Abstract
Recent research suggests that statins might be useful in the process of wound healing, playing a positive immune-modulatory role, improving microvascular function and reducing oxidative stress. The aim of this pilot study was to evaluate the efficacy of topic application of Simvastatin-based cream in the treatment of chronic vascular cutaneous ulcers, comparing this type of treatment to a collagen-based dressing, proven to be effective for ulcer treatment. A total of 20 ulcers were studied in 2 Groups of randomly-chosen patients for a period of one month. In the first Group a 0.5% Simvastatin-based cream was topically administered, while the second Group (control) was treated with an absorbable type I bovine collagen-based medication. Each week, wound healing progress was observed in both Groups, and the ulcers photographed. Wound healing rate was calculated by considering the absolute change in area and by the formula “healing ratio (%) = [(Area0 − Areat4)/Area0] × 100,” both sets of data being related to the days comprised in the study in order to calculate healing rate per day. Statistical analysis was performed by Student t test. Study endpoint equaling the time-course changes of ulcer areas. At the end of the study, when considering absolute change in area, the experimental Group appeared to heal better and faster than the control Group although differences between the Groups were not statistically significant. Conversely, rates of wound healing in the experimental and control Groups were 46.88% and 64% respectively, revealing statistically significant differences. (P < 0.05). In conclusion, topic application of a simvastatin-based cream proved to be well- tolerated but not effective in the management of vascular leg ulcers in a 4 week-period.
Keywords: Chronic skin ulcers, Vascular skin ulcers, Topic simvastatin
Introduction
Wound healing is a dynamic and complex process that involves a well-coordinated, highly regulated series of events, including inflammation, tissue formation, revascularization, and tissue remodeling.1 Processes such as angiogenesis, activation, migration, and proliferation of fibroblasts, myofibroblasts and endothelial cells, formation of granulation tissue and wound contraction are involved.2, 3 Inflammation is one of the important causes of delayed wound healing due to oxidative stress, proteolysis and accumulation of toxic substances that occur during inflammation.4 In addition, bacterial infection has a detrimental effect on the wound healing process by preventing angiogenesis and secretion of plasminogen activator and proteolytic enzymes that may affect the extracellular matrix, blocking wound contraction.5, 6
Recently, it has been demonstrated that statins have pleiotropic effects that could be useful for wound healing.7, 8
Statins are hydroxi-3-methylglutaril-coenzyme A reductase (HMG-CoA), the enzyme involved in the first step of cholesterol biosynthesis, inhibitors that are primarily used for lowering circulating cholesterol levels.9
Nowadays, statins are considered a potentially novel therapeutic approach for different pathological conditions such as psoriasis, sepsis, alopecia, wound healing and other inflammatory diseases7, 8 on account of their pleiotropic effects that are independent of their lipid-lowering activities.
Oral statins can cause a number of adverse effects such as myopathy and liver toxicity, so topical delivery of statins has been proposed as a reasonable alternative to oral administration in order to prolong their valuable effects and reduce the incidence of adverse effects.8
Several studies1, 7, 8, 9 have proved that statins may play an important role in the wound healing process: Topic application of statins on a wound may improve angiogenesis, lymph angiogenesis and microvascular function, reduce oxidative stress and infection, playing an immune-modulatory role and, thanks to the above-mentioned reasons, may accelerate and benefit the healing process. Different types of statins have been evaluated but Simvastatin has been utilized and studied the most frequently.7, 9 Anyhow, topical Simvastatin is not available in market by prescription and it is just experimental at present time.
The aim of this pilot study was to evaluate whether topic application of 0.5% Simvastatin had a positive impact on wound healing in the management of chronic vascular lower limb cutaneous ulcers.
Materials and Methods
Patients with chronic non-healing vascular cutaneous wounds were eligible for participation in this study. The trial was conducted in compliance with the Declaration of Helsinki and the Guidelines for Good Clinical Practice; all enrolled patients provided written informed consent before inclusion in the study. Twenty ulcers were considered: an experimental Group of 11 ulcers treated with 0.5% Simvastatin-based cream and 9 ulcers as a control Group, treated with an absorbable type I bovine collagen-based medication (Suprasorb C, Lohmann & Rauscher, Neuwied, Germany). The two Groups were compared weekly for a period of one month.
