Abstract
Introduction
The aim of the study was to compare clinical and radiological outcomes of arthroscopic single-bundle versus double-bundle anterior cruciate ligament (ACL) reconstruction.
Patient and methods
60 patients with isolated ACL injury were divided into single bundle (SB) (n = 30) and double bundle (DB) reconstruction groups (n = 30) and operated between July 2009 and July 2012. Outcome evaluation was performed using GNRB arthrometer, International Knee Documentation Committee & Lysholm scale. Rotational stability was determined by lateral pivot-shift test. Magnetic resonance imaging (MRI) was performed postoperatively to compare the reconstructed ACL graft orientation.
Results
Average follow-up was 34.8 months in SB and 36.2 months in DB group. At final follow-up, mean Lysholm score was 94.13 ± 2.67 in SB and 93.13 ± 3.31 in DB group (P value = 0.202, statistically non-significant). All patients in both groups were in grade A or B according to objective IKDC scores. Mean differential anterior tibial translation was 1.45 ± 0.6 mm in SB and 1.17 ± 0.8 mm in DB group (P value = 0.105, NS). All had negative pivot shift test in DB group while 2 patients had positive pivot shift in SB group. MRI of operated knees showed that values of mean sagittal ACL graft–tibial angle and mean coronal ACL graft–tibial angle were comparable in both groups (P value > 0.05, NS).
Conclusions
There was no statistically significant difference concerning knee stability, knee scores, subjective evaluations, and MRI evaluation of graft inclination angles between single- and double-bundle ACL reconstruction groups at an average of 35 months of follow-up.
Keywords: Single bundle, Double bundle, ACL, Clinico-radiological
1. Introduction
Reconstruction of anterior cruciate ligament (ACL) is the most frequently performed reconstructive surgery in the knee. Single-bundle ACL reconstruction (SBACLR) has stood the test of time and has provided excellent success rates, but some authors have noted residual instability and patient dissatisfaction after surgery (Table 1). In recent years, double-bundle ACL reconstruction (DBACLR) has gained in popularity. The proposed benefits of double-bundle reconstruction to better restore knee kinematics than single-bundle ACL reconstructions follow from biomechanical studies that suggest that each bundle – anteromedial (AM) and posterolateral (PL) – makes a unique kinematic contribution to knee function.1 The two bundles function together, but the AM bundle provides the major anterior restraint, whereas the PL bundle functions at extension and contributes more to rotational stability.2 An in vivo kinematics study has shown that single-bundle ACL reconstruction, which most closely imitates AM bundle reconstruction, can successfully restore anterior knee stability but does not sufficiently bring back rotational stability.3 Several clinical trials and meta-analyses have highlighted the advantages of DBACLR in achieving better anterior knee stability and rotational stability in the ACL-deficient knee compared with SBACLR but found no significant difference in the functional outcomes after the two procedures.4, 5, 2 A Cochrane database systemic review in 2012 concluded that there is insufficient evidence to determine the relative effectiveness of double-bundle over single-bundle reconstruction for ACL rupture in adults.6 There is also a dearth of published prospective trials in Indian population that compare outcomes of SB and DB ACL reconstruction.
Table 1.
Randomized controlled trials comparing DB and SB ACL reconstruction.
