Abstract
IgA nephropathy (IgAN) is a common chronic glomerular disease that, in most patients, slowly progresses to ESRD. The immune and autoimmune responses that characterize IgAN indicate a potential benefit for corticosteroids. The 2012 Kidney Disease Improving Global Outcome (KDIGO) guidelines suggest giving corticosteroids to patients with rather preserved renal function (GFR>50 ml/min per 1.73 m2) and persistent proteinuria >1 g/d, despite 3–6 months of optimized supportive care with renin-angiotensin system blockers. However, the evidence supporting this guideline was considered of low quality. More recent results from large cohort studies and randomized, controlled trials have provided conflicting messages about the benefits of corticosteroid treatment over supportive care alone, mostly involving optimized renin-angiotensin system blockade, which might generate further uncertainty in the therapeutic choice. Overall, these results indicate that corticosteroids are a powerful tool for treating patients with IgAN; however, treatment success is not universal and mostly occurs in patients who are highly proteinuric with early CKD. In patients with advanced CKD, the side effects of corticosteroids increase, and the renal protection decreases. This brief review aimed at integrating the findings of these recently published reports to provide balanced advice for clinicians as well as suggestions for future trials.
Keywords: IgA nephropathy, progression of chronic renal failure, glomerular disease, immunosuppression, risk factors
IgA nephropathy (IgAN) is a common glomerular disease characterized by dominant or codominant IgA glomerular deposits, variable clinical presentation, and variable course.1,2 Most patients have a slowly progressive disease, developing in 40% of the patients with ESRD within 20 years, but lasting remissions can occur—rarely spontaneously in adults—as well as rapidly progressive courses.3–8 After the diagnosis of IgAN, the main questions asked by the patient are whether progression is likely and which could be the most effective treatment to halt or slow down the loss of renal function. Several advancements have been made in the knowledge of the multihit pathogenesis of IgAN,9 which includes synthesis of galactose-deficient IgA1,10 antiglycan antibody production,11 circulating IgA1 immune complexes formation, and glomerular deposition triggering inflammation and damage.12,13 Biomarkers related to the pathogenetic process of IgAN can detect risk factors and identify new targets for focused therapies.14,15 However, while waiting for innovative drugs, the central role of the immune and autoimmune response activation in the development and progression of IgAN has rescued the interest in what we have presently available as most powerful (although potentially harmful) drugs (i.e., corticosteroids). In spite of decades of reports on the use of corticosteroids in IgAN, the results are still debated and controversial. This brief review will focus on recently reported retrospective and prospective studies, which have provided different messages—thus potentially generating further incertitude—aiming at finding a clue of interpretation and agreement of results and balanced advice for clinicians.
Corticosteroids in IgAN: Short History, Guidelines, and Systemic Reviews
The history of corticosteroids in IgAN is long and marked by mixed fortune. The pioneer uncontrolled pilot study by Kobayashi et al.16 30 years ago showed a clear benefit of oral prednisone (40 mg/d tapered over 1–2 years) in patients in early phase of the disease (creatinine clearance >70 ml/min) and persisting proteinuria of 1–2 g/d, with reduction in proteinuria and protection from functional decline at 10 years follow-up.17 These results were received with skepticism, because previous anecdotal experiences of using corticosteroids in IgAN at low doses and for short periods had been disappointing; moreover, the inflammatory nature of IgA deposits seemed, at this time, largely unproven.18 IgA was known to play a protective role against pathogens in mucosal secretions, being not as active as IgG in eliciting the inflammatory reaction by complement activation and mediators release.18,19 Over the following decade, it became clear that mesangial cells acted as not only glomerular capillary network support but also, highly reactive cells, proliferating and producing inflammatory mediators after contact with macromolecular IgA.20–22 Instead of a passive mesangial engulfment of scarcely immunologically active Igs, IgA glomerular deposits turned out to be a harmful event leading to mesangial cell activation, matrix production, proinflammatory cytokine release, and endocapillary influx of inflammatory cells, which led to sclerosis.23–25 Therefore, IgAN was appreciated as an inflammatory disease, giving rationale for corticosteroid therapy considering its pronounced anti–inflammatory effects and rather weak immunosuppressive activity. Over the following decade, the publication of successful randomized, controlled trials (RCTs)26–28 showing a favorable outcome in patients treated with corticosteroids for 6 months was not astonishing for the nephrologist at this point of knowledge on the pathobiology of IgAN.
At the same time, renin-angiotensin system blockers (RASBs) made an extraordinary successful career switch from antihypertensive agents to factors modulating renal hemodynamics, proteinuria, and progression to sclerosis, thus suggesting a key role in slowing nonimmune progression of any kind of renal disease,29 particularly when proteinuria was >1 g/d. Moreover, mesangial cells were found to have receptors for angiotensin II, inducing mesangial matrix production and sclerosis.30 Therefore, the positive outcomes reported by RCTs using RASBs in patients with proteinuric IgAN were perceived as not unexpected.31–33
All of the RCTs testing the effects of corticosteroids and/or RASBs in IgAN provided interesting results but suffered from various limitations, hence the need of guidelines for clinical practice. The Kidney Disease Improving Global Outcome (KDIGO) clinical guidelines published in 201234 reported the first attempt to summarize the results of the literature providing the indications to corticosteroids in IgAN (Table 1), although the level of evidence was considered of low quality and RASBs represented the first-line treatment (Table 1, guideline A). The KDIGO guidelines suggest giving corticosteroids to patients with GFR>50 ml/min per 1.73 m2 maintaining persistent proteinuria >1 g/d, despite 3–6 months of optimized supportive care with RASBs. The best results were obtained with 6-month corticosteroid regimens (Table 1, guideline B) using either a course of three intravenous pulses of 1 g methylprednisolone and 0.5 mg/kg oral prednisone on alternate days26 or a regimen of oral prednisone (0.8–1 mg/kg per day) for 2 months, weaning over 6 months27,28 (Table 1, guideline C). Both protocols induced reduction in disease progression and proteinuria without serious side effects. A long–term legacy effect was observed for the intravenous protocol.35
Table 1.
From the KDIGO guidelines for corticosteroids in IgAN34
| (A) Supportive care with antiproteinuric and antihypertensive drugs (statement 10.2). We recommend long–term ACE-I or ARB (RASBs) treatment when proteinuria is >1 g/d, with uptitration of drug depending on BP (1B). Suggestions to uptitrate RASBs as far as tolerated to achieve proteinuria <1 g/d (2C). Target BP <125/75 mmHg when proteinuria is >1 g/d (not graded). |
| (B) Corticosteroids (statement 10.3.1). We suggest that patients with persistent proteinuria >1 g/d, despite 3–6 mo of optimized supportive care (including RASBs and BP control) and GFR>50 ml/min per 1.73 m2, receive a 6-mo course of corticosteroid therapy (2C). |
| (C) Corticosteroid regimens |
| (a) iv Bolus injection of 1 g methylprednisolone for 3 d each at months 1, 3, and 5 followed by oral steroid (0.5 mg/kg prednisone) on alternate days for 6 mo.26 |
| (b) Oral prednisone starting with 0.8–1 mg/kg per d for 2 mo and then reduced by 0.2 mg/kg per d per mo for the next 4 mo.27,28 |
| (D) Immunosuppressive agents cyclophosphamide and azatiophrine (statement 10.4.1). We suggest not treating with corticosteroids combined with cyclophosphamide or azathioprine in patients with IgAN (unless there is a crescentic IgAN with rapidly progressive course; 2D). |
Evidence is graduated in levels: 1, recommendations; 2, suggestions; A to D indicates high quality to very low quality, respectively.34
Very limited data were available on the benefits of adding other immunosuppressive drugs to corticosteroids.36,37 The KDIGO guidelines suggest a combination of corticosteroids and cyclophosphamide or azathioprine only in patients with crescentic forms with rapidly progressive course (Table 1, guideline D). This review will not be focused on these patients but rather, will focus on the patients with the most common cases of IgAN with slow relentless progression.
