Abstract
Introduction
In the light of the advances in treatment measures and early discharge of patients with mental disorders from psychiatric hospitals, families play important role in caring for such patients.
Aim
The aim of this study is to determine the Quality of Life (QoL) of the family caregivers of patients with mental disorders.
Materials and Methods
This cross-sectional study was conducted in teaching health care centers affiliated with medical universities in Tehran, Iran. Sampling was conducted by convenience random technique. Participants were 238 family caregivers of mental disorder patients and the Short-Form Health Survey Questionnaire was used to gather data. The data were analyzed by Spearman’s correlation, t-test and ANOVA in SPSS 18.0.
Results
The women’s mean QoL was lower than the men’s. Regarding family relationship with the patients, the lowest QoL was observed among the mothers. There was a significant relationship between the caregivers QoL and economic status, the caregivers gender, family relationship with the patients and the patients’ gender (p<0.05).
Conclusion
The caregivers of mental disorder patients have lower QoL compared with general population. Appropriately developed plans should be implemented to improve QoL among the family caregivers of these patients.
Keywords: Psychiatric disorders, Caregivers health, Psychiatric patients
Introduction
Each year, almost 60 million people, almost equal to 25% of all adults, in the United States are diagnosed with mental disorders [1]. The prevalence of mental disorders has been reported to be about 10.81% in Iran [2]. In a systematic review, the overall prevalence of Major Depressive Disorder (MDD) was estimated to be 4.1% and women were 1.95 times more likely to have MDD [3]. Because of advances in treatment measures including pharmaceutical arrangements, mentally disordered patients are currently discharged earlier than before [1]. De-institutionalization and community-based care of psychiatric patients has led to a greater emphasis on family management in the community. Family members are often overwhelmed by the demands due to caring for patients with mental disorder [3,4]. Mental illness is a chronic disease that causes considerable stress in family members, which in turn will cause disturbance of Quality of Life (QoL), decline in mental and physical health and family dysfunction [5]. The occupational life of these patients’ family members is often characterized by certain problems such as job change, change in working hours and job quitting [6]. Zendjidjian et al., reported that QoL of the caregivers of patients with mood disorders was lower than the general population [7,8]. Negative experiences of the caregivers limit their ability to carry out their activities and influence their ability to care for the patients. They show high depression, anxiety and psychosomatic symptoms. Maintenance of the caregivers health is important for two reasons: 1) The caregivers own life; and 2) possible impacts on the patients’ health. Addressing the caregivers’ problems, it is necessary to provide appropriate treatment, continuous caring and social support for the patients [6].
Considering the increasing demand for family caregivers, their QoL, must be considered a variable in studies on the family caregivers patients with chronic disease [8]. One of the concepts that have been considered identical to the welfare and health is QoL that puts emphasis on the patient’s and families’ mental perspectives and therefore can be useful to provide better health for the patients [1,6,9,10]. Negative experiences, lack of social support, physical and emotional stress and financial problems cause change in the QoL of informal caregivers [11]. The QoL definition differs depending on the cultural characteristics and values, goals, expectations and standards [6] and includes an evaluation of physical health, mental status, autonomy level, social relationships, spiritual interests [12–14] and on the whole, feeling healthy [11,15]. Despite the fact that family plays a fundamental role in supporting patients and is the most valuable source of help for the disabled patients, most of the studies have emphasized on the patient and the illness. However, the caregiver’s relatives should be considered, as well [8]. In a professional relationship with the patients and their family caregivers, the researchers may encounter various problems including stress, anxiety and frequent relapse of mental disorders that can cause negative effects on all dimensions of the caregivers life, especially QoL. Considering the importance of benefiting from desirable QoL in maintenance and promotion of the individual, family and community health, recent increase in the number of mentally disordered patients that threatens their main caregivers’ health, and that many studies that have been undertaken so far investigated the QoL but few of them have investigated mentally disordered patients’ family caregivers [16]. This study was conducted to determine the QoL and the relevant subscales in the family caregivers of patients with mental disorders.
