Abstract
Objective
To determine the long-term clinical and functional results of arthroscopic elbow synovectomy in rheumatoid arthritis patients with refractory elbow synovitis in terms of improvement in pain, function, and active range of motion (AROM) or arc of motion.
Method
Fifteen rheumatoid elbows in 13 patients, not responding to DMARD therapy and with radiological changes not more than Larsen grade 3 were taken, who underwent arthroscopic elbow synovectomy. The main outcome measured in forms of Mayo Elbow Performance Scale (MEPS) score, measurement of pain using a Visual Analogue Scale (VAS), radiological angles of elbow, disease activity score (DAS-28), arc of motions (AOM) and complications, which were assessed at follow-up periods of 6 months, 24 months, and 30 months. Statistical analysis was done both qualitatively and quantitatively. Mann–Whitney U test, chi-square test, and Student t test were used as the statistical test for determining significance.
Results
In the study group, the improvement was sustained and significant as compared to baseline (VAS 1.28, MEPS 81.07 and mean flexion range 85°) (p value <0.001). No significant complications were encountered postoperatively after elbow synovectomy.
Conclusion
The study assesses the long-term results of arthroscopic synovectomy in elbow synovitis secondary to rheumatoid arthritis with significant results favoring arthroscopic synovectomy.
Keywords: Arthroscopic synovectomy, Visual Analogue Scale (VAS) score, Mayo Elbow Performance Scale (MEPS), Arc of motion (AOM), Disease activity score (DAS-28), Larsen grading
1. Introduction
Rheumatoid arthritis (RA) is a chronic inflammatory condition, autoimmune in nature, involving multiple joints usually presenting with pain, swelling, inflammation, stiffness, and possible loss of functions at joints.1, 2 The pattern of joint involvement varies, wrist being the most frequently involved joint (87%), whereas shoulder, knees, ankle, and elbow are involved in 47%, 56%, 53%, 21% respectively at the time of presentation.3 Rheumatoid arthritis is the most common cause of elbow arthritis. Involvement of elbow joint in rheumatoid arthritis occurs in 20–25% within 5 years, and about 66% will show definitive involvement within 15 years of disease onset.4, 5 Incidence of disease is variable in different regions but generally increases between 25 and 55 years of age, remain stable or in a static manner up to the age of 75 years and then decreases.1, 2 Drugs commonly used for treatment are NSAIDs, DMARDs, Steroids, and new biological modifier drugs including anti-TNF drugs. Due to their high cost, non-availability, poor motivation for drugs schedule, and observation of outcome in Indian population, these drugs are not widely used. There are poor immunity status and unhygienic conditions in Indian localities, which may lead to accentuation of active and latent infective complications and respiratory problems. There are several diseases in India like high prevalence of tuberculosis, which may be aggravated, or their progression and pathogenesis altered with changing immune status by mentioned drugs.6 Open or arthroscopic synovectomy may be useful in some patients with persistent mono-arthritis (mild to moderate), particularly when refractory to conservative management. As synovium primarily plays an important role in the pathogenesis and disease progression, synovectomy or removal of inflamed synovial membrane is the corner stone in the management of joint inflammation refractory to optimal DMARD therapy. Arthroscopies are being done with increasing frequency to diagnose and treat elbow disorders and arthroscopic synovectomy of elbow joint can be used successfully to provide pain relief.6, 7, 8, 9 Unfortunately, there are very few studies dealing with the effectiveness of elbow arthroscopic synovectomy in rheumatoid arthritis and there are none from the Indian sub-continent. The present study was undertaken to evaluate the effectiveness of arthroscopic synovectomy in rheumatoid arthritis involving elbow joint.
2. Material and methods
Fifteen diagnosed cases of rheumatoid elbow based on “The American College of Rheumatology 1987 Revised Criteria” for the diagnosis of rheumatoid arthritis not responsive to optimal DMARD therapy and radiological changes not more than Larsen grade 3 were selected. Exclusion criteria included history of trauma to the affected joint, patient with history of septic arthritis of elbow joint, gross deformity of the elbow, and severe radiological destruction of the joint with Larsen grade 4 or more. All the patients continued to have DMARD therapy.