| Study | Year published | Number of patients | Follow up | Outcome |
|---|---|---|---|---|
| Yubao Ma21 | 2014 | 108 | 32 months | No difference |
| Koga et al.22 | 2015 | 65 | 14 months | Better rotational stability in DB group |
| Järvelä et al.23 | 2008 | 77 | 2 years | Better rotational stability, fewer graft failures in DB group |
| Yagi et al.24 | 2007 | 60 | 1 year | Better rotational stability in DB group |
| Streich et al.25 | 2008 | 50 | 2 years | No difference |
| Siebold et al.10 | 2008 | 70 | 19 months | Better rotational stability and objective knee scores in DB group |
| Sastre et al.26 | 2012 | 40 | 2 years | No difference |
| Zaffagnini et al.27 | 2011 | 79 | 8 years | Better functional scores, less degenerative changes in DB group |
| Wang et al.28 | 2014 | 64 | 10 months | No difference |
| Present study | 2015 | 60 | 35 months | No clinic radiological difference |
In both single and double bundle ACL reconstructions, exact anatomical positioning of the graft tunnels resulting into anatomic inclination angles of the grafts is essential for optimal clinical outcomes. Incorrect placement of the grafts is a common primary reason for early graft failure, lack of extension and flexion, and residual instability after ACLR.7, 8 Recently, many anatomical studies have evaluated the femoral and tibial insertion sites of the ACL bundle to determine correct tunnel placement when performing ACL reconstruction with the single or double-bundle technique.9, 10, 11 Postoperative MRI scanning is a useful imaging tool to detail the graft orientation and inclination angles apart from its footprint size and tunnel location. However, there have been very few recently published studies that compare the graft morphology between reconstructed SB and DB ACLR using postoperative MRI scans.12, 13
In view of these, the present prospective study was done to evaluate the clinical and radiological outcomes of arthroscopic DBACLR compared with that of anatomical SBACLR. We hypothesized that DBACLR with hamstring tendon autograft using two tibial tunnels and two femoral tunnels would be advantageous in restoring anterior and rotational stability, as well as providing better subjective as well as objective clinical results, compared with anatomical single-bundle reconstruction.
2. Patients and methods
From July 2009 to July 2012, 60 ACL reconstruction surgeries were performed by the senior surgeon according to a prospective study design. The patients were sequentially selected to undergo either single-bundle or double-bundle reconstruction in an alternate manner based on their order of admittance to our hospital. Inclusion criteria were primary ACL tear with no combined posterior cruciate ligament injury, lateral collateral ligament injury, PL rotatory instability, or fracture around knee. Exclusion criteria were no previous knee ligament surgery, no arthritic changes, no subtotal or total meniscectomy, no malalignment, and a normal contralateral knee. Patient's height less than 174 cm, ACL tibial insertion site of less than 12 mm, and a PCL dominant intercondylar notch was regarded as contraindication for performing a DBACLR.
All patients underwent a preoperative assessment including a history, clinical examination, knee examination (Lachman test, Pivot shift), Lysholm score,14 International Knee Documentation Committee (IKDC) scale15 (subjective as well as objective), standard radiograph (AP and lateral view), and magnetic resonance imaging (MRI) (Fig. 3, Fig. 4). All patients underwent arthroscopic ACL reconstruction (SB or DB) under regional anesthesia after obtaining written consent from the patients.
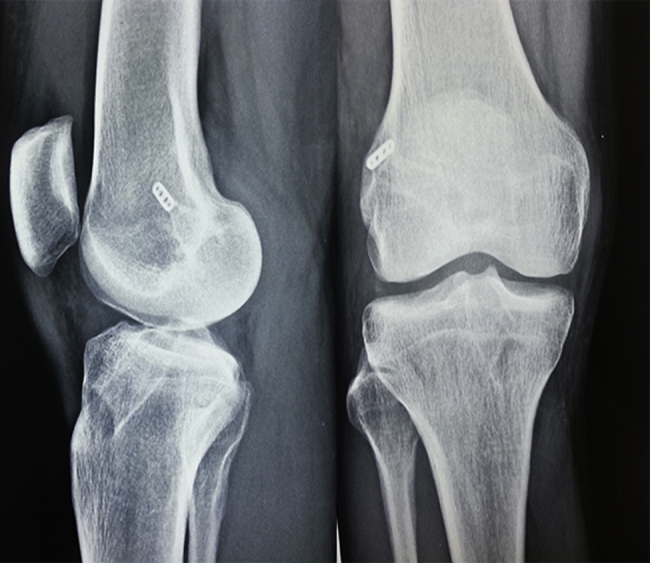
Fig. 3.

MRI imaging of single bundle ACL reconstructed knee showing coronal and sagittal ACL graft–tibial angles.
Fig. 4.

MRI imaging of double bundle ACL reconstructed knee showing coronal and sagittal ACL graft–tibial angles.