Materials and Methods
Participants
The present study is a descriptive-analytical study conducted from December, 2013 to February, 2014. The study population consisted of all the caregivers and their patients referring to six psychiatric clinics or health care centers in Tehran, Iran. The inclusion criteria were at least six months passing since the illness diagnosis of the family member and caring for him/her for at least six months; having 18-65 years of age; not suffering from a physical or mental chronic disease; no severe stress due to a loved one’s death or divorce; and caring for only one patient. The people who were involved as assistants to family caregivers were excluded because of not being the main caregivers. In addition, participants who did not respond to the questions of demographic characteristics or QoL completely were excluded from the study.
Materials
In this study, the patients were selected by convenience, random sampling, matched for gender and age and enrolled in the study if they met the inclusion criteria. Randomization code was developed with a computer random-number generator. The sample size enrolled from psychiatric clinics or health care centers, affiliated with medical universities of Tehran (one center), Iran (two centers), and Shahid Beheshti (two centers) and University of Social Welfare and Rehabilitation Sciences (one center), was decided to be 97, 47, 48, and 47, respectively, according to the mean number of referrals during six months and the formula below, to obtain significant correlation coefficients:
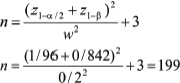 |
where α =0.05 (confidence interval 0.95), β = 0.02 (test power 80%), and W = 0.2 (correlation coefficient between resiliency and QoL). The data were collected from six psychiatric hospitals, clinics and psychiatric departments in Tehran.
Procedures
Data were gathered by the Personal Information Form (PIF) and the Short-Form Health Survey Questionnaire (SF-36). The participants responded to 11 questions of demographic characteristics including age, gender, family relationship with the patient, marital status, education level, employment status, economic status, number of family members, patient’s gender, care duration and illness diagnosis. The SF-36 is a general tool to measure the health status and QoL among both healthy and patient populations [17]. The Persian version of the SF-36 questionnaire, for measurement of the QoL with regard to health, consists of 36 questions on Physical (PCS) and Mental (MCS) Component Summary and eight subscales of health as follows: PCS consisting of subscales of Physical Functioning (PF), role limitation physical problems, bodily pain, general health and MCS consisting of subscales of vitality, social functioning, role limitation emotional problems and mental health. The questions were responded by two (Yes, No) to six choices: “at all times”, “most of the time”, “frequently”, “often”, “sometimes” and “never”. Scores of each subscale vary from 0 to 100, indicating the worst and the best status of the subscale, respectively. The score of each subscale is separately determined by the total score of that dimension and averaged. The obtained score is indicative of the health percentage in that dimension. To calculate the total score, the sum of the scores obtained for each subscale is divided by eight so that the obtained figure must be a number between 100 and 0. The validity and reliability of the QoL questionnaire have been confirmed for Iranian population and its subscales’ internal consistency coefficients have been obtained 0.70-0.79 and the test-retest coefficients with one-week interval have been reported to be 0.43-0.79 [18,19]. The researcher started the study after the approval of the ethics committee of the university (the code 92/s/130/2395) was provided. The participants filled out the written informed consent for participation in the study and were informed about the purpose of the study, the fact that declining to participate in the study would have no adverse effect on their use of services and the confidentiality of the data throughout the investigation process and the final reporting. Besides that, the centers’ officials were assured of being timely informed about the study results.
The researcher referred to the psychiatric hospitals, departments and clinics on different days of the week and gathered the required data using non-random accessible sampling and collected the questionnaires on the same day. The questionnaires were completed by the caregivers and if the caregivers were illiterate, the questions were read by the researcher, the caregivers responded to them and the researcher recorded the answers. The researcher did his best to read the questions in an unbiased manner.
Statistical Analysis
The data were analyzed by Spearman’s correlation coefficient, t-test and ANOVA in SPSS 18.0. Normal distribution of the data was investigated by Kolmogorov–Smirnov test. The p<0.05 was considered to be the level of significance.