3. Operative method
All the patients were given general anesthesia and placed in prone position with high tourniquet in the upper arm. The arm was abducted to 90° and elbow flexed to 90° with keeping forearm hanging free. The bony anatomical landmarks viz., the radial head, the olecranon, and the lateral and medial humeral epicondyles were outlined with a marking pen. Ulnar nerve was also palpated and marked. 20 ml of sterile normal saline was injected into the elbow joint through the soft spot, to distend it. Anteromedial, anterolateral, midlateral, posterocentral, and posterolateral portals were used for surgery to get a maximum view of the joint and to remove the synovium with help of 4 mm shaver tip. Posteromedial portal was omitted for arthroscopy to avoid ulnar nerve injury in such a stiff joint. Anteromedial portal (proximal medial portal) is the primary viewing portal for arthroscopy of the elbow in the prone position, located approx. one finger breadth proximal to the medial epicondyle and 1–2 cm anterior to the intermuscular septum. With the joint distended, median nerve lies approximately 2 cm, and the brachial artery 2.2 cm from the portal. The ulnar nerve is protected by keeping the trocar anterior to the intermuscular septum. Anterolateral portal (proximal lateral portal) is located 2 cm proximal to the lateral epicondyle and 1 cm anterior to the inter-muscular septum. It is approximately 4.8 mm away from the radial nerve with the elbow in extension and approximately 9.9 mm away with the elbow in flexion. Midlateral portal (soft spot portal) is located in the center of the triangle formed by the radial head, the lateral epicondyle of the humerus, and the tip of the olecranon. It is the portal most often used for the distension of the joint. Posterocentral (straight posterior) portal is located in the midline, approximately 3 cm proximal to the tip of the olecranon. It enters directly through the triceps tendon and is therefore safe. The midlateral and posterocentral (straight posterior) portals can be used alternately as diagnostic and operative portals. Posterolateral portal lies just lateral to the posterior portal, i.e., 3 cm proximal to olecranon tip just lateral to the midline. All the synovium from medial, lateral and posterior compartments was removed. No attempt was made to view the posteromedial compartment in order to avoid any risk to the ulnar nerve. Radial head excision was not done in any patient but clearing of soft tissue and loose bodies from olecranon fossa took place. The joint was washed thoroughly with three liters of normal saline and portals were closed with 2.0 nylon sutures. Antiseptic dressing was applied and compression bandages were given. Cefotaxime coverage was continued for two days and stopped. Oral analgesics were given for seven days postoperatively. Elbow mobilization and physiotherapy were started from the second post-operative day.
3.1. Evaluation and biostatics analysis
We studied and followed the following parameters in our study.5, 6, 7, 8, 9, 10, 11
-
-
Visual analogue score for pain
-
-
Mayo elbow performance score including 100 maximum points (pain, max. 45), (motions, max. 20), (daily function, max. 25) and (stability, max. 10 points)
-
-
Arc of flexion
-
-
Coronoid height ratio
-
-
Modified Larsen grade
-
-
Disease activity score-28 (DAS-28)
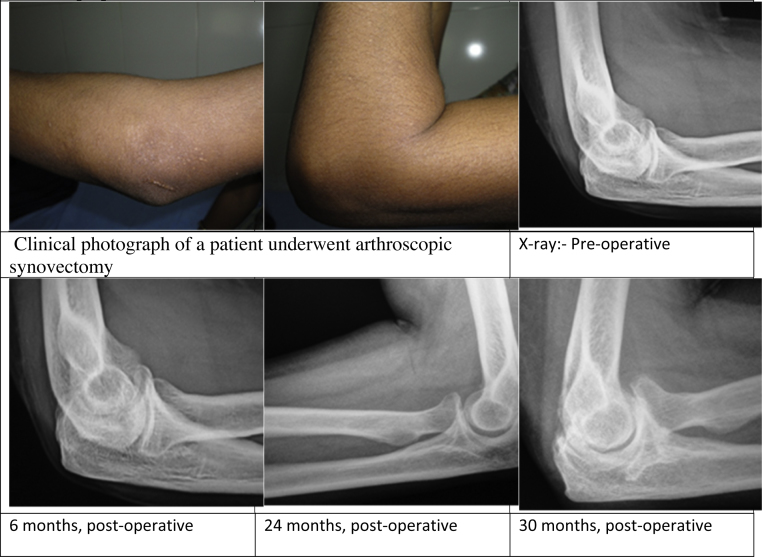
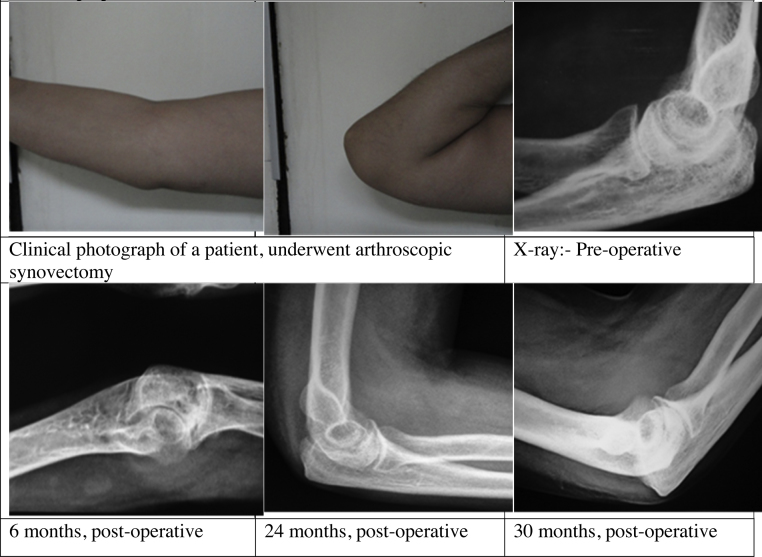
These parameters were recorded before the intervention and at 6 months, 24 months, and 30 months after intervention. The statistical analysis would be carried out by using SPSS version 15 for qualitative data. The analytical technique used would be chi square test or Fisher test wherever necessary. For quantitative data, Student t-test or Mann–Whitney test would be done. The changeover period of time in VAS score and CoHR would be analyzed by applying repeated measure analysis followed by post-hoc test. The p value of <0.05 would be considered as significant. Clinical and radiological follow-up of two patients are illustrated in Fig. 1, Fig. 2 (clinical and radiological photographs of a patient at pre-op and different follow-up periods).
