et alc Reference 3 |
1988–1994 |
2470 |
17–30y |
0% |
White: 28% Black: 33% Mexican: 35% Other: 4% |
Menarche at the age of 10 or younger is associated with higher ALS in young adult women. |
|
8 |
10 |
CV: SBP, DBP, HDL,
pulse, total cholesterol, homocysteine Metabolic: BMI, A1C, Albumin Immune: CRP |
Chyu et al. Reference 6 |
1999–2004 |
5765 |
≥18y |
0% |
White: 81% Black: 12% Mexican: 7% |
Compared to other racial/ethnic
groups, black women have the highest ALS. Mexican women not born in the US have lower ALS than their US-born counterparts. |
|
Upchurch et al. Reference 22 |
1999–2004 |
1680 |
40–59y |
0% |
White: 82% Black: 12% Mexican: 6% |
Higher levels of physical activity
and higher SES are associated with lower ALS. Black and Mexican American women have higher ALS than white women. |
|||
|
9 |
10 |
CV: SBP, DBP, TG,
total cholesterol, homocysteine Metabolic: BMI, A1C, albumin, eGFR Immune: CRP |
Geronimus et al. al. Reference 10 |
1999–2002 |
6586 |
18–64y |
51% |
White: 43% Black: 20% Other 37% |
Independent of income and throughout the life span, blacks have higher ALS than whites. |
|
Kaestner et al. Reference 11 |
1988–1994 |
6161 |
30–60y |
N/A |
White: 41% Black: 31% Mexican: 28% |
For Mexican immigrants, increased duration of stay in the United States is associated with higher ALS. |
|||
|
Slade et al. Reference 20 |
1999–2004 |
14184 |
≥18y |
47% |
White: 50% Black: 20% Hispanic: 27% Other: 3% |
Greater pain prevalence amongst low income groups is not explained by greater allostatic load. |
|||
|
10 |
10 |
CV: SBP, DBP, TG,
total cholesterol, homocysteine Metabolic: A1C, eGFR, albumin, WHR Immune: CRP |
Duru et al. Reference 8 |
1988–1994 |
4515 |
35–64y |
46% |
White: 58% Black: 42% |
Blacks have higher ALS than whites and this higher ALS in blacks explains, in part, the higher mortality rate experienced by blacks. |
|
11 |
9 |
CV: SBP, DBP, HDL,
pulse, total cholesterol Metabolic: Albumin, WHR, A1C Immune: CRP |
Frei et al.b Reference 9 |
1988–1994 |
14213 |
≥20y |
47% |
White: 43% Black: 26% Mexican: 27% Other: 4% |
Even after adjustment for biological, socioeconomic, lifestyle and health variables, low vitamin D concentrations are associated with high ALS. |
|
12 |
9 |
CV: SBP, DBP, HDL,
total cholesterol Metabolic: BMI, A1C, WC, albumin Immune: CRP |
Rainisch et al. Reference 16 |
1999–2008 |
8052 |
12–19y |
52% |
White: 71% Black: 16% Mexican: 13% |
Among adolescents,higher ALS is associated with older age and lower SES. Mexican American adolescents born in the United States have higher ALS than Mexican Americans born in Mexico. |
|
13 |
8 |
CV: SBP, DBP, HDL,
pulse, total cholesterol Metabolic: eGFR, albumin Immune: CRP |
Doamekpor et al. Reference 7 |
2001–2010 |
2897 |
≥20y |
48% |
Black: 100% (US-born: 95%; Foreign-born: 5%) |
Foreign-born blacks have lower ALS than American born blacks. |
|
C. High Risk for Each Biomarker by Quintile Analyses: (≥80th percentile for all variables except albumin and eGFR≤20th percentile) |
|||||||||
|
14 |
7 |
CV: HDL,
TG Metabolic: eGFR, albumin, A1C, WC Immune: CRP |
Zota et al. Reference 23 |
1999–2008 |
8194 |
40–65y |
49% |
White: 76% Black: 10% Hispanic: 10% Other: 4% |
Higher ALS appears to enhance the ability of lead to increase blood pressure |
|
D. Combination of Clinical Guidelines and Quartiles |
|||||||||
|
15 |
14 |
CV: SBP, DBP, HDL,
pulse, total cholesterol Metabolic: A1C, WHR, albumin, creatinine, cytomegalorvirus optical density, alkaline phosphatase, BUN, forced expiratory volume Immune: CRP |
Levine et al. Reference 13 |
1988–1994 |
9942 |
≥30y |
47% |
White: 83% Black: 9% Hispanic: 8% |
The model known as Biological Age is more highly associated with all-cause mortality and cancer mortality than either the Framingham Risk Score or ALS. |
|
16 |
11 |
CV: SBP, DBP, HDL, TG,
total cholesterol, peak menstrual flow Metabolic: A1C, BMI, eGFR, albumin Immune: CRP |
Allsworth et al.c Reference 3 |
1988–1994 |
2470 |
17–30y |
0% |
White: 28% Black: 33% Mexican: 35% Other: 4% |
Menarche at the age of 10 or younger is associated with higher ALS in young adult women. |
|
17 |
10 |
CV: SBP, DBP,
total cholesterol, TG, pulse Metabolic: WHR, A1C, albumin, eGFR Immune: WBC |
Kobrosly et al. Reference 12 |
1988–1994 |
4511 |
20–59y |
46% |
White: 36% Black: 30% Mexican: 30% Other: 4% |
Higher allostatic load which is referred to as physiologic dysfunction may be associated with a decline in working memory. |
|
E. Combination of Clinical Guidelines and ≥90th percentile for BP |
|||||||||
|
18 |
10 |
CV: SBP + DBP, HDL,
LDL, TG Metabolic: WC, fasting glucose, HOMA-IR, A1C Immune: CRP, asthma |
Theall et al. Reference 21 |
