Abstract
Background
We estimated the prevalence of irritable bowel syndrome (IBS) and its impact on patient-reported health-related quality of life (HR-QOL) in a university-based population aged between 18 and 30 years in Bogotá, Colombia.
Methods
The study had a cross-sectional design. Students, faculty, and staff aged 18-30 years of the Pontificia Universidad Javeriana, Bogotá, Colombia were randomly selected and invited to complete an electronic survey containing the Rome III IBS diagnostic questionnaire and an IBS-specific HR-QOL instrument (IBS-QOL).
Results
A total of 1082 individuals participated in this study. The prevalence of IBS was 24.0% (95% CI 21.3-26.6%). IBS-constipation was the most common subtype (41.9%; 95% CI 35.5-48.4%). The overall IBS-QOL score indicated HR-QOL impairment (72.1/100). IBS-unsubtyped patients had the highest overall HR-QOL (constipation: 70.6; diarrhea: 67.2; mixed: 67.0; unsubtyped: 77.8; P=0.003). IBS non-consulters had higher IBS-QOL “Food Avoidance” scores than IBS consulters (60.3 vs. 45.5; P=0.002).
Conclusion
IBS is a prevalent disorder in a university-based population aged 18-30 years and has a significant impact on HR-QOL. IBS-unsubtyped subjects had the highest HR-QOL compared to other subtypes. Food avoidance appears to be a key factor in seeking consultation.
Keywords: Irritable bowel syndrome, prevalence, health-related quality of life, Colombia
Introduction
Irritable bowel syndrome (IBS) is found everywhere; its prevalence depends on diagnostic criteria and on the population. Different countries and races have reported a wide range of frequencies [1,2]. Prevalence estimates in the western hemisphere range from 3-25%, with a 3:1 female predominance [3]. IBS is traditionally considered a disorder of young and mature adulthood [4,5], but there is evidence that its prevalence increases in the elderly [6]. Underdiagnosis of IBS in the elderly may be due to its symptoms being attributed to organic disease [7]. The incidence increases during adolescence and reaches its peak during the third and fourth decades of life [8]. Diagnosis is durable once IBS is established with clinical criteria [9].
IBS has a great impact on resource utilization and health-related quality of life (HR-QOL) [10]. The use of health services by IBS patients is high (up to 50%) in countries of the western hemisphere [10]. Moreover, the chronic and benign character of IBS makes HR-QOL an important outcome for both patients and physicians. The impact of IBS on HR-QOL is significant [11,12], even more than for other chronic diseases [13].
Young adults who study or work in universities are exposed to factors that could affect HR-QOL in the IBS population. Academic performance, pressure to succeed, and financial issues are major concerns associated with anxiety, stress and depression [14]. Academic stress has been linked to disordered eating [15] and inadequate eating habits, such as fast food consumption and skipping breakfast, which have been described in Latin American college students [16]. Furthermore, in our experience, a subgroup of these patients do not seek medical advice because they do not regard the symptoms as a manifestation of disease (a “family condition”) and do not consider them important, even though their IBS symptoms may already be affecting their HR-QOL without their being aware of it. Therefore, our aims were to estimate the prevalence of IBS and to assess its impact on HR-QOL in a population of students, faculty, and staff, aged 18-30 years, of a private university in Colombia.
Patients and methods
Study subjects
Eligible subjects were students, faculty, and staff of a private university (Pontificia Universidad Javeriana, Bogotá, Colombia), aged between 18 and 30 years between September and October of 2012. Women who reported pregnancy were excluded from the study.
The sampling frame contained 26,038 students and workers, of whom 18,828 (72.3%) met the age criteria. A stratified random sampling procedure with proportional allocation according to the participant’s role (student, faculty, or staff) and sex was used to divide the sample into six strata (male students: 41.1%; female students: 54.4%; male faculty: 1.0%; female faculty: 0.9%; male staff; 1.1%; female staff: 1.4%). Random samples were taken without replacement from the six strata using Microsoft Excel.
Study design
The study had a cross-sectional design. The IBS diagnosis was based on the Rome III criteria. Subsequently, the HR-QOL dimensions of IBS patients were evaluated using the Irritable Bowel Syndrome – Quality of Life questionnaire (IBS-QOL).
The face validity of Spanish adaptations of the Rome III Adult Questionnaire (RIIIAQ) [17,18] and the IBS-QOL instrument [19] were tested with the help of a group of fellow physicians who assessed question comprehension and their ease of use in an electronic survey. The Rome Foundation and MAPI institute granted the licenses for RIIIAQ and IBS-QOL, respectively.
Questionnaires
The diagnosis of IBS and the classification of IBS subtypes were established using the 10 related questions of the RIIIAQ [20], a self-administered questionnaire that is used in both clinical practice and research. IBS patient subtypes were classified as diarrhea (IBS-D), constipation (IBS-C), mixed (IBS-M) and unsubtyped (IBS-U).
IBS-QOL consists of 34 5-option Likert-type response items (ranging from “Not at all” to “A great deal” or “Extremely”) that describe the state of the respondent over the last 30 days. Domain and overall scores are obtained by the summation of item scores. Addressed domains are “Dysphoria”, “Interference with Activities”, “Body Image”, “Health Worry”, “Food Avoidance”, “Social Reaction”, “Sexual Function” and “Relationships”. The severity of symptoms is transformed to a scale that ranges from 0-100. Higher scores indicate better HR-QOL [21]. Chosen cutoff values were 80 points or more, indicating no association between the domain and intestinal problems, and less than 65 points, corresponding to moderate to severe IBS [22]. A difference of 14 points was considered clinically significant [23]. IBS-QOL is based on the HR-QOL concept developed by Patrick and Erickson [24].
IBS-QOL is a validated instrument that has shown high internal consistency (Cronbach’s alpha = 0.95), reproducibility over an average time of 7 days (CCI = 0.86), good discriminative ability [25,26] and sensitivity to change [23]. The scale has been translated into Spanish according to MAPI Research Institute protocols. The Spanish version of IBS-QOL had adequate construct validity in a population of Mexican women [19].
Data collection
Data from randomly selected respondents were captured with an electronic survey. Contact was made using the e-mail addresses provided by the University. Official announcements and surveys were sent through this service. Mails contained the aims of the study, a short description, and a link to access the electronic survey. Within a period of 20 days, non-respondents received a new invitation. This process was carried out on 2 occasions (three waves in total). The information was automatically archived to an exportable database that preserved the order of the variables in the original form.