Results
The findings showed that 72.3% of the caregivers were female, 76% married, 58.3% housewives and 49.8% lived in families with four to five members. Of the caregivers, 53.2% were engaged in caring for the patients for less than five years. The mean duration of caring for the patients was 7.84±2.96 years. Of the family caregivers, 41.2% were mothers and the rest first degree relatives of the patients. Of the patients, 50.5% were suffering from bipolar disorder. The mean age of the patients was 45.2±12.3 years. Of the caregivers, 68.5% had education levels of high school and lower and the rest academic education and 57.2% reported their financial status to be moderate. The number of the caregivers’ family members was 2-9 [Table/Fig-1].
[Table/Fig-1]:
Frequency distribution of demographic and background characteristics of family caregivers.
| Variable | Number * | % | |
|---|---|---|---|
| Age (year) | Lower than 31 | 33 | 14 |
| 31-40 | 44 | 18.6 | |
| 41-50 | 58 | 24.6 | |
| 51-60 | 63 | 26.7 | |
| Above 61 | 38 | 16.1 | |
| Gender | Female | 172 | 72.3 |
| Male | 66 | 27.7 | |
| Marital status | Single | 28 | 11.8 |
| Married | 180 | 76 | |
| Divorced | 11 | 4.6 | |
| Widow/widower | 18 | 7.6 | |
| Education | Illiterate | 29 | 12.2 |
| High school completion and lower education | 163 | 68.5 | |
| University | 46 | 19.3 | |
| Relative with patient | Father | 18 | 7.6 |
| Mother | 98 | 41.2 | |
| Spouse | 77 | 32.4 | |
| Children | 26 | 10.9 | |
| Sister | 12 | 5 | |
| Brother | 7 | 2.9 | |
| Employment status | Housewife | 136 | 58.3 |
| Employee | 24 | 10.3 | |
| Self-employed | 36 | 15.5 | |
| Unemployed | 14 | 6 | |
| Retired | 23 | 9.9 | |
| Economic status | Good (higher than 1,000 $ per month) | 11 | 4.6 |
| Average (between 500 and 1000 $ per month) | 136 | 57.2 | |
| Weak (under 500 $ per mounth | 91 | 38.2 | |
| Number of family members | 2-3 | 92 | 38.8 |
| 4-5 | 118 | 49.8 | |
| 6 and above | 27 | 11.4 | |
| Sex of patient | Female | 105 | 44.1 |
| Male | 133 | 55.9 | |
| Mental disorder | Schizophrenia | 35 | 16.8 |
| Bipolar | 105 | 50.5 | |
| Depression | 35 | 16.8 | |
| Substance Abuse | 12 | 5.8 | |
| Schizoaffective | 9 | 4.3 | |
| Other | 12 | 5.8 | |
| Care duration (year) | 0-4 | 126 | 53.2 |
| 5-9 | 59 | 24.9 | |
| 10-14 | 20 | 8.4 | |
| 15-19 | 17 | 7.2 | |
| Above 20 | 15 | 6.3 | |
*Some participants did not fill out the questionnaires completely. Therefore, we have missing data.
The mean QoL of the caregivers of the patients was 56.73±19.18%, mean PCS 58.50±20.43% and mean MCS 54.91±21.73%. Out of the subscales, the highest mean score was obtained for PF (70.44 ±24.43) and the lowest for role limitation physical problems (45±36.74). The mean QoL of the women and men was 54.55 and 62.73, respectively. The highest mean QoL (65.31±20.75) was obtained among the family caregivers of patients with other disorders (anxiety, obsession, personality disorder, delusional disorder, and judgment disorder) and the lowest mean QoL (49.37±12.66) among the caregivers of patients with substance use disorders. Regarding family relationships with the patients, the highest QoL was obtained for the children (65.28±23.03) and the lowest for the mothers (53.08±17.52). Regarding marital status, the single obtained the highest score (61.83±23.76) followed by the married (57.19±17.78), the widows/widowers (52.36±12.66) and the divorced (45.53±16.94). The QoL of the caregivers who cared for female patients (61.06±0.49) was higher than those caring for male patients (53.53±17.44). Comparison of different subscales of QoL showed a statistically significant difference between women and men in PF, bodily pain, general health, vitality and mental health [Table/Fig-2].
