Abstract
The intramedullary insertion of antibiotic impregnated PMMA rods, beads or nails are widely used and accepted modality of treatment for chronic osteomyelitis of long bones. But at times it becomes difficult to insert and remove these antibiotic delivery systems owing to narrowed medullary canals. Here we present a technique for preparing PMMA rods with diameter ranging from 6 mm to 3 mm. These rods could easily be placed in narrow intramedullary canal of long bones with chronic osteomyelitis or infected non-union.
We have used high viscosity bone cement (Simplex P) along with two antibiotics (cefuroxime and vancomycin) for preparing cement rods. Food grade straw and low profile teflon tube guide wire exchanger used in IM nailing were used as mold. Ilizarov wire, 1 mm K wire and 24 gauge stainless steel wire were used as internal support core material for imparting strength. We used this technique in seven cases and were successful in treating infection of long bones of upper and lower limbs (femur). With average follow up of 7.28 months rate of union in our series was 71% (five cases). Four cases (57%) had no evidence of infection and two cases (29%) had control of infection and in one case (14%) infection was still there but union was achieved.
Keywords: Antibiotic, PMMA, Rod, Osteomyelitis, Non-union
1. Introduction
Infected nonunion1 secondary to post traumatic fractures have always been a challenge to treat owing to numerous associated complexities. Adequate management of such cases necessitates a staged and well planned surgical procedure for achieving bony union and resolution of infection.
Standard treatment of non-union with infection1, 2, 3, 4 with implant in situ usually involves removal of implant, debridement, use of local antibiotic delivery system5 and I.V. antibiotics, along with a provision to provide stability at the fracture site in the form of external fixator or simply by using cast/splint and later on definitive treatment in the form of internal/external fixation with or without bone grafting.
Several methods6, 7, 8, 9 of local antibiotic delivery system using PMMA are being commonly used which includes hand fashioned or commercially available PMMA beads,10 PMMA rods11, 12, 13 and PMMA coated nails.1, 2, 3, 4 None of these methods provide adequate stability and necessitates secondary procedure for stability at the fracture site in form of intramedullary interlocking nailing, cephalomedullary nailing or LCP with or without autogenous bone grafting. In cases of infected non-union associated with obliteration of intramedullary cavity it is very difficult to use intramedullary antibiotic delivery system. At times it is very difficult to reconstruct medullary canal of size enough to receive a nail up to 9 mm thickness. Moreover it becomes difficult to remove these nails so we present a technique of making PMMA rods up to 6 mm diameter or even lesser which are placed in the pilot hole made for insertion of intramedullary implant later in cases of diaphyseal/diaphyseo-metaphyseal fractures with an obliterated medullary cavity and infected non-union. This study aims at providing a novel technique for designing and inserting antibiotic impregnated intramedullary cement rods in inaccessible narrow intramedullary canals of infected bones and assessing its effect on eradication of infection.
2. Material and method
This prospective study was conducted between Jan 2013 and Nov 2015 at our Institution. Subjects between age of 18 and 55 years without any comorbid condition preventing surgical intervention, who presented to us with infected non-union of long bones with or without implant in situ, with narrow medullary cavity (diameter <9 mm), not requiring extensive soft tissue reconstruction, were included in the study.
All the cases were managed as per two stage surgical protocol. In the first stage, surgical debridement and removal of implant if any, was done followed by intramedullary placement of hand fashioned antibiotic impregnated cement rods and if required, placement of cement rod or hand fashioned antibiotic impregnated cement beads in extra-periosteal/sub muscular plane for a period of six weeks. Second stage surgery was performed after six weeks in which we removed the bone cement along with further debridement if required and autogenous bone grafting with definitive internal fixation.
Technique for preparing PMMA rods: A pre chilled (at 4–8 °C) Simplex P, bone cement is hand mixed in a bowl. The cement is kept at a low temperature prior to mixing as at low temperature it retains its liquid form14 for a longer duration of time and thus allows for procedural time to prepare antibiotic delivery system. Two grams, each of cefuroxime and vancomycin is then added to the mixture9, 15 and stirred at the rate of one cycle/s for 30 s. Thereafter it is poured in a 50 ml or a 20 ml disposal syringe and then the plunger is inserted (Fig. 1, step 1).
