Abstract
Background
Sudden cardiac death (SCD) is a major cause of mortality secondary to coronary artery disease (CAD) in the industrialized societies. Although South Asians have a high prevalence of CAD, the frequency and underlying pathology of SCD among this population are unknown.
Methods
Medical records of consecutive patients presenting with unexplained sudden death (USD) in a tertiary care center were reviewed. Patients with trauma, violent deaths, positive toxicology and non-cardiac pathology were excluded to determine sudden cardiac death (SCD). Cardiac pathological findings were analyzed by autopsy. SCD rate was estimated based on census and government vital statistics for the years studied.
Results
During a two year period, 223 patients (mean age 55 + 10 yrs, 78.9% male, body mass index 26 + 4, 60% smokers, 39% known CAD, 46% hypertension, 43% diabetes) presented to hospital with USD. SCD was attributed to myocardial infarction (MI) in 87% of cases; 69% were acute (96% anterior MI); 76% were small/moderate infarct and 9.9% of the cohort had normal hearts. Based on official municipal vital statistics, the SCD rate in those >35 yrs of age was estimated as 39.7/100,000 with male/female ratio of 4.6.
Conclusions
SCD in this south Indian city occurred predominantly in men of relatively young age and was most frequently associated with small or moderate-sized acute MI. Improved health care access, preventive measures and enhanced emergency management may reduce SCD from acute MI in this locale.
Keywords: Sudden cardiac death, South India, Autopsy, Risk factors
1. Introduction
In developing countries such as India, cardiovascular disease is a major cause of mortality [1]. It is estimated that 60% of the world's coronary artery disease (CAD) patients are South Asians [2] who have a high prevalence of CAD risk factors at a relatively young age [3]. Acute myocardial infarction (AMI) is frequent and the associated mortality is high in this group. In addition, preventive measures, and myocardial revascularization are both low and heart failure is common in India [4], [5].
In Western societies, CAD is the major cause of sudden cardiac death (SCD) [6]. By contrast, there is a paucity of data regarding the incidence and causes of SCD in South Asian societies [7]. This deficiency is related to multiple factors such as absence of systematic record acquisition, non-uniform billing codes, variations in payment strategies, lack of reporting and social aversion to autopsy. Knowledge of the rate and underlying pathology of sudden death could promote strategies for prevention and therapy of this tragedy.
We sought to assess the incidence and causes of out of hospital SCD as determined by postmortem findings among patients presenting with unexplained sudden death (USD) to a suburban tertiary care center in south India.
2. Methods
After obtaining approval from the institutional ethics committee, the records of patients presenting with unexplained sudden death (USD) from January 1, 2010 to December 31, 2011 undergoing autopsy were reviewed for demographics, medical history and pathological findings. Patients were considered to have USD if they died at home or were found dead out of hospital without a known cause, and were brought to the autopsy suite for evaluation of cause of death. Patients with trauma, violent deaths and positive toxicology were excluded from the study. Resuscitation history was not available for these patients, but none were alive at presentation to the emergency department (ED), however there are no standardized emergency response systems available in the geographic area of this study. All study patients were known to have died within 24 h of presentation to the ED.
2.1. Autopsy
Autopsy methodology followed previously described procedures [8]. Gross anatomy of the heart, the great arteries and the cardiac valves were assessed in detail. The coronary arteries were examined for size, shape, position, number, and ostial patency, as well as course and dominance. Multiple transverse cuts at three mm intervals were made along the course of the epicardial arteries and their major branches to assess patency. If calcified coronary arteries could not to be opened, they were removed intact, decalcified and opened.
Stenosis of the coronary arteries was graded I-IV based on cross sectional area of the lumen [9].
Grade I - Artery appeared grossly normal but had microscopic findings of atherosclerosis such as inflammatory infiltrates and lipid deposits.
Grade II - Thickening of vessel wall with 25–50% narrowing of lumen.
Grade III- Thickening of vessel wall with >50–75% narrowing of lumen.
Grade IV - Thickening and calcification with >75% narrowing of lumen.