[Table/Fig-2]:
Comparison of quality of life in family caregivers for gender and quality of life in general population in Iran.
| Subscales | Female (n=172) | Male (n=66) | Total mean | General Population standard | p-value |
|---|---|---|---|---|---|
| Mean (Standard deviation) | Mean (Standard deviation) | Mean (Standard deviation) | Mean (Standard deviation) | ||
| Physical functioning | 66.58 ± 24.50 | 80.75 ± 20.99 | 70.44 ± 24.43 | 85.3 ± 20.8 | p<0.0001 |
| Role limitation physical problems | 42.75 ± 35.18 | 51.53 ± 39.98 | 45 ± 36.74 | 70 ± 38 | 0.123 |
| Bodily pain | 57.45 ± 29.56 | 67 ± 30.33 | 59.95 ± 30.05 | 79.4 ± 25.1 | 0.028 |
| General health | 56.01 ± 18.56 | 64.16 ± 16.51 | 58.31 ± 18.30 | 67.5 ± 20.4 | 0.002 |
| Vitality | 54.29 ± 20.72 | 61.30 ± 24.22 | 56.12 ± 21.94 | 65.8 ± 17.3 | 0.028 |
| Social functioning | 57.96 ± 25.89 | 64.77 ± 28.74 | 59.82 ± 26.78 | 76 ± 24.4 | 0.080 |
| Role limitation emotional problems | 46.27 ± 37.71 | 54.16 ± 37.79 | 48.36 ± 37.75 | 65.6 ± 41.4 | 0.155 |
| Mental health | 54.29 ± 22.66 | 63.03 ± 22.13 | 56.66 ± 22.80 | 67 ± 18 | 0.008 |
The data on age, care duration and number of family members were not normally distributed, therefore the Spearman’s correlation coefficient was used for statistical analysis. Spearman’s correlation coefficient, t-test and ANOVA indicated no significant relationship between the caregivers’ QoL and the variables age, education level, employment status, number of family members, marital status, duration of caring for the patient and diagnosis. In addition, there was a significant relationship between the QoL and the caregivers’ financial status p<0.0001), the caregivers’ gender (p=0.004), the caregivers’ family relationships with the patient (p=0.027) and the patients’ gender (p=0.004) [Table/Fig-3].
[Table/Fig-3]:
Comparison of total quality of life in family caregivers for demographic characteristics.
| Variable | p-value | Correlation |
|---|---|---|
| Economic | p<0.0001 | Df=2 F=12.16 |
| Gender | 0.004 | Df=224 T=2.92 |
| Relationship with patient | 0.027 | Df=5 F=2.58 |
| Patient’s gender | 0.004 | Df=192.24 T= -2.92 |
Discussion
The findings of this study showed that the caregivers of patients with mental disorders obtained lower scores in all eight subscales of QoL with reference to the Iranian community standards. Some studies have confirmed the low QoL of the patients’ caregivers [7,20]. Mental illnesses are chronic and therefore psychiatric patient’s family members experience considerable stress. Families may encounter frustration, loneliness and boredom, causing disturbance of the QoL and mental, decline in physical health of family members as well as family dysfunction [5] and ultimately diminishing family health [21]. Ghahremani et al., found that the QoL of the family caregivers of patients with Schizophrenia to be acceptable, which is not in agreement with the present study, possibly due to the difference in the data gathering tools [9]. This study showed that the family caregivers had low QoL, which is consistent with the results of Zendjidjian et al., and Ghahremani et al., [8,9]. The findings showed that among eight subscales of QoL, the highest score was obtained for the physical function subscale, which is in agreement with Zendjidjian et al., study [8]. Among the caregivers, the lowest QoL was obtained in the caregivers of patients with substance use disorders. These patients’ QoL was considerably lower than the Iranian society standards [22]. The family caregivers of patients with substance use disorders experienced certain problems such as anxiety, fear, frustration, and impaired interpersonal relationships that would reduce the QoL of these people [23]. The caregivers’ gender had significant relationship with their QoL and the men obtained higher scores of QoL in all subscales compared with the women, which is in agreement with other studies [4,24]. Comparison of different subscales of QoL showed a statistically significant difference between the women and men in PF, vitality, emotional health, bodily pain and general health, which indicates that in health care delivery, the needs of men and women are different based on the caregiver’s perception and understanding which can be influenced by his/her gender. Therefore, differentiating between men and women can enable the health care workers to improve the QoL of all family members [25]. This findings of this study showed that most of the caregivers were women (72.3%), which is consistent with other studies [7,20,24,26]. Women are still considered the main caregivers all over the world. In the United States, female caregivers comprise 66% of all caregivers [26,27]. Considering the social background and familial