The survey had mandatory fields and specific limits to avoid missing data and prevent the entry of extreme values. A weekly backup of the data was stored in a private virtual cloud account to maintain information security. The survey automatically created two unrelated independent databases aimed to preserve patient anonymity.
Data capture
The survey was built into Limesurvey Version 1.92, Build 120919 and hosted on the university’s servers. Questions appeared on the screen one at a time in the order of the original questionnaires. Thus, the respondent did not have to answer irrelevant questions and was not subject to visual saturation. Each question was mandatory and respondents were not allowed to jump to another item; however, the survey allowed them to go back to correct an answer. It also allowed respondents to save the answers and complete the questions at a later time to avoid abandonment. A 14-pt sans-serif font was selected for ease of reading. Each screen had help available, including the meanings of words that seemed difficult to comprehend.
The survey had 54 questions, distributed into seven sections:
Introduction: Consent form approved by the Research Ethics Committee; the purpose of the study was explained and prompted the respondent to continue or abandon the survey.
Demographics: Age, sex, role, marital status, socioeconomic status (classified according to the housing and environmental conditions method of the Colombian Statistics Department [27]), and pregnancy (6 items).
Diagnosis: RIIIAQ (10 items).
Quality of life: IBS-QOL questionnaire (34 items).
Health Services and Tobacco: Previous consultation for IBS related symptoms (2 items) and smoking (2 items).
Calculation inquiries: IBS-RIIIAQ and HR-QOL scoring (visible to researchers only).
Results: presentation and explanation of individual results to the respondent with recommendations on general health.
Statistical analysis
To obtain a 5-point absolute accuracy in the overall IBS-QOL score, with a 5% alpha error and 18-point standard deviation [22,28], 141 positive individuals were needed. Prevalence reports in Colombia ranged from 12% [29] to 20% [30]. We chose 12% prevalence, as it gave the most conservative sample size. Therefore 1175 respondents were needed. This sample size allowed a 3% absolute accuracy in IBS prevalence. Since the response rate from previous surveys in the university was 30%, to achieve 1175 respondents the sample size was increased to 3916.
The prevalence of IBS in the population was calculated as the weighted proportion of patients diagnosed with IBS using the Rome III criteria, according to the expansion factors for each stratum. Confidence intervals (95% CI) for the overall prevalence of IBS, IBS subtypes, marital status, socioeconomic status, and the proportion of IBS consulters were calculated. A design-based chi-square test was performed to explore associations between socioeconomic and marital status with IBS.
We measured the HR-QOL of IBS subjects with IBS-QOL, according to the User’s Manual rules [21]. Overall means of IBS consulters and non-consulters were calculated. Associations between HR-QOL and sex, role, socioeconomic status, IBS subtype, and consultation for symptoms related to IBS were explored. Normality was examined with the Shapiro–Wilk test. We explored associations between overall mean IBS-QOL scores and categories of marital status, role, IBS subtypes and consulter subgroups using design-based Mann–Whitney U and Kruskal–Wallis tests. P-values less than 0.05 were considered statistically significant. The internal consistency of the IBS-QOL scale was calculated post hoc with Cronbach’s alpha. We performed available-case analysis for missing data. Data analysis was performed using the R statistical software environment (version 3.1.1) [31].
The University’s Institutional Research Board approved the study (FM-CIE-5672-12). Individuals who completed the survey participated in a draw for three $25 gift cards.
Results
Invitations were sent in three waves (September 14, October 4 and 23, 2012) to 4000 students, faculty, and staff. One thousand and eighty-two subjects responded to the invitation (656 in the first wave, 243 in the second, and 183 in the third). Nineteen subjects were excluded from the study: 12 did not meet established age limits and seven reported pregnancy. Nine hundred and fifty-three (23.8%) answered all the questions in the survey.
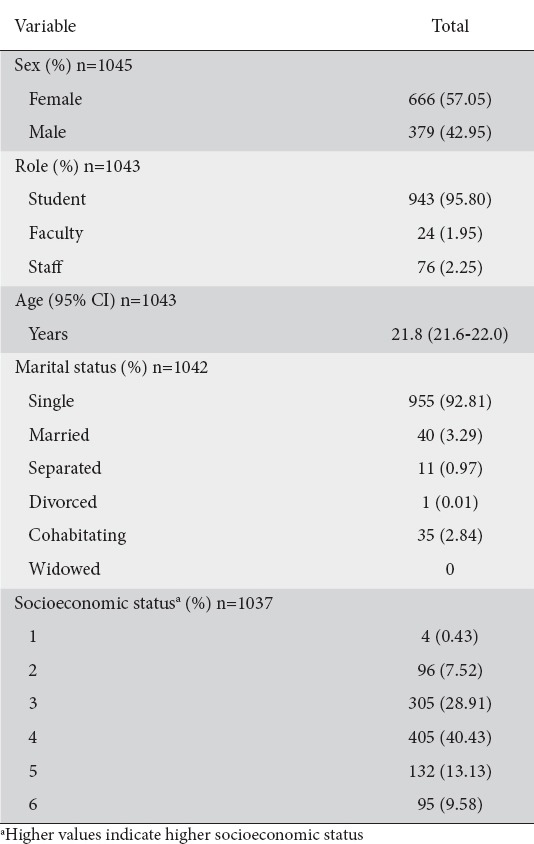
Table 1 shows the characteristics of the sample. In brief, the respondents had a mean age of 21.8 years (95% CI 21.6-22.0 years). The majority were single and of middle-income socioeconomic status. The estimated smoking prevalence was 25.0% (n=974, 95% CI 22.2-27.8). No statistically detected association was found between IBS status and smoking (χ2=0.39; df=1; P=0.558).
Table 1.
Weighted demographic characteristics of the sample
IBS
The estimated prevalence of IBS was 24.0% (95% CI 21.3-26.6%). The frequency of IBS was higher among respondents with low-income socioeconomic status (strata 1 and 2), those in stable relationships, and faculty (Table 2). The most common IBS subtypes were IBS-C and IBS-U (Table 3). Twenty-eight percent of respondents with an IBS diagnosis (n=233) had not consulted health services for symptoms related to this condition. No statistically detected significant association between IBS status and marital or socioeconomic status was found (Table 4).
Table 2.
