Abstract
Aim
To evaluate 30 patients who underwent distraction osteogenesis with monorail external fixator for complex femoral nonunion.
Method
Complex femoral nonunion includes infective non-union, gap nonunion, and limb-length discrepancy secondary to traumatic bone loss, which needs specialized treatment to ensure the functional integrity of femoral bone. 30 patients, including 28 male and 2 female (aged 22–62 years) patients, underwent surgical debridement followed by bone transport with monorail fixator. The lengthening index, radiographic consolidation index, functional status, bone healing, and various problems, obstacles, and complications encountered during the treatment were assessed.
Results
Patients underwent a mean of 2.2 (range 1–4) surgeries before presentation. The mean bone defect after surgical debridement was 5.83 cm (range 2–16 cm). The mean treatment duration was 204.7 days (range 113–543 days). The mean lengthening index was 13.06 days/cm with range from 12 to 16 days/cm. Mean maturation index was 23.51 days/cm with range from 17 to 45.5 days/cm. In our study, bone result was excellent in 17, good in 9, fair in 3, and poor in 1 patient. In our study functional outcome is excellent in 9 [30%], good in 14 [46.67%], fair in 5, and poor in 2 patients. In our study, we encountered 34 problems, 17 obstacles, and 8 complications.
Conclusion
We concluded that monorail external fixator is an effective treatment option for complex nonunion femoral shaft fracture and its functional outcome is comparable with any other treatment options. Lack of complications and its effectiveness makes monorail external fixator the treatment of choice for complex nonunion femoral shaft.
Keywords: Femur, Nonunion, External fixator, Osteogenesis, Ilizarov
1. Introduction
Complex femoral nonunion constituting infective nonunion, gap nonunion, and limb-length discrepancy secondary to bone loss needs specialized planning and assessment. Getting union along with correction of limb-length discrepancy is a challenging job for the orthopedic surgeon. It needed a comprehensive approach for the management of these types of nonunion, with managing of the nonunion and the bone gap simultaneously. Most often, segmental bone defects are managed by transplantation of vascularized or nonvascularized autogenous bone, allograft bone transplantation, or segment transport.1 However, problems with vascularized bone grafts include donor site morbidity,2 possibility of necrosis due to anastomotic complications,3 long remodeling time, and high fracture rate.4 There are many other ways to treat femoral nonunion. Internal fixation and external fixation along with biophysical enhancement are the classified methods of treatment. Internal fixation along with bone grafting can be done in aseptic nonunion without bone gap. In cases of infective nonunion, in which bone gap is created surgically after thorough debridement, and in cases with traumatic bone gap, bone transport based on principle of distraction osteogenesis is an effective way of getting union and functional limb without limb-length discrepancy.
Bone transport using external fixators alone, as first introduced by Ilizarov, needs long-term management with external fixators.5 Ilizarov external fixation works on the principle of distraction osteogenesis and is commonly used as effective treatment option for complex femoral nonunion. Ilizarov ring external fixator is the established mode of treatment. But it has many demerits as it is too bulky and cumbersome, has many complications like multiple pin track infections, pin breakage, injury to opposite thigh, knee stiffness, bone osteomyelitis, distraction failure, vascular complications, refracture, etc.6 Monorail unilateral external fixator based on principle of distraction osteogenesis for bone transport can be used as an effective treatment modality in these complex nonunion femoral shaft fractures. Therefore, we had used monorail fixator in our prospective study of managing 30 patients with femoral nonunion.
2. Material and methods
Our prospective study from 2010 to 2013 included 30 patients (28 male and 2 female) who underwent surgical treatment for complex femoral nonunion. This study was approved by the Medical college ethical board. Informed consent was taken from all the patients before including them in the study. A thorough history regarding mode and mechanism of injury, previous surgeries, and clinical examinations was undertaken. Patient demographics, presenting symptoms and duration, medical history, the presence of tenderness and pain, skin condition, shortening, deformity and function of the knee joint and distal neurovascular status, sinus, and pus discharge were recorded. The diagnostic workup of the patient included hemoglobin, TLC, differential leukocyte count, ESR and CRP, bleeding time, clotting time, blood group, random blood sugar, blood urea, serum sodium, serum potassium, roentgenogram of the affected limbs and chest, and sample for culture from the wound in open fractures (Table 1, Table 2).
Table 1.
Functional outcome according to ASAMI classification after bone transport with monorail fixator [n = 30].
| Functional outcome | Patients | Percentage [%]. |
|---|---|---|
| Excellent | 9 | 30.00 |
| Good | 14 | 46.67 |
| Fair | 5 | 16.66 |
| Poor | 2 | 6.67 |
Almost 77% patients got a healthy functional outcome and were satisfied with the treatment.