The experimental Group comprised 11 chronic lower limb vascular cutaneous ulcers on 7 randomly-enrolled patients. The Control group was composed of 8 randomly-enrolled patients, presenting a total of 9 vascular chronic cutaneous ulcers, treated with the afore-mentioned collagen-based wound dressing, proven for its efficacy in skin ulcer management.
Patient Enrollment
Patient Inclusion Criteria
Patients presenting with chronic cutaneous lower limb ulcers of vascular etiology lasting for at least 3 months. Sample size was calculated on the basis of an expected 50% healing rate in the simvastatin group and 30% in the placebo group after a month's treatment. Seven patients with 11 ulcers were randomly assigned to the experimental Group: Arterial insufficiency was the main etiology for five patients, whereas the other two patients suffered from venous deficiency. The control Group consisted in eight patients with 9 ulcers (4 arterial insufficiency, 5 venous insufficiency), who were treated with collagen-based medications.
Patient Exclusion Criteria
Patients with less than 18 years of age, or with wound infection, ulcers not due to vascular conditions, severe cardiac, respiratory, gastro-intestinal, liver or renal diseases or malignancy, history of intolerance to statin administration were excluded from the study. Pregnant women and nursing mothers were excluded.
Simvastatin-based Cream
The Simvastatin-based cream10 was prepared as follows:
Per 100 g: 0.5 g Simvastatin; 1 g Dimethicone 350; 5 g Caprylic/capric triglycerides; 5 g Panthenol; 2 g Polyacrylamide/isoparaffin; 86.5 g Distilled water.
Experimental Procedures and Treatment
Patients were followed for 4 weeks and treated weekly as follows:
-
•
Control group with an absorbable type I bovine collagen-based sponge (suprasorb C);
-
•
Experimental group with the above-mentioned 0.5% Simvastatin-based cream;
-
•
Patients with two lesions underwent the same treatment on each lesion.
Percentage change in area over the first 4 weeks of a given treatment is an easy-to-use and predictive measure for complete wound healing which varies independently of both wound size and duration, providing the best combination of positive and negative predictive values in this regard.10, 11, 12
Wound Management
During the weekly follow-ups, wound management consisted in:
-
•
Topical disinfection with chlorhexidine 0.05%;
-
•
Mechanical debridement when necessary (necrotic/slough tissue within or adjacent to the ulcers) in order for healthy tissue to be exposed;
-
•
Application of the wound dressing;
-
•
Elastic bandage (to keep in place until the following check-up);
-
•
The procedures were performed under aseptic conditions.
The primary endpoint of the study was the time-course changes of ulcer areas at one month. Secondary endpoints were complete ulcer healing and the onset of adverse events.
Measurements and Wound healing Rate Calculation
A total of 162 digital images were taken. As a scale comparison, a meter was placed at the side on the same plane as the lesion while taking the picture. Pictures were taken by placing the digital Camera on a parallel plane to the plane of the wound.
Wound progression was analyzed by studying the ulcer width-area calculated by the ImageJ 1.48 software (NIH, Bethesda, Maryland, USA) from pictures taken at the beginning of each weekly examination. Wound areas were calculated by tracing the perimeter of the wounds in the pictures using the same software.
The wound healing rate was calculated by the formulas5:
Areat4 is the wound area at weeks 4. Area0 is the baseline wound area. All wound areas were in cm2 and t was measured in days.
Statistical Analysis
Statistical analysis was performed with Prism 6 (GraphPad Software Inc., La Jolla, CA, USA) software. Results were analyzed with Column Statistics and Student t test. Statistical significance was assumed at p < 0.05.
Results
Neither the experimental group nor the control group experienced side effects, adverse reactions to topical application of simvastatin, or infections during the study (Table 1, Table 2).