Weighted prevalence of irritable bowel syndrome
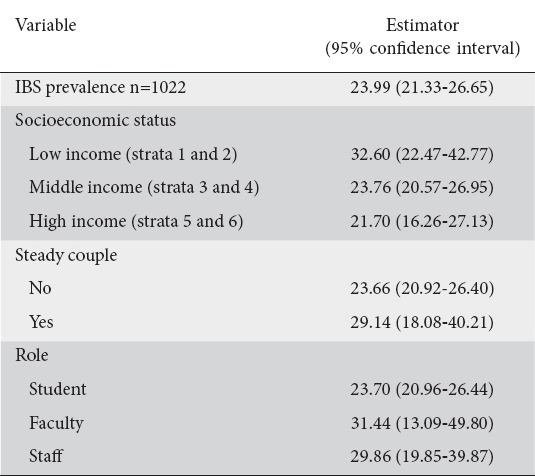
Table 3.
Weighted proportions of irritable bowel (IBS) subtypes (n=249)
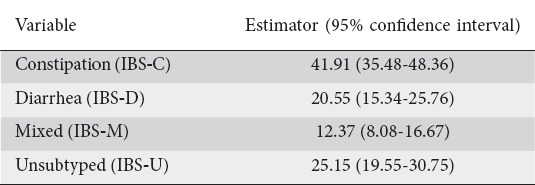
Table 4.
Weighted differences between IBS patients and controls with Rome III criteria (n=1022)
HR-QOL
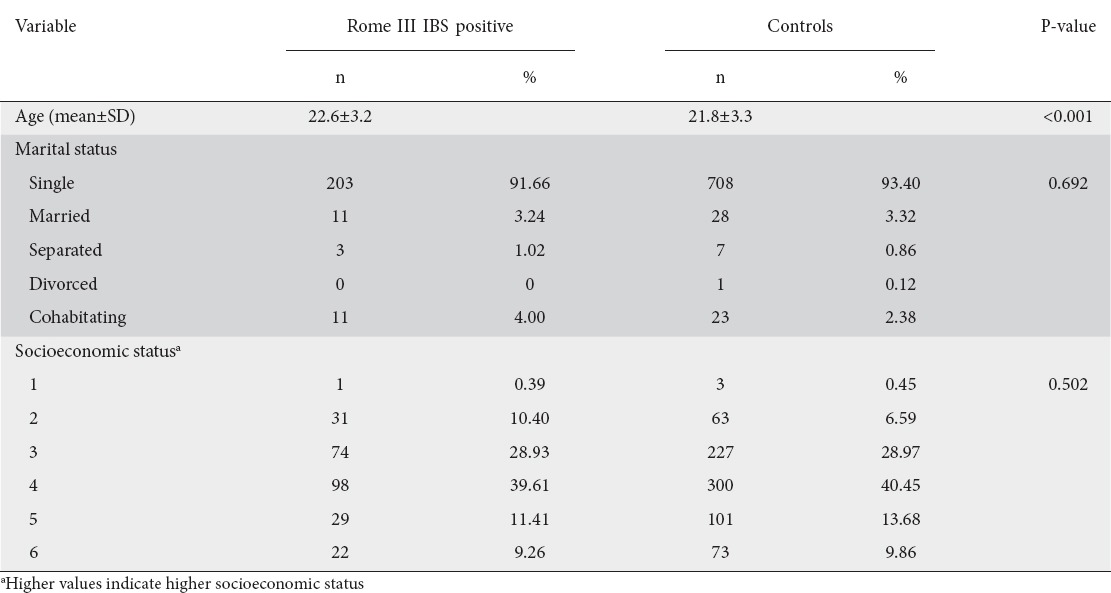
Patients diagnosed with IBS had a mean overall HR-QOL (IBS-QOL scale) of 71.2 (95% CI 68.6-73.7). “Health Worry” (54.5; 95% CI 51.0-58.0) and “Food Avoidance” (49.6; 95% CI 45.3-53.8) domains had moderate or severe HR-QOL impairment. “Dysphoria” and “Body Image” also had an average score below 80 (Fig. 1).
Figure 1.
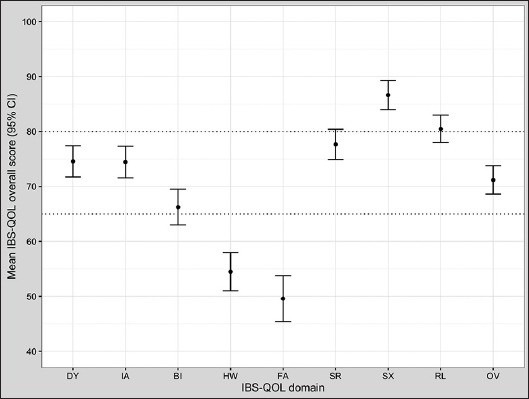
Mean irritable bowel syndrome quality of life (IBS-QOL) overall scores for patients with IBS
Higher scores in IBS-QOL indicate better health-related quality of life (HR-QOL). A score of 80 points or more suggests no association between overall mean HR-QOL and intestinal problems; scores less than 65 points correspond to moderate to severe IBS. Error bars show 95% confidence limits DY, dysphoria; IA, interference with activities; BI, body image; HW, health worry; FA, food avoidance; SR, social reaction; SX, sexual; RL, relationships; OV, overall
Table 5 shows IBS-QOL scores by demographic variables. Both sexes had overall mean scores below 80, with lower scores for females (t=-2.69; df=226; P=0.008). In specific domains, women only obtained a score above 80 in “Sexual Function”. A score below 65 was obtained for “Body Image”, “Health Worry”, and “Food Avoidance”, which indicate a moderate to severe compromise of HR-QOL. In men, “Health Worry” and “Food Avoidance” were the most affected domains.
Table 5.