Fig. 1.
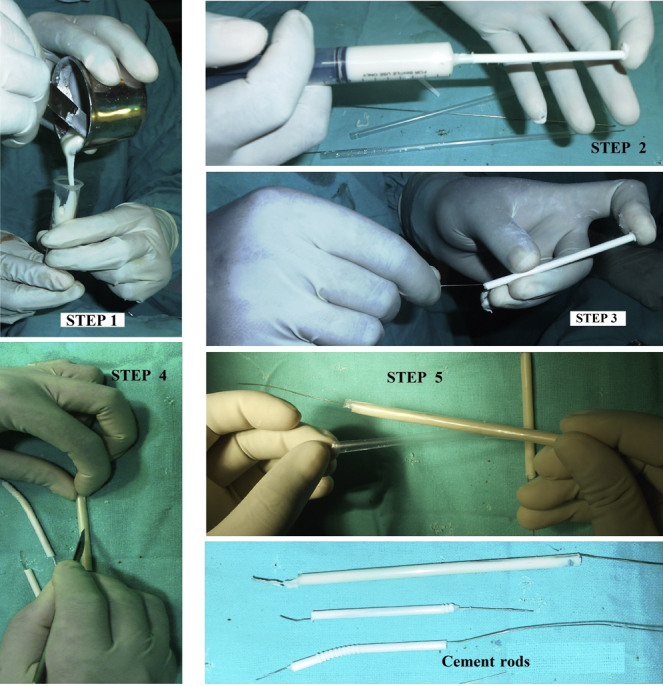
Technique for fashioning bone cement rods, Step I – Pre chilled cement mixed and attained liquid form. Step II – Straw being filled up with semi fluid cement. Step III – SS wire being introduced in cement within the straw. Step IV – Straw/mold being cut longitudinally. Step V – Cement rod being taken out.
2.1. For preparing PMMA rods of less than 5 mm diameter (Fig. 1, steps 2 to 5)
We have used food grade straw as a mold to make cement rods and pre sterilized it in glutaraldehyde 2% solution. Alternatively, commercially available teflon tubes or soft silicone tubes of desired dimension could be used. We have used 24 gauge SS wire or 1 mm K wire as internal support core material for imparting strength to the impregnated cement construct. K-wires are better and easy to use as they are relatively stiffer than SS wire and can be easily negotiated inside the core of cement which is about to set. Before the cement sets in completely, the shape of construct can be manipulated depending upon that we need a straight or a slightly curved cement rod. Once the cement sets in completely then it is a rigid construct. The above mentioned antibiotic impregnated PMMA is injected into the straw/tubes (step 2) and then wire with one end twisted in form of knot is inserted into the bone cement contained in tube till the knot gets flushed with bone cement (step 3). Protruded end of wire at other end is cut at desired length. This construct is left for 12–15 min as cement sets in and becomes hard. Thereafter the tube is slit longitudinally with scalpel to take out the cement rods (step 4, 5). Cement rods of required length can be fashioned in this way to be placed in medullary cavity.
The melting point of the straw molds16 is more than 157 °C and the heat dissipated as a result of exothermic reaction during polymerization of PMMA17 is up to 82.5 °C only. So, these molds retain their physical properties and safety profile.
The technique is cost effective as food grade straw which has been used is freely available and is very cheap and does not add to the cost of treatment significantly, whereas antibiotic bead preparation templates commercially available are very costly. It is easy to prepare without much of extra surgical time, as mold to prepare cement rod i.e., straw is easily available and after the cement sets in the mold then cast is obtained simply by removing the mold with an ordinary surgical blade without much of effort and does not require any technical expertise.