Fig. 1.
Clinical and radiological photographs of a patient at pre-op and different follow-up periods.
Fig. 2.
Clinical and radiological photographs of a patient at pre-op and different follow-up periods.
4. Observation and results
Patient profile and parameters at the commencement of study are listed in Table 1. In this study, the patient's age ranged from 26 to 62 years, the mean age being 41.7 ± 9.7 years. Male:female ratio was 1:12. All the parameters included and observed in study are summarized in Table 2. There was significant improvement in VAS after arthroscopic procedure when compared to pre-operative status at the end of 6 months, 24 months, and 30 months observation. One patient had exacerbation of pain and one of them experienced similar pain as pre-operative status during this period. There was significant improvement in MEPS score after the surgical procedure at the end of 6 months, 24 months, and at 30 months. All patients in our study presented with improvement in MEPS except for one patient where the score remained the same. No patient had any loss of function in this group. We did not observe any significant difference in the mean CoHR and modified Larsen scores between pre-operative and post-operative values in group. In our study, we observed significant results when compared between pre-op arc of flexion and 30-month follow-up and p value was found to be 0.026.
Table 1.
Parameters and characteristics of patients at the start of study.
| Parameters | Mean ± S.D. |
|---|---|
| Age (years) | 41.7 ± 9.7 |
| Duration of disease (months) | 94 ± 74.5 |
| Duration of right elbow involvement (months) | 59.2 ± 80 |
| Duration of left elbow involvement (months) | 54 ± 79 |
| E.S.R. (mm/1 h) | 58.5 ± 16.6 |
| Duration of NSAID intake (months) | 101.6 ± 72.1 |
| Duration of DMARD intake (months) | 51.7 ± 64.3 |
| Pre-op visual analogue score | 6.4 ± 1.7 |
| Pre-op Mayo elbow performance score | 53.3 ± 17 |
| Pre-op arc of flexion | 67.66 ± 27.70 |
| Pre-op modified Larsen score | 2.5 ± 0.5 |
| Pre-op coronoid height ratio | 50.4 ± 10.8 |
| Pre-op disease activity score | 6.6 ± 1.1 |
Table 2.
Patients parameters at pre-intervention and follow-up periods of 6, 24 and 30 months.
| Parameters (mean ± S.D.) | 0 month | 6 months follow-up | 24 months follow-up | 30 months follow-up | p value (0 and 6 months) | p value (0 and 24 months) | p value (0 and 30 months) |
|---|---|---|---|---|---|---|---|
| VAS | 6.21 ± 1.5 | 0.42 ± 0.5 | 1.14 ± 0.5 | 1.28 ± 0.5 | 0.001 | 0.001 | 0.001 |
| MEPS | 54.28 ± 17.19 | 91.07 ± 10.4 | 82.5 ± 15.28 | 81.07 ± 15.08 | 0.001 | 0.001 | 0.001 |
| Arc of flexion | 68.9 ± 28.29 | 94.2 ± 23.44 | 85.0 ± 21.03 | 85.0 ± 21.03 | 0.003 | 0.026 | 0.026 |
| Modified Larsen score | 2.42 ± 0.5 | 2.42 ± 0.5 | 2.5 ± 0.65 | 2.5 ± 0.65 | 1.0 | 0.336 | 0.336 |
| CoHR | 49.5 ± 10.63 | 49.85 ± 10.21 | 50.92 ± 10.9 | 51.14 ± 10.78 | 0.81 | 0.24 | 0.17 |
| DAS-28 | 6.48 ± 1.01 | 5.7 ± 1.04 | 5.86 ± 1.09 | 5.97 ± 1.09 | 0.001 | 0.005 | 0.005 |
Our study being followed up of thirteen months was not of enough period to note any significant radiological changes. Hence, we suggest that a long-term follow-up may give better information on the above to parameters with respect to time. Clinical and radiological photographs of two patients are illustrated in Fig. 1, Fig. 2, which elaborate changes over follow-up periods.