Overall and specific domain weighted IBS-QOL scores by demographic variables and IBS subtype
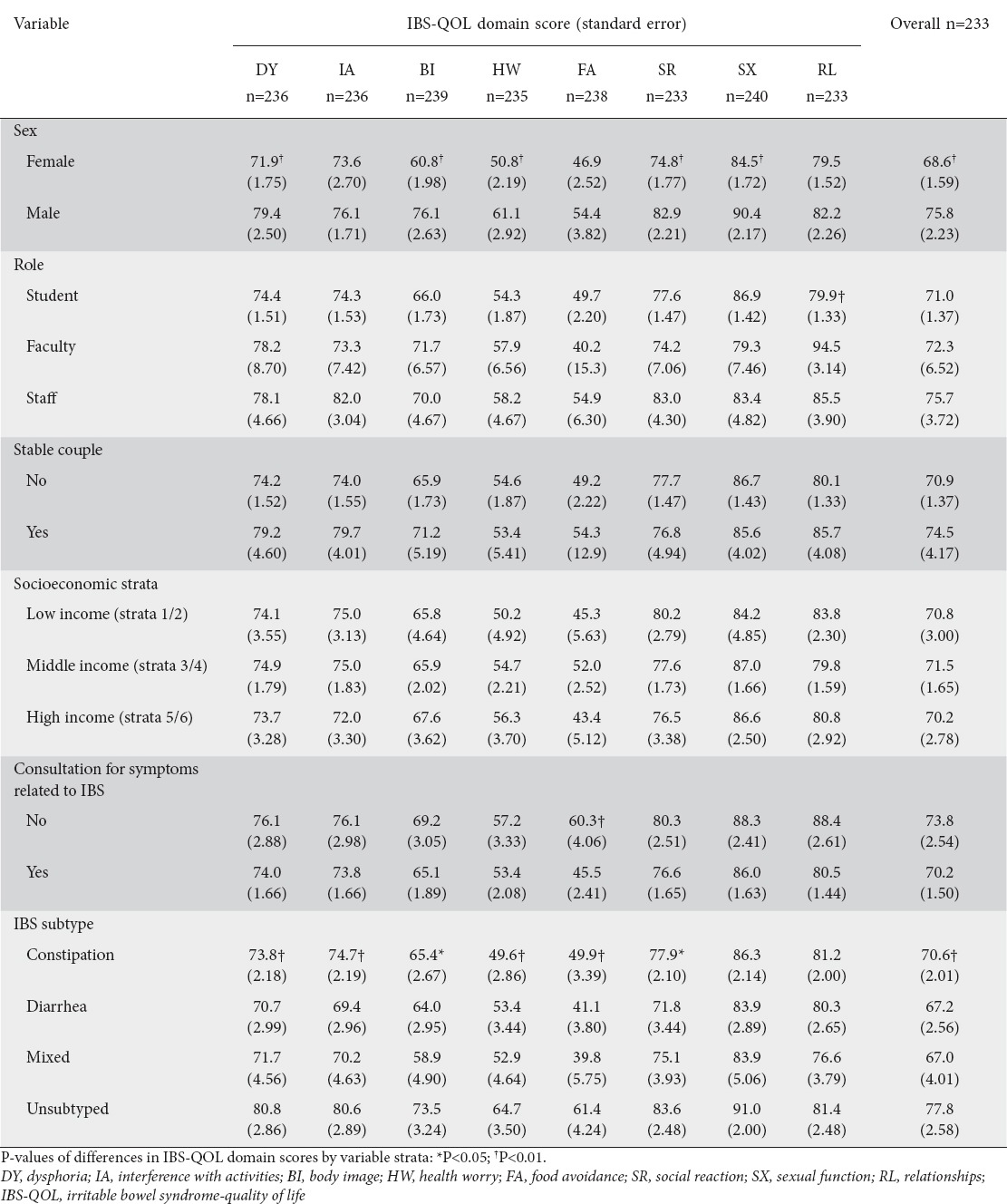
According to role and relationship status, overall mean scores ranged between 70.9 and 75.7 in all categories of these strata. No statistically detected differences in overall mean IBS-QOL between categories of role (χ2=1.45; df=2; P=0.484) or relationship status (t=0.85; df=226; P=0.395) were found. “Health Worry” and “Food Avoidance” domains had moderate to severe IBS (scores lower than 65 points) in every role category. Students scored close to the 65-point boundary in “Body Image”.
The categories of socioeconomic strata had similar overall mean IBS-QOL scores (χ2=1.24; df=2; P=0.536). IBS non-consulters had higher mean overall IBS-QOL scores compared to IBS consulters (t=-1.24; df=226; P=0.217). In general, IBS non-consulters had higher IBS-QOL domain scores than consulters, especially for “Food Avoidance” (t=-3.09; df=226; P=0.002).
The mean overall IBS-QOL scores for the four IBS subtypes were within the 65 and 80-point boundaries. IBS-U had the highest overall IBS-QOL score compared to the other subtypes (χ2=14.1; df=3; P=0.003) (Fig. 2). IBS-D and IBS-M had the lowest overall mean IBS-QOL scores.
Figure 2.
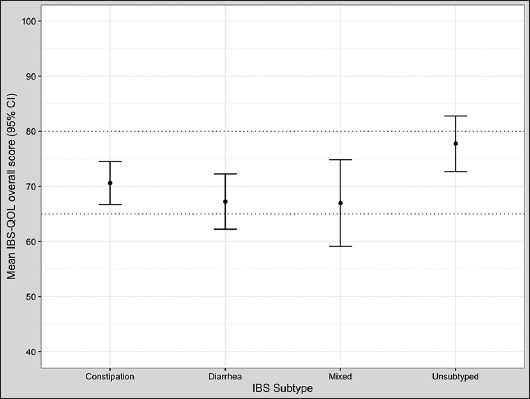
Mean irritable bowel syndrome quality of life (IBS-QOL) overall scores as a function of IBS subtypes
Higher scores in IBS-QOL indicate better health-related quality of life (HR-QOL). A score of 80 points or more suggests no association between overall mean HR-QOL and intestinal problems; scores less than 65 points correspond to moderate to severe IBS. A mean difference of 14 points was considered clinically important. Error bars show 95% confidence limits The internal consistency of the IBS-QOL questionnaire was high (Cronbach α = 0.96).
Discussion
The results of this study show a high prevalence of IBS in the study population. Other studies in Colombia reported lower prevalences: 19.9% in a population-based study (Rome III criteria) [30] and 12.5% among hospital employees (Rome I criteria) [29]. The results of the current study are consistent with those found in a sample of patients consulting a gastroenterology service (23%) [32]. Here, patients younger than 30 years had a lower prevalence (13.1%). IBS prevalence varied with diagnostic criteria, context and geographical location, age, socioeconomic and sociocultural factors, and the date the survey was conducted, factors that decrease the comparability of results across trials [4].
IBS is common in countries of the western hemisphere, with prevalence estimates reaching 22% in the United Kingdom and 32% in Iceland (Manning criteria) [33]. In Asia, the prevalence is lower, with frequencies between 11% and 14% (Manning or Rome II criteria). Reports of IBS prevalence have been published for Asian [34-38] and North American [39,40] university communities. In China, the range of prevalence estimates (Rome III criteria) was 7.9-10.4% in college students [36-38]. In the Western Hemisphere, studies report a 10.9% prevalence (Rome II criteria) in the United States [39] and up to 37% in Canada (Rome I criteria) [40].