and cultural norms as well as the expectations that strengthen the women’s caring role, women undertake this role more frequently than men so that the pressure of caring for the patients in home rests mainly on women’s shoulders, and accordingly they experience more negative impacts in their life [8,27]. The financial status has significant positive relationship with the QoL which is in agreement with the studies conducted by Ghahremani et al., Wong et al., and Andrén and Elmståhl [8,21,28] and inconsistent with Meecharoen et al., study [29]. Families with financial problems have limited access to health services, including medical and psychological treatments and face numerous limitations. These problems can cause adverse impacts on the family’s health. Most of such families experience more stress and mental health problems than others. A caregiver’s family relationship with the patient is significantly associated with his/her QoL. Among different relatives, the highest and lowest QoL was seen among the children and mothers, respectively. Regarding the health care delivered to the family, the parents’ and other family members’ needs are different, which should be considered in family training programs [25]. More than half of the caregivers had education levels of lower than high school completion, which is consistent with the study by Wong et al., [21]. There was no significant relationship between the caregivers’ QoL and their education level; this finding is in agreement with Meecharoen et al., study [29] and inconsistent with the studies by Ghahremani et al., and Wong et al., [9,21]. Moreover, marital status did not have significant relationship with the QoL as the single obtained the highest score followed by the married, the widows/widowers and the divorced.
There was a significant relationship between the patients’ gender and the caregivers’ QoL, such that the caregivers who cared for the female patients had higher QoL than those who cared for the male patients. No significant relationship was found between the QoL and age, which is in agreement with a study [27] and inconsistent with Wong et al., study [21]. There was no significant relationship between the duration of the patient’s illness and the caregiver’s QoL. In this study, the number of family members, the employment status and the illness diagnosis had no significant relationship with the caregivers’ QoL, which might be due to the low sample size or heterogeneity of the participants. Including the caregivers of patients with different mental disorders and identifying the factors related to the careqivers’ QoL was a strength of this study. However, further studies are recommended with larger sample size of the caregivers of patients with mental disorders. For example, interventional studies can be implemented to enhance the life skills to encounter psychosocial stressors and therefore prevent subsequent problems.
Limitation
A limitation of the present study was lack of considering cultural, economic and social differences among the caregivers, severity of the patients’ illness and emotional conditions of the caregivers during the study. The findings of this study may be affected by the patients’ data that were drawn from self-report questionnaires. Besides that, we had financial and time constraints to conduct this work.
Conclusion
According to the results of this study, it may be possible to obtain information about the factors influencing the QoL of the caregivers of patients with mental disorders. In this study, the QoL of these caregivers was obtained low. Therefore, it is important to develop suitable plans for improving their QoL at different subscales. Nurses can implement local and international changes to improve the caregivers’ QoL. Regular evaluation and screening of the caregivers’ QoL is necessary to identify the caregivers in need of support. Besides that, this helps to determine the needs of these patients’ families and to prevent adverse effects on other family members. Providing psychological counseling and educational programs seems essential for the patients’ families.
Conflict of Interest
The authors declared no potential conflict of interest regarding the research, authorship and/or publication of this article.
Acknowledgments
We hereby express our sincere thanks to all the patients’ caregivers who participated in this study despite abundant problems resulting from caring for their patients, the Tehran University of Medical Sciences for funding this work and all the honorable authorities of psychiatric hospitals in Tehran as well as the research assistants at Shahrekord, Iran, Tehran and Shahid Beheshti universities of medical sciences.
Financial or Other Competing Interests
None.