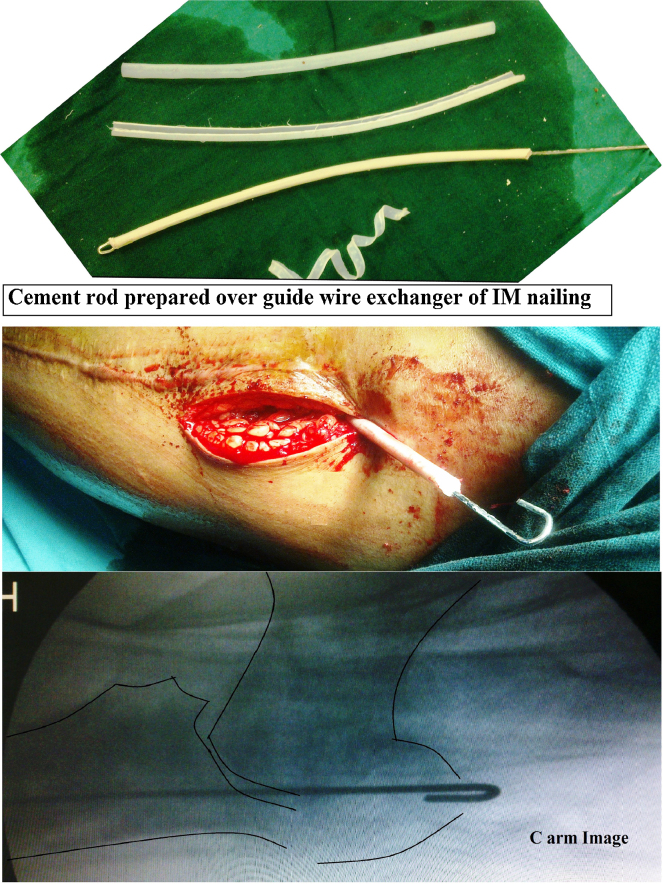
2.2. For preparing 5 mm PMMA rods
We have used low profile teflon tube guide wire exchanger (manufactured by Shakti Ortho-Surgicals India Pvt Ltd.) used in IM nailing as mold to make cement rods which was pre sterilized by autoclaving. Even a good quality teflon tube guide wire exchanger becomes soft after multiple autoclaving and could be easily cut. Alternatively, commercially available teflon tubes or soft silicone tubes of desired dimension could be used and preferably should be pre sterilized in glutaraldehyde 2% solution. In these tubes instead of SS wire/K wire we have used 1.8 or 2 mm Ilizarov wire as an internal support core material for imparting strength. Rest of the technique remains same.
In our technique after adding 4 g of antibiotic powder in 40 g pack of bone cement, we prepared a cured antibiotic impregnated cylindrical cement block of 64 g having a volume of 50 ml with density of 1.28 g/cm3 and the actual quantity of antibiotic contained per unit length of rod is described in Table 1.
Table 1.
Antibiotic contained in the rods prepared by our technique in comparison to antibiotic coated IM Nail.
| Type | Length | Antibiotic actually contained |
|---|---|---|
| PMMA Rod of 2.5 mm diameter | 10 cm | 40 mg |
| PMMA Rod of 5 mm diameter | 10 cm | 160 mg |
| Cement coated IM nail of 11 mm diameter (3 mm cuff of cement) | 10 cm | 368 mg |
2.3. Removal
Due to inherent stiffness and smoothness of rods they do not get entangled in fibrous tissues and fascia, thus it is easy to remove these rods by gently dilating the soft tissues and pulling them up by holding the protruded wire.
3. Results
Total seven cases were included in this series and the results were assessed at a minimum of three months follow up, the average follow up being 7.28 months. We have successfully treated seven cases of infected non-union by this technique and the details of the cases are elaborated in Table 2.
Table 2.
Results of our cases.
| Cases | Follow up at 3 months | Latest follow up | Result | |
|---|---|---|---|---|
| 1 | 44 years male presented with open fracture distal third both bone forearm, left with infected non-union with exposed and loose implants (DCP + Ex fix) | Uniting without clinico-radiological evidence of infection | 8 months | Good United without clinico-radiological evidence of infection |
| 2 | 26 years male presented with infected non-union of close inter-trochanteric fracture with sub trochanteric extension, left with implant failure (LCP, DCS) | Uniting without clinico-radiological evidence of infection | 24 months | Good United without clinico-radiological evidence of infection |
| 3 | 33 years male presented with infected non-union of close fracture shaft of ulna, right with implant failure (DCP) | Uniting without clinico-radiological evidence of infection | 5 months | Good United without clinico-radiological evidence of infection |
| 4 | 19 years female presented with infected non-union of fracture shaft of ulna, left with implant failure (DCP) | Infected union with discharging sinus. | 5 months | Satisfactory Infected union with scanty discharging sinus. |
| 5 | 24 years male presented with open fracture distal third both bone forearm, left with infected non-union with implant failure (Ex fix) | United without clinico-radiological evidence of active infection | 3 months | Good United without clinico-radiological evidence of active infection (controlled) |
| 6 | 22 years male presented with open fracture both bone forearm, right with infected non-union with loose square nails | Un united without clinico-radiological evidence of active | 3 months | Satisfactory Un united without clinico-radiological evidence of active infection (controlled) |
| 7 | 38 years female presented with open fracture shaft of humerus, right with infected non-union with loose Rush nails | Un united without clinico-radiological evidence of infection | Lost to follow up after 3 months | Satisfactory Un united without clinico-radiological evidence of infection |
While removing the rods we did not encountered any chip fragments of rods or debonding of cement over the wire or rod incarceration.