In 2015, a review of the Cochrane Database on immunosuppressive agents in IgAN38 analyzed 1781 patients included in 32 studies. Corticosteroids significantly improved the risks of progression to ESRD and doubling of serum creatinine, reducing proteinuria as well. The combination of corticosteroids and RASBs was even more effective, but only two studies were available.27,28 The benefit of adding cytotoxic agents was considered unproven.39 Available RCTs were few and small and had a high risk of bias, which did not allow the identification of patient baseline data that might predict response to therapy.
Unmet Needs and Unanswered Questions about the Use of Corticosteroids in IgAN
The results of the RCTs considered in the KDIGO and the 2015 Cochrane Database systematic review did not address some relevant questions, and still unmet needs were unsolved. Some issues were not defined, such as the effectiveness of corticosteroids in patients with IgAN with suboptimal renal function (GFR<50 ml/min for the KDIGO), advanced CKD (GFR<30 ml/min per 1.73 m2), or mild-moderate proteinuria (>0.5 to <1 g/d), as well as the dosage of corticosteroids with better results and minimal side effects.
The benefits of adding corticosteroids to strictly controlled supportive care were not satisfactory proven.40 In some previous RCTs, only some of the patients were treated with RASBs,26 and the BP control was not optimal by contemporary standards.34 In other patients, RASBs were halted before enrolment and then, started after randomization with corticosteroids, leading to inclusion of subjects who may have received benefits from RASB inhibition alone.27,28
No RCT has addressed whether the benefits of corticosteroids vary depending on baseline level of proteinuria, GFR, or renal pathology. The prognostic value of the lesions detected at renal biopsy acquired relevance after the Oxford clinicopathologic classification of IgAN.41,42 Four variables (mesangial hypercellularity M1, endocapillary hypercellularity E1, segmental glomerulosclerosis S1, and tubular atrophy/interstitial fibrosis T1–T2 [MEST score]) were found to be predictive of renal outcome independent of clinical data at the time of renal biopsy and during follow-up.42 Several validation studies followed,43–49 the largest being the European Validation Study of the Oxford Classification of IgA Nephropathy (VALIGA), which gathered 1147 patients from 13 European countries and followed them over 4.7 years.50 The VALIGA offered the possibility of new insights into the effects of corticosteroids in IgAN that were not deducible from RCTs or systematic reviews.
Effect of Corticosteroid Therapy from the Retrospective Observational VALIGA
The VALIGA cohort included patients with eGFR<30 ml/min per 1.73 m2 and proteinuria <0.5 g/d at renal biopsy and investigated the effect of pretreatment proteinuria or pathologic features on therapy.50,51 Most patients received RASBs (86%), 46% had corticosteroids (intravenous pulses in one third of the patients) in a minority of the patients associated with other various immunosuppressive drugs. The VALIGA confirmed M1, S1, and T1–T2 as predictors of the eGFR slope and renal survival to the combined end point of 50% reduction of eGFR or ESRD. In patients with proteinuria <0.5 g/d, E1 and M1 were significantly associated with increase in proteinuria to values ≥2 g/d.
The addition of M, S, and T scores to clinical variables increased the ability to predict progression only in patients who did not receive corticosteroids, indicating a possible favorable effect of this treatment.50 Two groups of patients with IgAN having superimposable clinical and histologic features and time-averaged proteinuria before starting corticosteroids were selected by a propensity score: 184 were treated with RASBs and corticosteroids, and 184 were treated with RASBs alone (Table 2).51 Patients treated with corticosteroids and RASBs had better outcomes compared with matched patients with RASBs alone for survival to the combined end point (P<0.01), rate of renal function decline (P=0.004), and reduction in proteinuria during the follow-up (P<0.001), with a significantly higher frequency of achieving proteinuria <1 g/d.
Table 2.
The retrospective cohort VALIGA50
| Propensity Score–Matched Patients with IgAN | RASB, n=184 | RASB and CS, n=184 | P Value |
|---|---|---|---|
| Age, yr | 38±14 | 39±16 | NS |
| eGFR, ml/min per 1.73 m2 | 69±29 | 68±31 | NS |
| Time-averaged proteinuria before starting CS, g/d | 1.1 (0.5, 2.3) | 1.2 (0.8, 2.3) | NS |
| M1, % | 30 | 31 | NS |
| E1, % | 9 | 12 | NS |
| S1, % | 76 | 76 | NS |
| T1–T2, % | 27 | 28 | NS |
| Outcomes | |||
| Rate of renal function decline, ml/min per 1.73 m2 per yr | −3.2±8.3 | −1.0±7.3 | 0.004 |
| Change in proteinuria during entire follow-up, g/d | −0.3 (−1.1, 0.3) | −0.8 (−1.6, −0.2) | <0.001 |
| Reduction proteinuria to <1 g/d, % | 54 | 84 | <0.001 |
| ESRD, % | 20 | 7 | 0.003 |
| Combined end point, % | 27 | 12 | <0.01 |
Using a propensity score from the 1147 patients enrolled, two groups each of 184 matched subjects were selected and compared.51 Data are reported as mean±SD. Renal biopsy MEST scores: M1, mesangial hypercellularity; E1, endothelial hypercellularity; S1, segmental glomerulosclerosis; and T1–T2, tubular atrophy and interstitial fibrosis. Combined end point: 50% reduction in GFR or ESRD. CS, corticosteroid.
Significantly better outcomes for survival to the combined end point and progressive loss of renal function were observed in patients with eGFR<50 ml/min per 1.73 m2 when receiving corticosteroids compared with matched subjects on RASBs alone (P=0.01). The benefits of corticosteroids increased according to pretreatment time–averaged proteinuria. The greatest protective effect was observed in patients with proteinuria >3 (P=0.001) or >1 g/d (P=0.03), whereas no difference was found between propensity-matched groups with corticosteroids added or not to RASBs at the available follow-up when proteinuria was <1 g/d. Time-averaged proteinuria <1 g/d was associated with better outcomes than higher levels, irrespective of the therapy adopted.
In the propensity-matched cohorts, therapy was given 1–6 months from renal biopsy. A lower rate of renal function decline and a greater reduction in proteinuria were observed when patients with M1, S1, and T1 scores were treated with corticosteroids compared with those treated with RASB alone.
In conclusion, the retrospective VALIGA study indicated clear benefits of corticosteroids in addition to RASBs compared with RASBs alone, particularly in patients with proteinuria >1 g/d, suggesting a value in patients with eGFR<50 ml/min per 1.73 m2 as well. However, because of the retrospective nature of the data collection and the limited knowledge on doses and compliance of corticosteroids, it was not possible to provide a recommendation, and all of the interest was focused on the results of the next RCTs.