According to the EULAR response criteria, there were no response over the time points in study group for 6, 24, and 30 months follow-up post-operatively as shown in Table 3.11 In the study, patients group performed better at 6 months follow-up, but it was difficult to conclude whether improvement was due to arthroscopy or continuation of DMARD. It is also difficult to make any decision regarding effectiveness of surmise that, how synovectomy of a single joint can have such a significant generalized improvement.
Table 3.
Change in disease activity score (DAS-28) improvement over time points (6, 24, 30 months) post-operatively.
| DAS-28 (>5.1) | 0–6 months | 0–24 months | 0–30 months |
| 0.78 | 0.62 | 0.51 | |
| No response | No response | No response |
5. Discussion
It is an autoimmune disease where the body's immune system affects joints, soft tissues, and periarticular soft tissues leading to inflammation and producing various symptoms, ranging from pain, morning stiffness to deformities of joints. Management of patients with RA involves an interdisciplinary approach, which attempts to deal with the various problems that persist in systemic manner. Drug treatment includes various drugs, either single or in combinations form. Combination drug therapy, using disease-modifying anti-rheumatic drugs and biologic therapies are very effective, and complete resolution of signs and symptoms is achievable in approximately 10% of patients. Intra-articular steroid injection may relieve joint inflammation and reduce symptoms in early stages. Surgery plays an important role in the management of patients with severely damaged joints by considering age, functional demands, etiology, and severity of elbow arthritis. Synovectomy, arthroplasty, and arthrodesis of elbow have been practiced since long with variable results. Synovectomy for inflamed joint has been practiced for long and has shown good results for pain relief in the past.12 Various studies have shown to improve the function of the joint following synovectomy, either in the form of open or arthroscopic synovectomy.13, 14, 15, 16, 17, 18, 19, 20 Open synovectomy is quiet easier and less demanding technically than arthroscopic procedure but there is less morbidity and early rehabilitation in arthroscopic approach.20 By avoiding neurovascular structures injury with proper pre-operative planning and intraoperative precautions, arthroscopic synovectomy can give better results in terms of less morbidity and early functional outcome.
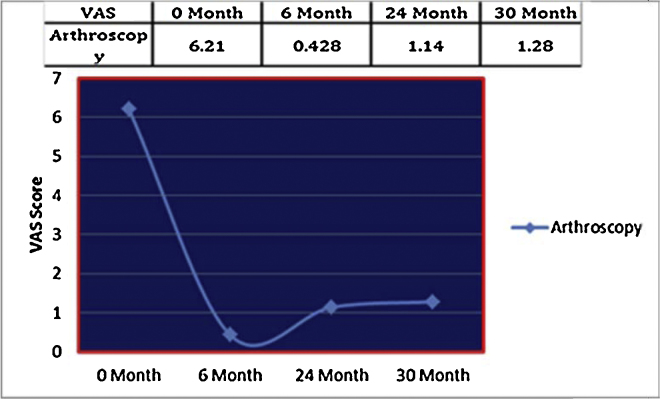
The mean duration of disease in study group was 94 months and the mean age of the patients in it was 41.7 ± 9.7 years. Male to female ratio was 1:12. The mean visual analogue score (VAS) at the time of enrolment in the study was 6.21 ± 1.57 (dreadful pain). Post-operatively, at 6-months follow-up, it was 0.42 ± 0.5 (nearly no pain). As the time passed away, pain increased progressively over 2 year in these patients. Mean VAS at the 24 months and 30 months follow-up were 1.14 ± 0.84 and 1.285 ± 1.06 (mild pain), respectively. Chung et al. conducted a study in 13 elbow joints for mean 34-months (range 18–78) follow-up.21 The mean VAS pain score decreased significantly from nine (range 5–10) preoperatively to four (range 2–6) at one week and to one (range 0–7) at the final follow-up of 34 months. The results were significant with p value of 0.005 and 0.004, respectively. These were similar to our results. Kang performed arthroscopic synovectomy and studied mean follow-up of 33.9 months on 26 rheumatoid elbows in 25 patients.22 The mean VAS for pain decreased from 6.5 points (range 5.1–9.2) preoperatively to 3.1 points (range 1.5–8.2 points) at the final follow-up, showing significantly less pain post-operatively with p value of 0.001. Our final VAS for pain score was 1.285 ± 1.06, much lower than this study. These changes over the time are illustrated in graph (Fig. 3).