2.1. Operative technique
For DBACLR, the semitendinosus tendon (for the AM bundle) and the gracilis tendon (for the PL bundle) were looped separately over closed loop endobutton. The thickness of the graft construct was measured using a tendon thickness measuring gauge to the nearest of 0.5 cm. While viewing at 90° of knee flexion, “lateral bifurcate ridge” is often seen on the femoral insertion between the AM and PL bundles, whereas a “lateral intercondylar ridge” is often seen on the upper limit of both the AM and PL bundles. These were useful surgical landmarks in addition to the native insertion fibers to locate the femoral tunnels. Drilling of the AM femoral tunnel was done through the AM portal with the knee bent 90° to place the AM portal jig guide. The femoral PL tunnel was drilled with the knee flexed to 120° and anatomic anterior cruciate ligament reconstruction (ACLR) PL femoral aimer (Smith and Nephew, Andover, USA) was inserted with an appropriate sized post into the already made AM tunnel.
In a single-bundle arthroscopic reconstruction of the ACL, traditional AM bundle reconstruction was done with quadrupled semitendinosus tendon and gracilis tendon graft using the AM portal technique with 100–120° of knee flexion. The femoral footprint was identified and minimally debrided and was used as a landmark to make the femoral tunnel.
In both SB and DBACLR, appropriate-sized endoscopic reamer was selected according to the graft diameter and the femoral sockets were made. Depth was regulated according to the desired insertion length and was 9–10 mm greater than the desired graft insertion to allow for the endobutton flip. Closed loop endobutton was used for graft fixation on femoral side in both SB and DB ACLR.
For tibial tunnel, in DBACLR, an ACL tip aimer (Smith and Nephew, Andover, USA) was set at 55° for the placement of the AM guide wire. Once AM tunnel was drilled an appropriate sized post on Smith and Nephew, anatomic ACLR PL tibial aimer was used. Once the post was secured, it was inserted into the AM tibial tunnel until the distal end was flush with the tibial surface. This slot was oriented to align with the anticipated center of the PL bundle. The PL tunnel had a more medial and distal entry point on the tibial cortex than a standard ACL tibial tunnel. In SBACLR, the center of tibial tunnel was the center of tibial footprint in line with the posterior border of anterior horn of the lateral meniscus.
The fixation method used on the tibial side was titanium/biodegradable interference screw for both the techniques and augmentation with tendon staple where needed (Fig. 1, Fig. 2). In double bundle group AM bundle was fixed in 60° flexion and the PL bundle was fixed in full extension. In SBACLR, graft was fixed in maximal tension in 5–10° of knee extension. No patient who was selected for DBACLR had to be converted to undergo SBACLR because of insufficient tibial insertion site or a PCL dominance in the intercondylar notch.
Fig. 1.
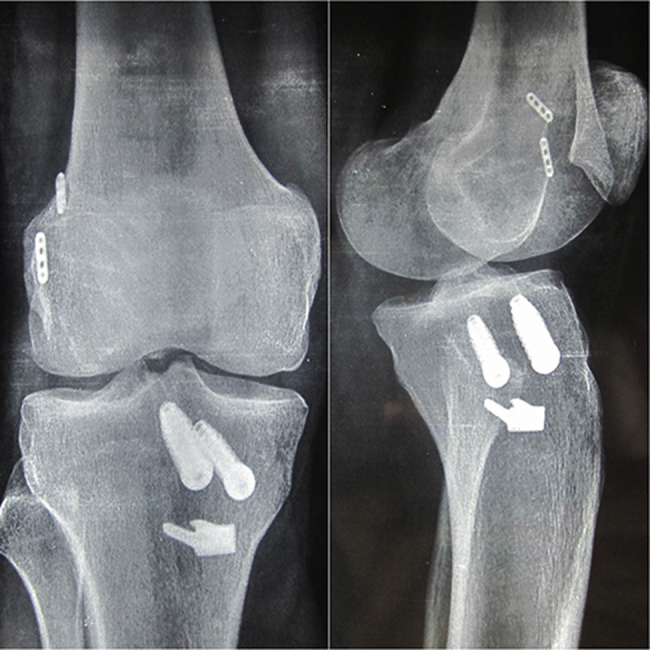
Postoperative anteroposterior and lateral skiagram of double bundle ACL reconstruction.