Table 2.
Complications according to classification of “PALEY” [n = 30].
| Difficulty | No. of patients | Problem | Obstacles | True complication |
|---|---|---|---|---|
| Superficial pin track infections | 26 | 26 | – | – |
| Residual shortening | 1 | – | 1 | |
| Severe pain | 8 | 8 | – | – |
| Knee contracture | 8 | – | – | 8 |
| Delayed consolidation | 5 | – | 5 | – |
| Angular deformity > 5° | 11 | – | 11 | – |
| Total | 59 | 34 | 17 | 8 |
| Complication rate | 100 | 57.6% | 28.80 | 13.6% |
All patients had a bone defect of >5 cm (preoperatively or after resection and debridement). Patient was placed on a simple operating table, which was compatible with C-arm image intensifier. The affected limb was painted and draped, and draping was done in such a way to get 90° of flexion intraoperatively to get maximum length of quadriceps muscle while applying the fixator. In cases of infected nonunion, lateral approach for femur was used. After dissection in proper planes, infected bone was exposed. The dead bone was resected and the infected tissues and sinus tract were debrided; soft tissue debridement was done adequately. Cortical bleeding – ‘Paprika sign’ – was the end point of debridement [Fig. 2] and surgically bone gap was created between healthy bone ends.7, 8, 9, 10, 11, 12 In cases of gap nonunion, bone gap was already present. Sclerosed fracture margin was freshened up till healthy bleeding bone. As bone gap was present, proper maintenance of femur alignment and rotation was necessary. In case of mid-shaft femur bone gap, alignment was made with the temporary application of 4.5 mm high-profile broad DCP and holding it with plate holding forceps or stainless steel wire or with application of proximal and distal screws. The plate was later removed after application of monorail fixator.
Fig. 2.
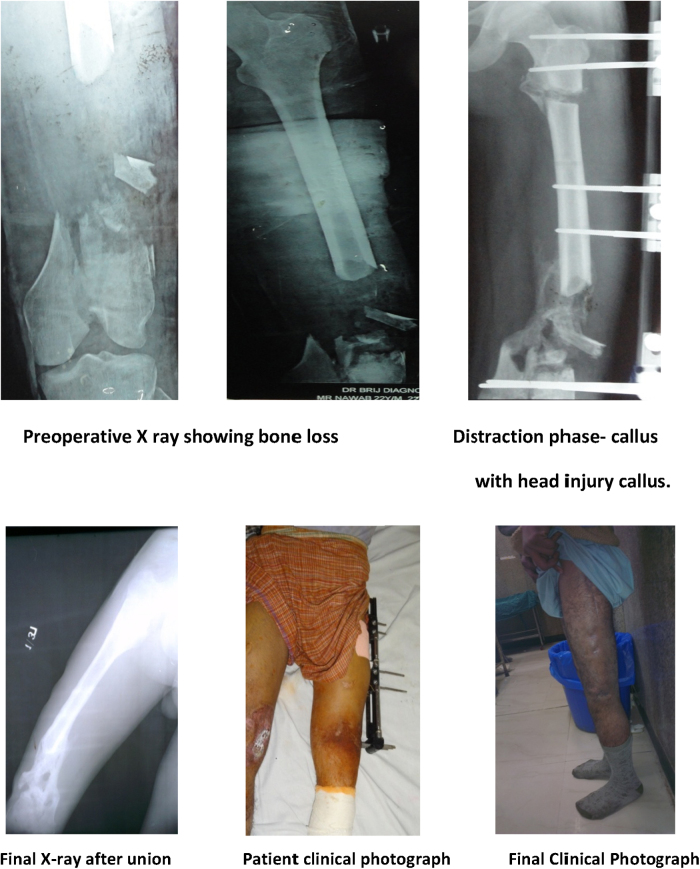
Young male patient suffered RTA with head injury with compound supracondylar femur fracture with 11 cm bone loss managed with monorail fixator to achieve limb length. Figure showing abundant head injury callus.
In cases of distal supracondylar femur gap, alignment was made with the application of anatomical precontoured distal femur locking plates (DFLP) and holding the plate with stainless steel wire or screws. Temporary application of these plates to get proper alignment and rotation allows 90 degrees knee flexion to get maximum length of quadriceps. Application of fixator with 90° knee flexion prevents quadriceps contracture and thus prevents knee stiffness. Fixation was performed using a monolateral external fixator. In all patients, the Rail External Fixator System (SH Pitkar Orthotools, Pune, India) was used. In 18 cases [60%], descending bone transport was done; in 8 cases, ascending bone transport was done, and in 4 cases, mid-diaphyseal lengthening was done (Fig. 3).