An RCT on Intensive Supportive Care Plus Corticosteroids in IgAN: The STOP Trial
The STOP Trial52 tested the hypothesis that, in patients with IgAN, corticosteroids/immunosuppressive therapy (corticosteroids in combination or not with alkylating/antimetabolite agents) plus comprehensive supportive care would be superior to supportive care alone. The primary end point, after 3 years, was full clinical remission (<0.2 mg urinary protein/1 mg creatinine with stable eGFR) or decrease in the eGFR>15 ml/min per 1.73 m2. Eligible patients had proteinuria >0.75 and <3.5 g/d and hypertension or eGFR<90–30 ml/min per 1.73 m2. During a 6-month run-in phase, comprehensive and rigorous supportive care was adopted with RASBs (also ACE-I and ARB in combination, although not recommended by KDIGO) to attain BP of <125/75 mmHg and in patients who were persistently proteinuric, maximum approved daily dose or highest dose without unacceptable side effects. Moreover, the supportive care included moderate restriction of protein intake, cholesterol control with statins, smoking and nephrotoxic drugs avoidance.
The randomization excluded 34% of responders to supportive care (proteinuria <0.75 g/d) and 12% of high-risk patients (proteinuria >3.5 g/d, eGFR<30 ml/min per 1.73 m2, or GFR decreased by >30% during the run-in phase). The other patients were assigned to continue supportive care alone or with corticosteroid/immunosuppression (Table 3).The latter consisted in two protocols: 55 patients with eGFR of >60 ml/min per 1.73 m2 received glucocorticoid for 6 months (three intravenous 1-g methylprednisolone pulses at months 1, 3, and 5 and oral prednisolone at 0.5 mg/kg on alternate days), and 27 patients with eGFR>30 and <59 ml/min per 1.73 m2 received, for 36 months, 1.5 mg/k per day cyclophosphamide followed by 1.5 mg/kg per day azathioprine plus 40 mg/d oral prednisolone, waning over 36 months.
Table 3.
The STOP Trial: Summary of protocol and results52
| Variable | Supportive Care, n=80 | Supportive Care Plus Immunosuppression, n=82 | P Value |
|---|---|---|---|
| Age, yr | 45.8±12.5 | 42.8±13.1 | NS |
| eGFR, ml/min per 1.73 m2 | 57.4±24.9 | 61.1±29.0 | NS |
| Proteinuria, g/d | 1.6±0.7 | 1.8±0 | NS |
| Systolic BP | 131±14.0 | 127±8.5 | NS |
| Diastolic BP | 78±7.0 | 77±7.0 | NS |
| Outcomes | |||
| Full clinical remission, (%) | 4/80 (5) | 14/82 (17) | 0.01 |
| eGFR decrease >15 ml/min per 1.73 m2 | 22/80 (28) | 21/82 (26) | NS |
| AEs | |||
| Patients with one or more serious AEs | 21/80 | 29/80 | NS |
| Total no. of events of infection | 111 | 174 | 0.07 |
| Impaired glucose tolerance or diabetes mellitus | 1 | 9 | 0.02 |
Data are reported as mean±SD. Supportive care: optimized doses of RASBs to maintain BP<125/75 mmHg and in patients who are persistently proteinuric, maximum approved daily dose or highest dose without unacceptable side effects. Immunosuppression: (1) in 55 patients with eGFR of >60 ml/min per 1.73 m2, glucocorticoid for 6 months (1 g/d intravenous methylprednisolone for 3 days at months 1, 3, and 5 and 0.5 mg/kg oral prednisolone on the other days); and (2) in 27 patients with eGFR>30 and <59 ml/min per 1.73 m2, 1.5 mg/kg per day cyclophosphamide for 3 months followed by 1.5 mg/kg per day azathioprine for months 4–36 plus 40 mg/d oral prednisolone tapered to discontinuation at month 36. Full clinical remission: <0.2 mg urinary protein/1 mg creatinine with stable eGFR.
At the end of the 3 years, 5% of patients in the supportive care group had full clinical remission (P=0.001) versus 17% in the immunosuppression group; however, no difference between the two groups was found in the decrease of eGFR>15 ml/min per 1.73 m2 (28% versus 26%, respectively). Patients in the corticosteroid/immunosuppression group had significantly lower mean proteinuria than those in the supportive care group at 1 year of follow-up, but the difference was no longer significant in the patients tested at 3 years, mostly because of an increase in proteinuria in subjects with advanced CKD. Microscopic hematuria disappeared more frequently in the corticosteroid/immunosuppression group at the end of the RCT. More patients receiving glucocorticoid monotherapy than those receiving combination immunosuppressive therapy had remission of proteinuria, hematuria, or both.
Serious adverse events (AEs) had similar frequencies in the two study groups, but patients treated with immunosuppression reported more cases of infection, impaired glucose metabolism, and body weight gain. Moreover, two patients had malignant neoplasms during combined immunosuppression.
The STOP Trial conclusion was that additional immunosuppressive therapy would not provide substantial kidney–related benefits in patients with high-risk IgAN, because there was no difference in the rate of decrease in eGFR, although corticosteroid/immunosuppressive therapy induced complete remission of proteinuria more frequently than supportive care alone.
Considerations on Corticosteroids Versus Supportive Care in Patients with Proteinuric IgAN after the STOP Trial
The supportive care adopted in the STOP Trial was very rigorous, multifocal, and protracted over a 6-month run-in phase aimed at optimizing BP and proteinuria control. A similar approach with good results was reported in unselected CKD.53 Results were impressive, because one third of patients lost the entering risk of progression criteria. The patients enrolled had a renal function decline of 1.6 ml/min per year only, which makes it difficult to prove the benefits of any additional treatment after a relatively short follow-up. Indeed, some of the differences in results from previous RCTs on the benefits of corticosteroids in IgAN are caused by a rapid decline of GFR in the control group26–28; this might have been improved by more severe supportive care, although a selection of scarcely progressive patients in the STOP Trial is possible, considering the inclusion criteria.
The STOP Trial enrolled patients with proteinuria <1 g/d who were likely not to benefit from the addition of corticosteroids to RASBs at least over the 3 years of the trial.50 Patients at very high risk with proteinuria >3.5 g/d or progressive loss of eGFR who, according to the KDIGO, may have had benefits from corticosteroids34 were excluded.
The two corticosteroid/immunosuppressive regimens were applied to two small groups of different patients; however, results were pooled according to trial design. In the corticosteroid monotherapy group, proteinuria at 1 year dropped largely below 1 g/d and remained stable until the third year, with full remission in 30% of the patients. Conversely, in the immunosuppressive combination therapy group, which included patients with eGFR<60 ml/min per 1.73 m2, proteinuria slightly decreased at 1 year but increased again above 1.2 g/d at the end of the follow-up. Only 11% of these patients went into full remission. The two groups, receiving two corticosteroid/immunosuppressive regimens, had different antiproteinuric responses, and the effects on eGFR decline on the long-term course are expected to be different. Remission of proteinuria <1 g/d predicted renal survival in the Toronto Registry54 over a follow-up of 15 years, which was not evident before 5 years. Similarly, in the VALIGA, the protective effect of proteinuria <0.5 g/d on the combined end point of 50% decline in eGFR and/or ESRD was detected after 10 years.50 Data analysis of the STOP Trial is further complicated by an unusual end point (i.e., a loss of eGFR of >15 ml/min per 1.73 m2; about 25% loss), which makes a direct comparison with previous reports impossible; anyway, some positive effects of corticosteroids in the monotherapy group may be expected after a follow-up lasting >3 years.