Fig. 2.
Postoperative anteroposterior and lateral skiagram of single bundle ACL reconstruction.
Immediate quadriceps and hamstring exercises were started and partial weight bearing was allowed with crutches/walker in first postoperative week. After first week, range of motion in arc of 0–90° (closed kinetic chain) was started. Full weight bearing was allowed by 3–4 weeks and running and cycling after one month. The patients were followed up at 2 weeks for suture removal, thereafter fortnightly for 2 months, monthly for next 3 months, and then once in 6 months for clinical evaluation and complications if any. MRI scan of the operated knee was performed at around 2 years of follow-up. Radiographic evaluation was done by a musculoskeletal radiologist who was unaware of the patients’ clinical and surgical data. A single orthopedic surgeon (first author) performed all the operations, and clinical follow-up assessments were made in a blinded manner by independent examiners (AS, MT).
2.2. Statistical analysis
Data were analyzed using the IBM SPSS version 19 (IBM, New York, United states of America). Preoperative values and values at the final follow-up were compared using paired t-test. P < 0.05 was considered to be statistically significant.
3. Results
Mean age was 23.73 ± 5.82 years in SB group and 25 ± 7.45 years in DB group. All patients were males in the DB group while two patients were females in SB group. Average follow-up was 34.8 months in SB group and 36.2 months in DB group. Right knee most commonly involved joint in both the groups. Most common mode of trauma was sports injury related pivot stress in both the groups. Isolated ACL tear associated with meniscal injury was present in 36 cases (22 in SB and 14 in DB group).
At the time of final follow-up, the mean Lysholm score was 94.13 ± 2.67 in SB group and 93.13 ± 3.31 in DB group (P value 0.202, non-significant – NS) (Table 2). Postoperative subjective IKDC score at final follow-up was 94.93 ± 2.78 in SB group and 93.87 ± 2.87 in DB group (P value 0.151, NS). All patients in both groups were in grade A or B as per the objective IKDC score at final follow-up. The mean differential anterior tibial translation by GNRB, arthrometer was 1.47 ± 0.6 mm in SB group and 1.17 ± 0.8 mm in DB group (P value 0.105, NS) (Table 2).
Table 2.
Comparison of single bundle & double bundle reconstruction groups.
| S no. | Parameter | Single bundle group (n = 30) |
Double bundle group (n = 30) |
P value* |
|---|---|---|---|---|
| 1 | Pre-op Lysholm score | 49.76 ± 9.92 | 46.33 ± 12.12 | 0.2352 |
| 2 | Post-op Lysholm score | 94.13 ± 2.67 | 93.13 ± 3.31 | 0.202 |
| 3 | Pre-op subjective IKDC | 47.56 ± 7.87 | 43.52 ± 9.20 | 0.0727 |
| 4 | Post-op subjective IKDC | 94.93 ± 2.78 | 93.87 ± 2.87 | 0.151 |
| 5 | Post-op objective IKDC | 100% normal or near normal (A + B) | 100% normal or near normal (A + B) | |
| 6 | Differential anterior tibial translation (mm) | 1.47 ± 0.6 | 1.17 ± 0.8 | 0.105 |
| 7 | Post-op mean sagittal tibial ACL angle (°) |
58.4 ± 4.8 | 56.1 ± 5.06 | 0.076 |
| 8 | Post-op mean coronal tibial ACL Angle (°) |
73.7 ± 5.1 | 74.86 ± 5.69 | 0.4091 |
| 9 | Post-op Pivot shift | 2 cases positive | All negative | 0.472 |
P value < 0.05 was considered statistically significant.
Though most of the patients regained very good range of motion (0–120° or above), 5 cases in SB group and 4 cases in DB group had mean 15° loss of terminal flexion. No patient in the both groups had terminal extension loss. All the patients showed a negative pivot shift test in DB group while 2 cases in SB group showed positive pivot shift at final follow-up (P = 0.472). Two patients in each group had endobutton flipped (>2 mm) in soft tissue outside the femoral cortex.