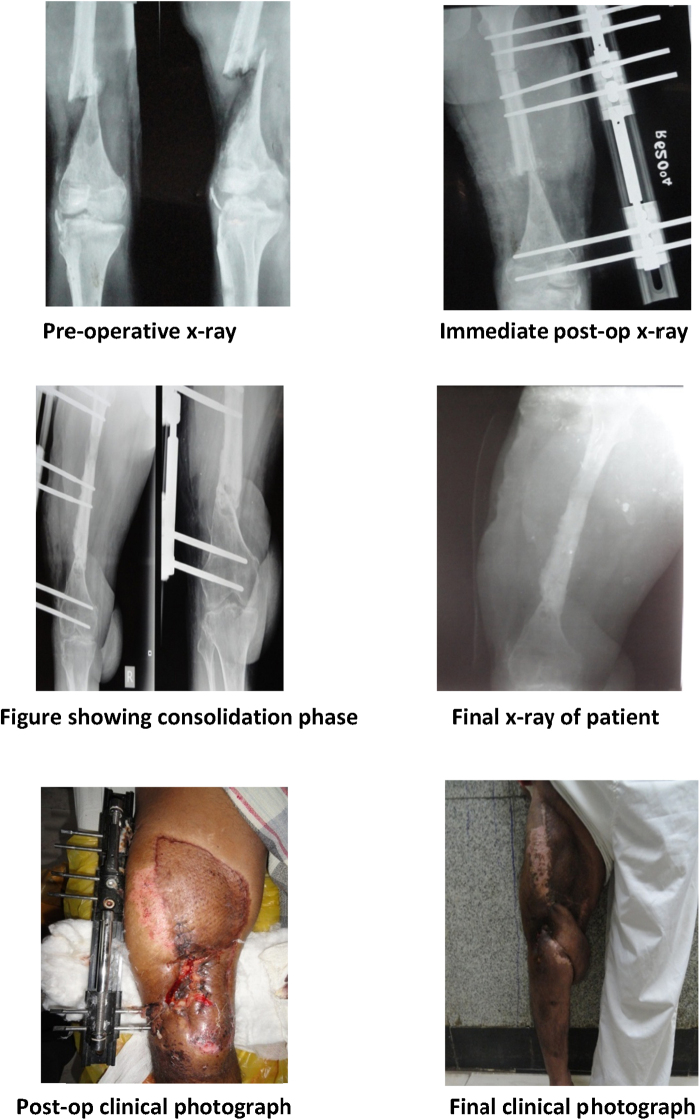
Fig. 3.
Young adult male suffered RTA with compound supracondylar femur fracture with 6 cm bone loss with soft tissue loss. Managed with monorail fixator and flap coverage later on.
Injectable antibiotics [cefazolin 2 g/6 h and gentamicin 3 mg/kg/day] were started for one week. Antibiotic were later on modified according to pus/tissue culture and sensitivity results. Antibiotic treatment was continued for a minimum of six weeks or until ESR and CRP becomes normal in cases of infected nonunion. Drain was removed on 2nd postoperative day, and knee physiotherapy, including static and dynamic quadriceps exercises and hamstring strengthening exercises, were advised. Partial weight bearing with walker assistance was started as soon as the patient's comfort allowed. Pin sites were dressed daily with sterile gauze and iodine for 2 weeks and then daily cleaned with spirit swabs only. Distraction at the rate of 0.25 mm four times a day [one-quarter rotation of compression–distraction unit] was started on 7th postoperative day. The patient was followed every fortnight and evaluated with X-rays for the quality and pattern of distraction callus; and the distraction rate is modified accordingly at 0.25 mm, twice to four times a day.