Table 1.
Baseline Demographic and Health Characteristics.
| Characteristics | Control group (n = 8) | Experimental group (n = 7) |
|---|---|---|
| Demographic | ||
| Age (mean, range) | 73,5 (55–91) | 66,57 (38–91) |
| Female (n; %) | 5; 62,5% | 2; 28,,6% |
| Male (n; %) | 3; 37,5% | 5; 71,4% |
| Comorbidities/health | ||
| Cardiac disease (n; %) | 1; 12,5% | 2; 28,6% |
| Obesity (n; %) | 0; 0% | 1; 14,3% |
| Infectious disease (HIV, HCV) (n; %) | 1; 12,5% | 1; 14,3% |
| Multiple wounds (n; %) | 1; 12,5% | 4; 57,1% |
Table 2.
Ulcer Characteristics.
| Ulcers characteristics | Control group (n = 8) | Experimental group (n = 7) |
|---|---|---|
| Ulcer, n= | 9 | 11 |
| Ulcer area t0 (mean; range) ± SD | 10,16 (3,01–32,49) ± 9,22 | 22,12 (3–73,24) ± 18–87 |
| Ulcer duration (mean; range) | 13,56 months (3–24) | 14,5 months (3–72) |
| Ulcer aetiologies | ||
| Arterial (n; %) | 3 (33,3%) | 9 (81,8%) |
| Venous (n; %) | 5 (55,6%) | 2 (18,2%) |
| Diabetes (n; %) | 1 (11,1%) | 0 (0%) |
| Ulcer localization | ||
| Leg (n; %) | 2 (22,2%) | 5 (45,4%) |
| Foot (n; %) | 1 (11,1%) | 0 (0%) |
| Malleolus (n; %) | 5 (55,6%) | 6 (54,6%) |
Area at t0
Considering the baseline wound area at t0, the mean area of the experimental group was higher (22,12 ± 18,87 cm2) than that of the control group (10,16 ± 9,22 cm2) as shown in Table 3. However, these differences were not statically significant (p value > 0,05).
Table 3.
Wound Areas at Initial Presentation.
| Characteristics | Control group (n = 8) | Experimental group (n = 11) | p value |
|---|---|---|---|
| Area T0 (mean ± SD) | 10,16 ± 9,22 cm2 | 22,12 ± 18,87 cm2 | 0.1002 |
| Range | 3,09–32,49 cm2 | 3–73,24 cm2 | 0.1002 |
| Median | 6,62 cm2 | 19,87 cm2 | 0.1002 |
| Sum | 91,47 cm2 | 243,3 cm2 | 0.1002 |
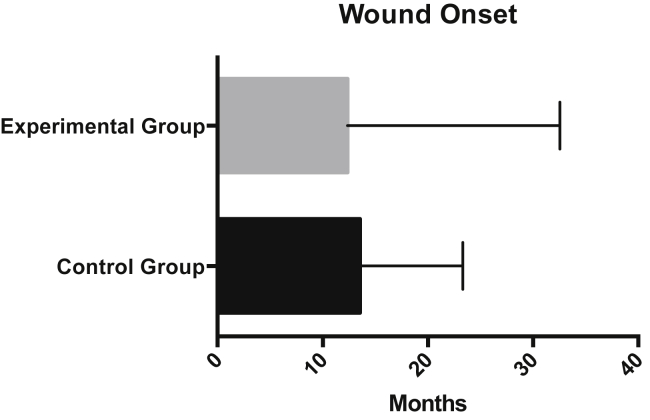
Furthermore, the mean of wound onset in the two Groups was similar and the difference between the two Groups was not statistically significant (p > 0,05) as shown in Table 4.
Table 4.