Fig. 3.
VAS score for pain in arthroscopy group patients.
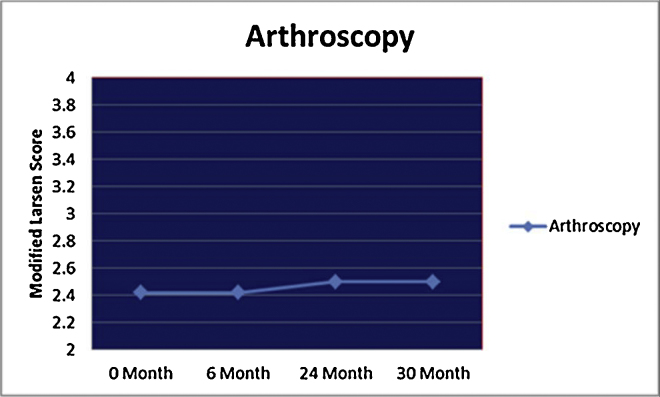
The mean modified Larsen grade at the time of commencement of the study was 2.428 ± 0.5 (range 2–3), and remained same at 6-months follow-up. The mean values for score were 2.50 ± 0.65 (range 2–4) at 24-months and 30-months follow-up. Kang et al. started a study of 26 patients, in which ten included in grade 1, thirteen in grade 2, and three patients in grade 3.22 At final follow-up, 10 elbows were classified as grade 1, 10 as grade 2, 4 as grade 3, and 2 as grade 4. After 33.9-months follow-up, there was a reduction in degenerative change by one grade in 6 elbows, progression by grade in 7 elbows and no change in thirteen elbows. Chung et al. mentioned Modified Larsen Grading for radiological assessment in pre-operative period, but did not evaluate same parameter in post-operative follow-up.21 Horiuchi et al. followed 21 patients, who underwent arthroscopic synovectomy with observation for a mean period of 97 months.20 Larsen grade increased in 17 out of 21 elbows even after surgery. We did not find any significant changes in modified Larsen grading. A long-term follow-up of 97 months may be a cause of such deterioration in above study in comparison to our study. These changes over the time are illustrated in graph (Fig. 4).
Fig. 4.
Modified Larsen score in arthroscopy group patients.
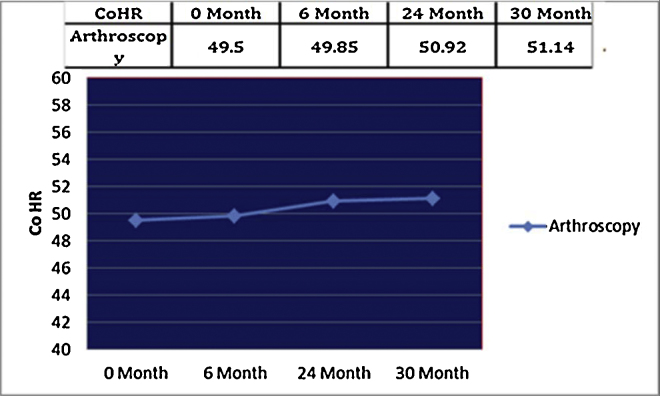
The mean coronoid height ratio (CoHR) at the time of commencement of our study was 49.5 ± 10.63 (range 33–70) and 49.85 ± 10.2 (range 30–70) at 6-months follow-up. It changed over time at the 24- and 30-months follow-up, 50.928 ± 10.91 and 51.142 ± 10.75, respectively. Nemoto et al. conducted a study and evaluated the results of arthroscopic synovectomy of eleven rheumatoid elbows in 10 patients with a mean follow-up of 3 years and 1 month.19 The mean CoHR in group A preoperatively was 54.2 ± 7.3 and postoperatively was 56.3 ± 6.8 and was found not significant. But in Group B preoperatively CoHR was 62.4 ± 6.2 and postoperatively was 67.4 ± 3.1 and it was found significant when compared with p < 0.05. We had patients only in Larsen grade 2 or 3 in our arthroscopic synovectomy group. We did not observe any significant difference in the mean CoHR between pre-operative and post-operative group similar to their study at the end of our follow-up. As there were no patients operated with a pre-operative Larsen grade 4, a correlation is not possible with group B. These changes over the time are illustrated in graph (Fig. 5).
Fig. 5.
Coronoid height ratio (CoHR) in arthroscopy group patients.
The mean disease activity score (DAS-28) at the time of commencement of our study was 6.48 ± 1.01 (range 4.9–7.9) and 5.70 ± 1.04 (range 4.3–7.9) at 6-months follow-up, which changed at 24 months as 5.86 ± 1.095 and at 30 months, to 5.97 ± 1.094 (range 4.4–7.68) in patients. There are no studies in literature, which show correlation between arthroscopy and DAS-28.