We found IBS-C was the predominant IBS subtype, followed by IBS-U, IBS-D, and IBD-M. In Colombia, IBS-M (58%) was reported as the most common subtype, and IBS-U as the least frequent (4.5%) [30]. Two studies of college students in China (Rome III criteria) showed different subtype predominance, IBS-M [38] and IBS-C [37]; the least frequent in both studies was IBS-U. In Latin America, the predominant subtypes by the Rome III criteria were IBS-M (47%) in Venezuela [41] and IBS-D in Peru (37%) [42].
In the current study, we found an overall HR-QOL below 80 points. These results are similar to those of other studies reporting lower HR-QOL scores in patients with IBS compared to those without the diagnosis [11,28,43-45]. The study population had moderate to severe alterations in “Health Worry” and “Food Avoidance” domains. Apart from “Sexual Function” and “Relationships”, there was some degree of impairment in the other domains. Therefore, symptoms could alter the perception of the state of health of the individual who suffers from IBS and limits food intake. Limitations imposed by dietary habits were the main concern of the study population.
Dietary habits such as inadequate caloric intake, low intake of fruits and vegetables, and a high intake of carbohydrates, have been reported in university students in Colombia [46]. This diet favors high consumption of nonabsorbable disaccharides such as fructose and fructans, other monosaccharides, polysaccharides, polyols (FODMAPs) [47,48], and high-fat fried foods [49] that are associated with an increase in IBS symptoms. Patients without dietary guidance consciously exclude some of these foods but continue consuming others [50]. However, dietary guidance, coupled with a nutritional journal that allows individualization of diet recommendations, could increase HR-QOL significantly [50]. Strict nutritional restrictions may have a negative impact on the HR-QOL of patients who would have no idea what to eat. This could be troublesome for students that come from abroad and must adapt to unfamiliar foods. Consequently, the aim of therapy should be less focused on dietary restrictions and more on avoiding their need, thereby increasing HR-QOL.
The study found a difference in overall HR-QOL between IBS-U and other subtypes. Mechanisms of avoidance and adaptation of IBS patients are consistent in all subtypes [51]. This partly explains the similarity in HR-QOL scores between the IBS-D, IBS-C, and IBS-M subtypes. However, the severity of abdominal pain or discomfort has a significant effect, larger than that of the subtype classification, on daily activities and beliefs about IBS, [52]. This supports the trend to include severity of IBS symptoms as an important dimension in therapy [53].
In general, HR-QOL was lower in IBS consulters than in IBS non-consulters. “Health Worry” HR-QOL was higher in those who did not seek consultation. The IBS college population does not seek consultation with health services because they feel their symptoms do not require medical attention (symptoms disappear on their own) [40]. Although “Food Avoidance” was affected in both consulters and non-consulters, it was significantly lower in IBS consulters. This could be the main reason for seeking consultation in IBS patients.
IBS patients tend to catastrophize abdominal pain or discomfort [54]. Cognitive factors facilitate the interpretation of visceral events in an exaggerated manner; patients are more alert to them and suffer more anxiety when they arise [54]. This produces a cycle that begins with the visceral event and continues to exacerbate feelings of symptom anxiety, which again increases the presence of these events. This could explain why it is common to find low scores in the “Health Worry” domain in several studies [22,28,55,56]. Even after a visit to the doctor, thoughts of a wrong diagnosis or fear of a worse condition may persist [51,57]. Patients believe IBS can evolve into conditions such as colitis, malnutrition, cancer, or those that require surgery [58].
Although we did not achieve the calculated sample size, a number of subjects was reached greater than that required to estimate both the prevalence and the mean HR-QOL. The random sampling selection scheme may have been affected by non-response; however, a significant part of the population was surveyed. Stratification produced a sample where all units and socioeconomic backgrounds were represented. Sex was a stratification variable, which accomplished distribution balance. In other studies there was a greater number of female participants [35,38], who are more likely to answer surveys [59] and have a greater severity of symptoms [60].
A limitation of the study is the possibility of prevalence overestimation because of non-response bias. In Colombia, a culture of high response rates to electronic surveys has yet to be created. We attempted to increase response rates by sending an agile electronic survey with short and focused invitation objectives, small incentives, several waves encouraging participation, and a simple and readable interface. However, the response rate was lower than 30%. The low response rate in the current study may be due to a cultural lack of motivation to answer online surveys in our community and specifically in young persons. This would need further study. Other countries with higher response rates to online surveys should consider this as a feasible technique for frequency studies. Sending the invitations to institutional e-mails, possibly not the respondents’ primary e-mails, could be one reason for non-response. In addition, at the time of the study, auto-forwarding to a primary e-mail was not available for the entire community. It would have been appropriate to take a sample of non-responders to establish the non-response bias. However, the sampling design made it difficult to access a subsample distributed across faculties and class schedules. Nonetheless, smoking prevalence (a calibration variable) was very similar to that found in 2009 (24.1%) [61]. This suggests that the data are valid and decreases the probability that respondents did not complete questions properly.
Lactose intolerance is a condition that could overestimate the prevalence of IBS. Tests for diagnosis include breath or blood tests that are not feasible as part of an electronic survey. Lactose intolerance symptoms are similar to those of IBS, and, to our knowledge, a valid scale to diagnose this condition has not been published. However, since both syndromes overlap by up to as much as 86%, it would be impractical to separate these two populations [62]. Furthermore, there appears to be no important difference between the two as regards to dietary recommendations [63].
As a clinical diagnosis was adopted, there is a possibility that organic diseases that mimic IBS were not diagnosed. The prevalence may have been overestimated, since no questions about the presence of organic conditions were posed. Diseases such as inflammatory bowel disease, which may score positive for IBS on the RIIIAQ [64], may have been present, as the RIIIAQ is not designed to distinguish between organic and functional disease. It is also possible that IBS-positive participants who did not seek medical attention could suffer from an undiagnosed organic condition, which would be impossible to exclude even if the survey included a relevant question.
Interventions in young patients with IBS should aim to inform patients about the course of the disease, while promoting individualized dietary counseling and strategies to adapt to symptoms. These factors are of interest to patients [58]. “Health Worry and “Food Avoidance” domains could improve if these aspects of therapy were considered in consultation.
In conclusion, the weighted prevalence of IBS in a population aged 18-30 years at the Universidad Javeriana was 24.0%. IBS-C was the most common subtype. Food avoidance and health worry were the most affected HR-QOL domains. Patients with IBS-U had higher HR-QOL compared to IBS-D and IBS-M. Twenty-eight percent of the IBS-positive population had not consulted healthcare personnel about IBS-related symptoms. Although no differences were found in overall HR-QOL between IBS consulters and non-consulters, food avoidance appears to be a key factor in seeking consultation. The prevalence if IBS could have been overestimated because of non-response bias and the presence of organic disease.