The intact heart weight was assessed and compared with the nomogram for age and gender. Left ventricular (LV) wall thickness was measured at the base of the papillary muscles and compared with normal values for age and gender [8]. LV free wall slices (anterior, lateral and posterior), ventricular septum, free wall of the right ventricle and right ventricular outflow tract, and a block from each atrium as well as any area with macroscopic abnormalities, were examined with hematoxylin and eosin stain and a connective tissue stain (van Gieson, trichrome).
Hypertrophy was diagnosed if the thickness of either ventricular wall exceeded the average for age and gender. Hypertrophic cardiomyopathy (HCM) was considered present if the ratio of interventricular septum to posterior wall was greater than 1.3 [10]. Myocardial infarction (MI) was considered acute or chronic based on the types of inflammatory cells and stage of necrosis of the infarcted LV segment. The presence of polymorphonuclear cells and soft necrosis was evidence of acute infarction and the presence of fibrosis, histiocytes and collagenization was indicative of chronic infarction. Infarct size was calculated using a derivation of the area by geometry and volume and multiplying by greatest depth after histological confirmation of the infarction. This factor was divided by total weight of the respective ventricular slices, yielding percent of ventricular involvement: small (<8%), moderate (8–14%), large (>14–22%) and very large (≥23%) [11]. Coronary thrombus was defined as the presence of clot with collections of platelets, fibrin, and trapped erythrocytes and leukocytes; atherosclerotic plaque was defined by presence of lipid core and disruption of the luminal fibrous cap with fissure or rupture into the lipid core [12]. Presence of inflammatory infiltrates in the coronary arterial wall was defined as coronary arteritis [13].
Patients with non-cardiac pathology were considered to have non-cardiac causes of USD. Cardiac abnormalities when present were considered to be the cause of SCD; conversely, absence of cardiac or non-cardiac pathological findings indicated non-structural cause of SCD.
2.2. Statistics
Results are expressed as mean (±standard deviation) or percentages. Chi square test and Student's t-test were used to compare proportions and means, respectively, using STATA 10. Differences were considered significant if p < 0.05.
2.3. Estimation of SCD incidence
Tirunelveli Medical College hospital is a tertiary care center which exclusively serves as an autopsy site for the City of Tirunelveli and its surrounding areas. All deaths in the district referred by physicians or by law enforcement requiring identification of cause of death to undergo autopsy at this institution were included in the study per criteria elaborated in methods section. Based on the number of SCDs, as determined by our pathological findings, an estimate of the SCD incidence was made from the death rate reported in the vital statistics for the district population during the period of this study.
3. Results
During the two year interval of this study, 223 patients underwent autopsy for USD, 80% of whom were male (Table 1). Mean age of the entire study cohort was 55 + 10 yrs, and BMI was 26 + 4. Patients' backgrounds included smoking in more than half; one third had a history of alcohol consumption; and more than a third had a history of CAD. Hypertension and diabetes were present in less than half of the total study group.
Table 1.
Baseline characteristics (n = 223).
| Age, mean (SD),yrs | 55 (10) |
| Gender, No.(%) (male) | 176 (78.9) |
| BMI, mean (SD) | 27 (4) |
| Known CAD, No. (%) | 87 (39) |
| Hypertension, No. (%) | 103 (46) |
| Diabetes mellitus, No.(%) | 95 (43) |
| Smoker, No. (%) | 133 (60) |
3.1. Autopsy findings
In forty two patients (19%), USD was attributable to non-cardiac causes such as infection, cerebrovascular accident and pulmonary embolism. The remainder of those who presented with USD were deemed to have died of cardiac causes, of which structural heart disease was present in a large majority (Table 2).
Table 2.
Causes of unexplained sudden death.
| Non cardiac causes, No. (%) | 42 (18.8) |
| Sudden cardiac death,No. (%) | 181 (81.2) |
| Identifiable cardiac causes, No. (%) | 163 (73.1) |
| No Identifiable cardiac causes, No. (%) | 18 (6.5) |
Coronary artery atherosclerosis was present in 163 (73%) patients, coronary thrombosis in 73 (33%), coronary arteritis in nine (4%), and ruptured coronary artery plaque in eight (2.7%). Coronary stenosis was present in 72% of the SCD cohort. In 17% of individuals, the stenoses were concentric and 55% had eccentric stenosis (grade 1: 26% of total cohort, grade 2: 11%, grade 3: 17%, and grade 4: 18%). Coronary plaque ulceration in the absence of thrombus was present in eight patients (3.5%). Mean mass of LV and right ventricle was 163 + 33 and 59 + 13 g, respectively. Twenty one percent of the individuals had LVH.