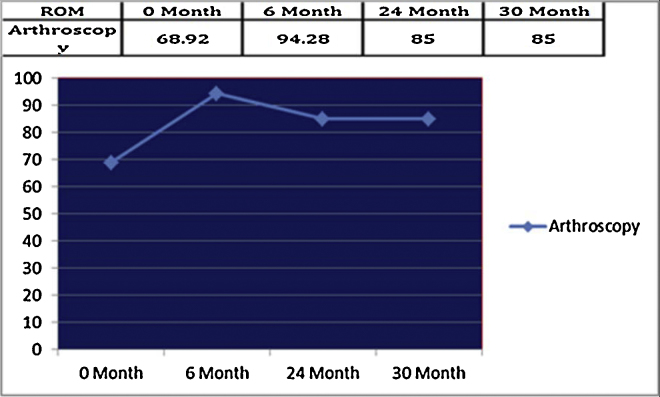
The mean arc of flexion at the time of commencement was 68.92 ± 28.29 (range 20–130°) and 94.28 ± 23.44 (range 30–130) at 6-months follow-up, which further decreased in mean values around 85 ± 21.031 (range 30–120) at final follow-up of 30 months. In Kang et al., study, the mean flexion-extension arc improved from 98.1° preoperatively to 113.3° post-operatively.22 The results were significant with p value of 0.032. The mean rotation arc increased insignificantly from 146.3° to 159.5° post-operatively, with p value of 0.75. In our study, we observed significant results when compared between pre-op arc of flexion and 30-months follow-up and p value was found to be 0.026. Results were similar to this study and show the effectiveness of arthroscopic synovectomy in rheumatoid elbow. Chung et al. in their study of arthroscopic synovectomy of 26 elbows observed for 34 months.21 The median elbow flexion-extension arc improved significantly from 75° to 105°, with p value of 0.004. Result was similar to that of our study. Lee and Morrey, evaluated fourteen arthroscopic synovectomies with mean arc of flexion preoperatively 91 (range 45–130°) and the mean in post-operative period 108 (range 75–120°), showing an improvement of 17°.23 We reported 16.08° improvement in our study. These changes over the time are illustrated in graph (Fig. 6).
Fig. 6.
Arc of flexion in arthroscopy group patients.
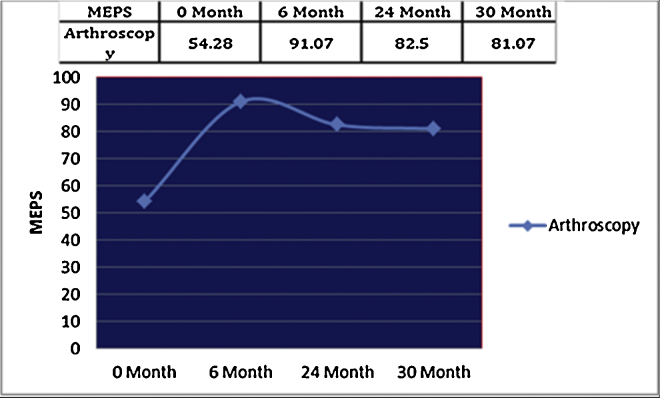
Pre-operative mean value of MEPS was 54.28 ± 17.19 (signifying poor elbow performance score) in the group. At 6-months follow-up, it was 91.07 ± 10.77 with excellent elbow performance score, while at the 24 and 30 months, the mean values were 82.5 ± 15.28 and 81.07 ± 15.086, respectively. We observed good results in all patients except one where the score deteriorated over the time of 24 months and 30 months. We also noticed no failure during our 6-months follow-up. Kang et al., in their study of 26 patients, observed improvement in mean Mayo elbow performance score from 58.5 points preoperatively to 77.4 points at the final follow-up with the p value of 0.02.22 Inglis et al., in their study of 28 patients, graded result as good, satisfactory, and poor without using of MEPS.13 They reported 50% good results (14 out of 28 patients). 6 patients had satisfactory results, while 4 as failures, with 3 ankylosed joints and 1 recurrent synovitis. Tanaka et al., conducted a study of 58 arthroscopic synovectomy and 53 open synovectomy with a follow-up of 13 years and 3–5 years mid-term follow-up.18 Mean MEPS in both the groups were 50 preoperatively. There was a similar improvement in MEPS in both the group at 3–5 year follow-up with MEPS 78 but noted a difference at 13 year follow up with MEPS in arthroscopy group 67 and open synovectomy group 71 and concluded that there is a significant improvement in MEPS in both arthroscopy and open synovectomy at short-term and long-term follow-up but the gain in improvement tends to decrease more in arthroscopy group than in open synovectomy group. Our study has a better gain in the MEPS (81.07 ± 15.086) at the 30-months follow-up but the results are formalized in 30-months follow-up as compared to 13-years follow-up in the above study. Lee and Morrey, performed arthroscopic synovectomy on 14 elbows and reported post-operative MEPS as 78 (signifying good elbow performance score).23 He concluded that arthroscopic synovectomy has a good short-term success but tends to deteriorate with time. Similar results were found in Horiuchi et al. study, where they performed arthroscopic synovectomy in 21 patients.20 Mean MEPS at 2-years follow-up was 77.5 while at 11-years follow-up, it was 69.8. We noticed in all previous studies that MEPS had improved significantly but there is a trend to deteriorate with passage of time. In a similar way, our study has excellent result at 6 months but deteriorate progressively at the 24-months and 30-months follow-up. These changes over the time are illustrated in graph (Fig. 7).