Remission of proteinuria is a recognized positive end point for IgAN as confirmed in recent reports.55–57 As commented in a letter to the New England Journal of Medicine,58 “the STOP-IgAN trial provided evidence that adding an aggressive immunosuppressive regimen to aggressive supportive therapies favours remission of proteinuria and microscopic haematuria, however at a high cost of infection—including one death for sepsis.” Recent meta-analyses confirmed the benefits of corticosteroids in reducing proteinuria and maintaining time-averaged proteinuria <1 g/d, regardless of the stage of CKD.57,59 However, the risk of major AEs increases in patients with impaired GFR when assuming azathioprine, even if this immunosuppression is not very aggressive.60
The STOP Trial did not consider the histopathology features and the time elapsed from renal biopsy and treatment. In the observational VALIGA, treatment was given at a median time of 3 months from renal biopsy. Apart from the MEST score, which was not available at the time of STOP Trial design, no data on the extent of irreversible chronic damage were reported. In a recent analysis of 901 patients followed for a median of 5.6 years,61 the value of combining MEST scores with clinical data at biopsy provided earlier risk prediction than what is currently considered the best predictor method on the basis of 2 years of follow-up data.62 In some cases, the value of pathology features indicated possible benefits of modification of treatment on the basis of personalized risk assessment. For instance, patients with M1 and proteinuria at biopsy <1 g/d had a high risk, like those recommended for corticosteroid therapy by the KDIGO, whereas patients without M and T lesions had low risk, even if proteinuria was 1–1.5 g/d, like those recommended for RASBs alone. A reanalysis of RCTs adopting the Oxford classification showed that E1 predicted a favorable response to corticosteroids.49 M1 and T1–T2 were independent predictors for the need of corticosteroid therapy in addition to RASBs.48 However, no study has been designed so far on baseline histopathology features.
New RCTs Just Finished and Reported at Congresses That Are about to Be Published
Some preliminary data from the Therapeutic Evaluation of Steroids in IgA Nephropathy (TESTING) Study have provided further evidence on benefits and side effects of corticosteroid treatment in patients with IgAN (ClinicalTrials.gov no. 01560052; ERA-EDTA 2016 abstract 3394). The TESTING Study involved 262 patients with IgAN, proteinuria >1 g/d, and eGFR=20–120 ml/min per 1.73 m2 randomized to 0.8 mg/kg per day oral methylprednisolone for 2 months, with weaning over 6–8 months. The RCT was discontinued after a median follow-up of 1.5 years because of excessive serious AEs, mostly infections, two of which were fatal. At the interim analysis, a significant benefit of corticosteroids was found compared with supportive therapy with optimized RASBs in 5.1% of treated patients versus 14.3% in the supportive care group (P=0.02); time-averaged proteinuria was significantly reduced in the corticosteroid arm (P>0.001). This stresses once more the association between reduction in proteinuria by corticosteroid and protective effect on kidney function. The conclusion of this study is that steroid therapy (at cumulative dose slightly higher than the KDIGO recommendation) was associated with a high frequency of serious AEs, although the interim analysis showed a benefit of corticosteroids on renal function decline and reduction of proteinuria.
Should we continue to expose patients with IgAN to the systemic effects of steroids in the future? The hypothesis of intestinal mucosal immunity involvement in the pathogenesis of IgAN63 suggested by clinical observations,64 experimental models,65,66 and GWAS studies67 offered the hypothesis of targeting corticosteroids to intestinal Peyer patches.64 The NEFIGAN Study, a phase 2b trial using enteric controlled release formulation of glucocorticoid budesonide for site–specific drug delivery at the ileocecal junction (ClinicalTrials.gov no. 01738035), was presented at the American Society of Nephrology 2015 Meeting. The primary end point of reduction in proteinuria after 9 months of treatment was met at interim analysis, and some protective effects on renal function decline compared with controls have been orally reported, although with some residual—theoretically unexpected—systemic steroid effects.
We look forward to seeing the full analysis from these studies.
Safety of Corticosteroids and Other Immunosuppressive Drugs in Treating Patients with IgAN
In a meta-analysis on 245 patients with IgAN treated with corticosteroids enrolled in nine RCTs, the incidence of severe AEs was 6.9% (mostly hypertension and diabetes and rarely, gastrointestinal bleeding).59 No direct comparison between AEs during oral versus intravenous treatment has been reported. In a recent meta-analysis on 325 patients treated with intravenous steroid pulses, the risk of AEs increased with decreasing eGFR from 2.3% in patients with mean eGFR of 90 ml/min per 1.73 m2 to 15.4% in those with 34 ml/min per 1.73 m2.57 The addition of immunosuppressants (usually azathioprine) increased the risk of AEs from 15% in the patients with preserved renal function to 30% in patients with eGFR<30 ml/min per 1.73 m2.
Summary and Conclusions
The benefit of corticosteroid therapy in slowing the progression of IgAN has been a matter of debate during the last months after the publication of RCTs and large cohort studies that provided new insights, sometimes conflicting, offering new hints for a constructive debate. Some statements of the 2012 KDIGO recommendations have been confirmed, and others have been rebutted. One cannot directly compare the results of RCTs with those from observational studies; however, it would be unwise not to take advantage of large cohort analysis. Observational studies do not suffer from patient selection at enrolment and when large enough, can compare subgroups of patients with very well selected baseline characteristics. However, only RCTs assure treatment prescription, doses and duration, and as far as possible, compliance.
The limitation of RCTs addressed to the most common form of slowly progressive IgAN is the difficulty of enrolment of patients who should have some chance of progression over the limited time of a RCT, while not belonging to the group of patients with truly high–risk, rapidly progressive cases. However, the enrolled subjects must have renal lesions potentially sensitive to the drug to be tested. Proteinuric patients are selected, because persistent proteinuria is the most accessible valuable biomarker of progression.54,56,57 However, proteinuria in IgAN can be the result of different pathologic processes. A crosstalk between mesangial cells and podocytes is responsible for podocitary changes and proteinuria,68,69 which may be reversible after corticosteroid/immunosuppressive treatment. However, non-nephrotic proteinuria can also be consequent to hemodynamic glomerular hyperfiltration and responsive to renin-angiotensin system inhibition only.70,71 Several factors are neglected in most RCTs: sclerosis in the previous biopsy, time elapsed from renal biopsy to therapy, persistence of proteinuria at least over the previous 6 months, and treatment in the years before, which may provide a late legacy effect.72 All recent studies suffer from follow-ups that are too short for a slowly progressive disease like IgAN.