Of the cardiac causes, the most common LV pathology was MI in 87% of the SCD group. In addition, small numbers of other entities were HCM, dilated cardiomyopathy and mitral valve disease. Approximately 10% of patients with SCD had no demonstrable cardiac or non-cardiac pathology (Table 3). Two-thirds of the MIs were judged to be acute (96% anterior MI) and infarct size was small or moderate in 74% (Fig. 1). Compared to patients without MI, those with infarcts had a higher frequency of diabetes (52.5% vs 32.2%, p = 0.01), were older (56 + 9 vs 52 + 10 yrs, p = 0.01) and had more frequent CAD (51.2% vs 13.6%, p < 0.001) (Table 4). There was no difference in infarct size between anterior and inferior wall MI or in acute vs. chronic infarcts.
Table 3.
Cardiac causes of unexplained sudden death (n = 181).
| No identifiable cause, No. (%) | 18 (9.9) |
| MI,a No. (%) | 158 (87) |
| Acute MI/chronic, No. (%) | 109 (60)/49 (27) |
| Anterior MI/Non anterior MI,No. (%) | 152 (96)/6 (4) |
| HCM,b No. (%) | 3 (1.7) |
| Non ischemic cardiomyopathy,No. (%) | 1 (0.6) |
| Mitral valve disease,No.(%) | 1 (0.6) |
MI –myocardial infarction.
HCM-Hypertrophic cardiomyopathy.
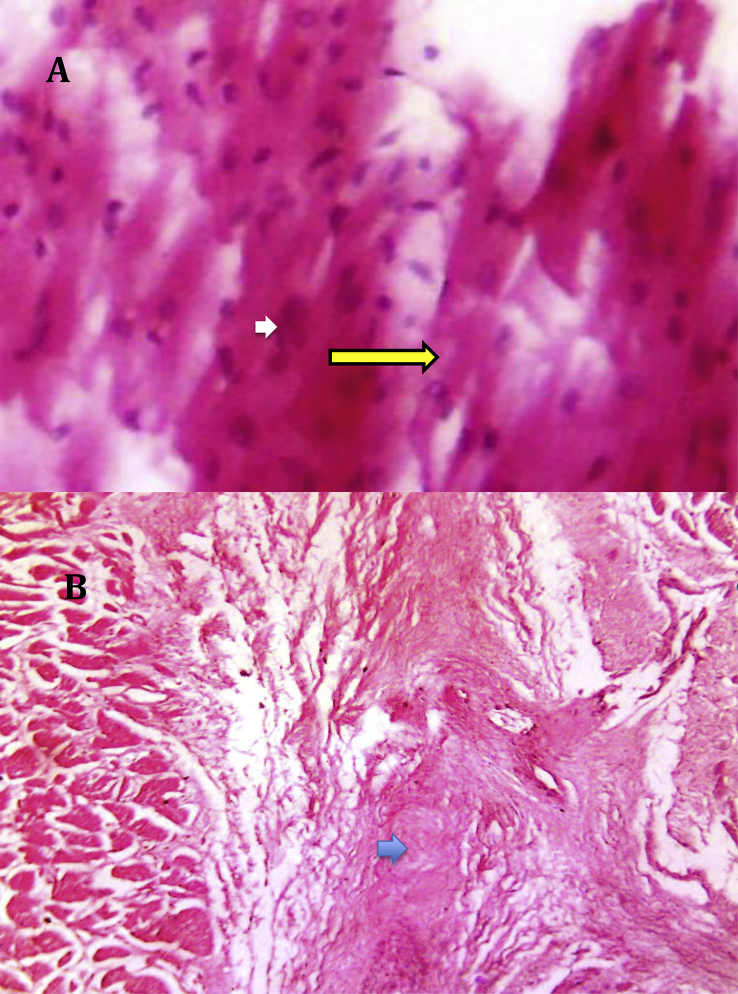
Fig. 1.