Summary Box.
What is already known:
Irritable bowel syndrome (IBS) decreases health-related quality of life (HR-QOL) in adults
Young adults with IBS are exposed to academic stress and disordered eating patterns, which could affect HR-QOL
What the new findings are:
IBS prevalence was high in a university-based population aged 18-30 years in Bogotá, Colombia
IBS-unsubtyped subjects had better HR-QOL compared to other subtypes
Approximately one-fourth of the IBS positive population did not seek consultation for IBS-related symptoms
Food avoidance was a clinically important factor for consultation in young adults with IBS
Biography
School of Medicine, Pontificia Universidad Javeriana, Bogotá D.C., Colombia
Footnotes
Conflict of Interest: None
References
- 1.Hillilä MT, Färkkilä MA. Prevalence of irritable bowel syndrome according to different diagnostic criteria in a non-selected adult population. Aliment Pharmacol Ther. 2004;20:339–345. doi: 10.1111/j.1365-2036.2004.02034.x. [DOI] [PubMed] [Google Scholar]
- 2.Mearin F, Badía X, Balboa A, et al. Irritable bowel syndrome prevalence varies enormously depending on the employed diagnostic criteria: comparison of Rome II versus previous criteria in a general population. Scand J Gastroenterol. 2001;36:1155–1161. doi: 10.1080/00365520152584770. [DOI] [PubMed] [Google Scholar]
- 3.Cremonini F, Talley NJ. Irritable bowel syndrome:epidemiology, natural history, health care seeking and emerging risk factors. Gastroenterol Clin North Am. 2005;34:189–204. doi: 10.1016/j.gtc.2005.02.008. [DOI] [PubMed] [Google Scholar]
- 4.Quigley EM, Abdel-Hamid H, Barbara G, et al. A global perspective on irritable bowel syndrome: a consensus statement of the World Gastroenterology Organisation Summit Task Force on irritable bowel syndrome. J Clin Gastroenterol. 2012;46:356–366. doi: 10.1097/MCG.0b013e318247157c. [DOI] [PubMed] [Google Scholar]
- 5.Saito YA, Schoenfeld P, Locke GR., 3rd The epidemiology of irritable bowel syndrome in North America: a systematic review. Am J Gastroenterol. 2002;97:1910–1915. doi: 10.1111/j.1572-0241.2002.05913.x. [DOI] [PubMed] [Google Scholar]
- 6.Talley NJ, O’Keefe EA, Zinsmeister AR, Melton LJ., 3rd Prevalence of gastrointestinal symptoms in the elderly: a population-based study. Gastroenterology. 1992;102:895–901. doi: 10.1016/0016-5085(92)90175-x. [DOI] [PubMed] [Google Scholar]
- 7.Bennett G, Talley NJ. Irritable bowel syndrome in the elderly. Best Pract Res Clin Gastroenterol. 2002;16:63–76. doi: 10.1053/bega.2001.0266. [DOI] [PubMed] [Google Scholar]
- 8.Ladep NG. Irritable Bowel Syndrome:Epidemiology, Pathophysiology and Diagnosis. Jos J Med. 2008;3:7–11. [Google Scholar]
- 9.Adeniji OA, Barnett CB, Di Palma JA. Durability of the diagnosis of irritable bowel syndrome based on clinical criteria. Dig Dis Sci. 2004;49:572–574. doi: 10.1023/b:ddas.0000026300.47363.3b. [DOI] [PubMed] [Google Scholar]
- 10.Badia X, Mearin F, Balboa A, et al. Burden of illness in irritable bowel syndrome comparing Rome I and Rome II criteria. Pharmacoeconomics. 2002;20:749–758. doi: 10.2165/00019053-200220110-00004. [DOI] [PubMed] [Google Scholar]
- 11.Amouretti M, Le Pen C, Gaudin AF, et al. Impact of irritable bowel syndrome (IBS) on health-related quality of life (HRQOL) Gastroenterol Clin Biol. 2006;30:241–246. doi: 10.1016/s0399-8320(06)73160-8. [DOI] [PubMed] [Google Scholar]
- 12.Lee V, Guthrie E, Robinson A, et al. Functional bowel disorders in primary care: factors associated with health-related quality of life and doctor consultation. J Psychosom Res. 2008;64:129–138. doi: 10.1016/j.jpsychores.2007.09.004. [DOI] [PubMed] [Google Scholar]
- 13.ten Berg MJ, Goettsch WG, van den Boom G, Smout AJ, Herings RM. Quality of life of patients with irritable bowel syndrome is low compared to others with chronic diseases. Eur J Gastroenterol Hepatol. 2006;18:475–481. doi: 10.1097/00042737-200605000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Beiter R, Nash R, McCrady M, et al. The prevalence and correlates of depression, anxiety, and stress in a sample of college students. J Affect Disord. 2015;173:90–96. doi: 10.1016/j.jad.2014.10.054. [DOI] [PubMed] [Google Scholar]
- 15.Costarelli V, Patsai A. Academic examination stress increases disordered eating symptomatology in female university students. Eat Weight Disord. 2012;17 doi: 10.1007/BF03325343. e164-e169. [DOI] [PubMed] [Google Scholar]
- 16.Lorenzini R, Betancur-Ancona DA, Chel-Guerrero LA, et al. Nutritional status of university students from México in relation with their lifestyle. Nutr Hosp. 2015;32:94–100. doi: 10.3305/nh.2015.32.1.8872. [DOI] [PubMed] [Google Scholar]
- 17.Morgan DR, Squella F, Peña E, et al. M1350 Multinational Validation of the Spanish ROME III Adult Diagnostic Questionnaire: Comparable Sensitivity and Specificity to English Instrument. Gastroenterology. 2010;138:S386. [Google Scholar]
- 18.Schmulson M, Morgan D, Cortés L, et al. Traducción y validación multinacional del cuestionario diagnóstico para adultos de Roma III en español. Rev Gastroenterol Méx. 2008;73:79. [Google Scholar]
- 19.Schmulson M, Ortiz O, Mejia-Arangure JM, et al. Further validation of the IBS-QOL: female Mexican IBS patients have poorer quality of life than females from North Carolina. Dig Dis Sci. 2007;52:2950–2955. doi: 10.1007/s10620-006-9689-9. [DOI] [PubMed] [Google Scholar]