1999–2006 |
11866 |
12–20y |
50% |
White: 62% Black: 14% Hispanic: 17% Other: 7% |
Adolescents who live in high-risk neighborhoods have higher ALS than their counterparts in low-risk neighborhoods. |
Each biomarker is turned into a dichotomous variable with 1 point assigned if the biomarker is in the high risk range and 0 if the biomarker is not in the low risk range. Score can be 0 to 14 depending on the number of biomarkers in each equation.
Frei et al. used 4 different ALS formulations: (1) 14 variables with thresholds based on clinical guidelines (Equation 1), (2) 14 variables with thresholds based on quartiles (Equation 6), (3) 9 variables with thresholds based on clinical guidelines (Equation 2), (4) 9 variables with thresholds based on quartiles (Equation 11).
Allsworth et al. used 2 different ALS formulation: (1) 11 variables with all thresholds determined from high risk quartiles (Equation 7), (2) 11 variables with thresholds determined from a combination of clinical guidelines and high risk quartiles (Equation 16).
Calculation of Allostatic Load Score
Across all 21 publications, ALS was calculated by turning each biomarker into a dichotomous variable with 1 point given if the biomarker was in the high risk range and 0 if not; the higher the score the greater the impact of stress on physiologic dysregulation. Of the 26 variables used in the 18 equations, 24 variables were continuous and two were categorical. The two categorical variables were asthma, present or absent and antibodies to herpes simplex virus I or II, present or absent[9,21]. Depending on the number of variables included in the ALS equation, scores ranged between 0 and 14.
To determine if a biomarker was in the high risk range, the continuous variables had to be converted to dichotomous variables. In the 18 equations described in this Perspective, five different methods were used to convert continuous variables into dichotomous variables. Table 2 presents each equation according to the method chosen to convert continuous variables into their dichotomous counterparts. In Section A (Equations 1 through 5), thresholds were determined by study-specific clinical guidelines. In Section B (Equations 6 through 13), the population was divided into quartiles and high risk was defined as greater than the 75th percentile for all variables except for albumin, high density lipoprotein (HDL) and estimated glomerular filtration rate (eGFR). For these three variables, high risk was defined as a value less than the 25th percentile. In Section C (Equation 14), the population was divided into quintiles. Then the procedure described for Equations 6–13 was followed. In Section D (Equations 15 through 17), a combined approach was used. For some variables, high risk was based on study-specific clinical guidelines and for other variables, a quartile analysis was performed. In Section E (Equation 18), all variables were based on study-specific clinical guidelines except for blood pressure for which cut-offs were based on 90th percentile values.
With the exception of Chyu et al. [6], the general practice was to assign the high risk category for a variable if treatment was provided (i.e. anti-hypertensive, hypolipidemic or glucose lowering medication). Only one study made specific reference to sex-specific cut-offs[23].
Overview
After decades of resistance there is now a genuine consensus that disease cannot be prevented or even successfully treated unless the role of stress is addressed alongside traditionally recognized factors such as genes and the environment. Our goal was to illuminate the variety of approaches that have been taken within the context of NHANES data to calculate ALS.
Until a consensus on how to measure ALS is developed, each investigator will have to use a previously published ALS equation or develop a new one tailored to a specific research question. In calculating the score, we think it is preferable to decide on thresholds of risk for each biomarker by dividing the population into quartiles or quintiles rather than relying on clinical guidelines. We have made this judgment for two reasons. First, there are no nationally accepted clinical guidelines for the variables used to calculate ALS. Second, clinical guidelines are rarely population-specific. For example, six of the twenty-six biomarkers used in the calculation of ALS, vary by ethnicity[24–26]. These variables are: HDL, triglyceride (TG), body mass index (BMI), waist to hip ratio (WHR), waist circumference (WC) and eGFR. Standard clinical guidelines rarely take into account how differences by ethnicity in these variables affect cardiometabolic risk[25,26].