Pathology of myocardial infarction-acute and chronic. A: Acute myocardial infarction – necrotic myocardium with hyper eosinophilic staining of cytoplasm (yellow arrow), polymorphonuclear cells (white arrow). B: Chronic myocardial infarction with replacement fibrosis of myocardium (blue arrow).
Table 4.
Comparison of patients who had myocardial infarct vs no infarct.
| Variable | No Infarct (44) | Infarct (158) | p Value |
|---|---|---|---|
| Age, mean (SD), yrs | 52 (10) | 56 (9) | 0.01 |
| Body mass Index, mean (SD) | 26 (3) | 26 (4) | ns |
| Gender (male), No. (%) | 31 (70.4) | 128 (81) | ns |
| Smoker, No.(%) | 25 (58.1) | 114 (72) | ns |
| Hypertension, No.(%) | 21 (48.3) | 80 (50.6) | ns |
| Diabetes mellitus, No.(%) | 14 (32.2) | 83 (52.5) | 0.04 |
| Known Coronary artery disease, No.(%) | 6 (13.6) | 81 (51.2) | <0.0001 |
| Coronary atherosclerosis, No.(%) | 14 (32.2) | 152 (96.2) | <0.0001 |
3.2. Estimated incidence of SCD
The population of Tirunelveli in 2011 is 474,838 with approximately 35% estimated to be ≥ 35 yrs based on Indian national census (2011). All but three patients in this study were ≥35 years old. Based on these data, by mathematical calculation, it is estimated that SCD occurred in 39.7/100,000 of the population ≥35 years of age during the study interval. This estimate was calculated based on the total death rate in adults ≥ age 35 years in the district for the interval studied, assuming that all patients who had unexplained SCD underwent autopsy. SCD was 4.6 times more frequent in males than females with an estimated incidence of 65.8/100,000 compared to 14.3/100,000 among females.
4. Discussion
South Asians constitute 60% of the world's CAD population, suggesting that this disease is a major cause of SCD in this group.(1) However the prevalence and pathological causes of SCD among South Asian populations is unknown, except for a “verbal autopsy” study in which 17% of deaths were attributed to SCD and the majority of them to CAD [7]. Our study is the largest investigation of which we are aware that includes autopsy data to assess the etiology of SCD in a South Asian population.
SCD is defined as nonviolent, unexpected, natural death occurring within 1 h of symptom onset, but this definition is difficult to apply in retrospective analyses of autopsy and public health data. (9) In their epidemiologic analysis of SCD in the US, Gillum et al. have defined SCD as death occurring out of hospital or upon arrival to or in the emergency department [14]. While this definition is more applicable to arrhythmias related to CAD, it is often unsatisfactory when deaths are unwitnessed or when patients die in their sleep. Therefore, the World Health Organization defines SCD as occurring within 24 h of symptom onset [15], [16], [17]. In our retrospective study, it is difficult to verify the duration of symptoms but death occurring within 24 h of symptom onset may be inferred based on local cultural practices of cremation/burial within 24 h of demise and the reported arrival time after death at the autopsy suite.
The definition of SCD strongly influences identifiable causes of this condition. Based on data compiled in the US, when SCD is defined as occurring less than 1–2 h after symptom onset, the frequency of MI is approximately 90% compared to 75% when defined as occurring within 24 h of clinical presentation [18], [19].In our study 71% of SCD was associated with MI, which is consistent with the foregoing reports.
It has been shown in autopsy studies in the US that SCD in the population <35 years of age has multiple causes including HCM myocarditis and coronary anomaly [20] whereas in those >age 35, CAD is predominant. The majority of our patients were >35 years of age (mean 55 + 10 yrs) and 80% were male. By contrast in the US, the median age of SCD is 69 yrs [21] and about two-thirds were male in the SCD report of Chugh et al. in Oregon, USA [22]. Based on data from the Framingham study, men were at 3.8 times the risk of SCD compared to females [23], [24]; In our study, male predominance is likely related to both a higher cardiac risk profile in men [5] and possible low autopsy rates in the female population.