- 20.Drossman DA. Rome III Diagnostic Questionnaire for the Adult Functional GI Disorders (including Alarm Questions) and Scoring Algorithm. The functional gastrointestinal disorders. McLean, Virginia: Degnon Associates; 2006. pp. 917–952. [Google Scholar]
- 21.Patrick DL, Drossman DA, Frederick HO. A quality-of-life measure for persons with irritable bowel syndrome (IBS-QOL):user’s manual and scoring diskette for United States version. Seattle, Washington: University of Washington; 1997. [Google Scholar]
- 22.Park JM, Choi MG, Kim YS, et al. Quality of life of patients with irritable bowel syndrome in Korea. Qual Life Res. 2009;18:435–446. doi: 10.1007/s11136-009-9461-7. [DOI] [PubMed] [Google Scholar]
- 23.Drossman D, Morris CB, Hu Y, et al. Characterization of health related quality of life (HRQOL) for patients with functional bowel disorder (FBD) and its response to treatment. Am J Gastroenterol. 2007;102:1442–1453. doi: 10.1111/j.1572-0241.2007.01283.x. [DOI] [PubMed] [Google Scholar]
- 24.Patrick DL, Erickson P. Health status and health policy: quality of life in health evaluation and resource allocation. New York: 1993. [Google Scholar]
- 25.Patrick DL, Drossman DA, Frederick IO, DiCesare J, Puder KL. Quality of life in persons with irritable bowel syndrome - development and validation of a new measure. Dig Dis Sci. 1998;43:400–411. doi: 10.1023/a:1018831127942. [DOI] [PubMed] [Google Scholar]
- 26.Drossman DA, Patrick DL, Whitehead WE, et al. Further validation of the IBS-QOL: a disease-specific quality-of-life questionnaire. Am J Gastroenterol. 2000;95:999–1007. doi: 10.1111/j.1572-0241.2000.01941.x. [DOI] [PubMed] [Google Scholar]
- 27.Departamento Administrativo Nacional de Estadística (DANE) de Colombia. Estratificación Socioeconómica. 2016. Estadísticas por Tema http://www.dane.gov.co/index.php/esp/estratificacion-socioeconomica/generalidades .
- 28.Akehurst RL, Brazier JE, Mathers N, et al. Health-related quality of life and cost impact of irritable bowel syndrome in a UK primary care setting. Pharmacoeconomics. 2002;20:455–462. doi: 10.2165/00019053-200220070-00003. [DOI] [PubMed] [Google Scholar]
- 29.Ángel LA, Amaya A, Perilla C, et al. Prevalencia del síndrome de intestino irritable y factores asociados. Acta Médica Colomb. 1997;22:219–224. [Google Scholar]
- 30.Gómez DF, Morales JG, Rojas LMA, et al. Factores sociosanitarios y prevalencia del intestino irritable según los criterios diagnósticos de Roma III en una población general de Colombia. Gastroenterol Hepatol. 2008;32:395–400. doi: 10.1016/j.gastrohep.2009.01.177. [DOI] [PubMed] [Google Scholar]
- 31.R Development Core Team. R: a language and environment for statistical computing [Google Scholar]
- 32.Restrepo LF, Páez ML, Guzmán DM, et al. Síndrome de intestino irritable y trastornos de ansiedad y depresión. Universidad del Rosario - Universidad CES. 2011 [Google Scholar]
- 33.Choung RS, Locke GR., 3rd Epidemiology of IBS. Gastroenterol Clin North Am. 2011;40:1–10. doi: 10.1016/j.gtc.2010.12.006. [DOI] [PubMed] [Google Scholar]
- 34.Okami Y, Kato T, Nin G, et al. Lifestyle and psychological factors related to irritable bowel syndrome in nursing and medical school students. J Gastroenterol. 2011;46:1403–1410. doi: 10.1007/s00535-011-0454-2. [DOI] [PubMed] [Google Scholar]
- 35.Kim YJ, Ban DJ. Prevalence of irritable bowel syndrome, influence of lifestyle factors and bowel habits in Korean college students. Int J Nurs Stud. 2005;42:247–254. doi: 10.1016/j.ijnurstu.2004.06.015. [DOI] [PubMed] [Google Scholar]
- 36.Dong YY, Chen FX, Yu YB, et al. A school-based study with Rome III criteria on the prevalence of functional gastrointestinal disorders in Chinese college and university students. PLoS One. 2013;8:e54183. doi: 10.1371/journal.pone.0054183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Dong YY, Zuo XL, Li CQ, Yu YB, Zhao QJ, Li YQ. Prevalence of irritable bowel syndrome in Chinese college and university students assessed using Rome III criteria. World J Gastroenterol. 2010;16:4221–4226. doi: 10.3748/wjg.v16.i33.4221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Dai N, Cong Y, Yuan H. Prevalence of irritable bowel syndrome among undergraduates in Southeast China. Dig Liver Dis. 2008;40:418–424. doi: 10.1016/j.dld.2008.01.019. [DOI] [PubMed] [Google Scholar]
- 39.Hazlett-Stevens H, Craske MG, Mayer EA, Chang L, Naliboff BD. Prevalence of irritable bowel syndrome among university students: the roles of worry, neuroticism, anxiety sensitivity and visceral anxiety. J Psychosom Res. 2003;55:501–505. doi: 10.1016/s0022-3999(03)00019-9. [DOI] [PubMed] [Google Scholar]
- 40.Gick ML, Thompson WG. Negative affect and the seeking of medical care in university students with irritable bowel syndrome: a preliminary study. J Psychosom Res. 1997;43:535–540. doi: 10.1016/s0022-3999(97)00141-4. [DOI] [PubMed] [Google Scholar]
- 41.Veitia G, Pernalete B, Cachima L, et al. Prevalencia del síndrome intestino irritable en la población adulta venezolana. Rev Gen. 2013;67:139–144. [Google Scholar]
- 42.Gonzales-Gamarra R, Ruiz-Sánchez J, Jiménez-Franco L, et al. Prevalencia del Sindrome de Intestino Irritable en la Población Adulta de Chiclayo durante el año 2011. Rev Gastroenterol del Peru. 2012;32:381–386. [PubMed] [Google Scholar]
- 43.Rey E, García-Alonso MO, Moreno-Ortega M, Alvarez-Sanchez A, Diaz-Rubio M. Determinants of quality of life in irritable bowel syndrome. J Clin Gastroenterol. 2008;42:1003–1009. doi: 10.1097/MCG.0b013e31815af9f1. [DOI] [PubMed] [Google Scholar]