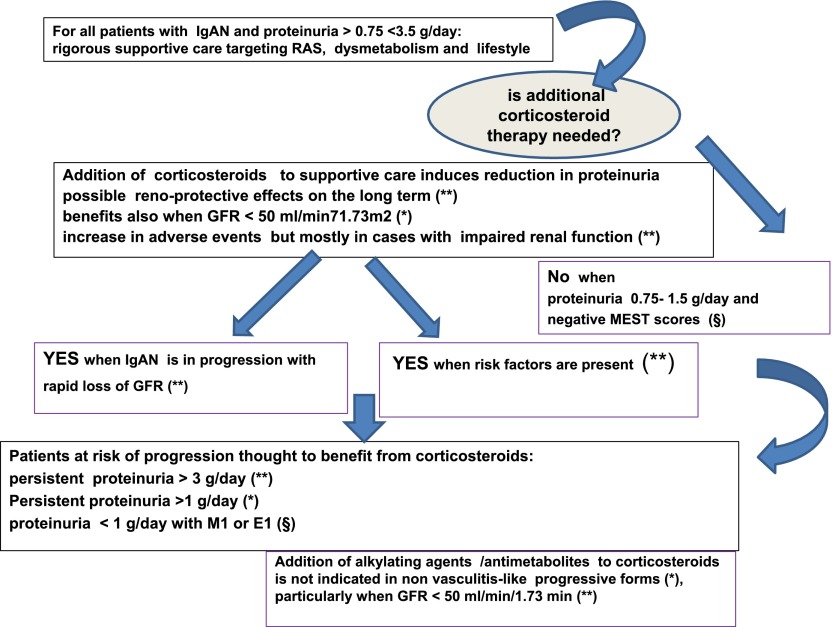
The following list is an attempt to find a clue of interpretation and agreement from results of recent studies on treatment of patients with IgAN (Figure 1).
Figure 1.
A proposed flow chart for treatment of IgAN on the basis of recent results from RCTs and large retrospective observational studies. RAS, renin-angiotensin system. *Consistent indication. **Strong indication. §Suggestion.
A protracted and rigorous supportive care, targeting RAS for BP and proteinuria, and multiple other metabolic and lifestyle targets can be of benefit in one third of patients with proteinuria >0.75 to <3.5 g/d and not at high risk of rapid progression (proteinuria <3.5 g/d, eGFR>30 ml/min per 1.73 m2, or eGFR decreased by <30% in the previous 6 months).52
Corticosteroids induced remission of proteinuria over 3 years more frequently than RASBs alone.52 After 3 years, no protection from 25% renal function decline was achieved in patients not at high risk.52
The correlations between reduction in follow-up proteinuria and reduction of loss of GFR are consistent in almost all cohort studies and RCTs.50,56 Hence, long-term benefits may be expected for corticosteroids in patients with GFR>60 ml/min who achieved mean proteinuria <1 g/d.50,54,56,57,59
Patients with eGFR<50 ml/min might have benefits from corticosteroid therapy51 but not with the association of alkylating drugs or antimetabolites, which increase the risk of AEs.57,60 Hence, this association in patients with impaired renal function is contraindicated.
Patients with persistent proteinuria >3 g/d may be protected from CKD progression when treated by corticosteroids in addition to RASBs.51
Corticosteroids added to RASBs may not provide additional benefits in patients with proteinuria 0.75–1.5 g/d in absence of mesangial hypercellularity or tubulointerstitial damage, at least at the follow-up analysis presently available.50,51,61
The following observations, strongly supported by observational studies, need confirmation from ad hoc designed RCTs.
Patients with proteinuria <1 g/d with mesangial hypercellularity (M1) may be at high risk of progression as patients meeting the present KDIGO recommendations and might benefit from corticosteroids.61 Patients with proteinuria <0.5 g/d with mesangial or endothelial hypercellularity (M1 or E1) may be at high risk of developing proteinuria >1–2 g/d and might benefit from early treatment.50,61
Histology in addition to proteinuria and eGFR at renal biopsy may help selecting patients likely to respond to corticosteroids, suggesting a need for new RCTs.61
The advice from recent studies is that it is time to design a trial for treatment with corticosteroids for patients with IgAN stratified for clinical and histologic data at renal biopsy. While looking for this future RCT, the clinician should consider that mesangial hypercellularity is a strong variable predicting progression and need of corticosteroids. Moreover, proteinuria should be considered in the light of coexisting irreversible sclerotic damage in respect to active mesangial and endocapillary lesions to give selective indications for corticotherapy to patients with potentially reversible proteinuria.
Disclosures
None.
Acknowledgments
Prof. Francesco Locatelli is greatly thanked for his thoughtful advice.
Footnotes
Published online ahead of print. Publication date available at www.jasn.org.
References
- 1.Wyatt RJ, Julian BA: IgA nephropathy. N Engl J Med 368: 2402–2414, 2013 [DOI] [PubMed] [Google Scholar]
- 2.Roberts IS: Pathology of IgA nephropathy. Nat Rev Nephrol 10: 445–454, 2014 [DOI] [PubMed] [Google Scholar]
- 3.Coppo R, D’Amico G: Factors predicting progression of IgA nephropathies. J Nephrol 18: 503–512, 2005 [PubMed] [Google Scholar]
- 4.Berthoux F, Mohey H, Laurent B, Mariat C, Afiani A, Thibaudin L: Predicting the risk for dialysis or death in IgA nephropathy. J Am Soc Nephrol 22: 752–761, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Shima Y, Nakanishi K, Hama T, Mukaiyama H, Togawa H, Sako M, Kaito H, Nozu K, Tanaka R, Iijima K, Yoshikawa N: Spontaneous remission in children with IgA nephropathy. Pediatr Nephrol 28: 71–76, 2013 [DOI] [PubMed] [Google Scholar]
- 6.Gutiérrez E, Zamora I, Ballarín JA, Arce Y, Jiménez S, Quereda C, Olea T, Martínez-Ara J, Segarra A, Bernis C, García A, Goicoechea M, García de Vinuesa S, Rojas-Rivera J, Praga M; Grupo de Estudio de Enfermedades Glomerulares de la Sociedad Española de Nefrología (GLOSEN) : Long-term outcomes of IgA nephropathy presenting with minimal or no proteinuria. J Am Soc Nephrol 23: 1753–1760, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee H, Hwang JH, Paik JH, Ryu HJ, Kim DK, Chin HJ, Oh YK, Joo KW, Lim CS, Kim YS, Lee JP: Long-term prognosis of clinically early IgA nephropathy is not always favorable. BMC Nephrol 15: 94, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tang Z, Wu Y, Wang QW, Yu YS, Hu WX, Yao XD, Chen HP, Liu ZH, Li LS: Idiopathic IgA nephropathy with diffuse crescent formation. Am J Nephrol 22: 480–486, 2002 [DOI] [PubMed] [Google Scholar]
- 9.Suzuki H, Kiryluk K, Novak J, Moldoveanu Z, Herr AB, Renfrow MB, Wyatt RJ, Scolari F, Mestecky J, Gharavi AG, Julian BA: The pathophysiology of IgA nephropathy. J Am Soc Nephrol 22: 1795–1803, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Moldoveanu Z, Wyatt RJ, Lee JY, Tomana M, Julian BA, Mestecky J, Huang WQ, Anreddy SR, Hall S, Hastings MC, Lau KK, Cook WJ, Novak J: Patients with IgA nephropathy have increased serum galactose-deficient IgA1 levels. Kidney Int 71: 1148–1154, 2007 [DOI] [PubMed] [Google Scholar]