By our technique we were able to achieve union in five cases (71%). There was no evidence of infection in six cases (85.7%), although we had one case with infected union (14.5%) in our series.
For consideration of scientific community, we present two cases from our series in whom antibiotic impregnated PMMA rods had been fashioned and successfully used by our technique:
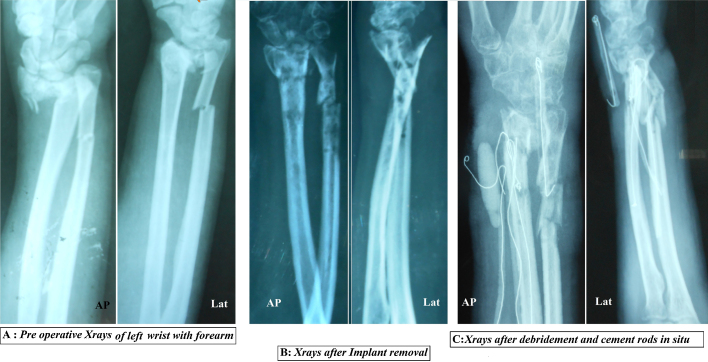
Case 1: 44 years male presented with open fracture distal third both bone forearm left, with infected non-union with exposed and loose implants (DCP + Ex Fix).
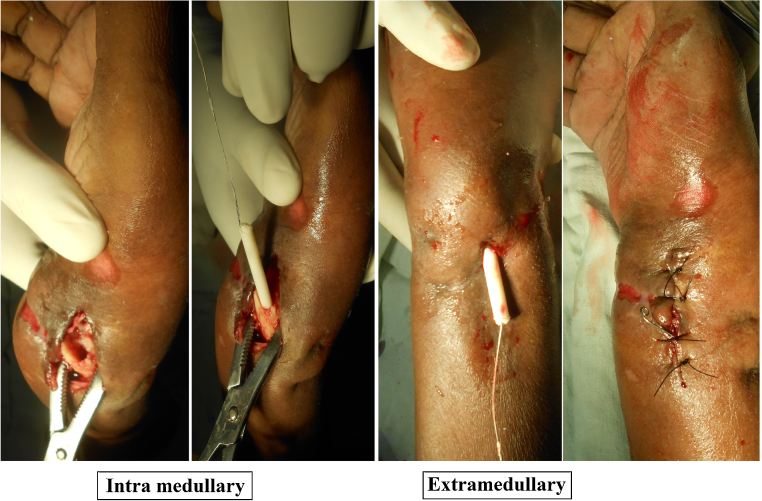
First stage: Implant was removed with surgical debridement and curettage of cavities and excision of sinus tract was performed. Then three, hand fashioned PMMA rods of 3 mm × 50 mm were placed in extra periosteal submuscular plane in distal forearm and 2.5 mm PMMA rod fashioned over 24 G SS wire of 100 mm length was placed in intramedullary cavity of radius through fracture site. Wound was closed in layers (Fig. 2, Fig. 3).
Fig. 2.
Stage one – sequential X rays of wrist with forearm.
Fig. 3.
Placement of PMMA antibiotic impregnated rods.