- 44.Vinaccia S, Fernández H, Amador O, et al. Calidad de vida, ansiedad y depresión en pacientes con diagnóstico de síndrome de colon irritable. Ter Psicológica. 2005;23:65–74. [Google Scholar]
- 45.Coffin B, Dapolgny M, Cloarec D, et al. Relationship between severity of symptoms and quality of life in 858 patients with irritable bowel syndrome. Gastroenterol Clin Biol. 2004;28:11–15. doi: 10.1016/s0399-8320(04)94834-8. [DOI] [PubMed] [Google Scholar]
- 46.Vargas-Zárate M, Becerra-Bulla F, Prieto-Suárez E. Evaluación de la ingesta dietética en estudiantes universitarios. Bogotá, Colombia. Rev Salud Pública. 2010;12:116–125. doi: 10.1590/s0124-00642010000100011. [DOI] [PubMed] [Google Scholar]
- 47.Shepherd SJ, Parker FC, Muir JG, Gibson PR. Dietary triggers of abdominal symptoms in patients with irritable bowel syndrome: randomized placebo-controlled evidence. Clin Gastroenterol Hepatol. 2008;6:765–771. doi: 10.1016/j.cgh.2008.02.058. [DOI] [PubMed] [Google Scholar]
- 48.Ong DK, Mitchell SB, Barrett JS, et al. Manipulation of dietary short chain carbohydrates alters the pattern of gas production and genesis of symptoms in irritable bowel syndrome. J Gastroenterol Hepatol. 2010;25:1366–1373. doi: 10.1111/j.1440-1746.2010.06370.x. [DOI] [PubMed] [Google Scholar]
- 49.Böhn L, Störsrud S, Törnblom H, Bengtsson U, Simrén M. Self-reported food-related gastrointestinal symptoms in IBS are common and associated with more severe symptoms and reduced quality of life. Am J Gastroenterol. 2013;108:634–641. doi: 10.1038/ajg.2013.105. [DOI] [PubMed] [Google Scholar]
- 50.Ostgaard H, Hausken T, Gundersen D, El-Salhy M. Diet and effects of diet management on quality of life and symptoms in patients with irritable bowel syndrome. Mol Med Rep. 2012;5:1382–1390. doi: 10.3892/mmr.2012.843. [DOI] [PubMed] [Google Scholar]
- 51.Farndale R, Roberts L. Long-term impact of irritable bowel syndrome: a qualitative study. Prim Health Care Res Dev. 2011;12:52–67. doi: 10.1017/S1463423610000095. [DOI] [PubMed] [Google Scholar]
- 52.Heitkemper M, Cain KC, Shulman R, Burr R, Poppe A, Jarrett M. Subtypes of irritable bowel syndrome based on abdominal pain/discomfort severity and bowel pattern. Dig Dis Sci. 2011;56:2050–2058. doi: 10.1007/s10620-011-1567-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Azpiroz F, Chang L, Chey W, et al. Multi-dimensional clinical profile (MDCP) for the functional gastrointestinal disorders. 1st ed. Raleigh, NC: The Rome Foundation; 2015. [Google Scholar]
- 54.Kennedy PJ, Clarke G, Quigley EM, Groeger JA, Dinan TG, Cryan JF. Gut memories: towards a cognitive neurobiology of irritable bowel syndrome. Neurosci Biobehav Rev. 2012;36:310–340. doi: 10.1016/j.neubiorev.2011.07.001. [DOI] [PubMed] [Google Scholar]
- 55.Paré P, Gray J, Lam S, et al. Health-related quality of life, work productivity, and health care resource utilization of subjects with irritable bowel syndrome: baseline results from LOGIC (Longitudinal Outcomes Study of Gastrointestinal Symptoms in Canada), a naturalistic study. Clin Ther. 2006;28:1726–1735. doi: 10.1016/j.clinthera.2006.10.010. [DOI] [PubMed] [Google Scholar]
- 56.Brun-Strang C, Dapoigny M, Lafuma A, Wainsten JP, Fagnani F. Irritable bowel syndrome in France: quality of life, medical management, and costs: the Encoli study. Eur J Gastroenterol Hepatol. 2007;19:1097–1103. doi: 10.1097/MEG.0b013e3282f1621b. [DOI] [PubMed] [Google Scholar]
- 57.Casiday RE, Hungin AP, Cornford CS, de Wit NJ, Blell MT. Patients’ explanatory models for irritable bowel syndrome: symptoms and treatment more important than explaining aetiology. Fam Pract. 2009;26:40–47. doi: 10.1093/fampra/cmn087. [DOI] [PubMed] [Google Scholar]
- 58.Halpert A, Dalton CB, Palsson O, et al. What patients know about irritable bowel syndrome (IBS) and what they would like to know. National survey on patient educational needs in IBS and development and validation of the patient educational needs questionnaire (PEQ) Am J Gastroenterol. 2007;102:1972–1982. doi: 10.1111/j.1572-0241.2007.01254.x. [DOI] [PubMed] [Google Scholar]
- 59.Sax LJ, Gilmartin SK, Bryant AN. Assessing response rates and nonresponse bias in web and paper surveys. Res High Educ. 2003;44:409–432. [Google Scholar]
- 60.Corney RH, Stanton R. Physical symptom severity, psychological and social dysfunction in a series of outpatients with irritable bowel syndrome. J Psychosom Res. 1990;34:483–491. doi: 10.1016/0022-3999(90)90022-v. [DOI] [PubMed] [Google Scholar]
- 61.Novoa MM ComitéAsesor Programa Universidad Saludable. Caracterización del consumo de cigarrillo en la comunidad universitaria de la Pontificia Universidad Javeriana. Bogotá, DC: Pontificia Universidad Javeriana; 2009. [Google Scholar]
- 62.Frissora CL, Koch KL. Symptom overlap and comorbidity of irritable bowel syndrome with other conditions. Curr Gastroenterol Rep. 2005;7:264–271. doi: 10.1007/s11894-005-0018-9. [DOI] [PubMed] [Google Scholar]
- 63.Parker TJ, Woolner JT, Prevost AT, Tuffnell Q, Shorthouse M, Hunter JO. Irritable bowel syndrome: is the search for lactose intolerance justified? Eur J Gastroenterol Hepatol. 2001;13:219–225. doi: 10.1097/00042737-200103000-00001. [DOI] [PubMed] [Google Scholar]
- 64.Halpin SJ, Ford AC. Prevalence of symptoms meeting criteria for irritable bowel syndrome in inflammatory bowel disease: systematic review and meta-analysis. Am J Gastroenterol. 2012;107:1474–1482. doi: 10.1038/ajg.2012.260. [DOI] [PubMed] [Google Scholar]