MRI scans of operated knees at 2 years follow-up showed the mean postoperative sagittal tibial-ACL angle as 58.4 ± 4.8° in the single bundle group and 56.1 ± 5.06° in patients with double bundle reconstruction (P = 0.076). Normal value for patients with closed physes is 58.8 ± 4.9°. Post-op mean coronal tibial–ACL angle in single bundle group was 73.7 ± 5.1° and in the group reconstructed with double bundle, it was 74.86 ± 5.69° (P = 0.4091) (Fig. 1, Fig. 2). Normal value for patients with closed physes is 69.1 ± 7.4°. There was no statistically significant difference between the two groups with respect to all the discussed criteria (Table 2).
4. Discussion
It has been reported that single-bundle reconstruction does not completely correct the rotational instability and it may result in anteroposterior instability in knee position of terminal extension.16, 17 Recently, double bundle ACL has gained in popularity where each bundle of the ACL is reconstructed separately with correct tensioning pattern of each bundle. The AM bundle is taut throughout the knee range of motion, reaching a maximum of between 45° and 60°, whereas the PL bundle is tight primarily in extension.16 Therefore, the AM and PL bundles are fixated accordingly, to restore their native tensioning behaviors. An in vivo kinematics study has shown that conventional single-bundle ACL reconstruction, which most closely imitates AM bundle reconstruction, can successfully restore anterior knee stability but does not sufficiently bring back rotational stability.3 In addition, cadaveric biomechanical studies have shown that double-bundle ACL reconstructions better restore knee kinematics especially rotator stability than single-bundle ACL reconstructions.10 In the present study also, two patients (6.6%) in single bundle group had positive pivot shift test implying a poorer rotatory control postoperatively, in comparison to none in double bundle group. However, it was not statistically significant (P value = 0.472).
Meredick et al.18 in a meta-analysis of the randomized controlled trials comparing single- versus DBACLR reported double-bundle reconstruction did not result in clinically significant differences in KT-1000 measurements for anterior stability or in pivot shift testing for rotational stability. Yasuda et al.19 in a current concepts review of anatomic DBACLR analyzed 10 prospective randomized studies comparing single- and double-bundle ACL reconstruction. In 8 (80%) of the 10 studies, the anterior and/or rotational stability of the knee was significantly better with the anatomic DBACLR than with conventional single-bundle reconstruction. A meta-analysis of random controlled trials by Xu et al.2 revealed that DBACLR resulted in significantly better anterior and rotational stability and higher IKDC objective scores compared with single-bundle reconstruction. However, this meta-analysis did not detect any significant differences in subjective outcome measures between double-bundle and single-bundle reconstruction, as evidenced by the Lysholm score, Tegner activity scale, and IKDC subjective score. Similarly, in our study, we also did not observe statistically significant difference between the two groups with respect to Lysholm score, subjective and objective IKDC, differential anterior tibial translation, as well as in postoperative mean sagittal and coronal tibial ACL angles on MRI scan (Table 2). Table 1 shows inconsistent results in literature survey of trials that were conducted to compare the results of SB and DBACLR. All these trials were prospective randomized comparative trials with a fairly large cohort and more than two years follow-up. Their results varied from no difference to better functional results of DBACLR.
Our study was conducted with a primary aim of comparing the postoperative clinico-radiological results of single bundle versus double bundle arthroscopic ACL reconstruction. We measured postoperative coronal–tibial and sagittal–tibial angle of the reconstructed ACL graft in patients of both the groups by MRI scanning at a follow-up of about two years. We found there was no statistically significant difference between the patients of the two groups with respect to various tibial–ACL graft angles (Table 2). In English literature, there has been no study conducted earlier with respect to radiological outcome in arthroscopic ACL reconstruction by single and double bundle technique. MRI of operated knees showed satisfactory placement of tunnels in both the groups which in turn led to comparable ACL graft tibial angles in both the groups. Exact positioning of the grafts is essential for optimal clinical outcome. Incorrect placement of the grafts is a primary reason for early graft failure, lack of extension and flexion, and residual instability with the single-bundle technique.7, 8, 20
Thus, these findings suggest that there is a need for a more anatomical ACL reconstruction using a design that closely replicates the 2 bundles of the ACL in terms of anatomical tunnel placement leading to anatomical ACL graft angles and inclination in both sagittal as well as coronal planes.