Fig. 7.
Mayo elbow performance score (MEPS) in arthroscopy patients.
6. Limitations
The sample size was small and the follow-up was only for two and an half years. A longer follow-up can reveal a different pattern of disease status, particularly radio-graphically. DMARDs and other drugs prescribed by rheumatologist were different in different patient according to their clinical picture. This confounding factor was not included in the study.
7. Conclusions
We concluded in our study that Pain and decreased range of movements of joints were the most important indications for any intervention in patients of rheumatoid arthritis. Short-term (at 6 months) pain relief after arthroscopic synovectomy was excellent. Long-term (at 30 months) pain relief is better achieved with arthroscopic synovectomy along with DMARD. Arthroscopic synovectomy produces satisfactory improvement in elbow functions in form of range of moments and MEPS parameters, both in short-term and long-term follow-up. Little deterioration over the time was observed in all the mentioned parameters. Significant changes in radiological grade are not notable in short-term (6 month) and long-term (30 months) follow-up. There is no response, according to new EULAR classification criteria in short-term as well as in long-term follow-up study for DAS-28 scoring. Therefore, arthroscopic synovectomy considered as an effective intervention, as a surgical management of rheumatoid elbow, refractory to conservative treatment.
Ethical statement
The study was started after obtaining ethical approval from members of ethics committee of institute with reference number IESC/T-207/06.05.2011.
Informed consent
Informed written consent was obtained from patients and their attendants.
Financial support
No author had any financial support for study and article.
Conflicts of interest
The authors have none to declare.
Acknowledgement
We are thankful to all patients and persons, who are actively involved in this study.
Contributor Information
Vivek Shankar, Email: drshankarvivek@gmail.com.
Pankaj Sharma, Email: dr.pankajkristwal@gmail.com.
Ravi Mittal, Email: ravimittal66@hotmail.com.
Samarth Mittal, Email: samarthmittal@gmail.com.
Uma Kumar, Email: Umaakumar@yahoo.com.
Shivanand Gamanagatti, Email: shiv223@gmail.com.
References
- 1.Elipsky P. Harrison's Principles of Internal Medicine. 17th ed. The McGraw-Hill Companies; New York: 2008. Rheumatoid arthritis; pp. 2083–2092. [Google Scholar]
- 2.Shah A., Clair E.W. Harrison's Principles of Internal Medicine. 19th ed. The McGraw-Hill Companies; New York: 2012. Rheumatoid arthritis; pp. 2136–2149. [Google Scholar]
- 3.Edward J.H., editor. Clinical features of Rheumatoid Arthritis. 1994. [Google Scholar]
- 4.Ellison M.R., Kelly K.J., Flatt A.E. The results of surgical synovectomy of the digital joints in rheumatoid disease. J Bone Joint Surg Am. 1971;53:1041–1060. [PubMed] [Google Scholar]
- 5.Scott D.L., Symmons D.P., Coulton B.L., Popert A.J. Long-term outcome of treating rheumatoid arthritis: results after 20 years. Lancet. 1987;16:1108–1111. doi: 10.1016/s0140-6736(87)91672-2. [DOI] [PubMed] [Google Scholar]
- 6.Shankar S., Handa R. Biological agents in rheumatoid arthritis. J Postgrad Med. 2004;50:293–299. [PubMed] [Google Scholar]
- 7.Morrey B.F., An K.N., Chao E.Y.S. Functional evaluation of the elbow. In: Morrey B.F., editor. In: The Elbow and Its Disorders. 2nd ed. W. B. Saunders; 1993. [Google Scholar]
- 8.Larsen A., Dale K., Eek M. Radiographic evaluation of rheumatoid arthritis and related conditions by standard reference films. Acta Radiol Diagn. 1977;18:481–491. doi: 10.1177/028418517701800415. [DOI] [PubMed] [Google Scholar]