Wound Onset.
| Characteristics | Control group (n = 9) | Experimental group (n = 11) | p value |
|---|---|---|---|
| Mean ± SD | 13,56 ± 9,76 | 12,36 ± 20,18 | 0,87 |
| Range | 3–24 | 3–72 | 0,87 |
Wound Healing Rate
A variety of methods have been used to calculate wound healing rates in clinical trials.10, 11, 12, 13 Most commonly a measure of the change in two-dimensional area of the wound is used and is expressed either as a raw number (cm2) or as a percentage of initial wound area. These measurements are usually given per unit of time. This is quantified either as time until total healing of each wound or by calculating the percentage of wounds that healed during the study time.13, 14, 15 The use of total wound healing as an endpoint in clinical studies has several drawbacks. Wound healing is often a lengthy process; observing wounds until they completely heal is cumbersome and frequently takes a significant amount of time. In this study, we considered the measurements of change of the initial wound area expressed as a raw number, as a percentage, and per unit of time (area healed/day or % area healed/day).
Firstly, absolute change in area and healing rate were measured with the following formulas:
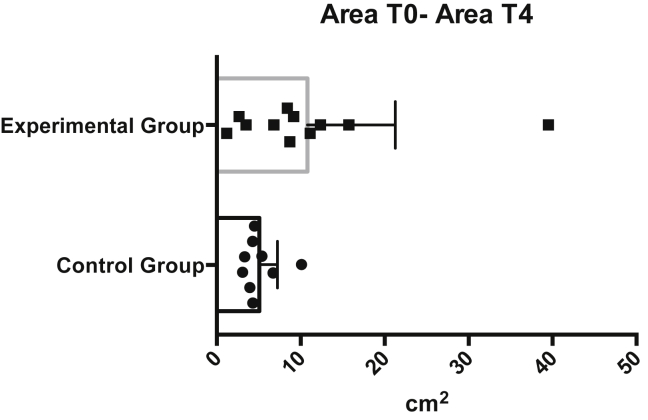
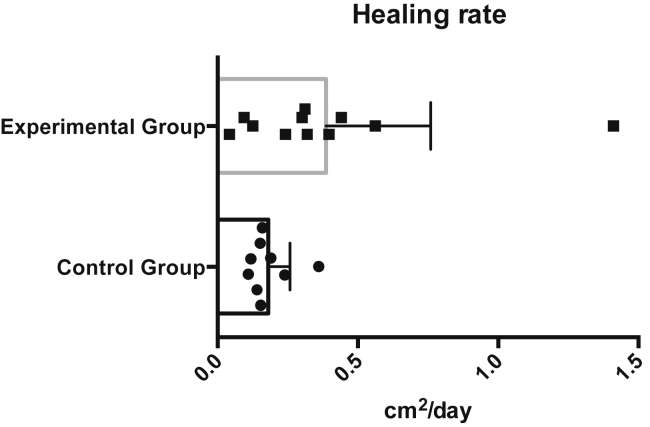
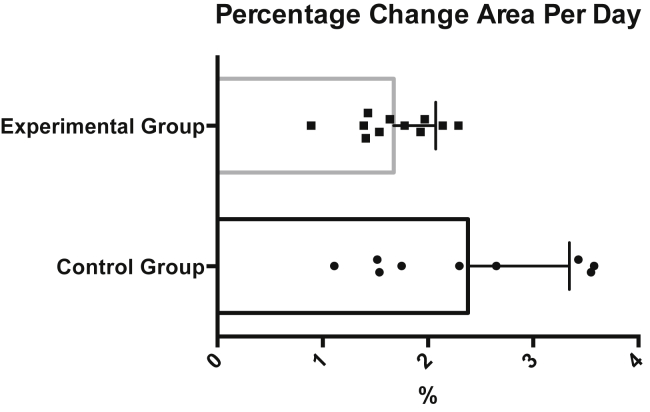
The values of the two groups were then compared, as shown in Table 5, Table 6. The experimental Group appeared to heal better and faster then the control Group but differences between the Groups were not statistically significant (p > 0,05).
Table 5.