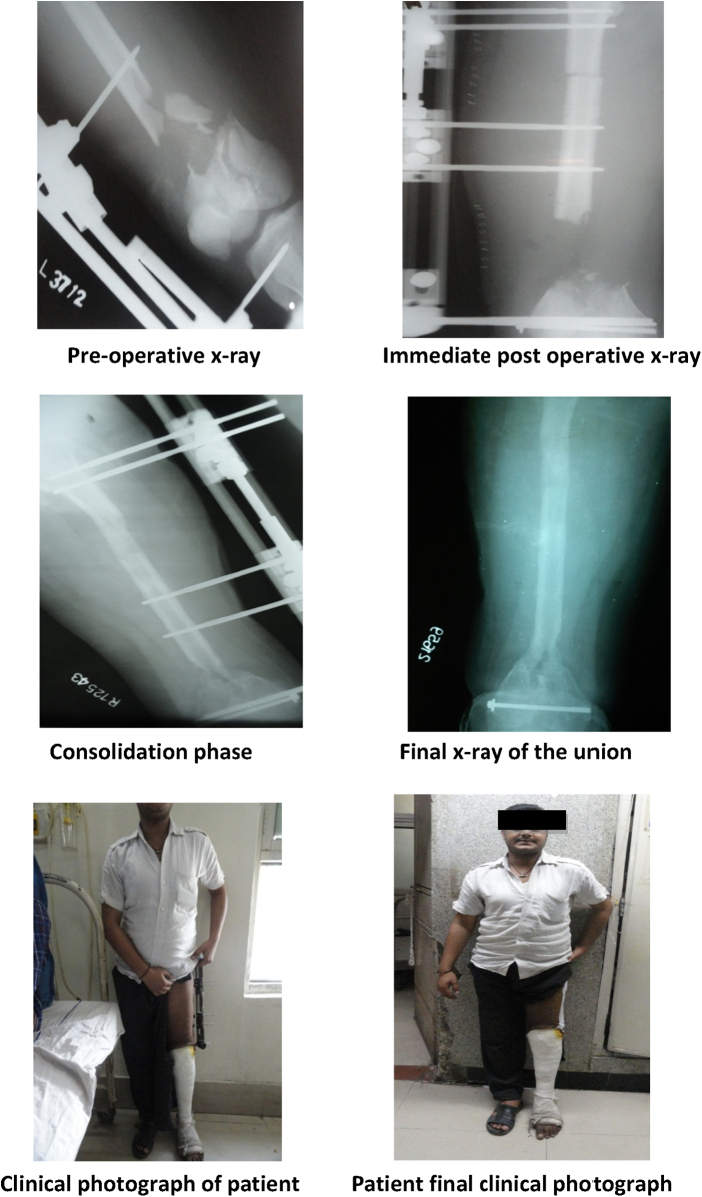
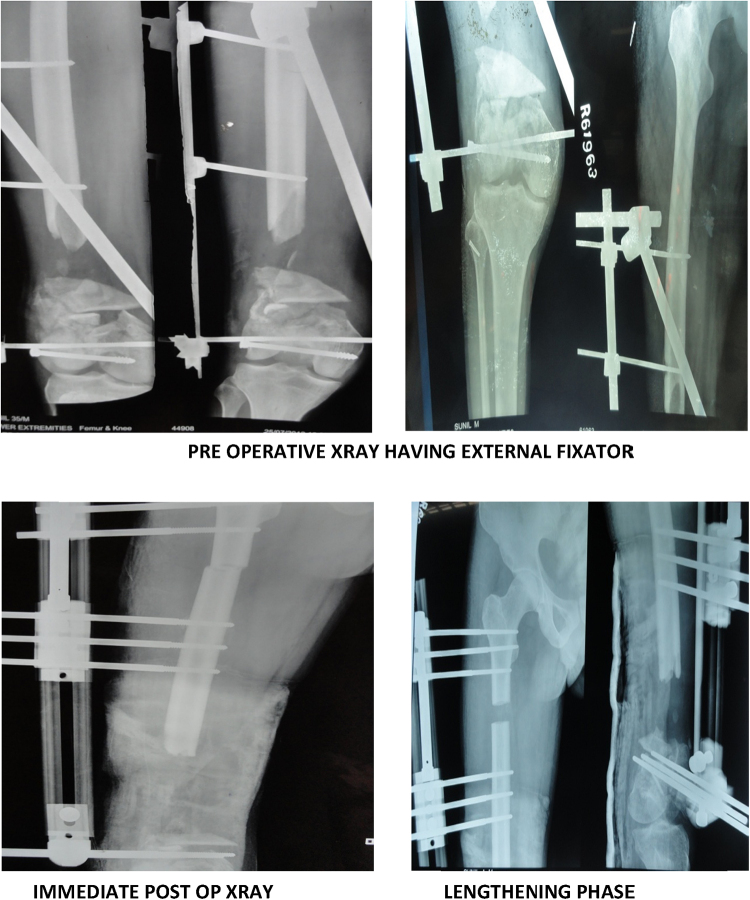
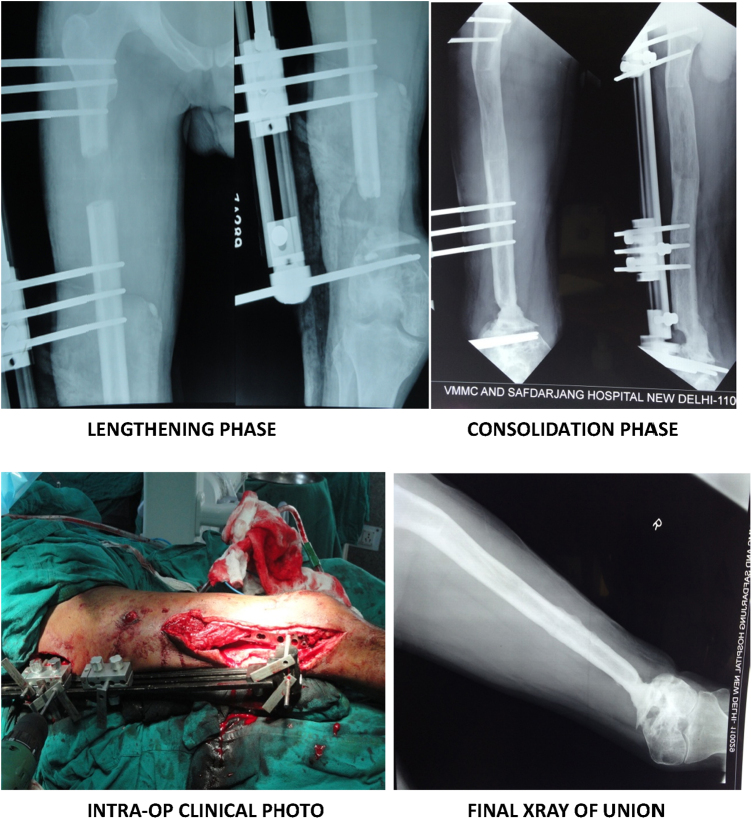
Failure of consolidation at the docking site in bone transport can present in follow-up. In such cases, the length of time elapsing between corticotomy and docking promotes the formation of fibrous tissue at the docking site.13, 14, 15 This is often an insoluble obstacle against consolidation, and warrants further surgery in order to clean and decorticate the region and get healthy bone ends (Fig. 1, Fig. 2, Fig. 3, Fig. 4, Fig. 5, Fig. 6).
Fig. 1.
Young adult male suffered RTA with compound supracondylar femur fracture with 12 cm bone loss. Primarily managed with external fixator elsewhere by distraction osteogenesis with monorail fixator.
Fig. 4.
Elsewhere managed case of compound supracondylar femur fracture with 15 cm shortening.
Fig. 5.
Clinical photograph showing use of plate to maintain alignment while applying monorail.
Fig. 6.
Final clinical photograph.
3. Outcome measures
The lengthening index was defined as the “Days of bone transport/lengthening per cm gain in length”.
Maturation index is the time required for 1 cm of newly formed callus to consolidate and it is determined by dividing the total length of time in days from time of stopping distraction to the time when the fixator is removed by the total increase in the length of the bone.
The treatment index was defined as the time (in days) to the appearance of consolidation in at least three cortices on the anteroposterior and lateral radiographs divided by the total amount of bone transported and/or the amount of lengthening (in cm).
Healing index [external fixator index] is determined as days of fixator use/centimeters of length gained. It is also termed as external fixator index.
Classification of callus was done as proposed by Li et al.16 classifying shape into fusiform, cylindrical, concave, lateral, central.
Functional assessment was done according to “ASAMI classification of bone transport applicable for femur and tibia bone”, which was based on five criteria: observable limp, stiffness of knee or hip [loss of >70° of knee flexion or loss of >15 of extension; loss of >50% hip motion in comparison with the normal contralateral side], soft tissue sympathetic dystrophy, pain that reduced