- 9.Ando T., Namiki O., Inagaki K., Hirahara H., Fujimaki E. Natural history of the elbow joint in rheumatoid arthritis. J Showa Med Assoc. 2000;60:399–406. [Google Scholar]
- 10.Prevoo M.L., van’t Hof M.A., Kuper H.H., van Leeuwen M.A., van de Putte L.B., van Riel P.L. Modified disease activity scores that include twenty-eight-joint counts. Development and validation in a prospective longitudinal study of patients with rheumatoid arthritis. Arthritis Rheum. 1995;38:44–48. doi: 10.1002/art.1780380107. [DOI] [PubMed] [Google Scholar]
- 11.Fransen J., van Riel P.L.C.M. The Disease Activity Score and the EULAR response criteria. Clin Exp Rheumatol. 2005;23:S93–S99. 51. [PubMed] [Google Scholar]
- 12.Lopes R.V., Furtado R.N.V., Parmigiani L., Rosenfeld A., Fernandes A.R.C., Natour J. Accuracy of intra-articular injections in peripheral joints performed blindly in patients with rheumatoid arthritis. Rheumatology. 2008;47:1792–1794. doi: 10.1093/rheumatology/ken355. [DOI] [PubMed] [Google Scholar]
- 13.Inglis A.E., Ranawat C.S., Straub L.R. Synovectomy and debridement of the elbow in rheumatoid arthritis. J Bone Joint Surg Am. 1971;53:652–662. [PubMed] [Google Scholar]
- 14.Maenpaa H., Kuusela P., Lehtinen J., Savolainen A., Kautiainen H., Belt E. Elbow synovectomy on patients with juvenile rheumatoid arthritis. Clin Orthop Relat Res. 2003;412:65–70. doi: 10.1097/01.blo.0000072463.53786.df. [DOI] [PubMed] [Google Scholar]
- 15.Maenpaa H.M., Kuusela P.P., Kaarela K., Kautiainen H.J., Lehtinen J.T., Belt E.A. Reoperation rate after elbow synovectomy in rheumatoid arthritis. J Shoulder Elbow Surg. 2003;12:4803. doi: 10.1016/s1058-2746(03)00167-8. [DOI] [PubMed] [Google Scholar]
- 16.Copeland S.A., Taylor J.G. Synovectomy of the elbow in rheumatoid arthritis: the place of excision of the head of the radius. J Bone Joint Surg Br. 1979;61:69–73. doi: 10.1302/0301-620X.61B1.422636. [DOI] [PubMed] [Google Scholar]
- 17.Ferlic D.C., Patchett C.E., Clayton M.L., Freeman A.C. Elbow synovectomy in rheumatoid arthritis. Long-term results. Clin Orthop Relat Res. 1987;220:119–125. [PubMed] [Google Scholar]
- 18.Tanaka N., Sakahashi H., Hirose K., Ishima T., Ishii S. Arthroscopic and open synovectomy of the elbow in rheumatoid arthritis. J Bone Joint Surg Am. 2006;88:521–525. doi: 10.2106/JBJS.E.00472. [DOI] [PubMed] [Google Scholar]
- 19.Nemoto K., Arino H., Yoshihara Y., Fujikawa K. Arthroscopic synovectomy for the rheumatoid elbow: a short-term outcome. J Shoulder Elbow Surg. 2004;13:652–655. doi: 10.1016/j.jse.2004.03.012. [DOI] [PubMed] [Google Scholar]
- 20.Horiuchi K., Momohara S., Tomatsu T., Inoue K., Toyama Y. Arthroscopic synovectomy of the elbow in rheumatoid arthritis. J Bone Joint Surg Am. 2002;84-A:342–347. doi: 10.2106/00004623-200203000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Chung C.Y.S., Yen C.H., Yip M.L.R., Koo S.C.J.J., Lao W.N. Arthroscopic synovectomy for rheumatoid wrists and elbows. J Orthop Surg. 2012;20:219–223. doi: 10.1177/230949901202000217. [DOI] [PubMed] [Google Scholar]
- 22.Kang H.J., Park M.J., Ahn J.H., Lee S.H. Arthroscopic synovectomy for the rheumatoid elbow. Arthroscopy. 2010;26:1195–1202. doi: 10.1016/j.arthro.2010.01.010. [DOI] [PubMed] [Google Scholar]
- 23.Lee B.P., Morrey B.F. Arthroscopic synovectomy of the elbow for rheumatoid arthritis. A prospective study. J Bone Joint Surg Br. 1997;79:770–772. doi: 10.1302/0301-620x.79b5.7466. [DOI] [PubMed] [Google Scholar]