For our analyses of the physiologic response to stress in African immigrants, we decided to use the ALS equation proposed by Geronimus et al. and subsequently by Kaestner et al. [10,11]. Both of these studies were designed to address the effect of socioeconomic status, racism, ethnic identity and immigration on ALS[10,11].
Clearly, the role of stress in the development and treatment of disease needs to be considered at every level of health care, from the formulation of public policy to the design of initiatives to improve health care delivery at the community and individual level. Going forward, great benefit could accrue from the convening of an expert panel to work on developing a consensus statement on how to measure allostatic load.
Acknowledgments
Author Michelle T. Duong, Author Brianna A. Bingham, Author Paola C. Aldana, Author Stephanie T. Chung and Author Anne E. Sumner were supported by the intramural program of the National Institute of Diabetes and Digestive and Kidney Diseases, National Institutes of Health
Anne E. Sumner is also supported by the intramural program of the National Institute of Minority Health and Health Disparities.
Organization which sponsored the research: Intramural Program of the National Institutes of Health. The grant number/intramural study protocol is: 99-DK-0002.
Footnotes
Conflict of Interest Statement
Author Michelle T. Duong declares she has no conflict of interest.
Author Brianna A. Bingham declares she has no conflict of interest.
Author Paola C. Aldana declares she has no conflict of interest.
Author Stephanie T. Chung declares she has no conflict of interest.
Author Anne E. Sumner declare that they have no conflict of interest.
Ethical Responsibilities of Authors
This manuscript has not been submitted to more than one journal for simultaneous consideration and has not been published previously. No data have been fabricated or manipulated to support our conclusions. No data, text, or theories by others are presented as if they were the author’s own.
Consent to submit has been received explicitly from all co-authors. Authors whose names appear on the submission have contributed sufficiently to the scientific work and therefore share collective responsibility and accountability for the results.
References
- 1.Juster RP, McEwen BS, Lupien SJ. Allostatic load biomarkers of chronic stress and impact on health and cognition. Neuroscience and biobehavioral reviews. 2010;35(1):2–16. doi: 10.1016/j.neubiorev.2009.10.002. [DOI] [PubMed] [Google Scholar]
- 2.McEwen BS. Protective and damaging effects of stress mediators. N Engl J Med. 1998;338(3):171–179. doi: 10.1056/NEJM199801153380307. [DOI] [PubMed] [Google Scholar]
- 3.Allsworth JE, Weitzen S, Boardman LA. Early age at menarche and allostatic load: data from the Third National Health and Nutrition Examination Survey. Ann Epidemiol. 2005;15(6):438–444. doi: 10.1016/j.annepidem.2004.12.010. [DOI] [PubMed] [Google Scholar]
- 4.Borrell LN, Dallo FJ, Nguyen N. Racial/ethnic disparities in all-cause mortality in U.S. adults: the effect of allostatic load. Public health reports (Washington, DC : 1974) 2010;125(6):810–816. doi: 10.1177/003335491012500608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Chen X, Redline S, Shields AE, Williams DR, Williams MA. Associations of allostatic load with sleep apnea, insomnia, short sleep duration, and other sleep disturbances: findings from the National Health and Nutrition Examination Survey 2005 to 2008. Ann Epidemiol. 2014;24(8):612–619. doi: 10.1016/j.annepidem.2014.05.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Chyu L, Upchurch DM. Racial and ethnic patterns of allostatic load among adult women in the United States: findings from the National Health and Nutrition Examination Survey 1999–2004. J Womens Health (Larchmt) 2011;20(4):575–583. doi: 10.1089/jwh.2010.2170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Doamekpor LA, Dinwiddie GY. Allostatic load in foreign-born and US-born blacks: evidence from the 2001–2010 National Health and Nutrition Examination Survey. Am J Public Health. 2015;105(3):591–597. doi: 10.2105/AJPH.2014.302285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Duru OK, Harawa NT, Kermah D, Norris KC. Allostatic load burden and racial disparities in mortality. J Natl Med Assoc. 2012;104(1–2):89–95. doi: 10.1016/s0027-9684(15)30120-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Frei R, Haile SR, Mutsch M, Rohrmann S. Relationship of Serum Vitamin D Concentrations and Allostatic Load as a Measure of Cumulative Biological Risk among the US Population: A Cross-Sectional Study. PloS one. 2015;10(10):e0139217. doi: 10.1371/journal.pone.0139217. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Geronimus AT, Hicken M, Keene D, Bound J. "Weathering" and age patterns of allostatic load scores among blacks and whites in the United States. Am J Public Health. 