Absolute Change in Area: Area0 – Areat4 (cm2).
| Characteristics | Control group (n = 9) | Experimental group (n = 11) | p value |
|---|---|---|---|
| Mean ± SD | 5,06 ± 2,18 | 10,83 ± 10,45 | 0,123 |
| Range | 3,07–10,1 | 1,19–39,50 | 0,123 |
| Median | 4,3 | 8,71 | 0,123 |
| Sum | 45,52 | 119,1 | 0,123 |
Table 6.
Healing Area per Day: (Area0 − Areat4)/t (cm2).
| Characteristics | Control group (n = 9) | Experimental group (n = 11) | p value |
|---|---|---|---|
| Mean ± SD | 0,18 ± 0,08 | 0,39 ± 0,37 | 0,124 |
| Range | 0,11–0,36 | 0,04–1,41 | 0,124 |
| Median | 0,15 | 0,31 | 0,124 |
It appears intuitively obvious that a smaller wound will take less time to heal. Literature is inconclusive on this point. Stacy et al found no correlation between initial wound size and complete wound healing.15 However, calculations of wound healing rate during a period of time on the basis of area are also inaccurate when wounds of differing size and shape are compared. A relatively small amount of healing in a large wound, in fact, will produce a great change in total area when compared with a small wound. To overcome this discrepancy, we calculated the ratio of healing by also considering the initial wound area with the following formulas, which have already been utilized in other studies for measuring wound healing rate.4
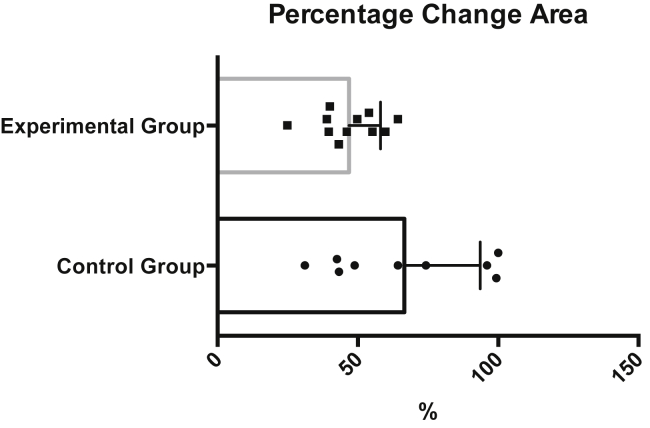
The results were compared as shown in Table 7, Table 8. With these formulas, which considered the initial wound area, the control Group healed better and faster than the experimental one, the differences between the two Groups being statistically significant (p < 0,05). One wound in the control Group healed completely during the study period.
Table 7.
Wound Area (%).
| Characteristics | Control group (n = 9) | Experimental group (n = 11) | p value |
|---|---|---|---|
| Mean ± SD | 64% ± 26,97% | 46,88% ± 11,23% | 0,0397 |
| Range | 31%–100% | 24,85%–64,27% | 0,0397 |
| Median | 64,26% | 46,03% | 0,0397 |
Table 8.
Healing Rate (%).