activity or disturbed Sleep, and inactivity [because of unemployment or an inability to return to daily activities due to the injury]. The functional result was classified by the following criteria: an excellent result was if the patient was active, able to accomplish his/her daily activities, and the other four criteria were absent. A good result was if the patient was active, but one or two of the other criteria were present. A fair result was if the patient was active, with three or four of the other criteria present. A poor result was if the patient was inactive, regardless of the presence of other criteria.
The bone results were determined according to “ASAMI classification of bone transport”,17, 18 which include 4 criteria: union, infection, deformity, and leg-length discrepancy. The bone bridging was followed at the site of the contact of transported and target fragments, as well as at the site of the new bone formation. The fracture was considered healed if an X-ray image revealed corticalization, if no clinical signs of motion or bending of fragments after axial loosening of the construction were found, and if the patient was able to walk without pain, relying on the operated leg. Bone healing was evaluated as follows: an excellent bone result was defined as a union without infection, with less than 7° deformity and less than 2.5 cm leg-length inequality. A good result was defined as a union, with two out of three criteria for an excellent result present. A fair result was defined as union, with one of the three criteria present. A poor result was a nonunion or refracture, without any of the above three criteria fulfilled.
To evaluate complications that occur during and after distraction osteogenesis, the classification according to Paley19 was used, as follows: A problem is a difficulty in the course of distraction/consolidation, which is fully resolved by the end of the treatment period by nonoperative means; an obstacle is a difficulty that arises in the course of distraction/consolidation that is fully resolved by the end of the treatment period by operative means; a true complication is a difficulty that occurs during distraction or in a period of consolidation, and remains unresolved till the end of the treatment, or remains unresolved after the treatment is completed.