Of the MI group in our cohort, the majority was acute and infarct size was small to moderate, suggesting arrhythmic death. Myocardial infarction involved the anterior wall in a majority (96%) of our acute MI group, consistent with the study of Farb et al [12]. Coronary thrombus was present in a third of our patients and plaque erosion in the absence of thrombus occurred in approximately 4%, which is disproportionately small relative to the number of acute MIs noted. In pathologic studies of SCD, about 70–80% of acute MIs are associated with acute thrombosis and in approximately a third of cases plaque erosion is noted [6], [25]. Our findings suggest an arrhythmic event or coronary artery spasm, neither of which can be determined by autopsy. It is also possible that SCD occurred after spontaneous lysis of thrombus. In a small autopsy study of Pakistani male military recruits presenting with SCD, the majority had evidence of coronary atherosclerosis. However, only approximately 55% had evidence of acute or old MI [26]. In this report HCM was found in 17% of the SCD group, thereby indicating a different study population than ours.
Our study is consistent with the well established relationship of SCD to cardiac risk factors and extensive CAD [3]. Of the three young patients in our study (<35 yrs), one had acute anterior MI and a very high coronary risk profile including diabetes mellitus, hypertension and smoking. Tobacco use, which was highly prevalent in our patients, is associated with multiple metabolic factors that promote coronary plaque rupture, thrombosis, vasospasm and arrhythmias, and may explain the young age in our study group compared to those from the US [6]. A small proportion of patients had non-coronary structural heart disease and in 10% of the group, SCD remained unexplained, suggesting a primary arrhythmic etiology unrelated to CAD.
Based on our findings and local population vital statistics, it is estimated that SCD occurred in 39.7 deaths/100,000 of the adult population (≥35 yrs) of Tirunelveli. The frequency of SCD in males was 4–5 times greater than in females. This incidence of SCD in the population >35 years is lower than has been reported in the US (60 deaths/100,000 population), although our subjects were younger [27].
Our study was based on autopsies performed on patients who were referred by the ED physician with family consent or by law for determination of cause of death for the purposes of death certificate; the latter group were those found in the field. Not all deaths at home or in the field resulted in autopsy which therefore significantly underestimates the incidence of SCD. However we were unable to estimate the autopsy rate for such reported deaths for which subjects did not undergo autopsy, therefore our reported incidence could be an underestimation of the real problem.
The toll of SCD is grim even in developed societies with well established preventive, therapeutic and advanced emergency medical services [28]. On the contrary, these advantages are limited in developing countries in South Asia, contributing to poor survival in patients with out of hospital cardiac arrest [5]. Our results indicate a crucial need for enhanced primary and secondary prevention programs with an essential focus on screening for risk factors, particularly smoking cessation and other improvements in life style including low carbohydrate diet. The local diet frequently comprises high carbohydrates, refined sugar and high fat content, contributing to the high prevalence of metabolic syndrome and diabetes in India [29], [30].
Study Limitations: This is a retrospective analysis that entails the limitations inherent in this method. However, this is the first investigation of SCD in a metropolitan population of South Asia. In addition, the autopsy data do not include the number of diseased coronary arteries, but detailed segmental coronary and myocardial pathology were important elements of our analysis. Although this is the largest study of SCD from South Asia, the total cohort is modest in number and we may have underestimated the actual frequency of SCD because of social mores which preclude autopsy.
5. Conclusions
Our findings highlight an increased risk of SCD in acute MI among relatively young men in their productive years in South India compared to developed societies. These results emphasize a need for enhanced preventive, interventional and acute cardiovascular care.
Disclosures
None.
Footnotes
Peer review under responsibility of Indian Heart Rhythm Society.