References
- [1].Zauszniewski JA, Bekhet AK, Suresky MJ. Effects on resilience of women family caregivers of adults with serious mental illness: the role of positive cognitions. Arch Psychiatr Nurs. 2009;23(6):412–22. doi: 10.1016/j.apnu.2008.12.004. [DOI] [PubMed] [Google Scholar]
- [2].Mohammadi MR, Davidian H, Noorbala AA, Malekafzali H, Naghavi HR, Pouretemad HR, et al. An epidemiological survey of psychiatric disorders in Iran. Clin Pract Epidemiol Ment Health. 2005;1:16. doi: 10.1186/1745-0179-1-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Sadeghirad B, Haghdoost AA, Amin-Esmaeili M, Ananloo ES, Ghaeli P, Rahimi-Movaghar A, et al. Epidemiology of major depressive disorder in iran: a systematic review and meta-analysis. Int J Prev Med. 2010;1(2):81–91. [PMC free article] [PubMed] [Google Scholar]
- [4].Gutierrez-Maldonado J, Caqueo-Urizar A, Kavanagh DJ. Burden of care and general health in families of patients with schizophrenia. Soc Psychiatry Psychiatr Epidemiol. 2005;40(11):899–904. doi: 10.1007/s00127-005-0963-5. [DOI] [PubMed] [Google Scholar]
- [5].Canam C, Acorn S. Quality of life for family caregivers of people with chronic health problems. Rehabil Nurs. 1999;24(5):192–6. 200. doi: 10.1002/j.2048-7940.1999.tb02176.x. [DOI] [PubMed] [Google Scholar]
- [6].Zauszniewski JA, Bekhet AK, Suresky MJ. Resilience in family members of persons with serious mental illness. Nurs Clin North Am. 2010;45(4):613–26. vii. doi: 10.1016/j.cnur.2010.06.007. [DOI] [PubMed] [Google Scholar]
- [7].Caqueo-Urizar A, Gutierrez-Maldonado J, Miranda-Castillo C. Quality of life in caregivers of patients with schizophrenia: a literature review. Health Qual Life Outcomes. 2009;7:84. doi: 10.1186/1477-7525-7-84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Zendjidjian X, Richieri R, Adida M, Limousin S, Gaubert N, Parola N, et al. Quality of life among caregivers of individuals with affective disorders. J Affect Disorders. 2012;136(3):660–65. doi: 10.1016/j.jad.2011.10.011. [DOI] [PubMed] [Google Scholar]
- [9].Ghahremani Z, Alavi MJ, Hosseini F. Correlates of quality of life in the family caregivers of schizophrenic patients with hope. Iran J Nurs. 2006;19:17–26. [Google Scholar]
- [10].Heydarnejad S, Dehkordi AH. The effect of an exercise program on the health-quality of life in older adults. A randomized controlled trial. Dan Med Bull. 2010;57(1):A4113. [PubMed] [Google Scholar]
- [11].Heydarnejad MS, Hassanpour DA, Solati DK. Factors affecting quality of life in cancer patients undergoing chemotherapy. Afr Health Sci. 2011;11(2):266–70. [PMC free article] [PubMed] [Google Scholar]
- [12].Hassanpour-Dehkordi A, Jivad N. Comparison of regular aerobic and yoga on the quality of life in patients with multiple sclerosis. Med J Islam Repub Iran. 2014;28:141. [PMC free article] [PubMed] [Google Scholar]
- [13].Wu HC. The protective effects of resilience and hope on quality of life of the families coping with the criminal traumatisation of one of its members. J Clin Nurs. 2011;20(13-14):1906–15. doi: 10.1111/j.1365-2702.2010.03664.x. [DOI] [PubMed] [Google Scholar]
- [14].Asadi Noghabi AA, Zandi M, Mehran A, Alavian SM, Dehkordi AH. The effect of education on quality of life in patients under interferon therapy. Hepat Mon. 2010;10(3):218–22. [PMC free article] [PubMed] [Google Scholar]
- [15].Dehkordi A, Heydarnejad MS, Fatehi D. Quality of life in cancer patients undergoing chemotherapy. Oman Med J. 2009;24(3):204–07. doi: 10.5001/omj.2009.40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Rapaport MH, Clary C, Fayyad R, Endicott J. Quality-of-life impairment in depressive and anxiety disorders. Am J Psychiatry. 2005;162(6):1171–78. doi: 10.1176/appi.ajp.162.6.1171. [DOI] [PubMed] [Google Scholar]