4. Results
30 patients, including 28 male and 2 female (aged 22–62 years), underwent a mean of 2.2 (range 1–4) surgeries before presentation. Right side involvement is more common than left with ratio of 19:11. Mode of injury was road traffic accidents (n = 19), fall (n = 8), and gunshot injury (n = 3). Complex femoral nonunion includes supracondylar femur fracture with traumatic bone loss (n = 10), infected nonunion shaft of femur (n = 18), and gap nonunion shaft of femur (n = 2).
Mean preoperative shortening was 2.30 cm (range 0–6 cm), which after surgical debridement becomes 5.83 ± 2.972 cm (range 2–16 cm). Mean time of distraction phase was 74.83 days (range 32–223 days). Mean lengthening index was of 13.06 days/cm (range 12–16 days/cm). Maturation index was 23.51 ± 5.93 days/cm (range 17–45.5 days/cm). Mean healing index was 36.536 days/cm (range 28–61.5 days/cm) with rate of distraction 1 mm/day. Total treatment duration ranges from 113 to 543 days, with a mean of 204.77 ± 88.35 [mean ± s.d.].
Distraction callus pattern was found to having fusiform pattern in 5 patients, cylindrical in 16 patients, concave in 5 patients, lateral in 3 cases, and central in 1 case. The most predominant type of callus pattern is cylindrical, being 53.33% among the total.
Bone result was excellent in 17, good in 9, fair in 3, and poor in 1 patient. In our study, functional outcome is excellent in 9 [30%], good in 14 [46.67%], fair in 5, and poor in 2 patients. None of the patients had neurovascular complication, joint instabilities, or newly formed bone fracture. The problems encountered include superficial pin tract infection in 26 cases [86.67%], severe pain in 8 patients [26.67%], knee stiffness in 8 patients [26.67%], and angular deformity of femur at the site of docking in 11 patients [36.67%]. In 5 patients [16.67%], we got delayed union which was treated with autologous bone graft. In our study, we encountered 34 problems, 17 obstacles, and 8 complications.
5. Discussion
Complex nonunion femoral shaft fractures include infective nonunion, gap nonunion, and atrophic nonunion with limb-length discrepancy secondary to traumatic bone loss. Infected nonunion of the supracondylar region of the femur is uncommon and is mostly due to a high-grade open fracture with bony comminution and segmental bone loss or after infection of internal fixation of a comminuted closed fracture.20 Soft tissue loss with multiple sinuses, osteomyelitis, osteopenia, complex multiplanar deformities, multibacterial multidrug-resistant infection, limb-length discrepancies, adjacent joint stiffness, and other comorbidities, like smoking etc. all complicate treatment and recovery.21 Reconstruction for infected nonunion is difficult; the underlying bone defect, limb and bone shortening, and deformity may further complicate matters.22 These factors make an unfavorable milieu for fracture union.23 Treatments for infected nonunion of the femur with bone loss include debridement, local/free muscle tissue transfer, and Ilizarov circular fixator/bone transport through an external fixator over a nail/monorail external fixator application. The latter is increasingly popular, as it can correct deformities, regenerate new bone via distraction osteogenesis, correct limb-length discrepancy, and enable weight bearing and early rehabilitation during the course of treatment.
The Ilizarov technique of distraction osteogenesis is a salvage procedure for these complexities. According to Ilizarov, gradual traction on living tissues creates stress that stimulates histogenesis and promotes regeneration and active growth of tissues (bone, muscle, fascia, tendon, nerve, vessels, skin, and its appendages). This principle is called the law of tension stress.24 The basic principles of the Ilizarov method include stable fixation, a low-energy corticotomy with gradual distraction, and osteogenesis by enhancing intramembranous ossification.25, 26 Femoral reconstruction, using the Ilizarov principle by an external fixator application, offers the surgeon an approach to a wide variety of femur pathologies as it allows to perform simultaneous limb lengthening as well as allowing correction of deformities and bone transport.7, 27, 28 The usual complications common with the Ilizarov ring external fixator are pin site infections, decreased joints ROM, neurological complications, and new deformities by inadvertent bone transport. In the lengthening group, the most common complications encountered were knee stiffness and contractures; this complication has been encountered by multiple surgeons with rates ranging from 0% to 100%.