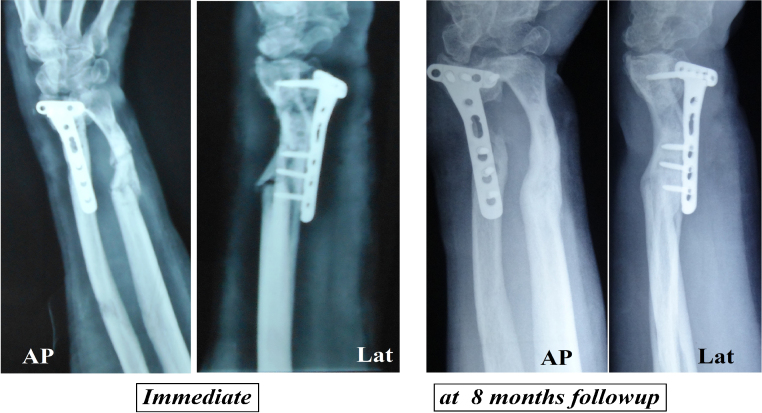
In the second stage after 6 weeks, removal of cement rods was done followed by autogenous bone grafting and internal fixation with Locked Juxta-articular T Plate (Fig. 4).
Fig. 4.
Stage two – sequential X rays of wrist with forearm.
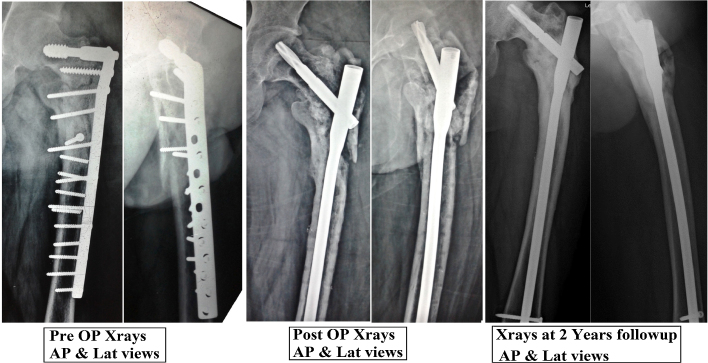
Case 2: 26 years male presented with infected non-union of close inter trochanteric fracture of femur left with sub trochanteric extension with implant failure (LCP, DCS).
First stage: Implant removal was done and a thorough surgical debridement was performed along with curettage of the cavity. This was followed by reaming of medullary canal from tip of trochanter till junction of distal and middle 1/3rd of shaft by flexible reamer of 8 mm size. The distal medullary canal was not reamed in order to prevent contamination of healthy medullary cavity. Thereafter hand fashioned antibiotic impregnated PMMA rod over Ilizarov wire (350 mm) was placed in the medullary cavity and antibiotic impregnated beads (5–10) prepared over 18 gauge SS wire was placed in the extra periosteal sub muscular plane in proximal thigh region (Fig. 5).
Fig. 5.
Stage one – intramedullary placement of cement rod in proximal femur.
In the second stage, after 6 weeks removal of both these antibiotic delivery systems was done followed by autogenous bone grafting and internal fixation with long PFN A-2 (Fig. 6).
Fig. 6.
Stage two – sequential X rays of left hip with thigh.
4. Discussion
Osseous infections are potentially a very serious condition and calls for an aggressive intervention into the matter, major concern being osteomyelitis in a fractured bone which may lead to delayed/non-union. Presence of compromised soft tissue condition complicates, and even worsens the situation.
Management of post traumatic infected non-union of fractures advocates staged procedures,5 but debridement to get rid of infection is the basic and most important procedure. Antibiotics can further be used as a means to control infection and if there is a fracture with or without implant in situ, one can suppress the infection and aim for delayed union. But in cases of established non-union or significant infection the management changes.
Several investigators2, 4, 15 have used antibiotic cement coated IM nails for stabilization of fractured long bones along with local antibiotic delivery with good outcomes but at times when there is severe osteolysis or obliterated or narrowed medullary cavity, it becomes difficult to use these nails. PMMA rods fashioned with our technique are quite helpful in these situations as far as stability component is considered, apart from splints and POP casts a spanning external fixator or bridging LCP with minimum number of screws can be used.