- 11.Suzuki H, Fan R, Zhang Z, Brown R, Hall S, Julian BA, Chatham WW, Suzuki Y, Wyatt RJ, Moldoveanu Z, Lee JY, Robinson J, Tomana M, Tomino Y, Mestecky J, Novak J: Aberrantly glycosylated IgA1 in IgA nephropathy patients is recognized by IgG antibodies with restricted heterogeneity. J Clin Invest 119: 1668–1677, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Mestecky J, Raska M, Julian BA, Gharavi AG, Renfrow MB, Moldoveanu Z, Novak L, Matousovic K, Novak J: IgA nephropathy: Molecular mechanisms of the disease. Annu Rev Pathol 8: 217–240, 2013 [DOI] [PubMed] [Google Scholar]
- 13.Magistroni R, D’Agati VD, Appel GB, Kiryluk K: New developments in the genetics, pathogenesis, and therapy of IgA nephropathy. Kidney Int 88: 974–989, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hastings MC, Moldoveanu Z, Suzuki H, Berthoux F, Julian BA, Sanders JT, Renfrow MB, Novak J, Wyatt RJ: Biomarkers in IgA nephropathy: Relationship to pathogenetic hits. Expert Opin Med Diagn 7: 615–627, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Coppo R: Biomarkers and targeted new therapies for IgA nephropathy [published online ahead of print June 20, 2016]. Pediatr Nephrol [DOI] [PubMed] [Google Scholar]
- 16.Kobayashi Y, Fujii K, Hiki Y, Tateno S: Steroid therapy in IgA nephropathy: A prospective pilot study in moderate proteinuric cases. Q J Med 61: 935–943, 1986 [PubMed] [Google Scholar]
- 17.Kobayashi Y, Hiki Y, Fujii K, Kurokawa A, Kamiyama M, Tateno S: Effect of corticosteroids on renal function in progressive IgA nephropathy--long-term follow-up study. Nippon Jinzo Gakkai Shi 30: 1135–1142, 1988 [PubMed] [Google Scholar]
- 18.Vaerman JP: The secretory immune system. Antibiot Chemother (1971) 39: 41–50, 1987 [PubMed] [Google Scholar]
- 19.Russell MW, Reinholdt J, Kilian M: Anti-inflammatory activity of human IgA antibodies and their Fab alpha fragments: Inhibition of IgG-mediated complement activation. Eur J Immunol 19: 2243–2249, 1989 [DOI] [PubMed] [Google Scholar]
- 20.Reterink TJ, Schroeijers WE, Es LA, Daha MR: Dimeric and polymeric IgA, but not monomeric IgA, enhance the production of IL-6 by human renal mesangial cells. Mediators Inflamm 5: 191–195, 1996 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Coppo R, Amore A: Aberrant glycosylation in IgA nephropathy (IgAN). Kidney Int 65: 1544–1547, 2004 [DOI] [PubMed] [Google Scholar]
- 22.Leung JC, Tang SC, Chan LY, Chan WL, Lai KN: Synthesis of TNF-alpha by mesangial cells cultured with polymeric anionic IgA--role of MAPK and NF-kappaB. Nephrol Dial Transplant 23: 72–81, 2008 [DOI] [PubMed] [Google Scholar]
- 23.Lai AS, Lai KN: Molecular basis of IgA nephropathy. Curr Mol Med 5: 475–487, 2005 [DOI] [PubMed] [Google Scholar]
- 24.Yanagihara T, Brown R, Hall S, Moldoveanu Z, Goepfert A, Tomana M, Julian BA, Mestecky J, Novak J: In vitro-generated immune complexes containing galactose-deficient IgA1 stimulate proliferation of mesangial cells. Results Immunol 2: 166–172, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pabst O: New concepts in the generation and functions of IgA. Nat Rev Immunol 12: 821–832, 2012 [DOI] [PubMed] [Google Scholar]
- 26.Pozzi C, Bolasco PG, Fogazzi GB, Andrulli S, Altieri P, Ponticelli C, Locatelli F: Corticosteroids in IgA nephropathy: A randomised controlled trial. Lancet 353: 883–887, 1999 [DOI] [PubMed] [Google Scholar]
- 27.Manno C, Torres DD, Rossini M, Pesce F, Schena FP: Randomized controlled clinical trial of corticosteroids plus ACE-inhibitors with long-term follow-up in proteinuric IgA nephropathy. Nephrol Dial Transplant 24: 3694–3701, 2009 [DOI] [PubMed] [Google Scholar]
- 28.Lv J, Zhang H, Chen Y, Li G, Jiang L, Singh AK, Wang H: Combination therapy of prednisone and ACE inhibitor versus ACE-inhibitor therapy alone in patients with IgA nephropathy: A randomized controlled trial. Am J Kidney Dis 53: 26–32, 2009 [DOI] [PubMed] [Google Scholar]
- 29.Jafar TH, Stark PC, Schmid CH, Landa M, Maschio G, de Jong PE, de Zeeuw D, Shahinfar S, Toto R, Levey AS; AIPRD Study Group : Progression of chronic kidney disease: The role of blood pressure control, proteinuria, and angiotensin-converting enzyme inhibition: A patient-level meta-analysis. Ann Intern Med 139: 244–252, 2003 [DOI] [PubMed] [Google Scholar]
- 30.Lai KN, Chan LY, Tang SC, Tsang AW, Li FF, Lam MF, Lui SL, Leung JC: Mesangial expression of angiotensin II receptor in IgA nephropathy and its regulation by polymeric IgA1. Kidney Int 66: 1403–1416, 2004 [DOI] [PubMed] [Google Scholar]
- 31.Praga M, Gutiérrez E, González E, Morales E, Hernández E: Treatment of IgA nephropathy with ACE inhibitors: A randomized and controlled trial. J Am Soc Nephrol 14: 1578–1583, 2003 [DOI] [PubMed] [Google Scholar]
- 32.Coppo R, Peruzzi L, Amore A, Piccoli A, Cochat P, Stone R, Kirschstein M, Linné T: IgACE: A placebo-controlled, randomized trial of angiotensin-converting enzyme inhibitors in children and young people with IgA nephropathy and moderate proteinuria. J Am Soc Nephrol 18: 1880–1888, 2007 [DOI] [PubMed] [Google Scholar]
- 33.Li PK, Leung CB, Chow KM, Cheng YL, Fung SK, Mak SK, Tang AW, Wong TY, Yung CY, Yung JC, Yu AW, Szeto CC; HKVIN Study Group : Hong Kong study using valsartan in IgA nephropathy (HKVIN): A double-blind, randomized, placebo-controlled study. Am J Kidney Dis 47: 751–760, 2006 [DOI] [PubMed] [Google Scholar]
- 34.Kidney Disease: Improving Global Outcomes (KDIGO) Glomerulonephritis Work Group : KDIGO Clinical Practice Guideline for Glomerulonephritis. Immunoglobulin A nephropathy. Kidney Int Suppl 2: 139–274, 2012 [Google Scholar]
- 35.Pozzi C, Andrulli S, Del Vecchio L, Melis P, Fogazzi GB, Altieri P, Ponticelli C, Locatelli F: Corticosteroid effectiveness in IgA nephropathy: Long-term results of a randomized, controlled trial. J Am Soc Nephrol 15: 157–163, 2004 [DOI] [PubMed] [Google Scholar]
- 36.Ballardie FW, Roberts IS: Controlled prospective trial of prednisolone and cytotoxics in progressive IgA nephropathy. J Am Soc Nephrol 13: 142–148, 2002 [DOI] [PubMed] [Google Scholar]