Few studies have been conducted to assess bone transport by external fixator over an intramedullary nail [monorail assembly] to shorten the treatment duration.7, 13 The long duration of bone transport and waiting consolidation is intolerable for patients but there is a risk of infection extending along the bone. Mainly, patients with complex femoral nonunion had already undergone multiple operations. The additional costs for the intramedullary nail, antibiotic-loaded PMMA beads or antibiotic bone cement, repeated infected tissue cultures, need for frozen sections, prolonged courses of intravenous antibiotics, multiphasic procedures [Wide resection of infected/dead bone, nail insertion, incorporation of external fixator, corticotomy, and fixator removal, with or without bone grafting], and prolonged hospital admissions pose a psychological, and financial burden for most patients in developing countries.29 The risk of creating an osteomyelitis with lengthening over nail (LON) is a known complication with infection rate of approx. 22% being reported.30, 31, 32
Monolateral fixators for bone transport are simple in design and application, easy to perform surgical procedure while maintaining it, and easy to remove in outdoor setting. Its tapered and hydroxyapatite-coated pins increase anchorage to bone and decrease the risk of bone infection. The monorail unilateral fixator has strong appeal for patients as it has better compliance and patients are not to be encumbered with a ring circular fixator on the thigh; however, the deformity correction after lengthening is less and as such the surgical planning technique and after care have to anticipate this factor.
Nonetheless, a monorail unilateral fixator is widely suitable for the majority of cases in need of femoral lengthening encountered in clinical practice.
Limitations of this study included the absence of a control group, a small cohort of patients, and lacking of long-term follow-up.
Conflicts of interest
The authors have none to declare.
References
- 1.Mekhail A., Abraham E., Gruber B., Gonzalez M. Bone transport in the management of posttraumatic bone defects in the lower extremity. J Trauma. 2004;56(2):368–378. doi: 10.1097/01.TA.0000057234.48501.30. [DOI] [PubMed] [Google Scholar]
- 2.El-Gammal T., Shiha A., El-Deen M. Management of traumatic tibial defects using free vascularized fibula or Ilizarov bone transport: a comparative study. Microsurgery. 2008;28(5):339–346. doi: 10.1002/micr.20501. [DOI] [PubMed] [Google Scholar]
- 3.Benacquista T., Kasabian A., Karp N. The fate of lower extremities with failed free flaps. Plast Reconstr Surg. 1996;98(5):834–840. doi: 10.1097/00006534-199610000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Minami A., Kimura T., Matsumoto O., Kutsumi K. Fracture through united vascularized bone grafts. J Reconstr Microsurg. 1993;9(3):227–232. doi: 10.1055/s-2007-1006649. [DOI] [PubMed] [Google Scholar]
- 5.Song H.R., Cho S., Koo K., Jeong S., Park Y.J., Ko J.H. Tibial bone defects treated by internal bone transport using the Ilizarov method. Int Orthop. 1998;22(5):293–297. doi: 10.1007/s002640050263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Iacobellis C., Berizzi A., Aldegheri R. Bone transport using the Ilizarov method: a review of complications in 100 consecutive cases. Strat Traum Limb Recon. 2010;5:17–22. doi: 10.1007/s11751-010-0085-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kocaoglu M., Eralp L., Rashid H., Sen C., Bilsel K. Reconstruction of segmental bone defects due to chronic osteomyelitis with use of an external fixator and an intramedullary nail. J Bone Joint Surg Am. 2006;88:2137–2145. doi: 10.2106/JBJS.E.01152. [DOI] [PubMed] [Google Scholar]
- 8.Krishnan A., Pamecha C., Patwa J. Modified Ilizarov technique for infected nonunion of the femur: the principle of distraction-compression osteogenesis. J Orthopaed Surg. 2006;14(3):265–272. doi: 10.1177/230949900601400307. [DOI] [PubMed] [Google Scholar]
- 9.Cattaneo R., Catagni M., Johnson E. The treatment of infected nonunion and segmental defects of the tibia by the methods of Ilizarov. Clin Orthop. 1992;280:143–152. [PubMed] [Google Scholar]
- 10.Cierny G., Mader J., Penninck J. A clinical staging system for adult osteomyelitis. Clin Orthop Relat Res. 2003;414:7–24. doi: 10.1097/01.blo.0000088564.81746.62. [DOI] [PubMed] [Google Scholar]