References
- 1.Yusuf A.A., Weinhandl E.D., St Peter W.L. Comparative effectiveness of calcium acetate and sevelamer on clinical outcomes in elderly hemodialysis patients enrolled in Medicare part D. Am J Kidney Dis. 2014;64:95–103. doi: 10.1053/j.ajkd.2013.11.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Gaziano T.A. Cardiovascular disease in the developing world and its cost-effective management. Circulation. 2005;112:3547–3553. doi: 10.1161/CIRCULATIONAHA.105.591792. [DOI] [PubMed] [Google Scholar]
- 3.McGorrian C., Yusuf S., Islam S., Jung H., Rangarajan S., Avezum A. Estimating modifiable coronary heart disease risk in multiple regions of the world: the INTERHEART Modifiable Risk Score. Eur heart J. 2011;32:581–589. doi: 10.1093/eurheartj/ehq448. [DOI] [PubMed] [Google Scholar]
- 4.Teoh M., Lalondrelle S., Roughton M., Grocott-Mason R., Dubrey S.W. Acute coronary syndromes and their presentation in Asian and Caucasian patients in Britain. Heart. 2007;93:183–188. doi: 10.1136/hrt.2006.091900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xavier D., Pais P., Devereaux P.J., Xie C., Prabhakaran D., Reddy K.S., Investigators Cr Treatment and outcomes of acute coronary syndromes in India (CREATE): a prospective analysis of registry data. Lancet. 2008;371:1435–1442. doi: 10.1016/S0140-6736(08)60623-6. [DOI] [PubMed] [Google Scholar]
- 6.Virmani R., Burke A.P., Farb A. Sudden cardiac death. Cardiovasc Pathol. 2001;10:275–282. doi: 10.1016/s1054-8807(01)00108-9. [DOI] [PubMed] [Google Scholar]
- 7.Madhavan S.R., Reddy S., Panuganti P.K., Joshi R., Mallidi J., Raju K. Epidemiology of sudden cardiac death in rural South India - insights from the Andhra Pradesh rural health initiative. Indian Pacing Electrophysiol J. 2011;11:93–102. [PMC free article] [PubMed] [Google Scholar]
- 8.Basso C., Burke M., Fornes P., Gallagher P.J., de Gouveia R.H., Sheppard M., Association for European Cardiovascular P Guidelines for autopsy investigation of sudden cardiac death. Virchows Arch. 2008;452:11–18. doi: 10.1007/s00428-007-0505-5. [DOI] [PubMed] [Google Scholar]
- 9.Chopra P., Sethi U., Gupta P.K., Tandon H.D. Coronary arterial stenosis. An autopsy study. Acta Cardiol. 1983;38:183–197. [PubMed] [Google Scholar]
- 10.Romhilt D.W., Greenfield J.C., Jr., Estes E.H., Jr. Vectorcardiographic diagnosis of left ventricular hypertrophy. Circulation. 1968;37:15–19. doi: 10.1161/01.cir.37.1.15. [DOI] [PubMed] [Google Scholar]
- 11.Hackel D.B., Ratliff N.B., Jr. A technic to estimate the quantity of infarcted myocardium post mortem. Am J Clin Pathol. 1974;61:242–246. doi: 10.1093/ajcp/61.2.242. [DOI] [PubMed] [Google Scholar]
- 12.Farb A., Tang A.L., Burke A.P., Sessums L., Liang Y., Virmani R. Sudden coronary death. Frequency of active coronary lesions, inactive coronary lesions, and myocardial infarction. Circulation. 1995;92:1701–1709. doi: 10.1161/01.cir.92.7.1701. [DOI] [PubMed] [Google Scholar]
- 13.Vaideeswar P., Verma R., Gupta R. Infective coronary arteritis: a pathological analysis at autopsy. Hum Pathol. 2012;43:2334–2341. doi: 10.1016/j.humpath.2012.04.005. [DOI] [PubMed] [Google Scholar]
- 14.Gillum R.F. Sudden coronary death in the United States: 1980-1985. Circulation. 1989;79:756–765. doi: 10.1161/01.cir.79.4.756. [DOI] [PubMed] [Google Scholar]
- 15.Furberg C.D. Overview of completed sudden death trials: US experience. Cardiology. 1987;74(Suppl. 2):24–31. doi: 10.1159/000174284. [DOI] [PubMed] [Google Scholar]
- 16.Oliva A., Brugada R., D'Aloja E., Boschi I., Partemi S., Brugada J. State of the art in forensic investigation of sudden cardiac death. Am J Forensic Med Pathol. 2011;32:1–16. doi: 10.1097/PAF.0b013e3181c2dc96. [DOI] [PubMed] [Google Scholar]