Several studies15, 18, 19 have shown that antibiotic cement beads have effective local antibiotic delivery owing to more surface area of spherical construct but removal is usually difficult in comparison to cylindrical construct. This difficulty in removal of antibiotic beads can also be overcome by using bio-degradable antibiotic delivery system20 but at the cost of compromised stability at the non-union site and increased expenditure. The elution of antibiotics can be enhanced by increased porosity and surface area of bone cement. Studies have shown that adding two antibiotics broadens the antibiotic spectrum and also increases the leaching, possibly by increasing the porosity of bone cement.15 This can be done by using PALACOS instead of PMMA which has been shown to have better antibiotic elution into the surrounding tissue. The elution of antibiotic is up to 3 cm only21 and depends on the local environment. So, it is necessary to place cement rods or beads as close as possible to the infected area.
Shyam et al.,3 in their study showed infection control in all the cases treated with ACIIN (Antibiotic cement impregnated intramedullary nail) in femur and tibia. Cheng et al.,11 in their study used antibiotic impregnated cement rods for treating intramedullary infections and achieved union in all twelve cases without any relapse of infection at an average of 59.1 month follow up. Similarly, Dhanasekhar et al.,22 showed eradication of infection in all the cases in their study using ACIIN for femur and tibia. Thones et al.,23 in their study using silicone tubing technique prepared ACIIN and showed low complication rates and achieved infection control in 85% cases of infected non-union. Comparing to this, in our study at average follow up of 7.28 months, we had achieved union in five cases (71%). There was no evidence of infection in six cases (85.7%), out of which four cases (57%) had a good union whereas two cases (29%) had a non-union, although we had one case with infected union (14.5%) in our series.
Local antibiotic delivery system holds a promising modality of treatment for handling difficult to control, chronic infections. Advantage of our technique is that we can easily prepare rods of required dimension and removal from medullary cavity and soft tissue is an easy task as compared to spherical construct (beads) in which removal is usually difficult. Limitation of our study is due to lesser number of cases included in the study, but we think that this article will motivate researchers to use this technique and come up with their results.
Conflicts of interest
The authors have none to declare.
References
- 1.Struijs P.A.A., Poolman R.W., Bhandari M. Infected nonunion of the long bones. J Orthop Trauma. 2007;21(August (7)):507–511. doi: 10.1097/BOT.0b013e31812e5578. [DOI] [PubMed] [Google Scholar]
- 2.Thonse R., Conway J. Antibiotic cement-coated interlocking nail for the treatment of infected nonunions and segmental bone defects. J Orthop Trauma. 2007;21(April (4)):258–268. doi: 10.1097/BOT.0b013e31803ea9e6. [DOI] [PubMed] [Google Scholar]
- 3.Shyam A.K., Sancheti P.K., Patel S.K., Rocha S., Pradhan C., Patil A. Use of antibiotic cement-impregnated intramedullary nail in treatment of infected nonunion of long bones. Indian J Orthop. 2009;43(October–December (4)):396–402. doi: 10.4103/0019-5413.55468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Riel R.U., Gladden P.B. A simple method for fashioning an antibiotic cement-coated interlocking intramedullary nail. Am J Orthop. 2010;39(1):18–21. [PubMed] [Google Scholar]
- 5.Buchholz H.W., Engelbrecht H. Depot effects of various antibiotics mixed with Palacos resins. Chirurg. 1970;41(11):511–515. [in German] [PubMed] [Google Scholar]
- 6.Baleani M., Persson C., Zolezzi C. Biological and biomechanical effects of vancomycin and meropenem in acrylic bone cement. J Arthroplasty. 2008;23(8):1232–1238. doi: 10.1016/j.arth.2007.10.010. [DOI] [PubMed] [Google Scholar]