| Characteristics | Control group (n = 9) | Experimental group (n = 11) | p value |
|---|---|---|---|
| Mean ± SD | 2,38% ± 0,96% | 1,67% ± 0,4% | 0,0395 |
| Range | 1,11%–3,58% | 0,89%–2,29% | 0,0395 |
| Median | 2,3% | 1,67% | 0,0395 |
Discussion
The effectiveness of statins appears to involve restoring or improving endothelial function through the attenuation of oxidative stress, thereby increasing the bioavailability of nitric oxide, improving microvascular function or inhibiting inflammatory response. All those processes are independent of lipid-lowering effects.16 In addition, statins cause a down regulation of the periendothelin-1 mRNA level in endothelial cells and thus reduce the synthesis of endothelin 1 (ET-1) which is a powerful vasoconstrictor; moreover, they reduce vascular response to angiotensin 2 and interfere with platelet aggregation. Statins have also been demonstrated to promote the neovascularization of ischemic tissue in normocholesterolemic animals by further increasing activity of endothelial progenitor cells (EPCs).16
Simvastatin has been shown to exhibit important immunomodulatory effects, lowering the expression of TNFalfa and IL-1b, and leukocyte infiltration.7 Statins appear to reduce the length of time needed for wound healing following surgery (13.0 days versus 18.7 days), potentially resulting in smaller scars.17
In another study, Simvastatin has been found to enhance vascular endothelial growth factor (VEGF) production and improve wound healing18; the effects of topical simvastatin on angiogenesis and lymph angiogenesis in animal models have also been evaluated and findings demonstrate that the topical application of Simvastatin promotes both angiogenesis and lymph angiogenesis in vivo.19 However, Simvastatin did not promote proliferation of lymphatic endothelial cells in vitro: the effect on lymph angiogenesis is mediated by the production of VEGF-C by infiltrating macrophages, the infiltration of which is stimulated by Simvastatin.19
In conclusion, several studies have proved that topical application of statins with avoidance of systemic adverse effects may be useful for cutaneous wound healing, in which angiogenesis plays a pivotal role.16
In the present pilot study, we considered two Groups of patients for a total of 20 ulcers of vascular etiology for one month: one experimental Group treated with a Simvastatin-based cream and one Group as control, treated with a collagen-based dressing. The ulcers were checked and photographed every week and the areas calculated and compared in order to measure the absolute change in wound area and the healing rate during this period.
During the study period, no infection, side effects or adverse reactions occurred in any patient.
According to our data, no statistically significant differences were found between the two Groups regarding absolute changes in wound areas and healing areas per day, while the percentages of changes in area and of healing rates were better in the control Group compared to the experimental one.
Conclusions
Our pilot study did not demonstrate that topic application of a simvastatin-based cream improved the healing process compared to a collagen-based dressing; at the same time, however, neither were there any side effects or adverse reactions. The topical administration of statins seems very promising and further studies are needed in order to find alternative topical delivery, formulation and application methods, capable of maximizing potential beneficial effects. To conclude, according to our data, topical application of a simvastatin-based cream proved to be well tolerated but not effective in the management of chronic vascular leg ulcers in a four-week-period. Anyhow, it should be stressed that our small sample size limited power to detect difference. Also, inclusion of both arterial and venous ulcers complicates results, since arterial ulcers are well known to heal difficultly without revascularization. A study including only venous ulcers might have shown different results. Our data should be supported by further studies involving a sufficient number of patients to provide more powerful results. Further issues should also be evaluated, e.g., whether conditions such as peripheral arterial disease, advanced age, diabetes, or hypertension attenuate the response to Simvastatin.
Footnotes