- 11.Green S., Jackson J., Wall D., Marinow H., Ishkanian J. Management of segmental defects by the Ilizarov intercalary bone transport method. Clin Orthop Relat Res. 1992;280:136–142. [PubMed] [Google Scholar]
- 12.Tetsworth K., Cierny G., 3rd Osteomyelitis debridement techniques. Clin Orthop Relat Res. 1999;360:87–96. doi: 10.1097/00003086-199903000-00011. [DOI] [PubMed] [Google Scholar]
- 13.Raschke M., Mann J., Oedekoven G., Claudi B. Segmental transport after unreamed intramedullary nailing. Preliminary report of a “monorail” system. Clin Orthop Relat Res. 1992;(282):233–240. [PubMed] [Google Scholar]
- 14.Scuderi C., Ippolito A. Non-union of supra-condylar fractures of the femur. J Int College Surg. 1952;17:1–18. [PubMed] [Google Scholar]
- 15.May, Jupiter J., Waland A., Byrd H. Clinical classification of post traumatic tibial osteomyelitis. Current concept review. J Bone Joint Surg. 1989;71a:1422–1428. [PubMed] [Google Scholar]
- 16.Li R., Saleh M., Yang L., Coulton L. During bone radiographic classification of osteogenesis distraction. J Orthop Res. 2006;24(3):339–347. doi: 10.1002/jor.20026. [DOI] [PubMed] [Google Scholar]
- 17.Maiocchi A., Aronson J. Operative Principles of Illizarov: Fracture Treatment, Non-union, Osteomyelitis, Lengthening, Deformity Correction. Williams and Wilkins; Baltimore: 1991. Non-union of the femur; pp. 245–262. [Google Scholar]
- 18.Catagni M., Villa A. Operative Principles of Illizarov: Fracture Treatment, Non-union, Osteomyelitis, Lengthening, Deformity Correction. Williams and Wilkins; Baltimore: 1991. Non-union of the leg (tibia) pp. 199–214. [Google Scholar]
- 19.Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990;250:81–104. [PubMed] [Google Scholar]
- 20.Chapman M.W., Finkemeier C.G. Treatment of supra-condylar non-unions of the femur with plate fixation and bone graft. J Bone Joint Surg. 1999;81a:1217–1228. doi: 10.2106/00004623-199909000-00003. [DOI] [PubMed] [Google Scholar]
- 21.Jain Ak., Sinha S. Infected nonunion of the long bones. Clin Orthop Relat Res. 2005;431:57–65. doi: 10.1097/01.blo.0000152868.29134.92. [DOI] [PubMed] [Google Scholar]
- 22.Peter A., Struijs A., Rudolf W., Poolman, Bhandari M. Infected nonunion of the long bones. J Orthop Trauma. 2007;21:507–511. doi: 10.1097/BOT.0b013e31812e5578. [DOI] [PubMed] [Google Scholar]
- 23.Meyer S., Weiland A., Willeneger H. The treatment of infected nonunion of fractures of long bones. J Bone Joint Surg. 1975;57a:836–842. [PubMed] [Google Scholar]
- 24.Charnley J., Baker Sl. Compression arthrodesis of the knee. A clinical and histological study. J Bone Joint Surg. 1952;34b:187–199. doi: 10.1302/0301-620X.34B2.187. [DOI] [PubMed] [Google Scholar]
- 25.Ilizarov G. The tension-stress effect on the genesis and growth of tissues: Part I. The influence of stability of fixation and soft-tissue preservation. Clin Orthop Relat Res. 1989;238:249–281. [PubMed] [Google Scholar]
- 26.De Pablos J., Barrios C., Alfaro C., Canadell J. Large experimental segmental bone defects treated by bone transportation with monolateral external distractors. Clin Orthop Relat Res. 1994;298:259–265. [PubMed] [Google Scholar]
- 27.Ali F., Saleh M. Treatment of distal femoral non-unions by external fixation with simultaneous length and alignment correction. Injury. 2002;33:127–134. doi: 10.1016/s0020-1383(01)00032-8. [DOI] [PubMed] [Google Scholar]
- 28.Green S.A. Skeletal defects. A comparison of bone grafting and bone transport for segmental skeletal defects. Clin Orthop. 1994;301:111–119. [PubMed] [Google Scholar]
- 29.Arora S., Batra S., Gupta V., Goyal A. Distraction osteogenesis using a monolateral external fixator for infected non-union of the femur with bone loss. J Orthopaed Surg. 2012;20(2):185–190. doi: 10.1177/230949901202000210. [DOI] [PubMed] [Google Scholar]
- 30.Simpson A., Cole A., Kenwright J. Leg lengthening over an intramedullary nail. J Bone Joint Surg. 1999;81:1041–1045. doi: 10.1302/0301-620x.81b6.9359. [DOI] [PubMed] [Google Scholar]
- 31.Kristiansen L., Steen H. Lengthening of the tibia over an intramedullary nail, using the Ilizarov external fixator. Major complications and slow consolidation in lengthenings. Acta Orthop Scand. 1999;70:271–274. doi: 10.3109/17453679908997806. [DOI] [PubMed] [Google Scholar]
- 32.Patel M., Herzenberg J. Current trends in limb lengthening. Curr Opin Orthop. 2000;11:431. [Google Scholar]