- [17].Fletcher BS, Miaskowski C, Given B, Schumacher K. The cancer family caregiving experience: an updated and expanded conceptual model. Eur J Oncol Nurs. 2012;16(4):387–98. doi: 10.1016/j.ejon.2011.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Hassanpour Dehkordi A, Khaledi Far A. Effect of exercise training on the quality of life and echocardiography parameter of systolic function in patients with chronic heart failure: a randomized trial. Asian J Sports Med. 2015;6(1):e22643. doi: 10.5812/asjsm.22643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].Hajbagheri A, Abbasinia M. Assessment of health-related quality of life in elderly patients with hip fracture with two instruments SF-36, EQ5D. Nurs Res. 2010;4:71–79. [Google Scholar]
- [20].Montazeri A, Goshtasebi A, Vahdaninia M, Gandek B. The Short Form Health Survey (SF-36): translation and validation study of the Iranian version. Qual Life Res. 2005;14(3):875–82. doi: 10.1007/s11136-004-1014-5. [DOI] [PubMed] [Google Scholar]
- [21].Wong DF, Lam AY, Chan SK, Chan SF. Quality of life of caregivers with relatives suffering from mental illness in Hong Kong: roles of caregiver characteristics, caregiving burdens, and satisfaction with psychiatric services. Health Qual Life Outcomes. 2012;10:15. doi: 10.1186/1477-7525-10-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Van Riper M. Families of children with Down syndrome: responding to "a change in plans" with resilience. J Pediatr Nurs. 2007;22(2):116–28. doi: 10.1016/j.pedn.2006.07.004. [DOI] [PubMed] [Google Scholar]
- [23].Sajjadi H, Vameghi M, Ghazinour M, Khodaeiardekani M. Caregivers’ quality of life and quality of services for children with cancer: a review from iran. Glob J Health Sci. 2013;5(3):173–82. doi: 10.5539/gjhs.v5n3p173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Marcon SR, Rubira EA, Espinosa MM, Barbosa DA. Quality of life and depressive symptoms among caregivers and drug dependent people. Rev Lat-Am Enferm. 2012;20(1):167–74. doi: 10.1590/s0104-11692012000100022. [DOI] [PubMed] [Google Scholar]
- [25].Khayatzadeh MM, Rostami HR, Amirsalari S, Karimloo M. Investigation of quality of life in mothers of children withcerebral palsy in Iran: association with socio-economic status, marital satisfaction and fatigue. Disabil Rehabil. 2013;35(10):803–08. doi: 10.3109/09638288.2012.708818. [DOI] [PubMed] [Google Scholar]
- [26].Schneider M, Steele R, Cadell S, Hemsworth D. Differences on psychosocial outcomes between male and female caregivers of children with life-limiting illnesses. J Pediatr Nurs. 2011;26(3):186–99. doi: 10.1016/j.pedn.2010.01.007. [DOI] [PubMed] [Google Scholar]
- [27].Khanjari S, Oskouie F, Langius-Eklof A. Lower sense of coherence, negative religious coping, and disease severity as indicators of a decrease in quality of life in iranian family caregivers of relatives with breast cancer during the first 6 months after diagnosis. Cancer Nurs. 2012;35(2):148–56. doi: 10.1097/NCC.0b013e31821f1dda. [DOI] [PubMed] [Google Scholar]
- [28].Andren S, Elmstahl S. Relationships between income, subjective health and caregiver burden in caregivers of people with dementia in group living care: A cross-sectional community-based study. Int J Nurs Stud. 2007;44(3):435–46. doi: 10.1016/j.ijnurstu.2006.08.016. [DOI] [PubMed] [Google Scholar]
- [29].Meecharoen W, Sirapo-Ngam Y, Monkong S, Oratai P, Northouse LL. Factors Influencing quality of life among family caregivers of patients with advanced cancer: A causal model. Pac Rim Int J Nurs Res. 2013;17:304–16. [Google Scholar]