In our study, objective antero-posterior stability as measured by GNRB arthrometer showed marginally better results in DBACLR; however, it was not statistically better than the results in SBACLR group (P value = 0.105, NS). The mean differential anterior tibial translation in both groups of patients in our study corresponded to the value observed in various studies over time (Table 3). More collagen in ACL footprints and differential tensioning of the two bundles in DBACLR could be the reason for a better antero-posterior and rotator stability. The mean anterior tibial translation in single-bundle group was also observed to be less from all other cited studies (Table 3). That could have been important in minimizing the difference in the translation between the single bundle and double bundle groups. Accurate anatomical tunnel placement with maximal coverage of native femoral and tibial footprint, pre-tensioning of the graft, and proper seating of the femoral endobutton by cycling of the knee after graft passage and tibial fixation at about 5–10° of knee flexion could be the reasons that might have led to tighter single-bundle constructs.
Table 3.
Differential anterior translation as compared to normal knee by GNRB arthrometer in the literature.
Our study therefore not only showed statistically similar functional (Lysholm and IKDC scores) and objective results (arthrometer based antero-posterior translation measurement) in the two groups, but also a radiological (MRI) depiction of similar anatomic inclination angles of the grafted ACL in the two groups. Hence DBACLR does not deliver any significant functional advantage over SBACL reconstructions. DB reconstructions are also more expensive due to increased cost of additional implants and this is important factor to consider in developing nations.
This study has some limitations. In our study, a lateral pivot-shift test was used, but this is a subjective test and it requires the patient's cooperation. In DBACLR group, we saw a improvement of rotational stability according to the pivot shift, which might be related to the additional PL bundle reconstruction and the differential tightening of the two bundles of the graft and one could speculate that the high number of negative pivot shift tests might be related to the four tunnel technique, which increases the size of the footprint of the reconstruction. However, the pivot shift test is a subjective clinical tool to assess rotational stability and unfortunately, we still lack an accurate objective measurement method to measure rotatory stability in the knee. Another limitation is that we failed to evaluate the characteristic proprioceptive function thought to be one of the merits of double-bundle reconstruction. In addition, there is the lack of a power analysis because of the small number of cases. Also, the method of sequential selection of patients in the two groups is not a very good method of randomization. However, the prospective nature of the study is its strength.
5. Conclusion
In our study, both the surgical techniques of ACL reconstruction were found to yield similar/comparable clinical and radiological results. 6.6% patients in single bundle group had rotatory instability in comparison to none in double bundle (NS). However, there was no statistically significant difference between single bundle and double bundle ACL reconstruction groups with respect to clinical and radiological outcomes at an average of 35 months of follow-up. Further long-term evaluation study with a larger cohort is needed to substantiate the long-term advantages if any, of Double bundle ACL reconstruction over traditional Single bundle ACL reconstructions.
Conflict of interest
The authors have none to declare.