- 7.Cerretani D., Giorgi G., Fornara P. The in vitro elution characteristics of vancomycin combined with imipenem-cilastatin in acrylic bone-cements: a pharmacokinetic study. J Arthroplasty. 2002;17:619–626. doi: 10.1054/arth.2002.32184. [DOI] [PubMed] [Google Scholar]
- 8.Gonzalez Della Valle A., Bostrom M., Brause B. Effective bactericidal activity of tobramycin and vancomycin eluted from acrylic bone cement. Acta Orthop Scand. 2001;72–3:237–240. doi: 10.1080/00016470152846547. [DOI] [PubMed] [Google Scholar]
- 9.Hanssen A.D. Local antibiotic delivery vehicles in the treatment of musculoskeletal infection. Clin Orthop Relat Res. 2005;437:91–96. doi: 10.1097/01.blo.0000175713.30506.77. [DOI] [PubMed] [Google Scholar]
- 10.Adams K., Couch L., Cierny G., Calhoun J., Mader J.T. In vitro and in vivo evaluation of antibiotic diffusion from antibiotic-impregnated PMMA beads. CORR. 1992;278(May):244–252. [PubMed] [Google Scholar]
- 11.Fan C.-Y., Hsieh M.-S., Chen W.-M., Chen C.-F. Successful management of infected intramedullary nailing with reaming, lavage and insertion of antibiotic-impregnated cement rods. J Exp Clin Med. 2011;3(3):137–141. [Google Scholar]
- 12.Paley D., Herzenberg J.E. Intramedullary infections treated with antibiotic cement rods: preliminary results in nine cases. J Orthop Trauma. 2002;16(November–December (10)):723–729. doi: 10.1097/00005131-200211000-00007. [DOI] [PubMed] [Google Scholar]
- 13.Qiang Z., Jun P.Z., Jie X.J., Hang L., Bing L.J., Cai L.F. Use of antibiotic cement rod to treat intramedullary infection after nailing: preliminary study in 19 patients. Arch Orthop Trauma Surg. 2007;127(December (10)):945–951. doi: 10.1007/s00402-007-0315-x. [DOI] [PubMed] [Google Scholar]
- 14.Bharti A., Swaroop A., Kumar P., Rawat A. A simple and cost-effective technique for vertebroplasty. Tech Orthop. 2015;30(March (1)):29–31. [Google Scholar]
- 15.Samuel S., Ismavel R., Boopalan P.R.J.V.C., Matthai T. Practical considerations in the making and use of high-dose antibiotic-loaded bone cement. Acta Orthop Belg. 2010;76:543–545. [PubMed] [Google Scholar]
- 16.Vanessa B., Philipp K., Thomas M., Armando G. Temperature evaluation during PMMA screw augmentation in osteoporotic bone – an in vitro study about the risk of thermal necrosis in human femoral heads. J Biomed Mater Res B: Appl Biomater. 2009;90 B:842–848. doi: 10.1002/jbm.b.31353. [DOI] [PubMed] [Google Scholar]
- 17.http://www.chandra-asri.com/products.php?component_product_id=6, http://www.chandraasri.com/UserFiles/File/TDS/TDS-HY3.8FY.pdf, 2016 April 14th.
- 18.Jiranek W.A., Hanssen A.D., Greenwald A.S. Anti bioticloaded bone cement for infection prophylaxis in total joint replacement. J Bone Jt Surg. 2006;88-A:2487–2500. doi: 10.2106/JBJS.E.01126. [DOI] [PubMed] [Google Scholar]
- 19.Masri B.A., Duncan C.P., Beauchamp C.P., Paris N.J., Arntorp J. Effect of varying surface patterns on antibiotic elution from anti-biotic-loaded bone cement. J Arthroplasty. 1995;10:453–459. doi: 10.1016/s0883-5403(05)80145-7. [DOI] [PubMed] [Google Scholar]
- 20.Dabov G.D. Osteomyelitis. In: Canale S.T., Beaty J.H., editors. Campbell's Operative Orthopaedics. 12th ed. Mosby/Elsevier; Philadelphia: 2013. pp. 737–738. [Google Scholar]
- 21.Cleveland K.B. General principles of infection. In: Campbell W.C., Canale S.T., Beaty J.H., editors. Campbell's Operative Orthopaedics. 11th ed. Mosby/Elsevier; Philadelphia: 2008. pp. 675–694. [Google Scholar]
- 22.Dhanasekhar R., Jacob P.J., Francis J. Antibiotic cement impregnated nailing in the management of infected non-union of femur and tibia. Kerala J Orthop. 2013;26:93–97. [Google Scholar]
- 23.Thones R., Conway J.D. Antibiotic cement coated nails for the treatment of infected nonunions and segmental bone defects. J Bone Jt Surg Am. 2008;90:163–174. doi: 10.2106/JBJS.H.00753. [DOI] [PubMed] [Google Scholar]