- 37.Tumlin JA, Lohavichan V, Hennigar R: Crescentic, proliferative IgA nephropathy: Clinical and histological response to methylprednisolone and intravenous cyclophosphamide. Nephrol Dial Transplant 18: 1321–1329, 2003 [DOI] [PubMed] [Google Scholar]
- 38.Vecchio M, Bonerba B, Palmer SC, Craig JC, Ruospo M, Samuels JA, Molony DA, Schena FP, Strippoli GF: Immunosuppressive agents for treating IgA nephropathy. Cochrane Database Syst Rev 3: CD003965, 2015 [DOI] [PubMed] [Google Scholar]
- 39.Pozzi C, Andrulli S, Pani A, Scaini P, Del Vecchio L, Fogazzi G, Vogt B, De Cristofaro V, Allegri L, Cirami L, Procaccini AD, Locatelli F: Addition of azathioprine to corticosteroids does not benefit patients with IgA nephropathy. J Am Soc Nephrol 21: 1783–1790, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Eitner F, Floege J: Glomerular disease: ACEIs with or without corticosteroids in IgA nephropathy? Nat Rev Nephrol 6: 252–254, 2010 [DOI] [PubMed] [Google Scholar]
- 41.Roberts IS, Cook HT, Troyanov S, Alpers CE, Amore A, Barratt J, Berthoux F, Bonsib S, Bruijn JA, Cattran DC, Coppo R, D’Agati V, D’Amico G, Emancipator S, Emma F, Feehally J, Ferrario F, Fervenza FC, Florquin S, Fogo A, Geddes CC, Groene HJ, Haas M, Herzenberg AM, Hill PA, Hogg RJ, Hsu SI, Jennette JC, Joh K, Julian BA, Kawamura T, Lai FM, Li LS, Li PK, Liu ZH, Mackinnon B, Mezzano S, Schena FP, Tomino Y, Walker PD, Wang H, Weening JJ, Yoshikawa N, Zhang H; Working Group of the International IgA Nephropathy Network and the Renal Pathology Society : The Oxford classification of IgA nephropathy: Pathology definitions, correlations, and reproducibility. Kidney Int 76: 546–556, 2009 [DOI] [PubMed] [Google Scholar]
- 42.Cattran DC, Coppo R, Cook HT, Feehally J, Roberts IS, Troyanov S, Alpers CE, Amore A, Barratt J, Berthoux F, Bonsib S, Bruijn JA, D’Agati V, D’Amico G, Emancipator S, Emma F, Ferrario F, Fervenza FC, Florquin S, Fogo A, Geddes CC, Groene HJ, Haas M, Herzenberg AM, Hill PA, Hogg RJ, Hsu SI, Jennette JC, Joh K, Julian BA, Kawamura T, Lai FM, Leung CB, Li LS, Li PK, Liu ZH, Mackinnon B, Mezzano S, Schena FP, Tomino Y, Walker PD, Wang H, Weening JJ, Yoshikawa N, Zhang H; Working Group of the International IgA Nephropathy Network and the Renal Pathology Society : The Oxford classification of IgA nephropathy: Rationale, clinicopathological correlations, and classification. Kidney Int 76: 534–545, 2009 [DOI] [PubMed] [Google Scholar]
- 43.Herzenberg AM, Fogo AB, Reich HN, Troyanov S, Bavbek N, Massat AE, Hunley TE, Hladunewich MA, Julian BA, Fervenza FC, Cattran DC: Validation of the Oxford classification of IgA nephropathy. Kidney Int 80: 310–317, 2011 [DOI] [PubMed] [Google Scholar]
- 44.Yau T, Korbet SM, Schwartz MM, Cimbaluk DJ: The Oxford classification of IgA nephropathy: A retrospective analysis. Am J Nephrol 34: 435–444, 2011 [DOI] [PubMed] [Google Scholar]
- 45.Alamartine E, Sauron C, Laurent B, Sury A, Seffert A, Mariat C: The use of the Oxford classification of IgA nephropathy to predict renal survival. Clin J Am Soc Nephrol 6: 2384–2388, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Zeng CH, Le W, Ni Z, Zhang M, Miao L, Luo P, Wang R, Lv Z, Chen J, Tian J, Chen N, Pan X, Fu P, Hu Z, Wang L, Fan Q, Zheng H, Zhang D, Wang Y, Huo Y, Lin H, Chen S, Sun S, Wang Y, Liu Z, Liu D, Ma L, Pan T, Zhang A, Jiang X, Xing C, Sun B, Zhou Q, Tang W, Liu F, Liu Y, Liang S, Xu F, Huang Q, Shen H, Wang J, Shyr Y, Phillips S, Troyanov S, Fogo A, Liu ZH: A multicenter application and evaluation of the oxford classification of IgA nephropathy in adult chinese patients. Am J Kidney Dis 60: 812–820, 2012 [DOI] [PubMed] [Google Scholar]
- 47.Katafuchi R, Ninomiya T, Nagata M, Mitsuiki K, Hirakata H: Validation study of oxford classification of IgA nephropathy: The significance of extracapillary proliferation. Clin J Am Soc Nephrol 6: 2806–2813, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Shi SF, Wang SX, Jiang L, Lv JC, Liu LJ, Chen YQ, Zhu SN, Liu G, Zou WZ, Zhang H, Wang HY: Pathologic predictors of renal outcome and therapeutic efficacy in IgA nephropathy: Validation of the Oxford classification. Clin J Am Soc Nephrol 6: 2175–2184, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Lv J, Shi S, Xu D, Zhang H, Troyanov S, Cattran DC, Wang H: Evaluation of the Oxford Classification of IgA nephropathy: A systematic review and meta-analysis. Am J Kidney Dis 62: 891–899, 2013 [DOI] [PubMed] [Google Scholar]
- 50.Coppo R, Troyanov S, Bellur S, Cattran D, Cook HT, Feehally J, Roberts IS, Morando L, Camilla R, Tesar V, Lunberg S, Gesualdo L, Emma F, Rollino C, Amore A, Praga M, Feriozzi S, Segoloni G, Pani A, Cancarini G, Durlik M, Moggia E, Mazzucco G, Giannakakis C, Honsova E, Sundelin BB, Di Palma AM, Ferrario F, Gutierrez E, Asunis AM, Barratt J, Tardanico R, Perkowska-Ptasinska A; VALIGA study of the ERA-EDTA Immunonephrology Working Group : Validation of the Oxford classification of IgA nephropathy in cohorts with different presentations and treatments. Kidney Int 86: 828–836, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tesar V, Troyanov S, Bellur S, Verhave JC, Cook HT, Feehally J, Roberts IS, Cattran D, Coppo R; VALIGA study of the ERA-EDTA Immunonephrology Working Group : Corticosteroids in IgA nephropathy: A retrospective analysis from the VALIGA Study. J Am Soc Nephrol 26: 2248–2258, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Rauen T, Eitner F, Fitzner C, Sommerer C, Zeier M, Otte B, Panzer U, Peters H, Benck U, Mertens PR, Kuhlmann U, Witzke O, Gross O, Vielhauer V, Mann JF, Hilgers RD, Floege J; STOP-IgAN Investigators : Intensive supportive care plus immunosuppression in IgA nephropathy. N Engl J Med 373: 2225–2236, 2015 [DOI] [PubMed] [Google Scholar]
- 53.Ruggenenti P, Perticucci E, Cravedi P, Gambara V, Costantini M, Sharma SK, Perna A, Remuzzi G: Role of remission clinics in the longitudinal treatment of CKD. J Am Soc Nephrol 19: 1213–1224, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Reich HN, Troyanov S, Scholey JW, Cattran DC; Toronto Glomerulonephritis Registry : Remission of proteinuria improves prognosis in IgA nephropathy. J Am Soc Nephrol 18: 3177–3183, 2007 [DOI] [PubMed] [Google Scholar]