References
- 1.Tashman S., Collon D., Anderson K., Kolowich P., Anderst W. Abnormal rotational knee motion during running after anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32:975–983. doi: 10.1177/0363546503261709. [DOI] [PubMed] [Google Scholar]
- 2.Xu M., Gao S., Zeng C. Outcomes of anterior cruciate ligament reconstruction using single-bundle versus double-bundle technique: meta-analysis of 19 randomized controlled trials. Arthroscopy. 2013;29(February (2)):357–365. doi: 10.1016/j.arthro.2012.08.024. [DOI] [PubMed] [Google Scholar]
- 3.Shen W., Forsythe B., Ingham S.M., Honkamp N.J., Fu F.H. Application of the anatomic double-bundle reconstruction concept to revision and augmentation anterior cruciate ligament surgeries. J Bone Joint Surg Am. 2008;90:20–34. doi: 10.2106/JBJS.H.00919. [DOI] [PubMed] [Google Scholar]
- 4.Li Y.L., Ning G.Z., Wu Q. Single-bundle or double-bundle for anterior cruciate ligament reconstruction: a meta-analysis. Knee. 2014;21(January (1)):28–37. doi: 10.1016/j.knee.2012.12.004. [DOI] [PubMed] [Google Scholar]
- 5.Chen G., Wang S. Comparison of single-bundle versus double-bundle anterior cruciate ligament reconstruction after a minimum of 3-year follow-up: a meta-analysis of randomized controlled trials. Int J Clin Exp Med. 2015;8(September (9)):14604–14614. [PMC free article] [PubMed] [Google Scholar]
- 6.Tiamklang T., Sumanont S., Foocharoen T., Laopaiboon M. Double-bundle versus single-bundle reconstruction for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev. 2012;11:CD008413. doi: 10.1002/14651858.CD008413.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lorenz S., Elser F., Mittere M., Obst T., Imhoff A.B. Radiologic evaluation of the insertion sites of the 2 functional bundles of the anterior cruciate ligament using 3-dimensional computed tomography. Am J Sports Med. 2009;37:2368–2376. doi: 10.1177/0363546509341577. [DOI] [PubMed] [Google Scholar]
- 8.Araujo P.H., Asai S., Pinto M. ACL graft position affects in situ graft force following ACL reconstruction. J Bone Joint Surg Am. 2015;97(November (21)):1767–1773. doi: 10.2106/JBJS.N.00539. [DOI] [PubMed] [Google Scholar]
- 9.Taketomi S., Inui H., Nakamura K. Clinical outcome of anatomic double-bundle ACL reconstruction and 3D CT model-based validation of femoral socket aperture position. Knee Surg Sports Traumatol Arthrosc. 2014;22(September (9)):2194–2201. doi: 10.1007/s00167-013-2663-0. [DOI] [PubMed] [Google Scholar]
- 10.Siebold R., Ellert T., Metz S., Metz J. Femoral insertions of the anteromedial and posterolateral bundles of the anterior cruciate ligament: morphometry and arthroscopic orientation models for double-bundle bone tunnel placement—a cadaver study. Arthroscopy. 2008;24:585–592. doi: 10.1016/j.arthro.2007.12.008. [DOI] [PubMed] [Google Scholar]
- 11.Pujol N., Queinnec S., Boisrenoult P., Maqdes A., Beaufils P. Anatomy of the anterior cruciate ligament related to hamstring tendon grafts. A cadaveric study. Knee. 2013;20(December (6)):511–514. doi: 10.1016/j.knee.2012.10.006. [DOI] [PubMed] [Google Scholar]
- 12.Lee D.H., Kim H.J., Ahn H.S., Bin S.I. Comparison of femoral tunnel length and obliquity between transtibial, anteromedial portal, and outside-insurgical techniques in single-bundle anterior cruciate ligament reconstruction: a meta-analysis. Arthroscopy. 2016;32(January (1)):142–150. doi: 10.1016/j.arthro.2015.07.026. [DOI] [PubMed] [Google Scholar]
- 13.Lee B.H., Seo D.Y., Bansal S., Kim J.H., Ahn J.H., Wang J.H. Comparative magnetic resonance imaging study of cross-sectional area of anatomic double bundle anterior cruciate ligament reconstruction grafts and the contralateral uninjured knee. Arthroscopy. 2015 doi: 10.1016/j.arthro.2015.08.009. pii: S0749-8063(15)00663-5 [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 14.Briggs K.K., Lysholm J., Tegner Y., Rodkey W.G., Kocher M.S., Steadman J.R. The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am J Sports Med. 2009;37:890–897. doi: 10.1177/0363546508330143. [DOI] [PubMed] [Google Scholar]