None of the authors has a conflict of interest or a financial interest in any of the products, devices, or drugs mentioned in this manuscript.
References
- 1.Toker S., Gulcan E., Kasim Çaicl M., Olgum E.G., Erbilen E., Özay Y. Topical atorvastatin in the treatment of diabetic wounds. Am J Med Sci. 2009;338:201–204. doi: 10.1097/MAJ.0b013e3181aaf209. [DOI] [PubMed] [Google Scholar]
- 2.Clark R.A.F. Wound repair. Overview and general considerations. In: Clark R.A.F., editor. The Molecular and Cellular Biology of Wound Repair. 2nd ed. Plenum; New York: 1996. pp. 3–50. [Google Scholar]
- 3.Martin P. Wound healing aiming for perfect skin regeneration. Science. 1997;276:75–81. doi: 10.1126/science.276.5309.75. [DOI] [PubMed] [Google Scholar]
- 4.Eming S.A., Krieg T., Davidson J.M. Inflammation in wound repair: molecular and cellular mechanisms. J Invest Dermatol. 2007;127:514–525. doi: 10.1038/sj.jid.5700701. [DOI] [PubMed] [Google Scholar]
- 5.Redd M.J., Cooper L., Wood W., Stramer B., Martin P. Wound healing and inflammation: embryos reveal the way to perfect repair. Philos Trans R Soc Lond B Biol Sci. 2004;359:777–784. doi: 10.1098/rstb.2004.1466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Perry A.W., Sutkin H.S., Gottlieb L.D. Skin graft survival. The bacterial answer. Ann Plast Surg. 1989;22:479–483. doi: 10.1097/00000637-198906000-00003. [DOI] [PubMed] [Google Scholar]
- 7.Filho A., Egito B., Brandão-Neto I., Medeiros A. Simvastatin improves the healing of infected skin wounds of rats. Acta Cir Bras. 2007;22:57–63. doi: 10.1590/s0102-86502007000700012. [DOI] [PubMed] [Google Scholar]
- 8.Schadi Farsaei S., Khalili H., Farboud E.S. Potential role of statins on wound healing: review of the literature. Int Wound J. 2012;9:238–247. doi: 10.1111/j.1742-481X.2011.00888.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Asai J., Takenaka H., Hirakawa S. Topical Simvastatin accelerates wound healing in diabetes by enhancing angiogenesis and lymphangiogenesis. Am J Pathol. 2012;181:2217–2224. doi: 10.1016/j.ajpath.2012.08.023. [DOI] [PubMed] [Google Scholar]
- 10.Kantor J., Margolis D.J. A multicentre study of percentage change in venous leg ulcer area as a prognostic index of healing at 24 weeks. Br J Dermatol. 2000;142:960–964. doi: 10.1046/j.1365-2133.2000.03478.x. [DOI] [PubMed] [Google Scholar]
- 11.Cardinal M., Eisenbud D.E., Phillips T., Harding K. Early healing rates and wound area measurements are reliable predictors of later complete wound closure. Wound Repair Regen. 2008;16:19–22. doi: 10.1111/j.1524-475X.2007.00328.x. [DOI] [PubMed] [Google Scholar]
- 12.Flanagan M. Improving accuracy of wound measurement in clinical practice. Ostomy Wound Manage. 2003;49:28–40. [PubMed] [Google Scholar]
- 13.Gelfand J.M., Hoffstad O., Margolis D.J. Surrogate endpoints for the treatment of venous leg ulcers. J Invest Dermatol. 2002;119:1420–1425. doi: 10.1046/j.1523-1747.2002.19629.x. [DOI] [PubMed] [Google Scholar]
- 14.Gorin D.R., Cordts P.R., LaMorte W.W., Menzoian J.O. The influence of wound geometry on the measurement of wound healing rates in clinical trials. J Vasc Surg. 1996;23:524–528. doi: 10.1016/s0741-5214(96)80021-8. [DOI] [PubMed] [Google Scholar]
- 15.Stacey M.C., Burnand K.G., Layer G.T., Pattison M., Browse N.L. Measurement of the healing of venous ulcers. Aust N Z J Surg. 1991;61:844–848. doi: 10.1111/j.1445-2197.1991.tb00169.x. [DOI] [PubMed] [Google Scholar]
- 16.Fujii T., Onimaru M., Yonemitsu Y., Kuwano H., Sueishi K. Statins restore ischemic limb blood flow in diabetic microangiopathy via eNOS/NO upregulation but not via PDGF-BB expression. Am J Physiol Heart Circ Physiol. 2008;294:H2785–H2791. doi: 10.1152/ajpheart.00149.2008. [DOI] [PubMed] [Google Scholar]
- 17.Gulcan E., Gulcan A., Erbilen E., Toker S. Statins may be useful in diabetic foot ulceration treatment and prevention. Med Hypotheses. 2007;69:1313–1315. doi: 10.1016/j.mehy.2007.03.022. [DOI] [PubMed] [Google Scholar]
- 18.Society of Thoracic Surgeons . ScienceDaily; 31 July 2014. Statins May Improve Wound Healing Following Cardiac Surgery.www.sciencedaily.com/releases/2014/07/140731094451.htm [Google Scholar]
- 19.Bitto A., Minutoli L., Altavilla D. Simvastatin enhances VEGF production and ameliorates impaired wound healing in experimental diabetes. Pharm Res. 2008;57:159–169. doi: 10.1016/j.phrs.2008.01.005. [DOI] [PubMed] [Google Scholar]