2006;96(5):826–833. doi: 10.2105/AJPH.2004.060749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kaestner R, Pearson JA, Keene D, Geronimus AT. Stress, Allostatic Load and Health of Mexican Immigrants. Social science quarterly. 2009;90(5):1089–1111. doi: 10.1111/j.1540-6237.2009.00648.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Kobrosly RW, Seplaki CL, Jones CM, van Wijngaarden E. Physiologic dysfunction scores and cognitive function test performance in U.S. adults. Psychosomatic medicine. 2012;74(1):81–88. doi: 10.1097/PSY.0b013e3182385b1e. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Levine ME, Crimmins EM. A comparison of methods for assessing mortality risk. American journal of human biology : the official journal of the Human Biology Council. 2014;26(6):768–776. doi: 10.1002/ajhb.22595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Merkin SS, Basurto-Davila R, Karlamangla A, Bird CE, Lurie N, Escarce J, Seeman T. Neighborhoods and cumulative biological risk profiles by race/ethnicity in a national sample of U.S. adults: NHANES III. Ann Epidemiol. 2009;19(3):194–201. doi: 10.1016/j.annepidem.2008.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Parente V, Hale L, Palermo T. Association between breast cancer and allostatic load by race: National Health and Nutrition Examination Survey 1999–2008. Psycho-oncology. 2013;22(3):621–628. doi: 10.1002/pon.3044. [DOI] [PubMed] [Google Scholar]
- 16.Rainisch BK, Upchurch DM. Sociodemographic correlates of allostatic load among a national sample of adolescents: findings from the National Health and Nutrition Examination Survey, 1999–2008. The Journal of adolescent health : official publication of the Society for Adolescent Medicine. 2013;53(4):506–511. doi: 10.1016/j.jadohealth.2013.04.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Rosenberg N, Park CG, Eldeirawi K. Relationship of serum carotenoid concentrations with allostatic load as a measure of chronic stress among middle-aged adults in the USA. Public Health Nutr. 2015;18(2):313–321. doi: 10.1017/S1368980014000056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sabbah W, Watt RG, Sheiham A, Tsakos G. Effects of allostatic load on the social gradient in ischaemic heart disease and periodontal disease: evidence from the Third National Health and Nutrition Examination Survey. Journal of epidemiology and community health. 2008;62(5):415–420. doi: 10.1136/jech.2007.064188. [DOI] [PubMed] [Google Scholar]
- 19.Seeman T, Merkin SS, Crimmins E, Koretz B, Charette S, Karlamangla A. Education, income and ethnic differences in cumulative biological risk profiles in a national sample of US adults: NHANES III (1988–1994) Soc Sci Med. 2008;66(1):72–87. doi: 10.1016/j.socscimed.2007.08.027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Slade GD, Sanders AE, By K. Role of allostatic load in sociodemographic patterns of pain prevalence in the U.S. population. The journal of pain : official journal of the American Pain Society. 2012;13(7):666–675. doi: 10.1016/j.jpain.2012.04.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Theall KP, Drury SS, Shirtcliff EA. Cumulative neighborhood risk of psychosocial stress and allostatic load in adolescents. Am J Epidemiol. 2012;176(Suppl 7):S164–S174. doi: 10.1093/aje/kws185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Upchurch DM, Rainisch BW, Chyu L. Greater Leisure Time Physical Activity Is Associated with Lower Allostatic Load in White, Black, and Mexican American Midlife Women: Findings from the National Health and Nutrition Examination Survey, 1999 through 2004. Women's health issues : official publication of the Jacobs Institute of Women's Health. 2015;25(6):680–687. doi: 10.1016/j.whi.2015.07.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zota AR, Shenassa ED, Morello-Frosch R. Allostatic load amplifies the effect of blood lead levels on elevated blood pressure among middle-aged U.S. adults: a cross-sectional study. Environmental health : a global access science source. 2013;12(1):64. doi: 10.1186/1476-069X-12-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC., Jr Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120(16):1640–1645. doi: 10.1161/CIRCULATIONAHA.109.192644. 10.1161/CIRCULATIONAHA.109.192644 [doi] [DOI] [PubMed] [Google Scholar]
- 25.Sumner AE, Cowie CC. Ethnic differences in the ability of triglyceride levels to identify insulin resistance. Atherosclerosis. 2008;196(2):696–703. doi: 10.1016/j.atherosclerosis.2006.12.018. 10.1016/j.atherosclerosis.2006.12.018 [doi] [DOI] [PubMed] [Google Scholar]
- 26.Sumner AE, Finley KB, Genovese DJ, Criqui MH, Boston RC. Fasting triglyceride and the triglyceride-HDL cholesterol ratio are not markers of insulin resistance in African Americans. Arch Intern Med. 2005;165(12):1395–1400. doi: 10.1001/archinte.165.12.1395. 10.1001/archinte.165.12.1395 [doi] [DOI] [PubMed] [Google Scholar]