- 15.Hefti F., Müller W. Current state of evaluation of knee ligament lesions. The new IKDC knee evaluation form. Orthopade. 1993;22:351–362. [PubMed] [Google Scholar]
- 16.Zantop T., Petersen W., Sekiya J.K., Musahl V., Fu F.H. Anterior cruciate ligament anatomy and function relating to anatomical reconstruction. Knee Surg Sports Traumatol Arthrosc. 2006;14:982–992. doi: 10.1007/s00167-006-0076-z. [DOI] [PubMed] [Google Scholar]
- 17.Aglietti P., Giron F., Buzzi R., Biddau F., Sasso F. Anterior cruciate ligament reconstruction: bone-patellar tendon-bone compared with double semitendinosus and gracilis tendon grafts. A prospective, randomized clinical trial. J Bone Joint Surg Am. 2004;86:2143–2155. [PubMed] [Google Scholar]
- 18.Meredick R.B., Vance K.J., Appleby D., Lubowitz J.H. Outcome of single-bundle versus double-bundle reconstruction of the anterior cruciate ligament: a meta-analysis. Am J Sports Med. 2008;36:1414–1421. doi: 10.1177/0363546508317964. [DOI] [PubMed] [Google Scholar]
- 19.Yasuda K., Tanabe Y., Kondo E., Kitamura N., Tohyama H. Anatomic double-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2010;26:21–34. doi: 10.1016/j.arthro.2010.03.014. [DOI] [PubMed] [Google Scholar]
- 20.Diamantopoulos A.P., Lorbach O., Paessler H.H. Anterior cruciate ligament revision reconstruction: results in 107 patients. Am J Sports Med. 2008;36:851–860. doi: 10.1177/0363546507312381. [DOI] [PubMed] [Google Scholar]
- 21.Ma Yubao, Deie Masataka, Iwaki Daisuke. Balance ability and proprioception after single-bundle, single-bundle augmentation, and double-bundle ACL reconstruction. Sci World J. 2014;2014 doi: 10.1155/2014/342012. Article ID 342012, 8 pages. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Koga H., Muneta T., Yagishita K. Effect of initial graft tension on knee stability and graft tension pattern in double-bundle anterior cruciate ligament reconstruction. Arthroscopy. 2015;31(September (9)):1756–1763. doi: 10.1016/j.arthro.2015.03.012. [DOI] [PubMed] [Google Scholar]
- 23.Järvelä T., Moisala A.S., Sihvonen R., Järvelä S., Kannus P., Järvinen M. Double-bundle anterior cruciate ligament reconstruction using hamstring autografts and bioabsorbable interference screw fixation: prospective, randomized, clinical study with 2-year results. Am J Sports Med. 2008;36(February (2)):290–297. doi: 10.1177/0363546507308360. [DOI] [PubMed] [Google Scholar]
- 24.Yagi M., Kuroda R., Nagamune K., Yoshiya S., Kurosaka M. Double-bundle ACL reconstruction can improve rotational stability. Clin Orthop Relat Res. 2007;454(January):100–107. doi: 10.1097/BLO.0b013e31802ba45c. [DOI] [PubMed] [Google Scholar]
- 25.Streich N.A1, Friedrich K., Gotterbarm T., Schmitt H. Reconstruction of the ACL with a semitendinosus tendon graft: a prospective randomized single blinded comparison of double-bundle versus single-bundle technique in male athletes. Knee Surg Sports Traumatol Arthrosc. 2008;16(March (3)):232–238. doi: 10.1007/s00167-007-0480-z. [DOI] [PubMed] [Google Scholar]
- 26.Núñez M., 1, Sastre S., Núñez E., Lozano L., Nicodemo C., Segure J.M. Health-related quality of life and direct costs in patients with anterior cruciate ligament injury: single-bundle versus double-bundle reconstruction in a low-demand cohort – a randomized trial with 2 years of follow-up. Arthroscopy. 2012;28(7):929–935. doi: 10.1016/j.arthro.2011.11.034. [DOI] [PubMed] [Google Scholar]
- 27.Zaffagnini S., Bruni D., Marcheggiani Muccioli G.M. Single-bundle patellar tendon versus non-anatomical double-bundle hamstrings ACL reconstruction: a prospective randomized study at 8-year minimum follow-up. Knee Surg Sports Traumatol Arthrosc. 2011;19(March (3)):390–397. doi: 10.1007/s00167-010-1225-y. [DOI] [PubMed] [Google Scholar]
- 28.Li Y., Li J., Wang J., Gao S., Zhang Y. Comparison of single-bundle and double-bundle isolated posterior cruciate ligament reconstruction with allograft: a prospective, randomized study. Arthroscopy. 2014;30(June (6)):695–700. doi: 10.1016/j.arthro.2014.02.035. [DOI] [PubMed] [Google Scholar]