- 17.Virmani R., Burke A.P., Farb A. Sudden cardiac death. Cardiovasc Pathol. 2001;10:211–218. doi: 10.1016/s1054-8807(01)00091-6. [DOI] [PubMed] [Google Scholar]
- 18.Kuller L.H., Traven N.D., Rutan G.H., Perper J.A., Ives D.G. Marked decline of coronary heart disease mortality in 35-44-year-old white men in Allegheny County, Pennsylvania. Circulation. 1989;80:261–266. doi: 10.1161/01.cir.80.2.261. [DOI] [PubMed] [Google Scholar]
- 19.Kuller L.H., Perper J.A., Dai W.S., Rutan G., Traven N. Sudden death and the decline in coronary heart disease mortality. J chronic Dis. 1986;39:1001–1019. doi: 10.1016/0021-9681(86)90136-0. [DOI] [PubMed] [Google Scholar]
- 20.Puranik R., Chow C.K., Duflou J.A., Kilborn M.J., McGuire M.A. Sudden death in the young. Heart Rhythm. 2005;2:1277–1282. doi: 10.1016/j.hrthm.2005.09.008. [DOI] [PubMed] [Google Scholar]
- 21.Chugh S.S., Jui J., Gunson K., Stecker E.C., John B.T., Thompson B. Current burden of sudden cardiac death: multiple source surveillance versus retrospective death certificate-based review in a large U.S. community. J Am Coll Cardiol. 2004;44:1268–1275. doi: 10.1016/j.jacc.2004.06.029. [DOI] [PubMed] [Google Scholar]
- 22.Chugh S.S., Uy-Evanado A., Teodorescu C., Reinier K., Mariani R., Gunson K. Women have a lower prevalence of structural heart disease as a precursor to sudden cardiac arrest: the Ore-SUDS (Oregon Sudden Unexpected Death Study) J Am Coll Cardiol. 2009;54:2006–2011. doi: 10.1016/j.jacc.2009.07.038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schatzkin A., Cupples L.A., Heeren T., Morelock S., Mucatel M., Kannel W.B. The epidemiology of sudden unexpected death: risk factors for men and women in the Framingham Heart Study. Am heart J. 1984;107:1300–1306. doi: 10.1016/0002-8703(84)90302-8. [DOI] [PubMed] [Google Scholar]
- 24.Adabag A.S., Luepker R.V., Roger V.L., Gersh B.J. Sudden cardiac death: epidemiology and risk factors. Nat Rev Cardiol. 2010;7:216–225. doi: 10.1038/nrcardio.2010.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Davies M.J., Bland J.M., Hangartner J.R., Angelini A., Thomas A.C. Factors influencing the presence or absence of acute coronary artery thrombi in sudden ischaemic death. Eur heart J. 1989;10:203–208. doi: 10.1093/oxfordjournals.eurheartj.a059467. [DOI] [PubMed] [Google Scholar]
- 26.Ahmad M., Afzal S., Malik I.A., Mushtaq S., Mubarik A. An autopsy study of sudden cardiac death. JPMA J Pak Med Assoc. 2005;55:149–152. [PubMed] [Google Scholar]
- 27.Stecker E.C., Reinier K., Marijon E., Narayanan K., Teodorescu C., Uy-Evanado A. Public health burden of sudden cardiac death in the United States. Circ Arrhythm Electrophysiol. 2014;7:212–217. doi: 10.1161/CIRCEP.113.001034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Holzer M., Sterz F., Hypothermia After Cardiac Arrest Study G Therapeutic hypothermia after cardiopulmonary resuscitation. Expert Rev Cardiovasc Ther. 2003;1:317–325. doi: 10.1586/14779072.1.2.317. [DOI] [PubMed] [Google Scholar]
- 29.Mohan V., Radhika G., Sathya R.M., Tamil S.R., Ganesan A., Sudha V. Dietary carbohydrates, glycaemic load, food groups and newly detected type 2 diabetes among urban Asian Indian population in Chennai, India (Chennai Urban Rural Epidemiology Study 59) Br J Nutr. 2009;102:1498–1506. doi: 10.1017/S0007114509990468. [DOI] [PubMed] [Google Scholar]
- 30.Gulati S., Misra A. Sugar intake, obesity, and diabetes in India. Nutrients. 2014;6:5955–5974. doi: 10.3390/nu6125955. [DOI] [PMC free article] [PubMed] [Google Scholar]