- 55.Nam KH, Kie JH, Lee MJ, Chang TI, Kang EW, Kim DW, Lim BJ, Park JT, Kwon YE, Kim YL, Park KS, An SY, Oh HJ, Yoo TH, Kang SW, Choi KH, Jeong HJ, Han DS, Han SH: Optimal proteinuria target for renoprotection in patients with IgA nephropathy. PLoS One 9: e101935, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Inker LA, Mondal H, Greene T, Masaschi T, Locatelli F, Schena FP, Katafuchi R, Appel GB, Maes BD, Li PK, Praga M, Del Vecchio L, Andrulli S, Manno C, Gutierrez E, Mercer A, Carroll KJ, Schmid CH, Levey AS: Early change in urine protein as a surrogate end point in studies of IgA nephropathy: An individual-patient meta-analysis [published online ahead of print March 29, 2016]. Am J Kidney Dis doi:10.1053/j.ajkd.2016.02.042 [DOI] [PubMed]
- 57.Sarcina C, Tinelli C, Ferrario F, Pani A, De Silvestri A, Scaini P, Del Vecchio L, Alberghini E, Buzzi L, Baragetti I, Pozzi C: Changes in proteinuria and side effects of corticosteroids alone or in combination with azathioprine at different stages of IgA nephropathy. Clin J Am Soc Nephrol 11: 973–981, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Ayoub I, Hebert L, Rovin BH: Intensive supportive care plus immunosuppression in IgA nephropathy. N Engl J Med 374: 991–992, 2016 [DOI] [PubMed] [Google Scholar]
- 59.Lv J, Xu D, Perkovic V, Ma X, Johnson DW, Woodward M, Levin A, Zhang H, Wang H; TESTING Study Group : Corticosteroid therapy in IgA nephropathy. J Am Soc Nephrol 23: 1108–1116, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Pozzi C, Andrulli S, Pani A, Scaini P, Roccatello D, Fogazzi G, Pecchini P, Rustichelli R, Finocchiaro P, Del Vecchio L, Locatelli F: IgA nephropathy with severe chronic renal failure: A randomized controlled trial of corticosteroids and azathioprine. J Nephrol 26: 86–93, 2013 [DOI] [PubMed] [Google Scholar]
- 61.Barbour SJ, Espino-Hernandez G, Reich HN, Coppo R, Roberts IS, Feehally J, Herzenberg AM, Cattran DC; Oxford Derivation, North American Validation and VALIGA Consortia; Oxford Derivation North American Validation and VALIGA Consortia : The MEST score provides earlier risk prediction in IgA nephropathy. Kidney Int 89: 167–175, 2016 [DOI] [PubMed] [Google Scholar]
- 62.Bartosik LP, Lajoie G, Sugar L, Cattran DC: Predicting progression in IgA nephropathy. Am J Kidney Dis 38: 728–735, 2001 [DOI] [PubMed] [Google Scholar]
- 63.Coppo R: The intestine-renal connection in IgA nephropathy. Nephrol Dial Transplant 30: 360–366, 2015 [DOI] [PubMed] [Google Scholar]
- 64.Smerud HK, Bárány P, Lindström K, Fernström A, Sandell A, Påhlsson P, Fellström B: New treatment for IgA nephropathy: Enteric budesonide targeted to the ileocecal region ameliorates proteinuria. Nephrol Dial Transplant 26: 3237–3242, 2011 [DOI] [PubMed] [Google Scholar]
- 65.Papista C, Lechner S, Ben Mkaddem S, LeStang MB, Abbad L, Bex-Coudrat J, Pillebout E, Chemouny JM, Jablonski M, Flamant M, Daugas E, Vrtovsnik F, Yiangou M, Berthelot L, Monteiro RC: Gluten exacerbates IgA nephropathy in humanized mice through gliadin-CD89 interaction. Kidney Int 88: 276–285, 2015 [DOI] [PubMed] [Google Scholar]
- 66.McCarthy DD, Kujawa J, Wilson C, Papandile A, Poreci U, Porfilio EA, Ward L, Lawson MA, Macpherson AJ, McCoy KD, Pei Y, Novak L, Lee JY, Julian BA, Novak J, Ranger A, Gommerman JL, Browning JL: Mice overexpressing BAFF develop a commensal flora-dependent, IgA-associated nephropathy. J Clin Invest 121: 3991–4002, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kiryluk K, Li Y, Scolari F, Sanna-Cherchi S, Choi M, Verbitsky M, Fasel D, Lata S, Prakash S, Shapiro S, Fischman C, Snyder HJ, Appel G, Izzi C, Viola BF, Dallera N, Del Vecchio L, Barlassina C, Salvi E, Bertinetto FE, Amoroso A, Savoldi S, Rocchietti M, Amore A, Peruzzi L, Coppo R, Salvadori M, Ravani P, Magistroni R, Ghiggeri GM, Caridi G, Bodria M, Lugani F, Allegri L, Delsante M, Maiorana M, Magnano A, Frasca G, Boer E, Boscutti G, Ponticelli C, Mignani R, Marcantoni C, Di Landro D, Santoro D, Pani A, Polci R, Feriozzi S, Chicca S, Galliani M, Gigante M, Gesualdo L, Zamboli P, Battaglia GG, Garozzo M, Maixnerová D, Tesar V, Eitner F, Rauen T, Floege J, Kovacs T, Nagy J, Mucha K, Pączek L, Zaniew M, Mizerska-Wasiak M, Roszkowska-Blaim M, Pawlaczyk K, Gale D, Barratt J, Thibaudin L, Berthoux F, Canaud G, Boland A, Metzger M, Panzer U, Suzuki H, Goto S, Narita I, Caliskan Y, Xie J, Hou P, Chen N, Zhang H, Wyatt RJ, Novak J, Julian BA, Feehally J, Stengel B, Cusi D, Lifton RP, Gharavi AG: Discovery of new risk loci for IgA nephropathy implicates genes involved in immunity against intestinal pathogens. Nat Genet 46: 1187–1196, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Lai KN, Leung JC, Chan LY, Saleem MA, Mathieson PW, Tam KY, Xiao J, Lai FM, Tang SC: Podocyte injury induced by mesangial-derived cytokines in IgA nephropathy. Nephrol Dial Transplant 24: 62–72, 2009 [DOI] [PubMed] [Google Scholar]
- 69.Coppo R, Fonsato V, Balegno S, Ricotti E, Loiacono E, Camilla R, Peruzzi L, Amore A, Bussolati B, Camussi G: Aberrantly glycosylated IgA1 induces mesangial cells to produce platelet-activating factor that mediates nephrin loss in cultured podocytes. Kidney Int 77: 417–427, 2010 [DOI] [PubMed] [Google Scholar]
- 70.Cravedi P, Remuzzi G: Pathophysiology of proteinuria and its value as an outcome measure in chronic kidney disease. Br J Clin Pharmacol 76: 516–523, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Woo KT, Lau YK: Proteinuria: Clinical significance and basis for therapy. Singapore Med J 42: 385–389, 2001 [PubMed] [Google Scholar]
- 72.Coppo R: Is a legacy effect possible in IgA nephropathy? Nephrol Dial Transplant 28: 1657–1662, 2013 [DOI] [PubMed] [Google Scholar]